Abstract (English)
Sonographic cardiac evaluation of newborns with suspected aortic coarctation (AoC) should tend to demonstrate a good phasic and pulsatile flow and the absence of pressure gradient along a normally conformed aortic arch from the modified left parasternal and suprasternal echocardiographic views; these findings, however, may not necessarily rule out a more distal coarctation in the descending aorta. For this reason, the sonographic exam of newborns with suspected AoC should always include a Doppler evaluation of abdominal aortic blood flow from the subcostal view. Occasionally, however, a clearly pulsatile Doppler flow trace in abdominal aorta may be difficult to obtain due to the bad insonation angle existing between the probe and the vessel. In such suboptimal ultrasonic alignment situation, the use of Tissue Doppler Imaging instead of classic Doppler flow imaging may reveal a preserved aortic pulsatility by sampling the aortic wall motion induced by normal flow. We propose to take advantage of the TDI pattern as a surrogate of a normal pulsatile Doppler flow trace in abdominal aorta when the latter is difficult to obtain due to malalignment with the insonated vessel.
Keywords: Tissue Doppler Imaging, Neonatology, Aortic coarctation, Newborn, Pediatric cardiology, Echocardiography
Abstract (Italian)
La valutazione ecocardiografica del neonato con sospetta coartazione aortica deve poter dimostrare, dalle proiezioni parasternale sinistra alta e soprasternale, un arco aortico normoconformato con traccia Doppler normale (flusso fasico) in assenza di gradiente transistmico; tali rilievi, tuttavia, non escludono la possibilità di una coartazione aortica più distale, sita in aorta discendente toracica. Per tale motivo, la valutazione ecografica neonatale nel sospetto di coartazione aortica deve sempre includere un’analisi Doppler del flusso in aorta discendente, visualizzata tramite approccio sottocostale. Talvolta, tuttavia, l’angolo che si viene a creare tra il fascio ultrasonoro e il vaso a questo livello può risultare subottimale ai fini di un adeguato campionamento Doppler che dimostri la presenza di flusso fasico e privo di run-off diastolico in aorta addominale. In tale situazione di allineamento non ottimale per l’analisi Doppler classica, la metodica TDI (Tissue Doppler Imaging) può rivelare una preservata pulsatilità aortica tramite l’analisi della motilità di parete del vaso indotta dal normale flusso fasico. Tale metodica di valutazione della pulsatilità di parete aortica potrebbe, se validata attraverso studi di numerosità adeguata sul neonato sano, rappresentare un adeguato surrogato di una traccia Doppler normale in aorta addominale nei casi in cui quest’ultima fosse difficoltosa da ottenere a causa di un malallineamento tra il vaso ed il fascio ultrasonoro esplorante.
One pivotal skill that must be mastered by ultrasonographers in the Neonatal Intensive Care Unit (NICU) setting is the evaluation of aortic arch and abdominal aortic flow in order to rule out a possible aortic coarctation (AoC) following physiologic ductal closure in the newborn [1], which usually occurs after 48 to 96 h of postnatal age in term infants [2].
After ductal closure, a good phasic and pulsatile flow and no pressure gradient should be observed along a normally conformed aortic arch from the modified left parasternal and suprasternal echocardiographic views; these findings, however, may not necessarily rule out a more distal coarctation in the descending aorta.
The sonographic exam of newborns with suspected AoC should then always include a Doppler evaluation of abdominal aortic blood flow from the subcostal view, caring to minimize the color box dimensions in order to improve the frame rate and enhance the color resolution, set the color Doppler gain at less than noise level, and avoid a too low pulse repetition frequency (PRF) to prevent aliasing.
However, even with an optimal machine setting, a clearly pulsatile Doppler flow trace in abdominal aorta may sometimes be difficult to obtain due to the bad insonation angle existing between the probe and the vessel (Fig. 1).
Fig. 1.

Pulsed-wave Doppler of abdominal aorta. Due to the bad insonation angle, scarce information about actual flow pulsatility at this level can be inferred
In such suboptimal ultrasonic alignment situation, the use of Tissue Doppler Imaging (TDI) instead of classic Doppler flow imaging may reveal a preserved aortic pulsatility by sampling the aortic wall motion induced by normal flow (Fig. 2).
Fig. 2.
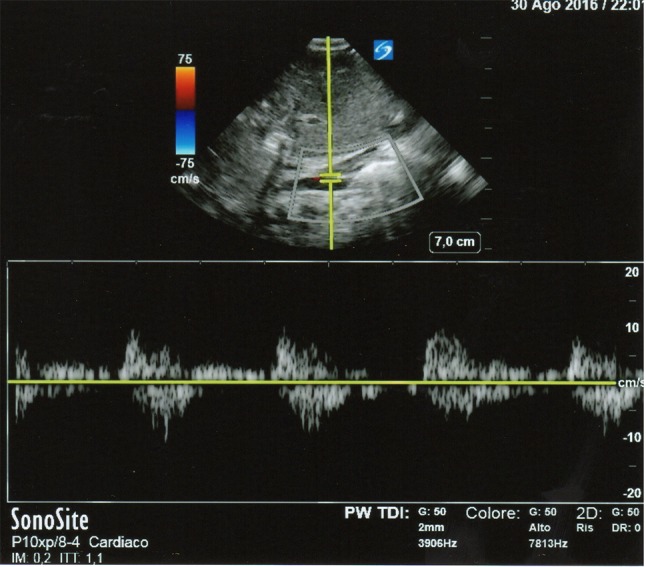
Pulsed-wave Tissue Doppler Imaging (TDI) of the abdominal aortic wall, showing phasic vessel pulsatility (same patient as Fig. 1)
We propose to take advantage of such a TDI pattern as a surrogate of a normal pulsatile Doppler flow trace in abdominal aorta when the latter is difficult to obtain due to malalignment with the insonated vessel. Such evaluation of abdominal aortic wall pulsatility might represent an useful tool to neonatologists in discriminating the presence and severity of an AoC in the NICU setting, in conjunction with the above-mentioned aortic arch analysis and other recently proposed ultrasonographic measures (distal transverse arch-to-ascending aorta ratio, isthmus-to-ascending aorta ratio, and carotid–subclavian artery index) [3]. Of course, physical examination still remains essential (and must precede any diagnostics such as echo) in posing the suspect of AoC. Physical signs suggestive of neonatal AoC include: continuous or late systolic murmur (better audible posteriorly over the thoracic spine) with associated systolic ejection click (if bicuspid aorta coexists); asymmetrical upper and lower pulses (with diminished and delayed pulses distal to obstruction); upper right limb hypertension [4].
More extensive studies enrolling large populations of healthy term newborns are needed to accurately define the TDI pattern of a normally pulsatile abdominal aortic wall in correlation with a normal Doppler flow pattern, in order to validate the use of the former alone when the latter is difficult to obtain.
Conclusions and final remarks
When a normal pulsatile Doppler flow trace in abdominal aorta is difficult to obtain due to malalignment with the insonated vessel, TDI might prove as an adequate surrogate to reveal a preserved aortic pulsatility by sampling the aortic wall motion induced by normal flow. This tool may be especially useful for the neonatologist in discriminating the presence and severity of an AoC in the NICU setting. More extensive studies enrolling large populations of healthy term newborns are needed to accurately define the TDI pattern of a normally pulsatile abdominal aortic wall, in order to validate the use of TDI alone when classic Doppler flow imaging is difficult to obtain.
Acknowledgements
We are especially grateful to Dr. Marco Mojoli (Cardiology Unit, Department of Cardiac, Thoracic and Vascular Sciences, University of Padua Medical School, Padova, Italy) and to Dr. Claudio Bonanno (Pediatric Cardiology and Adult Congenital Unit, Department of Experimental Diagnostic and Specialty Medicine, S. Orsola-Malpighi Hospital, University of Bologna, Bologna, Italy) for their precious assistance in the critical review of the manuscript.
Abbreviations
- NICU
Neonatal Intensive Care Unit
- AoC
Aortic coarctation
- PRF
Pulse repetition frequency
- TDI
Tissue Doppler Imaging
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Human and animal rights
This article does not contain any studies with animals performed by any of the authors.
Informed consent
Verbal informed consent was obtained from parents of the patient included in the study. Doppler scans have been submitted removing patient’s personal data.
References
- 1.Mertens L, Seri I, Marek J, Arlettaz R, Barker P, McNamara P, Moon-Grady AJ, Coon PD, Noori S, Simpson J, Lai WW. Writing Group of the American Society of Echocardiography (ASE); European Association of Echocardiography (EAE); Association for European Pediatric Cardiologists (AEPC). Targeted neonatal echocardiography in the neonatal intensive care unit: practice guidelines and recommendations for training. Eur J Echocardiogr. 2011;12:715–736. doi: 10.1093/ejechocard/jer181. [DOI] [PubMed] [Google Scholar]
- 2.Gentile R, Stevenson G, Dooley T, Franklin D, Kawabori I, Pearlman A. Pulsed Doppler echocardiographic determination of time of ductal closure in normal newborn infants. J Pediatr. 1981;98:443–448. doi: 10.1016/S0022-3476(81)80719-6. [DOI] [PubMed] [Google Scholar]
- 3.Al Akhfash AA, Almesned AA, Al Harbi BF, Al Ghamdi A, Hasson M, Al Habshan FM. Two-dimensional echocardiographic predictors of coarctation of the aorta. Cardiol Young. 2015;25:87–94. doi: 10.1017/S1047951113001790. [DOI] [PubMed] [Google Scholar]
- 4.Gach P, Dabadie A, Sorensen C, Quarello E, Bonello B, Pico H, Hugues N, Petit P, Gorincour G. Multimodality imaging of aortic coarctation: from the fetus to the adolescent. Diagn Interv Imaging. 2016;97:581–590. doi: 10.1016/j.diii.2016.03.006. [DOI] [PubMed] [Google Scholar]


