Abstract
Objective: To understand potential utilization of clinical services at a rural integrated health care system by generating optimal groups of telemedicine locations from electronic health record (EHR) data using geographic information systems (GISs).
Methods: This retrospective study extracted nonidentifiable grouped data of patients over a 2-year period from the EHR, including geomasked locations. Spatially optimal groupings were created using available telemedicine sites by calculating patients’ average travel distance (ATD) to the closest clinic site.
Results: A total of 4027 visits by 2049 unique patients were analyzed. The best travel distances for site groupings of 3, 4, 5, or 6 site locations were ranked based on increasing ATD. Each one-site increase in the number of available telemedicine sites decreased minimum ATD by about 8%. For a given group size, the best groupings were very similar in minimum travel distance. There were significant differences in predicted patient load imbalance between otherwise similar groupings. A majority of the best site groupings used the same small number of sites, and urban sites were heavily used.
Discussion: With EHR geospatial data at an individual patient level, we can model potential telemedicine sites for specialty access in a rural geographic area. Relatively few sites could serve most of the population. Direct access to patient GIS data from an EHR provides direct knowledge of the client base compared to methods that allocate aggregated data.
Conclusion: Geospatial data and methods can assist health care location planning, generating data about load, load balance, and spatial accessibility.
Keywords: electronic health records, telemedicine, geographic information systems, service planning
BACKGROUND AND SIGNIFICANCE
There has been acceleration in health care systems’ adoption of electronic health records (EHRs) since passage of the Health Information Technology for Economic and Clinical Health Act in 2009.1 In the last decade there has been increased interest in secondary utilization of patient data for research, analysis, quality and safety measurement, public health, and other business applications. This enables a health care system to enhance individuals’ health care experiences, increase knowledge about diseases and treatments, strengthen understanding of the system’s effectiveness and efficiency, and support public health goals.2 Geographic information system (GIS) technology integrates hardware, software, and data for capturing, managing, analyzing, and displaying forms of geographically referenced information.3 Geographic, visual, and spatial analytic techniques have been used to study health service availability and health care utilization patterns.4 Public health applications use GIS to map residential locations of patients in identifying origin and spread of infectious disease, which is critical in controlling outbreaks. GIS can be used to identify health trends, including conducting surveillance on cancer and chronic conditions such as diabetes5 and cardiovascular disease6 as well as planning for service deployment,7,8 and to demonstrate inequities in exposure to potential health risks.9
Research involving GIS data from EHRs has been limited, partly because of concerns around the availability of granular patient-level visit data due to confidentiality10 and the ongoing challenge of transposing patient data into GISs, which is the primary step before analysis. Although EHR adoption has rapidly increased, not all systems have a mature deployment with the ability to analyze EHR data repositories.11
About 16% of children in the United States live in rural areas,12 and they are more likely than children in urban areas to have adverse socioeconomic situations and poor health outcomes.13,14 Children with mental health, developmental, and behavioral problems are particularly vulnerable, and make up about 26% of children nationwide, or almost 6 million children.15 Lack of access to specialty care is particularly acute for isolated communities already facing physician shortages.16,17 Developmental-behavioral pediatrics (DBP) is a subspecialty of pediatrics that covers evaluation and management of child and adolescent developmental and behavioral problems, and involves significant geographic and time-access barriers for those patients and families.18,19 While clinician outreach has been found to improve access20 and is considered more family centered, it shifts the travel burden to the clinician, and the “windshield” time is often considered unproductive by health systems. Telemedicine allows patients access to distant clinicians, providing a means to retain care in the rural communities where people live and work, and helping to alleviate travel obstacles faced by patients,21 especially when accessing specialists.22 The field of DBP is well suited to telemedicine due to the paucity of clinicians in rural and other underserved areas and the nature of the interaction, which involves much interviewing and observation. Implementation of telemedicine in DBP may allow providers to become more efficient in their care by reducing the time spent driving to outlying clinic sites.23
Geomapping in pediatric populations has been used, for example, for pediatric burns and immunization.24 Previous studies involving DBP and GIS involved analysis of past utilization25; however, while GIS has been used to identify prospective telemedicine sites for other specialties,26 there has not been prospective determination/service planning in DBP using GIS patient data.
In this work, we demonstrate a method to extract patient-level GIS data from an EHR, paying attention to preserving privacy, in order to model optimal locations for telemedicine specialty pediatric service in a rural area.
OBJECTIVE
The objective of this study was first to describe current utilization of DBP services at a single rural integrated health care system, and subsequently to generate and analyze optimal groups of telemedicine locations through an analysis of EHR data using GIS.
MATERIALS AND METHODS
This retrospective study was approved by the Geisinger Institutional Review Board (IRB). The data source was EpicCare (Epic Systems, Verona, WI, USA), which contains detailed demographic, lifestyle, claims, procedural, laboratory, radiographic, vital, and other clinical data on all patients receiving care at outpatient and inpatient facilities in the Geisinger Health System. For this study, all patients receiving care at the neurodevelopmental pediatric service between January 1, 2011, and December 31, 2012, were eligible for cohort inclusion. Patient demographics (age, gender), primary insurance, primary diagnosis for visit, home address, and clinic location where the encounter took place were extracted. Patient street addresses were batch validated against a current US Postal Service database using BCC Mail Manager LE software (BCC Software, Rochester, NY, USA). Mail manager standardizes and corrects address components, adds ZIP+4, and returns a “911-style” address for some RR-style and post office box addresses. Addresses were geocoded using ArcGIS for Desktop 10.1 (ESRI, Redlands, CA, USA) as previously described.27 Match accuracy was controlled by setting spelling sensitivity high (ie, 90) and only accepting match scores above 80, to eliminate false positive matches. Spatial accuracy was documented by assigning a geocoding method score to each point. Using Method 1, 88.53% of addresses were located using standard interpolation along an address-ranged road line, then offset 20 feet depending on address parity. Using Method 2, 4.05% of patients were located to their ZIP+4 centroid. Using Method 3, 7.42% of patients were located to their 5-digit zip code centroid.
A total of 4027 visits by 2049 unique patients were observed. There were also 304 unique diagnosis codes listed as the primary conditions on the visits. Out of the 4027 visits, 828 were for new patients and 3199 for established patients. Number of visits ranged from 1 to 12; 51.4% had a single visit, 25.0% had 2, 11.5% had 3, and 5.8% had 4 visits. The data are summarized using frequency and percentage for categorical variables, and mean and standard deviation for continuous variables. Data from all visits as well as the first visit within the study observation period are summarized (Table 1).
Table 1.
Descriptive statistics
| Patients | Visits | |
|---|---|---|
| (N = 2049) | (N = 4027) | |
| Age (years) | 6.3 (4.2) | 7.4 (4.4) |
| Gender | ||
| Male | 1485 (72.5) | 3015 (74.9) |
| Female | 564 (27.5) | 1012 (25.1) |
| Site visited | ||
| Danville | 1765 (86.1) | 3342 (83.0) |
| Forty Fort | 125 (6.1) | 373 (9.3) |
| Grays Woods | 65 (3.2) | 127 (3.1) |
| Pottsville | 64 (3.1) | 134 (3.3) |
| Towanda | 30 (1.5) | 51 (1.3) |
| Diagnoses | ||
| ADHD/disruptive behavior disorders | 248 (12.1) | 594 (14.8) |
| Affective/mood disorders | 24 (1.2) | 31 (0.8) |
| Autism spectrum disorders | 519 (25.3) | 1323 (32.8) |
| CNS disorders | 238 (11.6) | 339 (8.4) |
| Chronic medical conditions | 13 (0.6) | 21 (0.5) |
| Genetic conditions | 152 (7.4) | 312 (7.8) |
| Intellectual disability/developmental delay | 301 (14.7) | 521 (12.9) |
| Language disorders | 263 (12.8) | 417 (10.4) |
| Learning disorders | 48 (2.3) | 77 (1.9) |
| Prematurity | 212 (10.4) | 340 (8.4) |
| Other | 31 (1.5) | 52 (1.3) |
| Insurance | ||
| Commercial | 1037 | |
| Medicaid | 927 | |
| Behavioral | 2 | |
| Military | 19 | |
| Other | 37 | |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; CNS, central nervous system
Geomasking28 was used to protect patients’ privacy by concealing their geocoded location. All geocoded address points were displaced a distance of 0–0.5 miles in a random direction 0–360° before latitude and longitude coordinates were calculated and submitted for analysis.
Spatial groupings of 3, 4, 5, and 6 telemedicine sites were created from the 18 possible sites. For each grouping, patients were allocated to the nearest site. Relative value of each grouping was determined by calculating the ATD for all patients to the closest site for each. A more realistic cost-of-distance was simulated by scaling distance by a standard 0.5 distance-decay exponent, with short trips being relatively more expensive per mile.29 Counts of patients for each site were used to evaluate patient load imbalances.
RESULTS
The optimality of the various groupings was evaluated using ATDs.
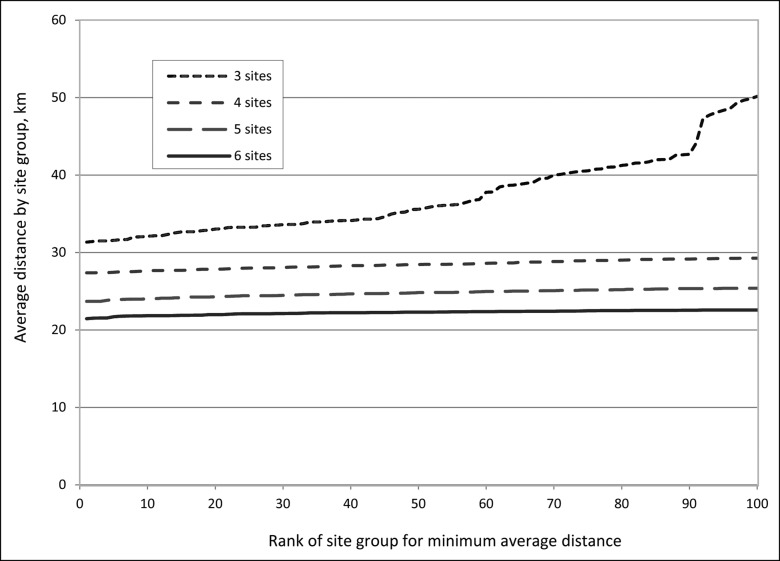
Figure 1 illustrates the best travel distances for groupings of 3, 4, 5, or 6 site locations. Site groupings are ranked on the y-axis by increasing ATD. Each one-site increase in the number of available telemedicine sites decreased minimum ATD by about 8%. For a given group size, the best groupings are very similar in minimum travel distance: for the best 30 groupings made from 4 sites, the ATD differed between sequentially ranked groups by only 21 m.
Figure 1.
Best average patient travel distances for groupings of 3, 4, 5, or 6 site locations. Site groupings are ranked on the y-axis by increasing ATD.
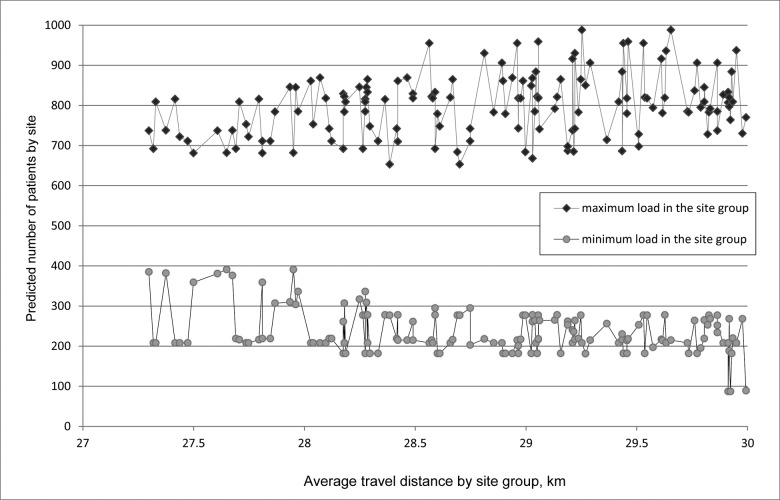
The patient balance by site for best groupings of 4 sites is compared in Figure 2. The most and least busy sites in each grouping are compared, plotted against ATD for the grouping. There are significant differences in patient traffic imbalance between otherwise similar groupings.
Figure 2.
Highest and lowest traffic for the extreme sites of each grouping, plotted against average patient travel distance for the groupings.
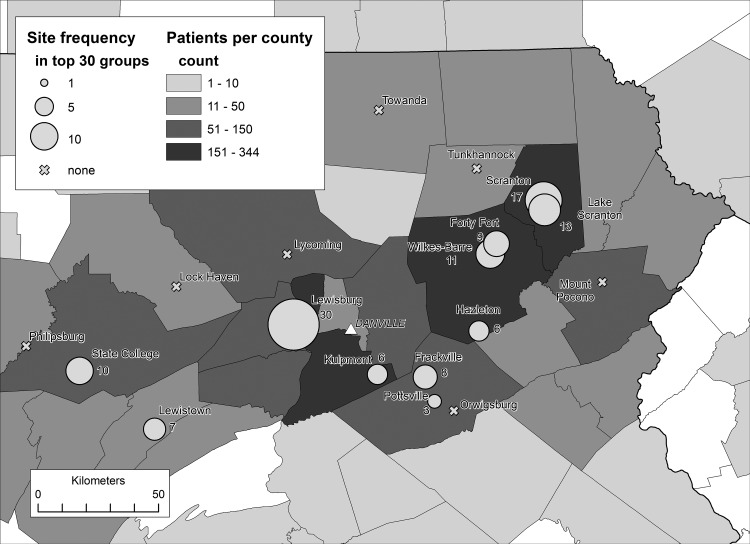
The values of individual sites within this telemedicine model are represented in Figure 3, which maps the frequency of occurrence of the potential sites in the top 30 groupings ranked by lowest ATD for groupings of 4 sites. The principal location was forced into each grouping. This shows that the highly concentrated geography of the patient distribution created an uneven pattern of site usage.
Figure 3.
Frequency of occurrence of each potential site in the top 30 groupings ranked by lowest average patient travel distance, for groupings of 4 sites. The principal location was forced into each grouping. Patient locations aggregated to county level.
A majority of the best site groupings used most of the same small number of sites, and urban sites were heavily used. Eleven sites appear in the top 30 site groupings, while 7 sites in small towns at the periphery of the region were not used in any of the best groupings.
DISCUSSION
Using EHR data at an individual patient level with a focus on geospatial data, we demonstrate the ability to model potential telemedicine sites for neurodevelopmental pediatrics access for patients in a rural geographic area. We identify that a few sites could serve most of the population using GIS mapping by minimal travel distance measurement. We show that selection of site groupings is vulnerable to imbalances between the busiest and least busy sites in otherwise similar groupings. This endeavor was undertaken to reduce spatial access barriers to a specialty pediatric service for a predominantly rural population that is relatively stable, with an out-migration rate under 4% every 4 years. Our study was possible due to a relatively mature (>14-year) experience with EHR data-collection procedures using a comprehensive enterprise-level data warehouse, with source data transformed through a standard “extract-transform-load” process.30
Spatial data is increasingly being viewed as an efficient resource in health care analysis, and GIS is particularly valuable when assessing community health needs due to its ability to integrate data from various sources and visualize through mapping.31 The use of distance decay32 is in keeping with other methods particularly relevant for sparsely populated rural areas such as in our study. The advantage of having access to patient GIS data from an EHR is that it gives us direct knowledge of the client base and allows for allocation to a finite set of sites, compared to census-based methods, which are allocated by aggregated data groups represented through a single location (a centroid, usually geometric or population-weighted).33 However, this approach requires data that are complete in terms of patient addresses and access to skilled GIS personnel to extract and geocode the data for analysis. We were fortunate to have one co-author (JD) experienced in GIS to address confidentiality issues with EHR data. Another concern is that match rate and accuracy can be affected by the dataset used for geocoding, which is updated frequently.34 By validating the input address file and geocoding with multiple address base maps from different sources and years, we were able to achieve a high match rate with minimal manual editing of the input address file. Furthermore, by flagging the resulting geocoded points with a geocoding method rank, we maintained some transparency regarding the spatial accuracy of geocoded locations.
There are legitimate concerns about confidentiality when dealing with EHR data, and although zip code alone is not considered protected health information, the Health Insurance Portability and Accountability Act35 provides guidelines on how to preserve confidentiality by employing minimum spatial denominator units on a map. Generally there is a trade-off between loss of usable information and disclosure risk to research subjects/patients, depending on the measures used to preserve confidentiality. The use of GIS methods with patient data raises issues related to protecting patient confidentiality, and no single method is considered ideal to reduce the risk of confidentiality breaches.36 For our study, we pursued IRB procedures and used a limited dataset with delinked identifiers to be sensitive to these concerns, and we used random perturbation and aggregation of data, which are recommended in a seminal National Academies Press publication on the matter.37 Other recommendations include conducting research into methods of disseminating useful data while protecting confidentiality; engaging professional societies, clinicians, researchers, and institutions in education around ethical issues; and creating “data enclaves” for dissemination and access to high-quality data that preserve confidentiality.37 We mainly demonstrated aggregated data, and maps were not presented at a granular enough level that would engender reverse coding and identification of patients.
One limitation is that this study involves only one service analysis of one health care system in one state; however, we believe that this method can be replicated by any system for one or more clinical services for predictive planning using EHR data. Additionally, this model uses retrospective data and may not actually predict specific access patterns or utilization. This is because planning for services based on spatial accessibility assumes that patients in an identified geographic region have equal access to clinicians, ignoring supply-demand variations and “distance decay”32 of utilization behavior, and that people may go beyond their region to seek care. It further presumes that providing service at new locations will not, in itself, shift demand. There are factors that need to be understood, such as availability of other services and the perceived institutional reputation of the specialty offered, that play into patient behavior related to access. DBP in particular has a limited supply of providers in our service area, so while telehealth has the potential to address certain access barriers for rural patients, access to the same limited number of providers may not alter the wait times. Furthermore, children with Medicaid coverage often have greater access barriers,38 but our dataset was limited and we were unable to elaborate on this.
The use of GIS has increased researchers’ appreciation of the intersection of space and place with health as health care systems attempt to further engage patients and make decisions to deliver care with an eye on spatial equity.39 Socioeconomic status (SES) impacts access to transportation and mobility, and no discussion of spatial equity is complete without acknowledging these variables. Affordability, acceptability, and accommodation are 3 nonspatial factors that determine access,40 and SES is a key variable, as it has implications for health insurance status and transportation access, among other factors.41 In our study, we did not include SES variables, and future directions will look at stratifying by income (although EHRs are generally not robust datasets for this information) and establishing “equity sorting” when determining numbers and locations of sites. Community data (such as census and Community Health Assessment) serve to complement EHR data in this endeavor to identify communities in need.42 Further, while we did use GIS mapping, we did not factor in elements such as traffic patterns, road quality, and temporary obstructions along the road.
Geographic information system technology can enable health care systems to plan for communities in need of specific health services through analysis of patient demographic data instead of assuming (or ignoring) the geographic and utilization characteristics of populations in the process of planning clinical services.8 This strategy complements the health care business planning process of estimating market volume and market share. Selecting potential clinical sites also includes such variables as the community location’s perceived need, willingness to cooperate, or other subjective considerations.26
In the near future, there will be a wave of data available from wearable technology (smart devices and sensors) and patient-reported personal data that will need to be addressed, and coordinating with community-level data helps to emphasize patient outcomes–oriented research.43 “Big data” approaches will need to be developed that are meaningful to clinicians while proactively addressing concerns regarding privacy, and secondary data use like this will help to create the learning health care system.44
CONCLUSION
Secondary data extracted and analyzed from the mature EHR of an integrated health care system can yield patient spatial data, which, using GIS methods, can assist health care location planning. A limited number of sites can be modeled to deliver relatively equal spatial access to a population for a particular service. Geomasking and other strategies are necessary when working with protected health information to assuage any concerns regarding privacy and confidentiality. Additional factors such as provider availability, spatial equity, and perceived need are to be considered when making decisions about optimal locations.
Future directions include seeking methods to model economic access for this population and reassessing access and utilization with the deployed telemedicine locations over a further 2-year period. As health systems move toward population health, it will be important to use efficient analyses of secondary spatial data with the help of GIS-skilled personnel, and to engage with clinicians and operational leaders in identifying patient-centered decisions around health care location planning. Patient-reported personal data and community-level data will further enhance this capability.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sector.
Competing interests
The authors have no competing interests to declare.
Contributors
All authors attest that they have made substantial contributions to the conceptualization and design of this paper, as below. Additionally, all authors participated in drafting and revising the manuscript and approve the final version submitted for publication.
NS conceived the concept, sought IRB approval, conducted the study, crafted the first draft of the manuscript, participated in revisions, and served as corresponding author.
JD conducted the GIS analysis of the project, contributed to the Methods, Results, and Discussion sections of the manuscript, and participated in revisions.
BM conducted the geomapping analysis of the project, contributed to the Methods, Results, and Discussion, and participated in revisions.
References
- 1. Health Information Technology for Economic and Clinical Health (HITECH) Act, Title XIII of Division A and Title IV of Division B of the American Recovery and Reinvestment Act of 2009 (ARRA), Pub. L. No. 111-5, 123 Stat. 226 (February 17, 2009). [Google Scholar]
- 2. Safran C, Bloomrosen M, Hammond WE et al. Toward a national framework for the secondary use of health data: an American Medical Informatics Association white paper. J Am Med Inform Assoc. 2007;141:1–9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Environmental Systems Research Institute What is GIS? http://www.esri.com/what-is-gis/. Accessed January 7, 2015. [Google Scholar]
- 4. McLafferty SL. GIS and Health Care Annu Rev Public Health. 2003; 24:25–42 [DOI] [PubMed] [Google Scholar]
- 5. Laranjo L, Rodrigues D, Pereira AM et al. Use of electronic health records and geographic information systems in public health surveillance of type 2 diabetes: a feasibility study. JMIR Public Health Surveill. 2016;21:e12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Clark RA, Driscoll A, Nottage J et al. Inequitable provision of optimal services for patients with chronic heart failure: a national geo-mapping study. Med J Aust. 2007;1864:169. [DOI] [PubMed] [Google Scholar]
- 7. Culpepper W, Cowper-Ripley D, Litt E et al. Using geographic information system tools to improve access to MS specialty care in Veterans Health Administration. J Rehabil ResDeve. 2010;47:583–92. [DOI] [PubMed] [Google Scholar]
- 8. Bazemore A, Phillips RL, Miyoshi T. Harnessing geographic information systems (GIS) to enable community-oriented primary care. J Am Board Fam Med. 2010;23:22–31. [DOI] [PubMed] [Google Scholar]
- 9. Maantay J. Mapping environmental injustices: pitfalls and potential of geographic information systems in assessing environmental health and equity. Environ Health Perspect. 2002;110(Suppl 2):161–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. VanWey LK, Rindfuss RR, Gutmann MP et al. Confidentiality and spatially explicit data: concerns and challenges. PNAS. 2005;10243:15337–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Charles D, Gabriel M, Searcy T. Adoption of electronic health record systems among U.S. Non-Federal Acute Care Hospitals: 2008–2014. ONC Data Brief, No. 23 Office of the National Coordinator for Health Information Technology: Washington, DC; 2015. [Google Scholar]
- 12. U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau. Child Health USA. Rockville, Maryland: U.S. Department of Health and Human Services; 2014. [Google Scholar]
- 13. U.S. Department of Health and Human Services, Health Resources and Services Administration, Maternal and Child Health Bureau. The Health and Well-Being of Children in Rural Areas: A Portrait of the Nation, 2011–2012. Rockville, Maryland: U.S. Department of Health and Human Services; 2015. [Google Scholar]
- 14. Skinner AC, Slifkin RT. Rural/urban differences in barriers to and burden of care for children with special health care needs. J Rural Health. 2007;232:1505.–. [DOI] [PubMed] [Google Scholar]
- 15. The Annie E. Casey Foundation, Kids Count Data Center. http://datacenter.kidscount.org. Accessed October 6, 2016. [Google Scholar]
- 16. Association of Medical Colleges (AAMC). Help Wanted: More Use Doctors – Projections Indicate America Will Face Shortage of M.D.s by 2020 [Brochure]. AAMC: Washington DC; 2006. [Google Scholar]
- 17. Gamm LD, Hutchison LL, Dabney BJ, Dorsey AMeds. Rural Healthy People 2010: A Companion Document to Healthy People 2010. College Station, TX: Texas A&M Health Science Center, School of Public Health, Southwest Rural Health Research Center; 2003. [Google Scholar]
- 18. Mayer ML. Are We There Yet? Distance to Care and Relative Supply Among Pediatric Medical Subspecialties .Pediatrics. 2006;1186:2313–21. [DOI] [PubMed] [Google Scholar]
- 19. National Association of Children’s Hospitals Pediatric Specialist Physician Shortages Affect Access to Care. https://www.childrenshospitals.org/issues-and-advocacy/graduate-medical-education/fact-sheets/2012/pediatric-specialist-physician-shortages-affect-access-to-care. Accessed August 13, 2016. [Google Scholar]
- 20. Gruen RL, Weeramanthri TS, Knight SS et al. Specialist outreach clinics in primary care and rural hospital settings. Cochrane Database Syst Rev. 2004;1:CD003798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. LeVert D. Telemedicine: revamping quality healthcare in rural America. Ann Health Law. 2010;19:215–26. [Google Scholar]
- 22. Marcin JP, Ellis J, Mawis R et al. Using telemedicine to provide pediatric subspecialty care to children with special health care needs in an underserved rural community. Pediatrics. 2004;113:1. [DOI] [PubMed] [Google Scholar]
- 23. Soares NS, Langkamp DL. Telehealth in developmental-behavioral pediatrics. J Develop Behav Pediatr. 2012;338:656–65. [DOI] [PubMed] [Google Scholar]
- 24. Jacobs BR. Geospatial Mapping & Analysis of Health Care Conditions in Children. 2012. https://www.himss.org/files/HIMSSorg/content/HIMSS12PhysPosters/BrianJacobs.pdf. Accessed September 15, 2016. [Google Scholar]
- 25. Soares NS, Johnson AO, Patidar N. Geomapping telehealth access to developmental-behavioral pediatrics. Telemed J E Health. 2013;198: 585–90. [DOI] [PubMed] [Google Scholar]
- 26. Shannon GW, Buker CM. Determining accessibility to dermatologists and teledermatology locations in Kentucky: demonstration of an innovative geographic information systems approach. Telemed J E Health. 2010;166:670–77. [DOI] [PubMed] [Google Scholar]
- 27. Schwartz BS, Stewart WF, Godby S et al. Body mass index and the built and social environments in children and adolescents using electronic health records. Am J Prevent Med. 2011;41:e17–e28. [DOI] [PubMed] [Google Scholar]
- 28. Armstrong MP, Rushton G, Zimmerman DL. Geographically masking health data to preserve confidentiality. Statist Med. 1999;18:497–525. [DOI] [PubMed] [Google Scholar]
- 29. Taaffe EJ, Gauthier HL, O’Kelly ME. Geography of Transportation. Upper Saddle River, NJ: Prentice Hall; 1996. [Google Scholar]
- 30. Denney MJ, Long DM, Armistead MG et al. Validating the extract, transform, load process used to populate a large clinical research database. Int J Med Inform. 2016;94:271–74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Boulos MNK. Towards evidence-based, GIS-driven national spatial health information infrastructure and surveillance services in the United Kingdom. Int J Health Geographics. 2004;3:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Shannon GW, Bashshur RL, Metzner CA. The concept of distance as a factor in accessibility and utilization of healthcare. Medical Care Review. 1969;26:143–61. [Google Scholar]
- 33. McGrail MR. Spatial accessibility of primary health care utilising the two step floating catchment area method: an assessment of recent improvements. Int J Health Geographics. 2012;11:50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Zandbergen PA. Influence of street reference data on geocoding quality. Geocarto Int. 2011;261:35–47. [Google Scholar]
- 35. The Health Insurance Portability and Accountability Act (HIPAA). Washington, D.C: U.S. Dept. of Labor, Employee Benefits Security Administration; 2004. [Google Scholar]
- 36. Zandbergen PA. Ensuring confidentiality of geocoded health data: assessing geographic masking strategies for individual-level data. Adv Med. 2014;2014:1–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Gutmann M, Stern P. Putting People on the Map: Protecting Confidentiality with Linked Social-Spatial Data. Washington, DC: National Academies Press; 2007. [Google Scholar]
- 38. DeVoe JE, Baez H, Angier H et al. Insurance plus access does not equal health care: typology of barriers to health care access for low-income families. Ann Fam Med. 2007;56:511–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Braveman P, Gruskin S. Defining equity in health. J Epidemiol Commun Health. 2003;57:254–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Levesque J-F, Harris MF, Russell G. Patient-centred access to health care: conceptualising access at the interface of health systems and populations. Int J Equity Health. 2013;12:18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wang F, Luo W. Assessing spatial and nonspatial factors for healthcare access: towards an integrated approach to defining health professional shortage areas. Health Place. 2005;112:131–46. [DOI] [PubMed] [Google Scholar]
- 42. Kaufman T, Geraghty EM, Dullet N et al. Geospatial information system analysis of healthcare need and telemedicine delivery in California. Telemed e-Health. November 2016. [Epub ahead of print, doi:10.1089/tmj.2016.0144]. [DOI] [PubMed] [Google Scholar]
- 43. Roth C, Foraker RE, Payne PRO, Embi PJ. Community-level determinants of obesity: harnessing the power of electronic health records for retrospective data analysis. BMC Med Inform Decis Making. 2014;14:36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Friedman CP, Wong AK, Blumenthal D. Achieving a nationwide learning health system. Sci Transl Med. 2010;257:1–3. [DOI] [PubMed] [Google Scholar]