Abstract
Background
Outcome of acute experimental spinal cord injury is strongly associated with tissue perfusion and oxygenation. Cardiopulmonary depression could affect outcome in dogs undergoing general anesthesia for surgical treatment of thoracolumbar intervertebral disk extrusion (IVDE).
Hypothesis/Objectives
To evaluate the effects of general anesthesia on functional outcome in dogs undergoing surgery to treat thoracolumbar IVDE.
Animals
Eighty‐four client‐owned dogs with acute thoracolumbar IVDE treated by decompressive hemilaminectomy.
Methods
Exploratory, retrospective observational study. Medical records were reviewed for clinical presentation and anesthetic monitoring variables, including duration of anesthesia and surgery, hypotension, bradycardia, temperature, and respiratory parameters. Multivariable regression tree analysis was performed to explore associations between anesthetic variables and functional outcome scores after 6 weeks, as well as return to ambulatory status.
Results
Episodes of bradycardia (69%) and hypotension (57%) were frequent. Across all outcome measures, regression tree analysis highlighted functional grade at presentation as the primary determining factor, and among pain perception negative dogs, there was a possible association between increased duration of surgery and poorer outcome. In dogs with intact pain perception, duration of bradycardia, mean body temperature, and mean end‐tidal carbon dioxide were highlighted.
Conclusions and Clinical Importance
Exploratory statistical methods can facilitate hypothesis‐generating studies to inform prospective investigations in veterinary medicine. Although the mechanism is uncertain, increased duration of surgery might be associated with poorer outcome in pain perception negative dogs with thoracolumbar IVDE.
Keywords: Anesthesia, Canine, Intervertebral disk extrusion, Prognosis, Spinal cord injury
Abbreviations
- CRI
constant rate infusion
- ETCO2
end‐tidal carbon dioxide
- IQR
interquartile range
- IVDE
intervertebral disk extrusion
- LOCF
last observation carried forward
- MABP
mean arterial blood pressure
- MPSS
methylprednisolone sodium succinate
- NCSU
North Carolina State University
- OFS
open field score
- PEG
polyethylene glycol
- RI
regularity index
- SBP
systolic blood pressure
- SCI
spinal cord injury
Acute thoracolumbar intervertebral disk extrusion (IVDE) is the most common cause of acute spinal cord injury (SCI) in dogs and can cause death or permanent disability in affected dogs.1, 2 Treatment can be medical or surgical, with the decision to perform surgery based on clinical factors such as the severity and rate of progression of neurological deficits.3, 4, 5, 6, 7 Surgical management aims to decompress the spinal cord, usually through a hemilaminectomy procedure.8, 9
While the varying outcome of dogs with different initial severities of thoracolumbar SCI has been well described, the possibility that there are factors associated with surgical and anesthetic procedures that affect outcome has not been investigated.6, 10, 11, 12, 13, 14, 15 It has long been recognized in the experimental setting that perfusion of the spinal cord is highly associated with outcome.16, 17, 18 Recent human and veterinary studies have furthered our understanding of the role of spinal cord perfusion and hemodynamic changes, as well as the benefits of taking appropriate measures to maintain optimal spinal cord blood flow.19, 20, 21, 22, 23 Spinal cord perfusion is dependent on the relationship between systemic blood pressure and intrathecal pressure, in the same way that cerebral perfusion pressure is defined by mean arterial blood pressure (MABP) and intracranial pressure.17, 19, 24 Systemic hypotension might have serious consequences for the injured spinal cord, and alongside the avoidance of systemic hypoxia, management of blood pressure remains the mainstay of neuroprotective treatment in veterinary and human acute SCI.7, 19, 21, 25, 26
Hypotension secondary to reduced systemic vascular resistance or decreased cardiac output due to bradycardia occurs commonly under general anesthesia in dogs.27, 28, 29 As a result, it is possible that dogs undergoing surgical decompression to treat thoracolumbar IVDE could be exposed to hemodynamic changes that could affect functional recovery. Indeed, a recent study found an association between intraoperative hypotension and the frequency of adverse events after surgical management of cervical IVDE by ventral slot decompression.30 It is not known whether intraoperative variations in MABP, heart rate, and other measured variables, as well as duration of anesthesia or surgery, could affect outcome in dogs undergoing surgical management of thoracolumbar IVDE. This is a complex question to ask in a clinical population in which the majority of dogs recover ambulation. However, investigating the anesthetic records of a cohort of dogs with prospectively quantified outcome using exploratory statistical methodology could reveal associations worthy of further study. Furthermore, using an objective measure of normal stepping sequence, a function that is frequently not fully recovered, provides a highly discriminatory outcome measure with which to measure effects in these dogs.31
The primary aim of this exploratory study was therefore to investigate the relationship between intraoperative variables including systemic arterial blood pressure, heart rate, respiratory rate, body temperature, end‐tidal partial pressure of carbon dioxide and duration of anesthesia and surgery, and functional outcome in dogs undergoing decompressive surgery to treat acute IVDE in order to identify variables of interest to further investigate in prospective studies.
Materials and Methods
Case Selection
The dogs included in this study participated in 2 clinical trials at North Carolina State University (NCSU) Veterinary Hospital. The first was a trial evaluating the effect of methylprednisolone sodium succinate (MPSS) and polyethylene glycol (PEG) on outcome after acute SCI (n = 17),32 and the second was a trial evaluating the efficacy of cranberry extract compared to placebo (n = 67) at reducing prevalence of urinary tract infections after spinal surgery.33 Inclusion criteria for both of these trials included acute onset of thoracolumbar myelopathy due to an acute IVDE. In the first trial, all dogs were paraplegic with no conscious pain perception and had to present within 24 hours of onset of paralysis. For the second trial, dogs had to be nonambulatory paraparetic or paraplegic with or without conscious pain perception. All dogs underwent imaging and decompressive surgery, followed by a prescribed standardized home physical therapy plan and strict rest, as is standard protocol at the study institution. As neither trial demonstrated an effect of treatment over placebo, all dogs followed at NCSU were included in this study (from the first trial—MPSS: n = 6, PEG: n = 6, saline: n = 5, and from the second trial—cranberry: n = 32, placebo: n = 35).32, 33 For each dog, age, breed, sex and body weight were recorded, as well as duration of clinical signs, any preoperative medication administered by the referring veterinarian, IVDE site and ordinal functional grade (modified Tarlov grade: grade 1 = neurologically normal, grade 2 = ambulatory paraparesis, grade 3 = nonambulatory paraparesis, grade 4 = paraplegia with intact conscious pain perception, grade 5 = paraplegia with absent conscious pain perception) at presentation.34 Only nonambulatory dogs (grade 3, 4, or 5) were included. Exclusion criteria were as follows: incomplete medical or anesthetic records, dogs that underwent multiple spinal surgeries, dogs without follow‐up data, and those euthanized in the immediate postoperative period.
Anesthesia Records
Data acquired from anesthetic monitoring records included: number of periods of bradycardia (defined as heart rate <60 beats per minute [bpm] for at least 2 consecutive 5‐minute recordings), number of periods of hypotension (defined as MABP <60 mmHg or systolic blood pressure [SBP] <90 mmHg, for at least 2 consecutive 5‐minute recordings), episodes of cardiac arrhythmias, mean body temperature (°F), and end‐tidal carbon dioxide partial pressure (ETCO2—mmHg), and mean respiratory rate (spontaneous or mechanical ventilation) throughout the period of general anesthesia. The total duration of bradycardia and hypotension in minutes was then calculated by multiplying the number of recordings by 5. These parameters were monitored using continuous multiparameter patient monitoring systems during general anesthesia,1 , 2 with blood pressures recorded by indirect oscillometric (n = 75), indirect Doppler (n = 7), or direct invasive (n = 2) methods. All indirect blood pressure measurements were performed using inflatable cuffs applied to a target cuff width to leg circumference ratio of 40%. Blood pressure measurements were performed at table level, with dogs in sternal recumbency, approximating the level of the right atrium. Additional data acquired were duration of general anesthesia and duration of surgery, number of intervertebral spaces operated on, years of surgical training of the primary surgeon, drugs used for premedication, induction and maintenance of anesthesia, and any additional anesthesia medications or IV fluid boluses. Anesthetic protocol was selected based upon individual patient requirements and the preferences of the attending clinician and veterinary anesthesiologists. Cefazolin3 (22 mg/kg IV) was administered before surgery and every 2 hours intraoperatively for routine antibiosis in all dogs. Nonsteroidal anti‐inflammatories were administered perioperatively, unless contraindicated or if the dog was already receiving an oral course.
Outcome
Follow‐up data were acquired from records of re‐examinations performed at 6 weeks postoperatively. Outcome was assessed by recording whether the dog reached independent ambulatory status within 6 weeks, alongside 2 scoring methods: (1) ordinal 12‐point open field score (OFS, score of 1–12, as outlined in previous studies),35 and (2) a recently described treadmill‐based gait scoring method shown to generate linear, continuous outcome data (regularity index, RI).31 The latter method involves videotaping the dog attempting to walk on a treadmill and then recording the number and sequence of complete steps taken with each limb. From this data, using a total of 50‐step cycles, RI was calculated from the total number of step cycles taken in a normal step cycle pattern (as previously defined31) multiplied by 4 to give the total number of coordinated steps, and then divided by the total number of steps taken.36 Outcome using OFS was additionally quantified as the change in OFS from presentation to 6‐week re‐examination, with dogs presenting as modified Tarlov grades 4 and 5 (paraplegic with and without conscious pain perception) classified as an OFS of 0 at presentation, and grade 3 (nonambulatory paraparetic) at presentation classified as an OFS of 2 (representing the mean OFS that a grade 3 dog could have at presentation on the 12‐point scale). A full description of the technique used for acquiring the open field and treadmill scores is available elsewhere.31 For statistical analysis, when outcome data were missing for RI and OFS at 6 weeks, if data were available for 2 or 4 weeks postsurgery, this was also used as a measure of final outcome using the last‐observation‐carried‐forward (LOCF) convention.
Statistical Analysis
Before performing regression tree analysis to explore anesthetic variables, initial bivariate analysis was performed to exclude potential associations between outcome and preoperative descriptive patient variables. This was performed using independent‐samples t‐tests and chi‐square to evaluate normally distributed data and categorical variables, respectively, and Mann‐Whitney U‐ or Kruskal‐Wallis tests for non‐normally distributed data. Pearson's correlation coefficient was used to test for linear association between continuous variables. Clinical trial drugs were not included in statistical analysis due to the lack of effect demonstrated in prior analysis.32, 33 Data were evaluated for normality using Shapiro‐Wilk tests.
We then performed an exploratory data analysis of the recorded surgical and anesthetic data using regression tree analysis, which was used to identify candidate predictors to use in general linear and logistic regression models.37 Regression trees recursively partition the observed data into subgroups defined by thresholding subject covariates (such as premedication, surgery duration, duration of bradycardia so that subjects within each subgroup are similar in terms of the outcome of interest. Subgroups formed in this way can then be expressed as a binary tree from which it is easy to identify covariate interactions and associations between covariates and the outcome. For this analysis, functional grade at presentation as well as the recorded anesthetic variables (premedication drugs used, duration of general anesthesia, duration of surgery, number of disk spaces operated on, total duration of low MABP, total duration of low SBP, total duration of bradycardia, mean temperature, mean ETCO2, IV fluid boluses, and glycopyrrolate4 boluses as well as years of surgical training of the surgeon) was included to control for the well‐established effect of initial injury severity on outcome (Table 2).10, 12, 13, 15 The variables identified by the regression tree analysis were then selected for further multivariable analysis by fitting a linear model for continuous outcome scores (OFS and RI) fit using ordinary least squares, and a logistic regression model fit using maximum likelihood with a ridge penalty for the binary outcome measure (ambulatory status).38, 39 The reported coefficients are for the final selected models, where selection was performed using stepwise variable selection with the Bayesian information criterion. The full code to replicate our analyses is provided in Data 1. Statistical significance was established as P < .05 where relevant; however, because the initial set of candidate variables and the final selected model were chosen using the data, these P‐values are not uniformly distributed under the null (that the coefficient is zero) and might overstate statistical significance. Data analysis was performed using a commercially available statistical software program,5 and the “rpart” package in R.6
Table 2.
Summary of outcome according to functional grade at presentation
| Outcome Measure | Grade 3 (n = 25) | Grade 4 (n = 24) | Grade 5 (n = 35) | P | All Dogs (n = 84) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 6 Weeks | n | inc. LOCF | n | 6 Weeks | n | inc. LOCF | n | 6 Weeks | n | inc. LOCF | n | 6 Weeks | n | inc. LOCF | n | ||
| Ambulatory at 6 weeks | 25 (100) | 25 | n/a | 24 (100) | 24 | n/a | 16 (45.7) | 35 | n/a | <.001 | 65 (77.4) | 84 | n/a | ||||
| OFS | 11 (9–12) | 19 | 11 (8.8–12) | 22 | 9 (7–11) | 20 | 9 (7–11) | 23 | 6 (3–8) | 26 | 4 (2.8–8) | 30 | <.001 | 9 (6–11) | 65 | 8 (6–11) | 75 |
| OFS improvement | 8.5 (6.5–9.5) | 19 | 8.5 (6.3–9.5) | 22 | 9 (7–11) | 20 | 9 (7–11) | 23 | 6 (3–8) | 26 | 4 (2.8–8) | 30 | .001 | 8 (6–9.5) | 65 | 7.5 (4.5–9.5) | 75 |
| RI | 93.9 (87.4–97.9) | 16 | 93.1 (78.5–96.5) | 22 | 63 (50.2–95.2) | 17 | 63 (46.8–94.2) | 21 | 0 (0–37.1) | 14 | 0 (0–59.4) | 15 | <.001 | 63.0 (21.6–93.9) | 47 | 75.8 (33.7–93.9) | 58 |
OFS, open field score; RI, regularity index; LOCF, last observation carried forward.
Values are number of dogs (percentage), or median (25th–75th percentiles).
Results
Population
Of 91 dogs that fulfilled the initial inclusion criteria, 7 dogs were excluded due to lack of follow‐up data, leaving 84 suitable dogs. Breeds comprised 54 Dachshunds, 8 mixed‐breed dogs, 8 Pekingese dogs, 3 Chihuahuas, 3 Shih Tzus, 2 Beagles, and 1 each of the following breeds: Lhasa Apso, American Cocker Spaniel, Basset Hound, Boston Terrier, Maltese Terrier, and Pembroke Welsh Corgi. There were 50 male dogs (60%) of which 14 were sexually intact, and 34 female dogs (40%) of which 4 were sexually intact, with a mean age of 5.7 ± 2.5 years and a mean body weight of 7.7 ± 3.3 kg.
Clinical Characteristics
All dogs presented for further investigation of an acute onset of paraparesis or paraplegia, with neuroanatomical localization to a T3‐L3 (n = 81) or L4‐S3 (n = 3) myelopathy. Twenty‐five dogs (30%) presented with a modified Tarlov functional grade of 3, 24 (29%) were grade 4, and 35 (42%) were grade 5. Fifty‐eight dogs (69%) presented within 12 hours of the onset of clinical signs, 17 (20%) presented between 12 and 24 hours of onset, 5 dogs (6%) presented between 24 and 48 hours of onset, and 4 dogs (5%) presented >48 hours after the onset. Forty‐five dogs (54%) received no medication before referral, whereas 23 (27%) received nonsteroidal anti‐inflammatories, 15 (18%) received corticosteroids, and 1 dog (1%) received PEG before referral. IVDE was diagnosed on CT (n = 53), MRI (n = 29), or CT myelogram (n = 2), with decompressive hemilaminectomy subsequently performed in all dogs at the intervertebral disk spaces determined by the attending clinician. Forty‐seven hemilaminectomies (56%) were over a single intervertebral disk space, 26 (31%) were over 2 spaces, 7 (8%) were over 3 spaces, 3 (4%) were over 4 spaces, and 1 (1%) hemilaminectomy was performed over 5 spaces, all of which were on a single side. The hemilaminectomy site was between the T10‐11 and L1‐2 intervertebral disk spaces in 66 cases (79%), with 16 (19%) extending to, or exclusively between L2‐3 to L5‐6, as well as 1 procedure at the T8‐9 space and 1 at the T9‐10 space. Prophylactic fenestration was performed of the intervertebral disks from T11 to L3 in all dogs, as is standard procedure at the study institution. A durotomy was not performed in any of the dogs.
Anesthetic Parameters
Anesthetic premedication was IV or IM hydromorphone7 (0.05–0.2 mg/kg) alone in 40 dogs (48%), in combination with dexmedetomidine8 (2–4 mcg/kg) in 25 dogs (29.8%), dexmedetomidine alone in 1 dog (1%), and an IV bolus of fentanyl9 (2–5 mcg/kg) in 18 dogs (21%). Anesthesia was induced with propofol10 (4–6 mg/kg, IV to effect) in all dogs, except for 1 dog in which anesthesia was induced with a ketamine11 and midazolam12 combination. Isoflurane13 was used to maintain anesthesia in all dogs, with 6 dogs receiving sevoflurane14 during MRI before changing to isoflurane for surgery. A constant rate infusion (CRI) of fentanyl (0.3 μg/kg/min—adjusted as required) was also used in 50 dogs (60%), with a CRI of remifentanil15 (0.3 μg/kg/min—adjusted as required) used in 6 (7%).
Total general anesthesia time including diagnostic imaging lasted a mean of 5.1 ± 1.5 hours, with a mean surgical duration of 3.3 ± 1.2 hours. Of the monitored intraoperative patient variables, abnormalities of heart rate and blood pressure were commonly encountered, with 58 dogs experiencing episodes of bradycardia (69%) and 48 dogs experiencing episodes of hypotension (57%). Mean average body temperature during anesthesia for all dogs was 98.1 ± 1.6°F. Cardiac arrhythmias were detected in 12 dogs (14%), with 10 dogs experiencing transient 2nd degree atrioventricular block, 1 case experiencing transient 1st degree atrioventricular block, and 1 a ventricular arrhythmia, and all resolved with appropriate treatment. In response to hypotension, 28 (33%) dogs received an intraoperative isotonic crystalloid fluid bolus administered IV at some point during anesthesia, with 4 (5%) receiving an IV infusion of dopamine, and 39 (46%) dogs received a bolus of glycopyrrolate to address bradycardia. A summary of the recorded intraoperative anesthetic variables is shown in Table 1.
Table 1.
Summary of anesthetic variables
| Variable | All Dogs (n = 84) |
|---|---|
| Duration of general anesthesia (hours) | 5.1 ± 1.5 |
| Duration of surgery (hours) | 3.3 ± 1.2 |
| Perioperative hypotension—MABP | 32 (38.1) |
| Duration of hypotension (MABP, minutes) | 0 (0–10) |
| Minimum MABP (mmHg) | 54.8 ± 8.1 |
| Perioperative hypotension—SBP | 40 (47.6) |
| Duration of hypotension (SBP, minutes) | 0 (0–33.8) |
| Minimum SBP (mmHg) | 73.4 ± 11.9 |
| Perioperative bradycardia | 58 (69.0) |
| Duration of bradycardia (minutes) | 40 (0–115) |
| Minimum heart rate (bpm) | 49.6 ± 11.5 |
| Mean temperature (°F) | 98.1 ± 1.6 |
| Mean end‐tidal CO2 (mmHg) | 42.3 ± 4.6 |
| Ventilated respiratory rate (bpm) | 10 (8–12) |
| Perioperative arrhythmia | 12 (14.3) |
| Intravenous fluid bolus | 28 (33.3) |
| Glycopyrrolate bolus | 39 (46.4) |
| Dopamine constant rate infusion | 4 (4.8) |
MABP, mean arterial blood pressure; SBP, systolic blood pressure.
Values are mean ± standard deviation, median (25th–75th percentiles) or number of dogs (percentage).
Outcome
No dogs were euthanized in the immediate postoperative period. Ambulatory status 6 weeks postsurgery was available for all 84 dogs, with OFS available in 64 (76%) dogs, increasing to 75 dogs when including LOCF data (5 lost after 2 weeks, 6 lost after 4 weeks). Regularity index treadmill gait scores were available in 47 (56%) dogs, increasing to 58 dogs when including LOCF data (5 lost after 2 weeks, 6 lost after 4 weeks). Overall, 65 of 84 dogs (77%) regained ambulatory function within the 6‐week follow‐up period. The median OFS reached was 8.0 (interquartile range [IQR] 6.0–9.5) with an overall median improvement from presentation of 8.0 (IQR 6.0–11.0). Median RI treadmill gait score at the final follow‐up evaluation was 75.8 (IQR 33.7–93.9). Outcome data are summarized in Table 2, demonstrating the consistent negative effect of increasing functional grade at presentation across outcome measures. Tests for associations between outcome and preoperative patient variables are summarized in Table S1. Only a small positive correlation between patient age and RI outcome score was found, which is likely to be a result of the age distribution among groups of initial injury severity in this population, with the grade 3 group containing older dogs (mean 7.0 ± 2.4 years) than the more severely affected grade 4 (5.8 ± 3.0 years) or grade 5 (4.9 ± 1.9 years, P = .006) groups. Functional grade at presentation was selected for inclusion in regression tree analysis to control for this effect of initial injury severity on outcome.
Associations Between Anesthetic Variables and Outcome
The estimated regression tree displaying associations between recorded variables and OFS as an outcome measure is displayed in Figure 1. The subgroups of dogs with similar OFS improvements identified by the estimated regression tree are dictated by 4 covariates: functional grade at presentation, duration of surgery, duration of general anesthesia, and duration of bradycardia. The estimated regression tree for outcome as measured by RI is displayed in Figure 2, with subgroups dictated by functional grade at presentation, mean body temperature, and mean ETCO2. For ambulatory status at 6 weeks postoperatively, the estimated regression tree shows subgroups of similar outcomes determined by functional grade at presentation, duration of surgery, and duration of low SBP (Fig 3).
Figure 1.
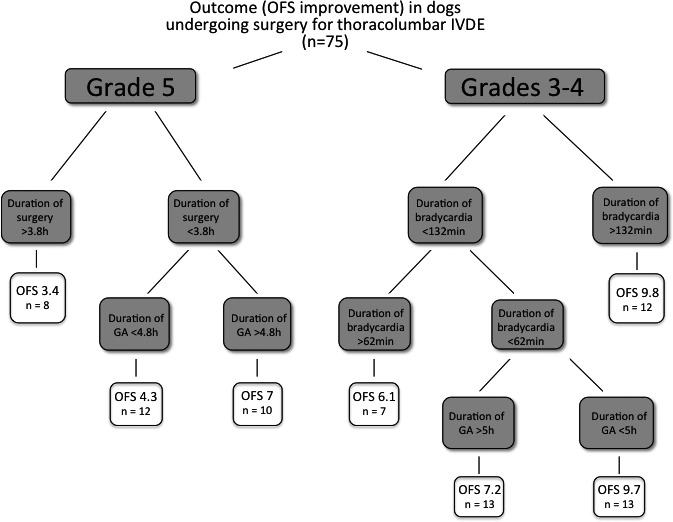
An estimated regression tree displaying associations between recorded variables and outcome, as measured by improvement in open field score (OFS: 0–12) 6 weeks after hemilaminectomy to treat intervertebral disk extrusion (IVDE). Each gray box represents a variable that subdivides the population—branches to the left correspond to a lower OFS and therefore poorer outcome while branches to the right correspond to subgroups with better outcome, with numbers in the terminal white boxes representing the estimated average OFS improvement achieved, and the number of dogs for that subgroup (n). The hierarchical nature of the tree suggests that the primary discriminating factor in predicting OFS improvement is functional grade at presentation (Grade), with Grade 5 dogs having poorer OFS improvement. Of the grade 5 dogs, those undergoing surgery of duration >3.8 hours had the poorest average OFS improvement of 3.4. In this way, each further branching describes the interactions between these variables and OFS improvement for different subgroups of dogs. This regression tree therefore suggests that there might be a relationship between OFS improvement and total duration of surgery, duration of general anesthesia (GA), and duration of bradycardia, and that these are therefore candidate variables for fitting a general linear model (Table 3).
Figure 2.
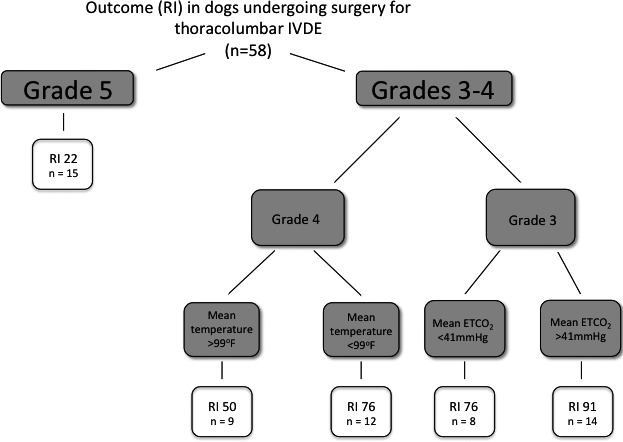
An estimated regression tree displaying associations between recorded variables and outcome, as measured by regularity index (RI: 0–100) 6 weeks after hemilaminectomy to treat intervertebral disk extrusion (IVDE). The branching of the tree follows the same rules as outlined for Figure 1. This regression tree therefore suggests that the primary discriminatory factor in predicting RI is functional grade at presentation (Grade), and that there might be a relationship between RI outcome and mean temperature and mean end‐tidal carbon dioxide (ETCO2) in grade 3 and grade 4 dogs. These candidate variables are therefore selected for fitting a general linear model to predict RI (Table 4).
Figure 3.
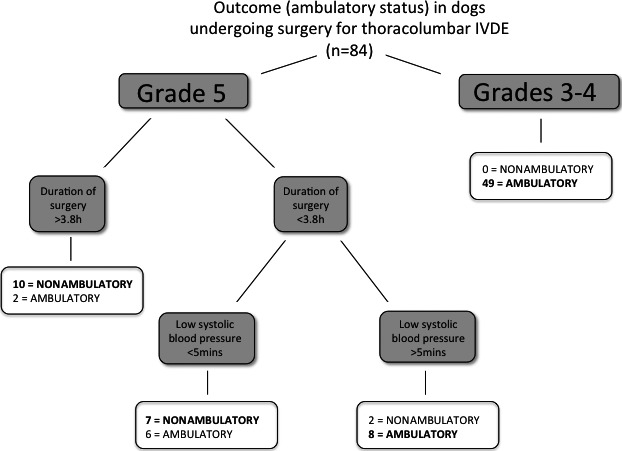
An estimated regression tree displaying associations between recorded variables and outcome, as measured by ambulatory status 6 weeks after hemilaminectomy to treat intervertebral disk extrusion (IVDE). The branching of the tree follows the same rules as outlined for Figure 1. This tree suggests that the primary discriminatory factor in predicting ambulatory status improvement is functional grade at presentation (Grade), and that of grade 5 dogs those undergoing surgery duration >3.8 hours might have a lower probability of regaining ambulatory status. There might also be a relationship between duration of low systolic blood pressure in a subgroup of dogs. These candidate variables are therefore selected for fitting a ridge regression model to predict ambulatory status (Table 5).
These variables were therefore carried forward and selected for further evaluation by fitting general linear or binary ridge regression models for each outcome measure. The final selected model for predicting OFS improvement suggests a negative association with functional grade 5 at presentation, duration of anesthesia, and total duration of bradycardia, with the latter 2 variables positively associated with each other (Table 3). The selected model for RI postsurgery retains only a negative association with increasing functional grade at presentation (Table 4). For predicting the binary outcome measure of ambulatory status 6 weeks postsurgery, the final selected ridge regression model suggests that alongside absence of conscious pain perception at presentation (functional grade 5), an increased duration of surgery was associated with decreased odds of regaining ambulatory function, while also controlling for duration of low SBP (Table 5). A receiver operating characteristic (ROC) curve for the fitted ridge regression model had an area under the curve of 0.94, and is included in Figure S1.
Table 3.
Final general linear model for predicting open field score improvement after surgery
| Variable | Category | Coefficient | 95% Confidence Interval | P | |
|---|---|---|---|---|---|
| Functional grade at presentation | 3 | Reference | Reference | n/a | |
| 4 | 0.63 | −0.97 | 2.24 | .44 | |
| 5 | −3.26 | −4.77 | −1.75 | <.001 | |
| Duration of anesthesia | −4.73 | −8.77 | −0.70 | .022 | |
| Duration of bradycardia | −1.90 | −3.56 | −0.24 | .026 | |
| Duration of anesthesia:bradycardia | 1.18 | 0.18 | 2.18 | .021 | |
This table shows the final selected general linear model for predicting open field score improvement. Reference indicates that grade 3 was used as the reference category within functional grade at presentation.
Table 4.
Final general linear model for predicting regularity index (RI) after surgery
| Variable | Category | Coefficient | 95% Confidence Interval | P | |
|---|---|---|---|---|---|
| Functional grade at presentation | 3 | Reference | Reference | n/a | |
| 4 | −19.82 | −35.86 | −3.77 | .016 | |
| 5 | −62.60 | −80.21 | −44.99 | <.001 | |
This table shows the final selected general linear model for predicting RI. Reference indicates that grade 3 was used as the reference category within functional grade at presentation.
Table 5.
Final ridge regression model for predicting ambulatory status 6 weeks after surgery
| Variable | Category | Odds Ratio | 95% Confidence Interval | P | |
|---|---|---|---|---|---|
| Duration of surgery (hours) | 0.78 | 0.55 | 0.98 | .035 | |
| Functional grade at presentation | 3 | Reference | Reference | n/a | |
| 4 | 2.36 | 1.93 | 3.13 | <.001 | |
| 5 | 0.14 | 0.08 | 0.25 | <.001 | |
| Duration of low SBP (minutes) | 1.009 | 1.003 | 1.016 | .005 | |
SBP, systolic blood pressure.
This table shows the final selected ridge regression model for predicting ambulatory status. Reference indicates that grade 3 was used as the reference category within functional grade at presentation.
Discussion
This study aimed to utilize exploratory statistical methodology to identify anesthetic variables of interest regarding outcome in a population of dogs undergoing surgical management of acute thoracolumbar IVDE. Our findings suggest that further studies are warranted to evaluate the potential significance of an increased duration of surgery or general anesthesia on outcome in these dogs, particularly those presenting paraplegic with absent pain perception. Total duration of bradycardia, duration of low SBP, mean temperature, and mean end‐tidal carbon dioxide during anesthesia were also highlighted by our regression tree analysis, identifying these areas as also worthy of further study. Periods of hypotension and bradycardia were particularly common occurrences during surgery in the study population. Associations between anesthetic or surgical variables and outcome in dogs with surgically managed thoracolumbar IVDE have not previously been reported, and the findings of the current study highlight areas of interest for further prospective investigations in this population of dogs.
The primary aim of the current study was to take an exploratory approach to a large dataset of recorded anesthetic variables, in a cohort of prospectively followed dogs after surgical management of acute thoracolumbar IVDE. This was achieved using the multivariable statistical technique of regression tree analysis, designed to extract potentially important associations within large volumes of data, such as multiple recorded anesthetic variables and outcome measures.37, 40 Without focusing on traditional measures of statistical significance, these analyses allowed us to highlight several variables as having potential associations with outcome, and therefore worthy of further study. Multivariable statistical modeling using these variables further supported the identified relationships in this population, although the reported P‐values should be treated with caution in light of this data‐driven model‐building procedure. While it is important to acknowledge that this affects the validity of the statistical significance in the models, the results support possible associations with outcome and assist in hypothesis generation and identification of targets for further studies, the primary aim of this study.
Using the regression tree approach, we found that across all measures of outcome (OFS, RI, and ambulatory status), the population of dogs could be initially divided into those presenting with a function grade of 5 (pain perception negative dogs) and those with grades 3 or 4 (Figs 1, 2, 3). Consistent with previous studies,11, 12, 13, 14, 15, 41, 42 45.7% of grade 5 dogs became ambulatory within 6 weeks, compared with 100% of grade 3 and 4 dogs. While the regression tree for the OFS outcome measure revealed conflicting effects of total duration of anesthesia in a small subgroup (Fig 1), considering the similar findings in the regression tree analysis for ambulatory status (Fig 3) as well as the final general linear and ridge regression models, the predominant relationship identified in grade 5 dogs was a poorer outcome with increased duration of surgery (Figs 1, 3; Tables 3, 5). An increased duration of surgery could result from a number of different parameters including more extensive spinal cord compression requiring a multilevel hemilaminectomy, differences in the volume of disk material, intraoperative hemorrhage, number of disks fenestrated (although this was uniform in the current study population), and the skill or experience of the surgeon. An increased duration of surgery could be related to a more challenging procedure, potentially due to the nature of the disk extrusion, and could therefore be directly related to the intrinsic severity of the initial contusion, cord compression, and consequent SCI. Indeed, a recent study found a small but statistically significant association between increased surgical duration and postoperative neurological deterioration in dogs undergoing potentially more complex cervical dorsal laminectomy procedures.43 In the current study, parameters that might affect surgery duration such as the number of sites surgically decompressed, and surgical expertise was not identified in the regression tree analysis as influencing outcome. A prospective study design would be of interest to address more specific questions, for example regarding the degree of difficulty in removing herniated disk material, extent of decompression, or number of sites fenestrated in order to investigate this potential association between outcome and surgical duration further as this could have implications for decision making regarding surgical procedures. Further investigations should aim to determine whether this is a true relationship but merely a reflection of initial injury severity, or a sign of damaging consequences of longer anesthesia.
Aside from reflecting the intrinsic severity of the initial injury, the association between surgical duration and outcome could also support the possibility that increased exposure to the cardiopulmonary consequences of general anesthesia, such as fluctuations in MABP and heart rate, ventilation, or other less well‐defined parameters, could have deleterious consequences. In the current study population, hemodynamic changes during general anesthesia were common, as is reported widely in veterinary medicine (Table 1).27, 28, 29 Episodes of bradycardia were recorded in 69.4% of dogs, recently reported to be a common finding in miniature Dachshunds, the most common breed in the current study.44 Our regression tree analysis highlighted a possible association between duration of bradycardia and OFS improvement in grade 3 or 4 dogs (Fig 1). Although this does not imply statistical significance and the 2 branches pertaining to duration of bradycardia suggest alternate directions for this association, duration of bradycardia was retained in the final general linear model for predicting OFS improvement suggesting there could be a potential relationship worthy of further study. Similarly, there was a possible association between increased duration of low SBP (<90 mmHg) and achieving ambulatory status (Fig 3). However, this relationship was only present in 1 subgroup of dogs and the duration of low MABP was not highlighted by the regression tree models. It is possible that the retrospective analysis of anesthetic records in the current study, from data recorded at 5‐minute intervals using predominantly indirect blood pressure recording techniques, meant that the severity and regularity of hypotension were underestimated. A recent study also suggested that acute spikes of systemic hypertension at the time of experimental SCI are associated with poorer outcome in rodent models, suggesting that both extremes of blood pressure might in fact have harmful consequences, and hypertension would have been missed with the current study design.45 The effect of systemic hypotension on outcome in acute SCI has been extensively evaluated in experimental studies and human medicine.21, 26 As a consequence of the loss of autoregulation that occurs during acute secondary SCI, spinal cord blood flow becomes directly vulnerable to fluctuations in MABP and intrathecal pressure.17, 46 A recent study in dogs undergoing ventral slot surgery for cervical IVDE found perioperative hypotension to be associated with major adverse events, including neurological deterioration.30 It is important to consider however that perioperative hypotension might be a more clinically significant finding in cervical spinal surgery due to a greater risk of serious hemorrhage.30, 47 The results of the current study therefore suggest that in dogs undergoing surgical decompression to treat acute thoracolumbar IVDE, a scenario whereby autoregulation of spinal cord blood flow is likely to be compromised and intrathecal pressure increased,22, 48 episodes of hypotension and bradycardia are common. Dogs undergoing longer periods of general anesthesia for more complicated surgical procedures might therefore be subjected to suboptimal spinal cord blood flow, potentially harming SCI recovery.22, 23, 48 As a result, a prospective study design utilizing frequent, direct blood pressure recordings including both extremes of fluctuation in a large number of dogs is required to further evaluate the clinical significance of blood pressure in this population of dogs.
There was 1 regression tree subdivision that suggested improved RI outcome scores in a subgroup of grade 4 dogs with lower mean body temperatures during anesthesia (Fig 2). Therapeutic systemic or local hypothermia has been widely evaluated in the human and experimental animal literature as a neuroprotective strategy for SCI management, with highly variable results so far.49 However, most studies have utilized moderate (82–90°F) to modest (90–93°F) degrees of systemic hypothermia to achieve beneficial effects.49, 50 These are degrees of hypothermia far more marked than that experienced by the dogs in this study, where we recorded a mean average temperature of 98.1°F, and only 16 dogs (19.0%) had mean body temperatures of <97°F. As a result, this finding should be treated with caution given the narrow range of temperatures observed, with only relatively mild degrees of hypothermia recorded. Similarly, the same regression tree subdivided grade 3 dogs according to mean ETCO2, with improved RI scores associated with increased mean ETCO2. Although increased arterial partial pressure of carbon dioxide has been shown experimentally to increase spinal cord blood flow through changes in local vascular resistance,51 our finding does not suggest a causal relationship with outcome at this stage and only concerns a subgroup of grade 3 dogs for which RI was available (n = 22). This does however highlight another potential area for further investigation with carefully designed study protocols.
While this study leverages prospective outcome data due to the inclusion of dogs enrolled in clinical trials, 1 limitation is that it was retrospective with regard to the collection and exploratory analysis of anesthetic records. As a result, the number of cases suitable for inclusion was limited, with the expected instances of missing and incomplete data. To capture follow‐up and anesthetic data more reliably, a prospective study design is required, although this would reduce case recruitment and therefore potentially limit statistical power.10 Due to the retrospective nature of anesthetic data collection, most cases in the current study underwent indirect oscillometric blood pressure recordings, which might be inferior to direct invasive recordings.52 Although the oscillometric monitor used in this study1 has previously been evaluated for validity with encouraging results,53 this method does reduce the accuracy of measurements when compared to direct arterial measurement and the results should be considered in light of this. Future studies could therefore better evaluate associations between hemodynamic anesthetic variables and long‐term outcome by utilizing more consistent techniques for prospectively monitoring intraoperative systemic perfusion parameters, such as continuously recorded direct arterial blood pressure recordings,26 as well as defined anesthetic medication protocols and using recently described methods for directly monitoring local indicators of tissue perfusion such as spinal cord blood flow and intraspinal pressure.19, 22, 23, 48 A prospective design in future studies could also utilize recordings of other downstream indicators of tissue perfusion such as plasma l‐lactate concentration. Although the anesthetic drugs used in the current study did not appear to have an association with outcome, there were a limited number of protocols used whereas a prospective study would allow direct evaluation of different treatment groups. Another limitation of the current study is the lack of longer term follow‐up data beyond 6 weeks postoperatively, as some dogs that were nonambulatory at 6 weeks could have gone on to recover ambulatory function in the longer term. However, previous studies have shown that the majority of postoperative functional recovery after SCI in dogs occurs within 4–8 weeks of surgery, supporting this observation time frame.11, 13, 32, 42 To maximize the outcome data available, we used 2 functional scoring systems postsurgery; an ordinal 12‐point score (OFS) and a treadmill‐based gait score (RI), both described and validated previously.31, 35 The RI treadmill gait score yields a more discriminatory continuous score from 0 to 100, allowing more accurate quantification of function within 6 weeks of surgery compared to more traditional ordinal scales or the binary outcome of ambulatory status.31, 33 In prior work, recovery of RI has been shown to be incomplete even in dogs that recover strong ambulation, increasing the chances of detecting clinically relevant effects.33 However, relatively low numbers of dogs in current study with complete RI outcome data limited the strength of this analysis.
In conclusion, this study reports an initial investigation of the effect of recorded anesthetic and surgical parameters on outcome in dogs undergoing surgical management of acute thoracolumbar IVDE. By taking an exploratory, hypothesis‐generating approach using regression tree analysis to evaluate the associations among multiple anesthetic variables and prospectively recorded outcome scores, our results highlight several areas of interest for further study. These include the possibility that an increased duration of surgery might be negatively associated with outcome, particularly in dogs presenting with paraplegia and absent conscious pain perception. Further studies with prospectively determined anesthetic protocols and measurement techniques, allowing more accurate characterization of potential surgical challenges and hemodynamic changes during surgery, are now required to investigate these potential relationships further.
Supporting information
Data S1. EDA for outcome measures associated with GA.
Table S1. Results of tests of bivariate associations between patient variables and final outcome for all dogs.
Fig S1. A receiver operating characteristic (ROC) curve for the ridge regression model in Table 5 of the manuscript. The area under the curve is 0.94.
Acknowledgments
Any opinions, findings and conclusions, or recommendations expressed in this material are those of the authors and do not necessarily reflect those of the National Science Foundation.
Grant support: The authors acknowledge the support of the Morris Animal Foundation through grants D07CA‐064 and D10CA‐022. This work was supported in part by the Division of Mathematical Sciences of the National Science Foundation through grants DMS‐1557733 and DMS‐1513579
Conflict of Interest Declaration: Authors declare no conflict of interest.
Off‐label Antimicrobial Declaration: Authors declare no off‐label use of antimicrobials.
The research was performed at the College of Veterinary Medicine, North Carolina State University.
This research included dogs enrolled on clinical trials supported by the Morris Animal Foundation.
Footnotes
Cardell Veterinary Monitor, Midmark Corporation, OH
Passport 8 Patient Monitor, Mindray DS USA Inc, Mahwah, NJ
West‐Ward Pharmaceutical Corp, Eatontown, NJ
American Regent Inc, Shirley, NJ
SPSS v22, IBM SPSS Inc, Chicago, IL
R Core Team (2015). R: A language and environment for statistical computing. R Foundation for Statistical Computing, Vienna, Austria. ISBN 3‐900051‐07‐0, URL http://www.R-project.org/; rpart package: https://cran.r-project.org/web/packages/rpart/vignettes/longintro.pdf
Hydromorphone HCl, West‐Ward Pharmaceutical Corp
Dexdomitor, Zoetis Inc, Kalamazoo, MI
Fentanyl Citrate, Hospira Inc, Lake Forest, IL
Hospira Inc, Lake Forest, IL
Ketamine Hydrochloride, Putney Inc, Portland, ME
Midazolam Injection, Hospira Inc
Piramal Enterprises Ltd, Andhra Pradesh, India
SevoFlo, Abbott Laboratories, North Chicago, IL
Ultiva, Mylan Institutional LLC, Rockford, IL
References
- 1. Fluehmann G, Doherr MG, Jaggy A. Canine neurological diseases in a referral hospital population between 1989 and 2000 in Switzerland. J Small Anim Pract 2006;47:582–587. [DOI] [PubMed] [Google Scholar]
- 2. Granger N, Carwardine D. Acute spinal cord injury: Tetraplegia and paraplegia in small animals. Vet Clin North Am Small Anim Pract 2014;44:1131–1156. [DOI] [PubMed] [Google Scholar]
- 3. Levine JM, Levine GJ, Johnson SI, et al. Evaluation of the success of medical management for presumptive thoracolumbar intervertebral disk herniation in dogs. Vet Surg 2007;36:482–491. [DOI] [PubMed] [Google Scholar]
- 4. Jeffery ND, Levine JM, Olby NJ, et al. Intervertebral disk degeneration in dogs: Consequences, diagnosis, treatment, and future directions. J Vet Intern Med 2013;27:1318–1333. [DOI] [PubMed] [Google Scholar]
- 5. Brisson BA. Intervertebral disc disease in dogs. Vet Clin North Am Small Anim Pract 2010;40:829–858. [DOI] [PubMed] [Google Scholar]
- 6. Ferreira AJ, Correia JH, Jaggy A. Thoracolumbar disc disease in 71 paraplegic dogs: Influence of rate of onset and duration of clinical signs on treatment results. J Small Anim Pract 2002;43:158–163. [DOI] [PubMed] [Google Scholar]
- 7. Olby N. The pathogenesis and treatment of acute spinal cord injuries in dogs. Vet Clin North Am Small Anim Pract 2010;40:791–807. [DOI] [PubMed] [Google Scholar]
- 8. McKee WM. A comparison of hemilaminectomy (with concomitant disc fenestration) and dorsal laminectomy for the treatment of thoracolumbar disc protrusion in dogs. Vet Rec 1992;130:296–300. [DOI] [PubMed] [Google Scholar]
- 9. Wheeler S, Sharp N. Thoracolumbar disc disease In: Wheeler Sharp, ed. Small Animal Spinal Disorders: Diagnosis and Surgery, Vol. London: Mosby, 2004:121–159. [Google Scholar]
- 10. Olby N, Harris T, Burr J, et al. Recovery of pelvic limb function in dogs following acute intervertebral disc herniations. J Neurotrauma 2004;21:49–59. [DOI] [PubMed] [Google Scholar]
- 11. Olby N, Levine J, Harris T, et al. Long‐term functional outcome of dogs with severe injuries of the thoracolumbar spinal cord: 87 cases (1996–2001). J Am Vet Med Assoc 2003;222:762–769. [DOI] [PubMed] [Google Scholar]
- 12. Laitinen OM, Puerto DA. Surgical decompression in dogs with thoracolumbar intervertebral disc disease and loss of deep pain perception: A retrospective study of 46 cases. Acta Vet Scand 2005;46:79–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Scott HW, McKee WM. Laminectomy for 34 dogs with thoracolumbar intervertebral disc disease and loss of deep pain perception. J Small Anim Pract 1999;40:417–422. [DOI] [PubMed] [Google Scholar]
- 14. Yovich JC, Read R, Eger C. Modified lateral spinal decompression in 61 dogs with thoracolumbar disc protrusion. J Small Anim Pract 1994;35:351–356. [Google Scholar]
- 15. Jeffery ND, Barker AK, Hu HZ, et al. Factors associated with recovery from paraplegia in dogs with loss of pain perception in the pelvic limbs following intervertebral disk herniation. J Am Vet Med Assoc 2016;248:386–394. [DOI] [PubMed] [Google Scholar]
- 16. Guha A, Tator CH, Rochon J. Spinal cord blood flow and systemic blood pressure after experimental spinal cord injury in rats. Stroke 1989;20:372–377. [DOI] [PubMed] [Google Scholar]
- 17. Martirosyan NL, Feuerstein JS, Theodore N, et al. Blood supply and vascular reactivity of the spinal cord under normal and pathological conditions. J Neurosurg Spine 2011;15:238–251. [DOI] [PubMed] [Google Scholar]
- 18. Tator CH, Fehlings MG. Review of the secondary injury theory of acute spinal cord trauma with emphasis on vascular mechanisms. J Neurosurg 1991;75:15–26. [DOI] [PubMed] [Google Scholar]
- 19. Werndle MC, Saadoun S, Phang I, et al. Monitoring of spinal cord perfusion pressure in acute spinal cord injury: Initial findings of the injured spinal cord pressure evaluation study. Crit Care Med 2014;42:646–655. [DOI] [PubMed] [Google Scholar]
- 20. Phang I, Werndle MC, Saadoun S, et al. Expansion duroplasty improves intraspinal pressure, spinal cord perfusion pressure, and vascular pressure reactivity index in patients with traumatic spinal cord injury: Injured spinal cord pressure evaluation study. J Neurotrauma 2015;32:865–874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Vale FL, Burns J, Jackson AB, et al. Combined medical and surgical treatment after acute spinal cord injury: Results of a prospective pilot study to assess the merits of aggressive medical resuscitation and blood pressure management. J Neurosurg 1997;87:239–246. [DOI] [PubMed] [Google Scholar]
- 22. Malik Y, Spreng D, Konar M, et al. Laser‐Doppler measurements of spinal cord blood flow changes during hemilaminectomy in chondrodystrophic dogs with disk extrusion. Vet Surg 2009;38:457–462. [DOI] [PubMed] [Google Scholar]
- 23. Blaser A, Lang J, Henke D, et al. Influence of durotomy on Laser‐Doppler measurement of spinal cord blood flow in chondrodystrophic dogs with thoracolumbar disk extrusion. Vet Surg 2012;41:221–227. [DOI] [PubMed] [Google Scholar]
- 24. Noussitou FL, Gorgas D, Rohrbach H, et al. Assessment of intramedullary spinal pressure in small breed dogs with thoracolumbar disk extrusion undergoing hemilaminectomy. Vet Surg 2015;44:944–948. [DOI] [PubMed] [Google Scholar]
- 25. Hawryluk GW, Rowland J, Kwon BK, et al. Protection and repair of the injured spinal cord: A review of completed, ongoing, and planned clinical trials for acute spinal cord injury. Neurosurg Focus 2008;25:E14. [DOI] [PubMed] [Google Scholar]
- 26. Hawryluk GW, Whetstone WD, Saigal R, et al. Mean arterial blood pressure correlates with neurological recovery following human spinal cord injury: Analysis of high frequency physiologic data. J Neurotrauma 2015;32:1958–1967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Iizuka T, Kamata M, Yanagawa M, et al. Incidence of intraoperative hypotension during isoflurane‐fentanyl and propofol‐fentanyl anaesthesia in dogs. Vet J 2013;198:289–291. [DOI] [PubMed] [Google Scholar]
- 28. Costa RS, Raisis AL, Hosgood G, et al. Preoperative factors associated with hypotension in young anaesthetised dogs undergoing elective desexing. Aust Vet J 2015;93:99–104. [DOI] [PubMed] [Google Scholar]
- 29. Gaynor JS, Dunlop CI, Wagner AE, et al. Complications and mortality associated with anesthesia in dogs and cats. J Am Anim Hosp Assoc 1999;35:13–17. [DOI] [PubMed] [Google Scholar]
- 30. Rossmeisl JH Jr, White C, Pancotto TE, et al. Acute adverse events associated with ventral slot decompression in 546 dogs with cervical intervertebral disc disease. Vet Surg 2013;42:795–806. [DOI] [PubMed] [Google Scholar]
- 31. Olby NJ, Lim JH, Babb K, et al. Gait scoring in dogs with thoracolumbar spinal cord injuries when walking on a treadmill. BMC Vet Res 2014;10:58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Olby NJ, Muguet‐Chanoit AC, Lim JH, et al. A placebo‐controlled, prospective, randomized clinical trial of polyethylene glycol and methylprednisolone sodium succinate in dogs with intervertebral disk herniation. J Vet Intern Med 2016;30:206–214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Rousse CA, Olby NJ, Williams K, et al. Recovery of stepping and coordination in dogs following acute thoracolumbar intervertebral disc herniations. Vet J 2016;213:59–63. [DOI] [PubMed] [Google Scholar]
- 34. Tarlov IM, Klinger H. Spinal cord compression studies. II. Time limits for recovery after acute compression in dogs. AMA Arch Neurol Psychiatry 1954;71:271–290. [PubMed] [Google Scholar]
- 35. Olby NJ, De Risio L, Munana KR, et al. Development of a functional scoring system in dogs with acute spinal cord injuries. Am J Vet Res 2001;62:1624–1628. [DOI] [PubMed] [Google Scholar]
- 36. Koopmans GC, Deumens R, Honig WM, et al. The assessment of locomotor function in spinal cord injured rats: The importance of objective analysis of coordination. J Neurotrauma 2005;22:214–225. [DOI] [PubMed] [Google Scholar]
- 37. Breiman L. Classification and Regression Trees. Belmont, CA: Wadsworth; 1984. [Google Scholar]
- 38. Hoerl AE, Kennard RW. Ridge regression ‐ biased estimation for nonorthogonal problems. Technometrics 1970;12:55–67. [Google Scholar]
- 39. Hastie T, Tibshirani R, Friedman JH. The Elements of Statistical Learning: Data Mining, Inference, and Prediction. New York, NY: Springer; 2001. [Google Scholar]
- 40. Lemon SC, Roy J, Clark MA, et al. Classification and regression tree analysis in public health: Methodological review and comparison with logistic regression. Ann Behav Med 2003;26:172–181. [DOI] [PubMed] [Google Scholar]
- 41. Loughin CA, Dewey CW, Ringwood PB, et al. Effect of durotomy on functional outcome of dogs with type I thoracolumbar disc extrusion and absent deep pain perception. Vet Comp Orthop Traumatol 2005;18:141–146. [PubMed] [Google Scholar]
- 42. Ito D, Matsunaga S, Jeffery ND, et al. Prognostic value of magnetic resonance imaging in dogs with paraplegia caused by thoracolumbar intervertebral disk extrusion: 77 cases (2000–2003). J Am Vet Med Assoc 2005;227:1454–1460. [DOI] [PubMed] [Google Scholar]
- 43. Taylor‐Brown FE, Cardy TJ, Liebel FX, et al. Risk factors for early post‐operative neurological deterioration in dogs undergoing a cervical dorsal laminectomy or hemilaminectomy: 100 cases (2002–2014). Vet J 2015;206:327–331. [DOI] [PubMed] [Google Scholar]
- 44. Harrison RL, Clark L, Corletto F. Comparison of mean heart rate in anaesthetized dachshunds and other breeds of dog undergoing spinal magnetic resonance imaging. Vet Anaesth Analg 2012;39:230–235. [DOI] [PubMed] [Google Scholar]
- 45. Nielson JL, Paquette J, Liu AW, et al. Topological data analysis for discovery in preclinical spinal cord injury and traumatic brain injury. Nat Commun 2015;6:8581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Hickey R, Albin MS, Bunegin L, et al. Autoregulation of spinal cord blood flow: Is the cord a microcosm of the brain? Stroke 1986;17:1183–1189. [DOI] [PubMed] [Google Scholar]
- 47. Smith BA, Hosgood G, Kerwin SC. Ventral slot decompression for cervical intervertebral disc disease in 112 dogs. Aust Vet Pract 1997;27:58–64. [Google Scholar]
- 48. Kunz RE, Rohrbach H, Gorgas D, et al. Assessment of intrathecal pressure in chondrodystrophic dogs with acute thoracolumbar disk disease. Vet Surg 2015;44:687–693. [DOI] [PubMed] [Google Scholar]
- 49. Alkabie S, Boileau AJ. The role of therapeutic hypothermia after traumatic spinal cord injury‐a systematic review. World Neurosurg 2016;86:432–449. [DOI] [PubMed] [Google Scholar]
- 50. Purdy PD, Novakovic RL, Giles BP, et al. Spinal cord hypothermia without systemic hypothermia. Am J Neuroradiol 2013;34:252–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51. Griffiths IR. Spinal cord blood flow in dogs. 2. The effect of the blood gases. J Neurol Neurosurg Psychiatry 1973;36:42–49. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Seliskar A, Zrimsek P, Sredensek J, et al. Comparison of high definition oscillometric and Doppler ultrasound devices with invasive blood pressure in anaesthetized dogs. Vet Anaesth Analg 2013;40:21–27. [DOI] [PubMed] [Google Scholar]
- 53. Sawyer DC, Guikema AH, Siegel EM. Evaluation of a new oscillometric blood pressure monitor in isoflurane‐anesthetized dogs. Vet Anaesth Analg 2004;31:27–39. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1. EDA for outcome measures associated with GA.
Table S1. Results of tests of bivariate associations between patient variables and final outcome for all dogs.
Fig S1. A receiver operating characteristic (ROC) curve for the ridge regression model in Table 5 of the manuscript. The area under the curve is 0.94.


