Abstract
Background
Teachers and school staff should be competent in managing asthma in schools. Demonstrated low levels of asthma knowledge mean that staff may not know how best to protect a child with asthma in their care, or may fail to take appropriate action in the event of a serious attack. Education about asthma could help to improve this knowledge and lead to better asthma outcomes for children.
Objectives
To assess the effectiveness and safety of asthma education programmes for school staff, and to identify content and attributes underpinning them.
Search methods
We conducted the most recent searches on 29 November 2016.
Selection criteria
We included randomised controlled trials comparing an intervention to educate school staff about asthma versus a control group. We included studies reported as full text, those published as abstract only and unpublished data.
Data collection and analysis
At least two review authors screened the searches, extracted outcome data and intervention characteristics from included studies and assessed risk of bias. Primary outcomes for the quantitative synthesis were emergency department (ED) or hospital visits, mortality and asthma control; we graded the main results and presented evidence in a 'Summary of findings' table. We planned a qualitative synthesis of intervention characteristics, but study authors were unable to provide the necessary information.
We analysed dichotomous data as odds ratios, and continuous data as mean differences or standardised mean differences, all with a random‐effects model. We assessed clinical, methodological and statistical heterogeneity when performing meta‐analyses, and we narratively described skewed data.
Main results
Five cluster‐RCTs of 111 schools met the review eligibility criteria. Investigators measured outcomes in participating staff and often in children or parents, most often at between 1 and 12 months.
All interventions were educational programmes but duration, content and delivery varied; some involved elements of training for pupils or primary care providers. We noted risk of selection, performance, detection and attrition biases, although to a differing extent across studies and outcomes.
Quanitative and qualitative analyses were limited. Only one study reported visits to the ED or hospital and provided data that were too skewed for analysis. No studies reported any deaths or adverse events. Studies did not report asthma control consistently, but results showed no difference between groups on the paediatric asthma quality of life questionnaire (mean difference (MD) 0.14, 95% confidence interval (CI) ‐0.03 to 0.31; 1005 participants; we downgraded the quality of evidence to low for risk of bias and indirectness). Data for symptom days, night‐time awakenings, restricted activities of daily living and school absences were skewed or could not be analysed; some mean scores were better in the trained group, but most differences between groups were small and did not persist to 24 months.
Schools that received asthma education were more adherent to asthma policies, and staff were better prepared; more schools that had received staff asthma training had written asthma policies compared with control schools, more intervention schools showed improvement in measures taken to prevent or manage exercise‐induced asthma attacks and more staff at intervention schools reported that they felt able to administer salbutamol via a spacer. However, the quality of the evidence was low; results show imbalances at baseline, and confidence in the evidence was limited by risk of bias and imprecision. Staff knowledge was higher in groups that had received asthma education, although results were inconsistent and difficult to interpret owing to differences between scales (low quality).
Available information about the interventions was insufficient for review authors to conduct a meaningful qualitative synthesis of the content that led to a successful intervention, or of the resources required to replicate results accurately.
Authors' conclusions
Asthma education for school staff increases asthma knowledge and preparedness, but studies vary and all available evidence is of low quality. Studies have not yet captured whether this improvement in knowledge has led to appreciable benefits over the short term or the longer term for the safety and health of children with asthma in school. Randomised evidence does not contribute to our knowledge of content or attributes of interventions that lead to the best outcomes, or of resources required for successful implementation.
Complete reporting of the content and resources of educational interventions is essential for assessment of their effectiveness and feasibility for implementation. This applies to both randomised and non‐randomised studies, although the latter may be better placed to observe important clinical outcomes such as exacerbations and mortality in the longer term.
Plain language summary
Asthma education for school staff
Background to the question
Teachers and school staff need to know how to manage asthma in schools. If they have little knowledge of asthma, staff may not know how best to protect a child with asthma, or may fail to act in the event of a serious attack. We aimed to assess the benefits and possible harms of asthma education for school staff, and to explore how this education can best be delivered.
Study characteristics
We found five studies including more than 100 schools that compared an asthma education programme for school staff against a control. Researchers measured outcomes for teachers and staff, and often for children or parents as well, most often at between 1 and 12 months. We conducted the most recent search for studies on 29 November 2016.
Main results
We could not tell whether educating school staff reduced the number of children who needed to visit the emergency department (ED) or hospital, and no studies reported any deaths. Study authors measured asthma control in different ways but found little benefit, especially more than a year after the intervention was provided.
Schools that received asthma education stuck to asthma policies better and staff were better prepared; more schools that had received staff asthma training had written asthma policies compared with control schools, more intervention schools showed improvement in measures taken to prevent or manage exercise‐induced asthma attacks and more staff at intervention schools felt that they were able to administer salbutamol using a spacer.
We wanted to assess what the education sessions should cover and how they could best be delivered, but we did not find enough information to do this.
To sum up, asthma education for school staff increases asthma knowledge and preparedness in the schools, but we do not know much about actual benefits of this education for children with asthma.
Quality of the evidence
The small number of studies and the variation between them mean that we cannot be sure of the overall effect of educating school staff about asthma. The ways researchers allocated schools, teachers or children to groups may have caused some bias. Also, the fact that teachers knew whether they were in the active or control group may have affected how they behaved and answered questionnaires, and this may have led to overestimation of benefits. Lots of people who were included in the studies did not return questionnaires at the end of the study, which means that we do not have a full picture of the results of asthma education interventions.
Summary of findings
for the main comparison.
| Asthma education for school staff compared with control | |||||
|
Patient or population: school staff Settings: schools of any type Intervention: education about asthma Comparison: no education | |||||
| Outcomes | Illustrative comparative risks* (95% CI) | Number of participants (studies) | Quality of the evidence (GRADE) | Comments | |
| Assumed risk | Corresponding risk | ||||
| Control group | Staff asthma education | ||||
|
Visits to ED/hospital Over previous 12 months, measured at 1 and 2 yearsa |
One study reported mean numbers of hospital visits, ED visits and urgent care visits per child in education and control groups at 1 year and 2 years Data were skewed and were not pooled |
472 (1 RCT) Bruzzese 2006 |
Not graded | ||
| Mortality | No studies reported the outcome. None mentioned any deaths during the study period | 0 RCTs | Not graded | ||
|
Asthma control Quality of life (PAQLQ) 0 to 7 scale; higher is better 6 months to 1 year |
Mean score in the control group was 5.15 | Mean score in the intervention groups was 0.14 better (0.03 worse to 0.31 better) | 1005 (2 RCTs) |
⊕⊕⊝⊝ LOWb,c,d,e | MCID of the scale is 0.5 ‐ difference not statistically or clinically significant |
|
Asthma control Narrative 1 year and 2 years |
Mean night‐time awakenings, symptom days and disruption to ADLs were a bit lower in the intervention group at 1 year, but the data are skewed and difficult to interpret. No apparent difference after 2 years | 472 (1 RCT) Bruzzese 2006 |
Not graded | Skewed data, not analysed | |
|
Adherence to asthma policies 6 months to 1 year |
6/28 control schools had an asthma policy at the end of the study | 16/29 schools that received education had an asthma policy | 57 schools (2 RCTs) | ⊕⊕⊝⊝f,g LOW |
All results better in the education group, but some imbalances at baseline |
| 4/12 control schools improved measures to prevent attacks | 14/17 schools that received education improved measures to prevent attacks | 29 schools (1 RCT) |
|||
| 3/16 control schools were able to administer salbutamol | 14/17 schools that received education were able to administer salbutamol | ||||
|
Absenteeism related to asthma Narrative |
Mean absences were a bit lower in the intervention group at 1 year, but the data are skewed and difficult to interpret. No apparent difference at 2 years | 472 (1 RCT) Bruzzese 2006 |
Not graded | Skewed data, not analysed | |
|
Staff preparedness ‐ asthma knowledge NAKQ 0 to 31 scale; higher is better. 1 to 8 months |
Mean NAKQ score in the control group was 16.33 | Mean score in the intervention groups was 0.74 standard deviations better (0.33 to 1.16 SDs better) | 640 (3 RCTs) | ⊕⊕⊝⊝b,h LOW | Two studies used the NAKQ; 1 used the AGKQ. Analysis conducted using SMD |
| *The basis for the assumed risk (e.g. median control group risk across studies) is provided in footnotes. The corresponding risk (and its 95% confidence interval) is based on the assumed risk in the comparison group and the relative effect of the intervention (and its 95% CI) AGKQ: Asthma General Knowledge Questionnaire; CI: confidence interval; ED: emergency department; MCID: minimal clinically important difference; NAKQ: Newcastle Asthma Knowledge Questionnaire; PAQLQ: Paediatric Asthma Quality of Life Questionnaire; RCT: randomised controlled trial; RR: risk ratio; SMD: standardised mean difference | |||||
| GRADE Working Group grades of evidence High quality: Further research is very unlikely to change our confidence in the estimate of effect Moderate quality: Further research is likely to have an important impact on our confidence in the estimate of effect and may change the estimate Low quality: Further research is very likely to have an important impact on our confidence in the estimate of effect and is likely to change the estimate Very low quality: We are very uncertain about the estimate | |||||
aReporting mean number of events per child can be a skewed way to report these data, which appears likely given the size of the SDs. Mean difference must be interpreted with caution
bDowngraded for risk of bias. Self‐reported measure that would be subject to performance and detection biases. Possible selection and attrition bias as well
cNot downgraded for inconsistency. One study used student report and one used a caregiver scale. Results are not statistically inconsistent but are difficult to interpret
dNot downgraded for imprecision. Confidence limits cross the line of no effect but lie within the MCID for the scale
eDowngraded for indirectness as quality of life is not a direct measure of asthma control, only really a proxy
fDowngraded for imprecision. Confidence intervals did not cross the line of no effect but were very wide, ranging from a modest to a very large effect
gDowngraded for risk of bias. Issues with performance and detection bias may not be directly relevant to this outcome, but problems with allocation concealment may have introduced selection bias
hDowngraded for inconsistency (I² = 71%)
Background
Description of the condition
Asthma, the most common childhood long‐term condition, has increased in prevalence over the past two decades. As many as 334 million people worldwide are affected by asthma, and in some countries, up to 20% of 13‐ to 14‐year‐olds have asthma symptoms (Global Asthma Report 2014). Great advances in diagnosis and treatment have been made, but considerable morbidity and mortality are reported worldwide, particularly in lower‐ and middle‐income countries (Global Asthma Report 2014). Since inhaled steroids were introduced, researchers have observed a significant drop in asthma mortality, but rates have failed to improve in recent years (Martinez 2008). Childhood asthma is a leading cause of school absence, impacting negatively individual educational opportunities and more widely economies through increased time off work for parents and guardians (Meng 2012). Children with asthma have higher rates of school absence and grade failure and are at greater risk of learning disability than children without health conditions (Fowler 1992).
Access to and compliance with inhaled medications and ownership of a personalised asthma action plan (PAAP) are important factors in the control of day‐to‐day symptoms and in prevention of life‐threatening attacks (BTS/SIGN 2014; GINA 2015). Children and adults who are socially isolated or who belong to minority groups have higher rates of mortality and morbidity associated with asthma (Global Asthma Report 2014). This may be related at least in part to reduced compliance and less commonplace use of PAAPs in these populations, although uptake of PAAPs in general is surprisingly low (Ring 2015) despite long‐term recommendations for their use (BTS/SIGN 2014; GINA 2015). Lack of knowledge, high costs, limited access to primary health care, myths about medication, worries about addiction or side effects and difficult dosing regimens all contribute to poor compliance (Cochrane 1999).
The National Review of Asthma Deaths (NRAD) in the UK recently reported that 80% of deaths among children younger than 10 years of age and around three‐quarters of deaths among 10‐ to 19‐year‐olds happened before patients reached the hospital (NRAD 2015). Furthermore, NRAD found potentially avoidable factors that contributed to 90% of deaths in children and young people. As a result, the report describes overall care of children with asthma as inadequate, and a key recommendation of the report is that "parents and children, and those that care for or teach them, should be educated about managing asthma".
Description of the intervention
Children spend a considerable proportion of their waking hours in school, and much work has been aimed at managing asthma in this environment (Cicutto 2014). Lack of knowledge in schools and among teaching staff has been recognised as a potential contributor to preventable morbidity and mortality (Murphy 2006). It is important to understand what can go wrong with management of asthma in schools, so that guidelines for educational interventions can be compiled for staff. No agreement has been reached on what constitutes a successful educational intervention for school staff (Coffman 2009), but problem areas to be addressed include poor access to asthma medications in schools, use of out‐of‐date inhalers, local regulations about medication administration and confusion about inhaler types and the ways in which they are used (Hillemeier 2006; Reznik 2015). Indeed, given the proliferation of inhaler devices and types of medications, it has become confusing even for those who work in health care to stay up‐to‐date with medications and how and when to use them (Baverstock 2010; Hanania 1994). School staff may hope to rely on the school nurse to be the expert; however, this does not remove the responsibility of school staff members to have sufficient knowledge to know how, why and when they should call for assistance or use medication (NRAD 2015).
Asthma charities and research organisations list various specific, deliverable interventions that may improve the safety of children and young people with asthma in school, ranging from simple checklists to ensure that each child has his or her own PAAP and in‐date inhalers to more complex online education packages (e.g. Asthma UK; NAEPP 2014). Educational interventions may take various forms, from teaching staff and teachers to recognise the symptoms of a distressed child to ensuring that they have confidence in managing a full‐blown asthma attack. School policies vary locally and internationally but can be basic, non‐specific to asthma, voluntary and difficult to enforce. For example, the UK government has issued regulations to help school governing bodies develop a policy that supports pupils with medical conditions, "so that they can play a full and active role in school life, remain healthy and achieve their academic potential" (Department for Health 2015). This document outlines advice on the responsibilities of governing bodies, head teachers, parents, pupils, school staff, school nurses and healthcare professionals but does not detail how policies or training for staff should be designed or implemented, and stresses that policy templates are voluntary. Asthma attacks are difficult and frightening to witness, and school staff should receive specific training so they can act quickly and appropriately (Wu 1998). Fear associated with asthma attacks and lack of self‐efficacy among untrained staff can serve as barriers to appropriate care for children in life‐threatening situations (Abdel Gawwad 2007).
How the intervention might work
Asthma education for school staff aims to increase the knowledge of those responsible for children and young people with asthma. Ultimately, the aims of any asthma education programme or policy within a school are to prevent children from dying as the result of a slow or incorrect response to an asthma attack, and to encourage and promote effective management of a child's symptoms to reduce the effects of asthma on quality of life and education. These outcomes may be difficult to capture in practice, and demonstration and description of benefits following educational interventions have long been problematic and enthusiastically sought (Bates 2004). Education on self‐management for people with asthma has been shown consistently to improve outcomes (BTS/SIGN 2014), but it is unclear how one can best measure the effects of an intervention that is focused on school staff. Short‐term outcomes regarding how the intervention has worked in terms of staff knowledge and preparedness may be most obvious and easiest to measure, but more important is the intended benefit for asthma‐related outcomes among children and adolescents with asthma, which may take longer to become apparent.
The school environment poses unique and manifest challenges, including co‐ordination and collaboration between adult and child, and between family and school, and these challenges can be made more difficult by differences in language and literacy (Williams 1998). Any asthma education intervention aimed at school staff should work by sharing key information specific to each child, so that the responsibility for recognising potentially dangerous symptoms at school lies not only with the child's teacher, but also with other staff in contact with the child, with parents and with the child himself (NAEPP 2014).
Why it is important to do this review
Children and young people still die at home and in school, and potentially avoidable factors contribute to their death in at least 9 out of 10 cases (NRAD 2015). Overall care of children with asthma has been described as inadequate, and involvement of school staff is recognised as paramount (NRAD 2015). Better care in schools has the potential to reduce childhood deaths from asthma, improve the quality of life of children with asthma, maximise a child's education and minimise time off school. Some schools have recently introduced policies to address dangerous barriers to protecting children with asthma, such as use of emergency rescue inhalers when a child with asthma cannot access her own inhaler (Department of Health 2014), but obstacles and difficulties persist (Reznik 2015). Factors specific to the school environment require particular attention to keep children with asthma safe in schools, such as frequent asthma attacks in the autumn term due to the concentration of aero‐allergens, and exercise‐induced attacks during sports activities (Asthma UK).
It is important to review systematically the evidence that has sought to address deficits identified in asthma education for school staff (NRAD 2015), and to assess the attributes of training packages, so they can be applied effectively (Norcini 2011). The extent to which we can answer 'how' training can be designed, 'why' it is effective and 'for whom and when' will depend on descriptive data within primary studies, but it is important to highlight this information to help professionals understand and deliver health education in a reliable and reproducible manner (Gordon 2011; Gordon 2013).
Objectives
To assess the effectiveness and safety of asthma education programmes for school staff, and to identify content and attributes underpinning them.
Methods
Criteria for considering studies for this review
Types of studies
We included parallel randomised controlled trials (RCTs). We excluded non‐randomised studies because they would restrict our ability to imply causation of intervention effects, and because they are more likely to be subject to selection biases and confounders. We summarised narratively any non‐randomised evidence that we discovered and contrasted our results in the discussion. We included studies using individual or cluster‐randomisation, but we excluded cross‐over studies because of the likelihood of carryover effects. We included studies reported as full text, those published as abstract only and unpublished data.
Types of participants
We included studies in which the intervention was aimed at school staff of all types, including teachers, classroom assistants, school nurses and administrative staff. We applied no restrictions with regard to gender, age or qualifications of staff, and we included staff from any type of school with pupils up to age 19 (state‐run or private; comprehensive or single‐sex; primary, preparatory or secondary).
Types of interventions
We included studies comparing staff asthma education versus no intervention or a minimal intervention control. We included interventions aimed at educating school staff about asthma management and how to respond during an asthma attack. We excluded studies of interventions that involved multiple components other than asthma education unless the control group also received them.
Types of outcome measures
Primary outcomes
Visits to emergency department (ED)/hospital
Mortality
Asthma control (measured on a validated scale such as the Asthma Control Questionnaire (ACQ))
Secondary outcomes
Other adverse events (e.g. worsening of symptoms, delay in receiving short‐term therapy)
Adherence to asthma policies (e.g. proportion of children with an up‐to‐date PAAP at school, in‐date medications at school)
Absenteeism related to asthma
Staff self‐efficacy and preparedness
Qualitative synthesis
We recorded and synthesised the following to characterise educational interventions.
Educational content (primary material, learning outcomes, theoretical underpinning).
Teaching attributes of training programmes used (staff and resource requirements, length of course, any follow‐up service or session).
Search methods for identification of studies
Electronic searches
We searched for studies in the Cochrane Airways Group Trials Register, which is maintained by the Information Specialist for the Group. The Cochrane Airways Trials Register contains studies identified from several sources.
Monthly searches of the Cochrane Central Register of Controlled Trials (CENTRAL), through the Cochrane Register of Studies Online (crso.cochrane.org).
Weekly searches of MEDLINE Ovid SP 1946 to date.
Weekly searches of Embase Ovid SP 1974 to date.
Monthly searches of PsycINFO Ovid SP.
Monthly searches of the Cumulative Index to Nursing and Allied Health Literature (CINAHL) EBSCO.
Monthly searches of the Allied and Complementary Medicine Database (AMED) EBSCO.
Handsearches of the proceedings of major respiratory conferences.
Studies contained in the Trials Register are identified through search strategies based on the scope of the Cochrane Airways Group. We have provided details of these strategies, as well as a list of handsearched conference proceedings, in Appendix 1. See Appendix 2 for search terms used to identify studies for this review.
We also conducted searches of the Web of Science, the Pediatric Academic Societies archive, the Education Resources Information Center (ERIC), ClinicalTrials.gov (www.ClinicalTrials.gov) and the World Health Organization (WHO) trials portal (www.who.int/ictrp/en/) using appropriately adapted search terms (Appendix 3). We searched all databases from their inception to the present, and we imposed no restriction on language of publication. We conducted the most recent searches on 29 November 2016.
Searching other resources
We checked the reference lists of all primary studies and review articles for additional references.
On 20 October 2016, we searched for errata or retractions from included studies published in full text on PubMed (www.ncbi.nlm.nih.gov/pubmed).
Data collection and analysis
Selection of studies
Two review authors (RC and KK) independently screened titles and abstracts of all potential studies for inclusion identified as a result of the search, and coded them as 'retrieve' (eligible or potentially eligible/unclear) or 'do not retrieve'. We retrieved full‐text study reports/publications; two review authors (KK and RC, TD or MG) independently screened them to identify studies for inclusion and identified and recorded reasons for exclusion of ineligible studies. We resolved disagreements through discussion or by consultation with a third review author (RC, TD or MG, depending on who did the initial screen). We identified and excluded duplicates and collated multiple reports of the same study, so that each study rather than each report was the unit of interest in the review. We recorded the selection process in sufficient detail to complete a PRISMA (Preferred Reporting Items for Systematic Reviews and Meta‐Analyses) flow diagram and a Characteristics of excluded studies table (Moher 2009).
Data extraction and management
We used a data collection form that had been piloted on at least one study in the review to document study characteristics and outcome data. One review author (KK) extracted the following study characteristics from the included studies.
Methods: study design, total duration of study, details of any 'run‐in' period, number of study centres and locations, study setting, withdrawals and dates of study.
Participants: N, mean age, age range, gender, ethnicity, language, socioeconomic status, severity of condition, diagnostic criteria, baseline lung function, smoking history, inclusion criteria and exclusion criteria.
Interventions: intervention, comparison, concomitant medications and excluded medications.
Outcomes: primary and secondary outcomes specified and collected and time points reported.
Notes: funding for trial and notable conflicts of interest of trial authors.
Two review authors (KK and RC, TD or MG) independently extracted outcome data from included studies. We noted in the Characteristics of included studies table if outcome data were not reported in a useable way. We resolved disagreements by consensus. One review author (KK) transferred data into the Review Manager (RevMan 2014) file. We double‐checked that data were entered correctly by comparing data presented in the systematic review against those provided in study reports. A second review author (RC) spot‐checked study characteristics for accuracy against the trial report.
Assessment of risk of bias in included studies
Two review authors (KK and RC, TD or MG) independently assessed risk of bias for each study using the criteria outlined in the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011). We resolved disagreements by discussion or by consultation with other members of the review author team. We assessed risk of bias according to the following domains.
Random sequence generation.
Allocation concealment.
Blinding of participants and personnel.
Blinding of outcome assessment.
Incomplete outcome data.
Selective outcome reporting.
Other bias.
We graded each potential source of bias as high, low or unclear and provided a quote from the study report together with a justification for our judgement in the 'Risk of bias' table. We summarised risk of bias judgements across different studies for each of the domains listed. We considered blinding separately for different key outcomes when necessary (e.g. for unblinded outcome assessment, risk of bias for all‐cause mortality may be very different than for a patient‐reported pain scale). When information on risk of bias is related to unpublished data or correspondence with a trialist, we noted this in the 'Risk of bias' table.
When considering treatment effects, we took into account the risk of bias for studies that contributed to those outcomes.
Assessment of bias in conducting the systematic review
We conducted the review in accordance with this published protocol and reported deviations from it in the Differences between protocol and review section of the systematic review.
Measures of treatment effect
We analysed dichotomous data as odds ratios, and continuous data as mean differences or standardised mean differences. We entered data presented as a scale with a consistent direction of effect.
We undertook meta‐analyses only when this was meaningful (i.e. when treatments, participants and the underlying clinical question were similar enough for pooling to make sense).
We narratively described skewed data reported as medians and interquartile ranges.
When multiple trial arms were reported in a single trial, we included only relevant arms. If two comparisons (e.g. two types of asthma education interventions vs usual care) were combined in the same meta‐analysis, we halved the control group to avoid double‐counting.
If both change from baseline and endpoint scores were available for continuous data, we used change from baseline unless most studies reported endpoint scores. If a study reported outcomes at multiple time points, we used the end‐of‐study measurement.
When both an analysis including only participants who completed the trial and an analysis that imputed data for participants who were randomly assigned but did not provide endpoint data (e.g. last observation carried forward) were available, we used the latter.
Qualitative analysis
We extracted and planned a synthesis of qualitative data about content and attributes of educational interventions tested in the included studies to supplement the main quantitative analyses. We did not include studies that were qualitative reports of training programmes, with no quantitative assessment. When qualitative data were provided, we avoided making a priori hypotheses and conclusions, in keeping with a grounded theory approach. After collecting data and contacting study authors for additional information, we were unable to conduct the planned synthesis. If we had been able to, two review authors (MG and KK) would have individually coded data and developed an initial thematic index, and would have added emerging thematic categories according to interpretation of data content. We planned that the analysis would proceed through three stages, consisting of open, axial and selective coding, with comparison through each phase. We designed the analysis in this way to provide categories that could be used to explore themes of the data and to build an interpretation that could address overarching research questions.
Unit of analysis issues
For dichotomous outcomes, we used participants, rather than events, as the unit of analysis (i.e. number of children admitted to hospital, rather than number of admissions per child). We meta‐analysed data from cluster‐RCTs only if available data could be adjusted to account for clustering. In the case of Bell 2000, study authors did not report any adjustment for clustering; we adjusted the data using an estimated intracluster correlation coefficient (ICC) of 0.05 for the one meta‐analysis to which this study contributed.
Dealing with missing data
We contacted investigators or study sponsors to verify key study characteristics and to obtain missing numerical outcome data when possible (e.g. when we identified a study as abstract only). When this was not possible, and we believed that missing data might introduce serious bias, we explored the impact of this by assigning the GRADE rating for each outcome.
Assessment of heterogeneity
We assessed educational heterogeneity by comparing the distribution of important participant characteristics between trials (e.g. age of pupils concerned, learner groups) and methodological heterogeneity through trial characteristics (randomisation, concealment, blinding of outcome assessment, losses to follow‐up, treatment type, co‐interventions). We collected and presented these characteristics in the Characteristics of included studies tables and summarised similarities and differences between studies in the results. We assessed statistical heterogeneity by examining the I² statistic ‐ a quantity that describes the proportion of variation in point estimates that is due to variability across studies rather than to sampling error. We interpreted the I² statistic as suggested in the latest version of Higgins 2011.
0% to 40%: might not be important.
30% to 60%: may represent moderate heterogeneity.
50% to 90%: may represent substantial heterogeneity.
75% to 100%: suggests considerable heterogeneity.
We also evaluated the confidence interval (CI) for the I² statistic. We employed a Chi² test of homogeneity, with a 5% level of significance, to determine the strength of evidence that heterogeneity is genuine.
Review authors judged clinical and methodological heterogeneity by discussion once data had been extracted. We did this to identify barriers to effective and appropriate meta‐analysis, as well as to any relevant sensitivity analysis, based on this primary data set.
Assessment of reporting biases
We were not able to pool more than 10 studies, so we could not create or examine a funnel plot to explore possible small‐study and publication biases.
Data synthesis
We used a random‐effects model and performed a sensitivity analysis by using a fixed‐effect model.
'Summary of findings' table
We created a 'Summary of findings' table using the primary and secondary outcomes listed in the protocol. We used the five GRADE (Grades of Recommendation, Assessment, Development and Evaluation Working Group) considerations (study limitations, consistency of effect, imprecision, indirectness and publication bias) to assess the quality of a body of evidence as it relates to studies that contribute data to meta‐analyses for prespecified outcomes. We used methods and recommendations as described in Section 8.5 and Chapter 12 of the Cochrane Handbook for Systematic Reviews of Interventions (Higgins 2011) while using GRADEpro GDT software. We justified all decisions to downgrade or upgrade the quality of studies by using footnotes, and we made comments to aid the reader's understanding of the review when necessary.
Subgroup analysis and investigation of heterogeneity
We planned the following subgroup analyses for primary outcomes.
Primary school (entry age to 11 years) versus secondary school interventions (11 to 19 years of age).
Children at primary school may have broadly different needs from adolescents at secondary school with regards to behaviours, social support and extent of involvement of parents and school staff in their asthma care. We anticipated that trials conducted in different countries would vary in their terminology and in the ages at which children progress to 'secondary' education, so we have been transparent in the way we classified studies.
We recognise that, for various reasons, children who are socially isolated or who belong to minority groups have higher mortality and morbidity from asthma (Global Asthma Report 2014), but assessing the effects of these factors would not have been straightforward if we had performed a subgroup analysis. Alternatively, we presented key characteristics of study populations and interventions in an additional table to capture potential sources of heterogeneity that were not easily assessed in subgroups (e.g. socioeconomic status, duration and content of interventions, ethnicity, first language, asthma severity criteria).
We planned to use the formal test for subgroup interactions provided in Review Manager (RevMan 2014).
Sensitivity analysis
We planned the following sensitivity analyses to remove the following from the primary analyses.
Unpublished data.
Studies at high risk in any selection bias domain.
Results
Description of studies
Results of the search
We identified 240 records by searching the Cochrane Airways Group Specialised Register (CAGR), and we identified 151 in additional searches: 39 from Web of Science, seven from ERIC, six from the Pediatric Academic Societies Archive, 10 from clinicaltrials.gov and 89 from the WHO trials portal. Thirteen were duplicates, and we sifted the remaining 378 unique records. We excluded 331 after looking through titles and abstracts, and we obtained full texts for the other 47. We excluded 41 that did not meet the inclusion criteria, which we collated and listed as 34 studies (see Figure 1 and Excluded studies). We included six records related to five studies.
1.
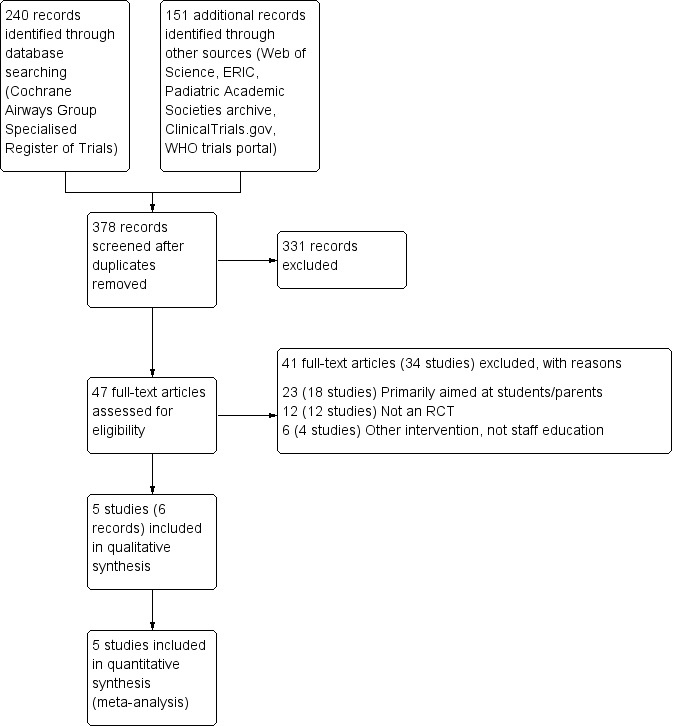
Study flow diagram.
Included studies
We provided additional details for each of the included studies in the Characteristics of included studies table and an overview of intervention characteristics in Table 2.
1. Intervention characteristics.
| Study | Population | Setting | Asthma prevalence | Follow‐up | Asthma diagnosis | Intervention |
| Bell 20000 | 113 teachers | Primary schools, UK | % classes by children with asthma: 0 = 17% 1 to 4 = 59% 5 or more = 23% |
1 month | Unclear | Single 40‐minute session for teachers |
| Bruzzese 2006 | 591 children with asthma and their families | Primary schools, USA | All families had a child with asthma | Most 12 months, some outcomes at 24 months+ | Clinician diagnosis and persistent symptomsa | 3‐day health team workshop, single 45‐minute sessions for teachers, ongoing school support |
| Henry 2004 | 1815 teachers (776 with data) | Year 8 classes, Australia | 23.7% of intervention group; 20.8% of control group | 6 to 8 months | Clinician diagnosis + asthma medication or attack in the previous year | Seminar + 3 in‐school teacher‐led sessions for staff |
| Kawafha 2015 | 80 teachers | Primary schools, Jordan | None | 3 months | N/A | 3 in‐school sessions for teachers |
| McCann 2006 | 209 children with asthma and their families | Primary schools, UK | All families had a child with asthma | 12 months | Asthma medication and wheeze in previous year | Single 1‐hour session for teachers + 45‐minute workshop for pupils |
| aNHLBI criteria = daytime symptoms at least 3 times a week and night‐time symptoms 3 or more times a month | ||||||
Design
This review includes five RCTs (Bell 2000; Bruzzese 2006; Henry 2004; Kawafha 2015; McCann 2006). The trials involved 111 schools, although one study (Kawafha 2015) did not report the number of schools included. Four studies used a parallel cluster‐RCT design (Bell 2000; Bruzzese 2006; Henry 2004; McCann 2006), with schools as the unit of allocation for randomisation, and one used a pre‐test/post‐test cluster‐RCT design, in which teachers were randomised to intervention or control groups (Kawafha 2015). The period of observation ranged from 4 weeks (Bell 2000) to 12 months for most outcomes, and one study conducted follow‐up at 24 months and measured absences at 2.5 years (Bruzzese 2006).
Sample sizes
Three studies included teachers as participants, randomising 1815 (Henry 2004), 113 (Bell 2000) and 80 (Kawafha 2015); investigators included data from only 776 (38.6%) in the analyses, primarily because only 60% of the randomised teachers in Henry 2004 completed baseline questionnaires. In one study, participants consisted of 591 families with a child for whom asthma had been diagnosed (Bruzzese 2006), and another study included 209 children with asthma as participants (McCann 2006).
Participants and setting
Investigators carried out all studies in schools ‐ two in the UK (Bell 2000; McCann 2006), one in the United States (Bruzzese 2006), one in Jordan (Kawafha 2015) and one in Australia (Henry 2004). Four studies included children of primary age (Bell 2000; Bruzzese 2006; Kawafha 2015; McCann 2006), and one study enrolled students during year 8 of high school (13 to 14 years of age) (Henry 2004). Three studies did not report socioeconomic status (Bell 2000; Henry 2004; McCann 2006); one of these stated that results showed no differences in markers of social deprivation between groups but that baseline information was not available (McCann 2006). In one study, more than 50% of students in eligible schools were receiving free lunch and more than 67% belonged to ethnic minorities (Bruzzese 2006). Another study sampled schools from selected areas that consisted of urban and rural participants of different socioeconomic status (Kawafha 2015). One study provided no details about the children included (Bell 2000). In three studies, boys and girls were equally represented (Bruzzese 2006; Henry 2004; McCann 2006), and in another study, only girls participated (Kawafha 2015).
Three studies defined asthma as a current diagnosis of asthma in children (Bruzzese 2006; Henry 2004; McCann 2006). Bruzzese 2006 stipulated that children had to have a prior asthma diagnosis and had to meet National Heart Lung and Blood Institute (NHLBI) criteria for persistent symptoms (daytime symptoms at least three times a week and night‐time symptoms three times a month). Henry 2004 required a doctor's diagnosis plus use of asthma medication or an asthma attack in the past 12 months, and McCann 2006 required use of asthma medication and recent wheeze symptoms. Two studies specifically recruited families of children with asthma but did not report the proportion with asthma within the schools (Bruzzese 2006; McCann 2006). Bell 2000 reported the number of children with asthma in each participating class (17% included no children with asthma; 60% included one to four children with asthma; and 23% included five or more children with asthma), and Henry 2006 reported that 23.7% of children in the intervention group and 20.8% of those in the control group had received a diagnosis of asthma; one study specifically stated that the classes of teachers who participated in the study included no children with asthma (Kawafha 2015). When teachers were the participants (Bell 2000; Kawafha 2015), only one study reported their baseline characteristics; all were female with a mean age of 36 years in the intervention group and 34 years in the control group (Kawafha 2015). One study reported that 91.7% of teachers in the intervention group and 62.2% of those in the control group had received previous training in asthma (Bell 2000).
Interventions
Interventions provided in these studies included educational programmes or training sessions (Table 2). In three studies, training sessions generally lasted about 40 to 45 minutes (Bell 2000; Bruzzese 2006; McCann 2006), and in two studies, the intervention consisted of three in‐school sessions (Henry 2004; Kawafha 2015) with a seminar added to one of these (Henry 2004). In two studies, researchers delivered sessions to teachers (Bell 2000; Kawafha 2015). One of these was a pharmacist (Bell 2000), and the other a nurse (Kawafha 2015). Other studies selected a school nurse and a physician (Bruzzese 2006), teachers who had attended a one‐day in–service seminar (Henry 2004) or a nurse (McCann 2006) to lead sessions.
Training sessions for teachers in all studies provided information about the pathophysiology, symptoms and trigger factors for asthma, as well as medications used, actions to be taken in an emergency and the role of teachers in helping children manage asthma at school. Three studies also included pupil workshops (Bruzzese 2006; Henry 2004; McCann 2006) as part of the Personal Development (PD) portion of the curriculum (Henry 2004), or consistent with the Science National Curriculum (McCann 2006). One study provided training for students' primary care providers (Bruzzese 2006). Three studies indicated that they offered the intervention to schools in the control group after the study had concluded (Bell 2000; Bruzzese 2006; Henry 2004).
Outcomes
Two studies measured asthma knowledge at baseline and follow‐up using the Newcastle Asthma Knowledge Questionnaire (NAKQ) (Bell 2000; Henry 2004). One study used a structured questionnaire that requested demographic data and the Asthma General Knowledge Questionnaire for Adults (AGKQA) (Kawafha 2015). Two studies collected follow‐up data from students on quality of life and use of asthma treatments(Henry 2004; McCann 2006), and one study collected these data from caregivers (Bruzzese 2006). Three studies reported school absences (Bruzzese 2006; Henry 2004; McCann 2006).
Bell 2000 recorded observations for four weeks, Kawafha 2015 for three months, Henry 2004 for six to eight months and Bruzzese 2006 and McCann 2006 for one year. Bruzzese 2006 followed up via telephone for some outcomes at two years and measured absences up to 2.5 years.
Funding sources
Three studies received funding from a variety of sources (Bruzzese 2006; Henry 2004; McCann 2006). One study received no financial support (Kawafha 2015), and one study did not report funding (Bell 2000).
Excluded studies
We listed 32 studies as excluded after consulting the full texts to determine their eligibility. The most common reason for exclusion was that the intervention was aimed solely or primarily at students or parents rather than at school staff (18 studies; Al‐Sheyab 2015; Bruzzese 2011; Bruzzese 2011a; Bruzzese 2014; Bush 2014; Cicutto 2003; Cicutto 2013; Clark 2004; Gallefoss 1997; Gerald 2006; Horspool 2013; Kintner 2009; Kintner 2015; McGhan 2000; Monforte 2012; NCT00304304; NCT01607749; Perry 2015). We excluded 11 studies because they did not use a randomised controlled trial design (Abdel Gawwad 2007; Clark 2013; Gibson‐Young 2014; Hazell 1995; Henry 2006; Korta Murua 2012; Murray 2007; NCT00005736; Olympia 2005; Soo 2013; Wong 2004). Some of these were otherwise directly relevant to this review, and we have summarised them in the discussion (Abdel Gawwad 2007; Hazell 1995; Korta Murua 2012; NCT00005736; Olympia 2005; Snow 2004; Wong 2004). Four studies tested different types of interventions in schools: Halterman 2012 and Tapp 2011 assessed web‐based asthma management systems that connected schools and healthcare providers, Francis 2000 assessed whether asthma reviews could be provided at school instead of at the office of the child's general practitioner (GP) and Splett 2006 tested an intervention aimed at schools and clinics to improve overall adoption of guideline‐based care.
Risk of bias in included studies
Figure 2 presents a summary of risk of bias judgements.
2.
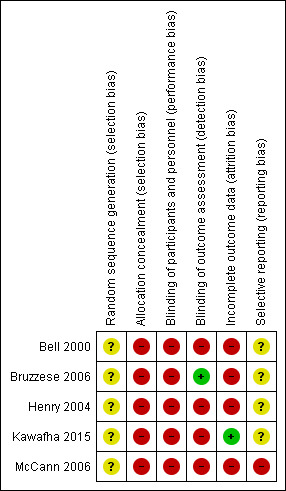
Risk of bias summary: review authors' judgements about each risk of bias item for each included study.
Allocation
We determined that none of the studies was at low risk of bias for either of the selection bias domains. We judged all studies as having unclear risk for random sequence generation because study authors did not describe methods. Most of the information provided concerned selection of eligible schools that were approached to take part and how investigators attempted to balance characteristics across groups, rather than how the random code was generated. We considered all studies to be at high risk of bias owing to issues with allocation concealment, primarily the way in which study investigators matched and assigned participants or schools to balance characteristics across groups. This was particularly the case in cluster trials, which paired schools before randomisation to balance factors such as types and locations of schools and socioeconomic variables. Although legitimate, this matching would have prevented full concealment of allocation and may have led to selection biases, especially when clusters were few.
Blinding
Owing to the nature of the interventions delivered in these studies, blinding was not possible for those delivering or receiving the intervention, and this may have, intentionally or unintentionally, affected how participants and study staff in each group behaved. This performance bias is evident in the treatment that each group received and in the ways participants behaved simply by knowledge of their allocation, and it may have affected outcomes in different ways. Only one study described methods used to blind outcome assessors (Bruzzese 2006), but some outcomes will not be biased by lack of outcome assessor blinding. For this reason, we considered the possible effects of performance and detection biases separately for each outcome when we applied GRADE criteria.
Incomplete outcome data
We considered one study to be at low risk of bias (Kawafha 2015); although dropout was higher in the intervention group (10%) than in the control group (5%), investigators reported few missing data over the course of the three‐month study.
We considered four studies to be at high risk of attrition bias (Bell 2000; Bruzzese 2006; Henry 2004; McCann 2006). Bell 2000 tested a four‐week intervention but reported 32% missing data in the intervention group and 25% in the control group because teachers did not fill out the questionnaires. Bruzzese 2006, Henry 2004 and McCann 2006 were longer studies (with time points ranging from six months to two years) that described a large quantity of missing data by the time of final data collection. In Bruzzese 2006, the level of retention was similar between groups and researchers performed intent‐to‐treat analyses, but the quantity of missing data (and hence of data that had to be imputed) was high, especially by the two‐year endpoint (around 38% for caregivers and children). Henry 2004 could analysed only data from students or teachers that could be paired from both time points, meaning that 82.7% of students and 43.9% of teachers contributed to the data analysis. Furthermore, analysis included far more teachers from the control group (54%) than from the intervention group (37.8%).
In McCann 2006, although the number of children dropping out was fairly low and balanced (12.3% and 11.5% for intervention and control groups, respectively), a substantial quantity of data was missing for some outcomes, particularly staff asthma knowledge. Therefore, risk of attrition bias for this study is dependent on outcomes.
Selective reporting
We did not identify trial registrations for any of the included studies, so it was difficult to assess the extent to which study authors reported their planned outcomes. For this reason, we rated four studies as having unclear risk of reporting bias (Bell 2000; Bruzzese 2006; Henry 2004; Kawafha 2015). We judged McCann 2006 to be at high risk of reporting bias because investigators reported data for several outcomes of interest to the review in a way that did not allow their inclusion in a meta‐analysis. The publication focused on associations with treatment modifiers (e.g. sex, pet ownership, social deprivation) rather than on overall treatment effects versus the control group, and study authors reported some outcomes simply as "no effect" (e.g. absence).
Effects of interventions
See: Table 1
Primary outcomes
Visits to emergency department (ED)/hospital
Bruzzese 2006 reported mean numbers of ED visits, urgent visits and hospital visits per participant in the previous 12 months, both at one year and at two years post intervention. We did not analyse the data because an obvious skew makes the results difficult to interpret. We presented the data as reported in the paper (Analysis 1.1) and did not attempt to apply GRADE criteria to this outcome.
1.1. Analysis.
Comparison 1 Staff asthma education versus control, Outcome 1 Visits to ED/hospital (mean per child).
| Visits to ED/hospital (mean per child) | |||||
|---|---|---|---|---|---|
| Study | Type of visit |
Education (N=244) 1 year |
Control (N=228) 1 year |
Education (N=195) 2 years |
Control (N=173) 2 years |
| Bruzzese 2006 | Hospital visits | 0.1 (0.4) | 0.1 (0.6) | 0.2 (0.6) | 0.1 (0.3) |
| Bruzzese 2006 | ED visits | 1.0 (1.8) | 1.3 (3.2) | 0.9 (2.2) | 0.9 (1.8) |
| Bruzzese 2006 | Urgent care visits | 2.1 (3.5) | 3.2 (13.8) | 1.7 (3.0) | 1.8 (3.6) |
Mortality
We found no reports of any deaths that occurred during the course of these studies.
Asthma control
No studies reported validated measures of asthma control such as the Asthma Control Test (ACT) or the Asthma Control Questionnaire (ACQ). Two studies reported validated measures of asthma‐related quality of life, which we have presented as a post hoc proxy for asthma symptom control. When we pooled 12‐month caregiver data from Bruzzese 2006 with student‐reported measurements from Henry 2004, we found no differences between groups (mean difference (MD) 0.14, 95% confidence interval (CI) ‐0.03 to 0.31; 1005 participants; two studies; I² = 0%; low‐quality evidence); both confidence limits were well below the 0.5 minimal clinically important difference (MCID) for the scale. A sensitivity analysis based on a fixed‐effect model did not change these results. Follow‐up data at 24 months in Bruzzese 2006 were in the opposite direction but confidence limits again fell almost entirely within the 0.5‐point MCID (also shown in Analysis 1.2). Bruzzese 2006 presented data as final scores with evidence of imbalance at baseline, so we calculated the change from baseline and used variance for final scores. This may have resulted in underestimated precision, but this is not an issue because effect estimates were neither statistically nor clinically significant.
1.2. Analysis.
Comparison 1 Staff asthma education versus control, Outcome 2 Asthma control ‐ quality of life (PAQLQ).
Bruzzese 2006 also reported non‐validated counts of symptom days, night‐time awakenings and restricted activities of daily living (ADLs), all for the past two weeks and the past six months, at 12 and 24 months. We did not analyse the data, as they were skewed; some mean scores were better in the active group, but most differences between groups were small and did not persist to 24 months. We did not attempt to apply GRADE criteria to this outcome.
Secondary outcomes
Other adverse events
No studies reported adverse events (e.g. worsening of symptoms, delay in receiving short‐term therapy) that occurred during the course of the interventions. The only study that reported adverse events related to asthma was Bruzzese 2006; we have summarised these data in the section 'Visits to ED/hospital' under Effects of interventions.
Adherence to asthma policies
Two studies reported the number of schools that had asthma policies before and after the intervention (Henry 2004; McCann 2006), and one study reported the number of schools that improved measures taken to prevent exercise‐induced asthma attacks and the number of principals reporting that most or all of their staff knew how to administer salbutamol via a spacer. We have presented these data side by side in Analysis 1.3.
1.3. Analysis.
Comparison 1 Staff asthma education versus control, Outcome 3 Adherence to asthma policies.
More schools that had received staff asthma training had written asthma policies compared with control schools (odds ratio (OR) 4.45, 95% CI 1.38 to 14.30). However, more intervention schools had policies at baseline, both in McCann 2006 (5/12 intervention; 3/12 control) and in Henry 2004 (3/17 intervention; 2/16 control).
Henry 2004 found that more intervention schools showed improvement in measures taken to prevent or manage exercise‐induced asthma attacks (OR 9.33, 95% CI 1.65 to 52.68) and more of these schools reported that staff felt able to administer salbutamol via a spacer (OR 20.22, 95% CI 3.45 to 118.65).
Overall, we assessed the evidence for this outcome to be of low quality because we had concerns about risk of bias in the included studies and about imprecision.
A sensitivity analysis based on a fixed‐effect model did not change the results.
Absenteeism related to asthma
Two studies measured absenteeism (Bruzzese 2006; McCann 2006). Data from Bruzzese 2006 were skewed, so we did not analyse them as a mean difference. Instead, we have presented in Analysis 1.4 the data reported by Bruzzese 2006 at one and two years for the mean number of absences per child over the past two weeks.
1.4. Analysis.
Comparison 1 Staff asthma education versus control, Outcome 4 Absenteeism related to asthma (mean per child).
| Absenteeism related to asthma (mean per child) | |||||
|---|---|---|---|---|---|
| Study | Timepoint | Education group | Education N | Control group | Control N |
| Bruzzese 2006 | 1 year | 0.5 (SD 1.4) | 244 | 0.9 (SD 1.8) | 228 |
| Bruzzese 2006 | 2 years | 0.8 (SD 1.5) | 195 | 0.8 (SD 1.6) | 173 |
McCann 2006 reported that "no effect of the intervention was found" after adjusting for social deprivation, and that "absences were considerably lower than...anticipated in relation to the power calculations on which the recruitment numbers were based".
We did not attempt to apply GRADE criteria to this outcome.
Staff self‐efficacy and preparedness
Three studies used staff knowledge scales that could be combined in an analysis (Bell 2000; Henry 2004; Kawafha 2015). Knowledge was higher in groups that had received asthma education, although it is difficult to interpret the meaningfulness of this difference (standardised mean difference (SMD) 0.74, 95% CI 0.33 to 1.16; 640 participants; three studies; I² = 73%). Statistical heterogeneity in the analysis might be explained by differences in the scales used or variation in the time points at which measurements were taken (four weeks to eight months). A sensitivity analysis based on a fixed‐effect model yielded a more precise estimate but did not change the conclusions.
Studies reported various other measures that reflected staff preparedness. Bell 2000 provided mainly categorical data on questions within the knowledge questionnaire regarding how many staff recognised wheeze or cough as a symptom after the four‐week intervention, the number of trigger factors that were correctly identified, the number of ways used to prevent exercise‐induced asthma that were correctly identified and the number of preventive medicines that were correctly identified. The data, although difficult to interpret, generally point to somewhat better responses in the intervention group, which would be expected.
Henry 2004 reported the number of schools seeking additional input about asthma, which may reflect greater appreciation of the seriousness of asthma after the intervention; 11 of 17 intervention schools sought additional information about asthma during the observation period, compared with 3 of 16 control schools. This study also reported staff attitudes (split into 'internal control', 'powerful others' and 'chance'), which we did not deem relevant for inclusion in this review.
McCann 2006 narratively reported staff asthma knowledge. Investigators noted that some measures of asthma knowledge were low at baseline (e.g. only 16.8% and 17.7% noted exercise and colds as asthma triggers, respectively) but that most staff correctly identified differences between reliever and preventer medications. Around half of the teachers were concerned about having children with asthma in their class, and 40% reported that they were not confident about dealing with an asthma attack. It is important to note that intervention schools did not reveal a significant change in these measures.
Qualitative synthesis
We recorded information regarding educational content and teaching attributes of the interventions. Information in published reports was not sufficient to allow a meaningful synthesis of the content that led to a successful intervention, nor of the resources required to replicate it accurately. We have provided a summary of details for each study in the Characteristics of included studies table and in the descriptions of studies above.
Discussion
Summary of main results
This review includes five cluster‐randomised controlled trials (RCTs) (Bell 2000; Bruzzese 2006; Henry 2004; Kawafha 2015; McCann 2006), which included a total of 111 schools in the UK, the United States, Australia and Jordan. Investigators measured outcomes among participating staff and often in children or parents, most often at between 1 month and 12 months.
Researchers carried out all studies in schools. Interventions provided were educational programmes or training sessions, but the duration, content and method of delivery varied. Some studies also involved workshops for pupils or training sessions for primary care providers. Owing to the necessary design of these trials, risks of selection, performance, detection and attrition bias were present to a differing extent across studies and outcomes.
Quanitative and qualitative analyses were limited. Only one study reported visits to emergency department (ED) or hospital, and these data were too skewed for analysis. No studies reported any deaths or adverse events. Studies did not report asthma control consistently but data from the paediatric asthma quality of life questionnaire revealed no differences between groups (mean difference (MD) 0.14, 95% confidence interval (CI) ‐0.03 to 0.31; 1005 participants; quality downgraded to low for risk of bias and indirectness). All data on symptom days, night‐time awakenings, restricted activities of daily living and school absences were skewed or could not be analysed; some mean scores were better in the trained group, but most differences between groups were small and did not persist to 24 months.
Schools that received asthma education were more adherent to asthma policies, and staff at these schools were better prepared; more schools that had received staff asthma training had written asthma policies compared with control schools, more intervention schools showed improvement in measures taken to prevent or manage exercise‐induced asthma attacks and more staff at intervention schools felt that they were able to administer salbutamol via a spacer. However, the quality of the evidence was low; data showed some imbalance at baseline, and confidence in the evidence was limited by risk of bias and imprecision. Staff knowledge was higher in groups that had received asthma education, although results were inconsistent and were difficult to interpret owing to differences between scales (low quality).
Information about the interventions was insufficient to allow a meaningful qualitative synthesis of content that led to a successful intervention or of resources required to replicate findings accurately.
Overall completeness and applicability of evidence
The five included studies enrolled more than 100 schools, although data for no more than 1005 students with asthma, 640 teachers or 57 schools contributed to any single analysis. This reduced the applicability of study findings, limited the precision of results and prevented investigation into moderating factors of interventions and participants. We could not conduct subgroup analysis as planned to test whether effects of educating school staff differed between primary and secondary schools (none of the studies included children older than 13 years of age), nor could we test the robustness of results by limiting analyses to published data or to studies at low risk of selection bias.
This review could not identify the content and attributes underpinning successful interventions, which means that review findings are difficult to apply in real‐world settings. We set out to find evidence about interventions aimed at educating staff on how to respond during an asthma attack and how to manage children's asthma effectively at school, but interventions often included additional materials and elements aimed at other groups (e.g. pupil workshops, training sessions for healthcare providers), making it difficult to isolate the effects of interventions, and the small number of included studies prevented meaningful assessment of different aspects of the interventions provided. Required resources varied from a short single session (Bell 2000) to repeated longer sessions (Henry 2004; Kawafha 2015), and we could not discern whether more intensive interventions led to larger or more sustained effects.
Although we could not assess formally whether asthma education provided for school staff is more or less important for children from minority backgrounds or for those from lower‐income families, we noted a good demographic spread within and between studies. No studies took place in lower‐income or lower‐middle‐income countries, one was conducted in an upper‐middle‐income country (Jordan) and four were completed in high‐income countries (Australia, the UK and the United States). One study specifically focused on a population of lower socioeconomic status (Bruzzese 2006).
We designed this review to focus on important clinical effects of staff asthma education on children's health, but identified studies often were not designed or powered to measure or detect benefit for rare events such as mortality or hospital visits. The resources required to conduct studies of complex interventions in community settings are significant, and this may explain why follow‐up was limited for most of the included studies. Outcomes measured in the included studies that were not captured in this review may provide important insights on matters such as sustainability of the intervention (Henry 2004) or benefit for case detection (Bruzzese 2006). These important considerations may be more suitably assessed by a review of non‐randomised literature designed to supplement randomised evidence of effectiveness. We chose to limit this review to randomised evidence so that we could make more solid inferences about cause and effect, but in practice, we found this difficult to do owing to biases that were difficult to control. The larger non‐randomised evidence base, which has been reviewed previously and is summarised below, serves to bolster our findings, but the lack of evidence on how (and whether) staff apply the knowledge gained from such programmes is discouraging (Jaramillo 2015; Murray 2007; Soo 2013).
Quality of the evidence
We were not able to apply GRADE criteria to all outcomes as planned because we could not pool data for some analyses. When pooling was possible, we had low confidence in the evidence. Primarily, our confidence in study findings was limited by inherent biases related to trial design. Cluster, open‐label trials are most appropriate for assessing this type of intervention but often cannot control for biases related to participants' knowledge of allocation, difficulties in concealing allocation while trying to balance moderating factors and incomplete data from participating children and teachers. These characteristics mean that although trials are being conducted in a real‐world context, presenting strong conclusions about their findings is difficult, especially across trials with variations in design and implementation.
Heterogeneity, methodological and statistical, also reduced our confidence in some findings. Methodological heterogeneity was sometimes introduced because trials used different measures or time points for the same outcome, but multiple unidentifiable sources of heterogeneity within this sort of review may be due to the complexity of interventions and contexts. For this reason, although we were able to pool results for some meta‐analyses, we limited this approach in favour of more nuanced narrative syntheses. We found that results were sometimes limited by imprecision of the estimates related to the fact that only scant data could be pooled.
Potential biases in the review process
We carried out the review according to the published protocol (Kew 2016) and detailed any deviations from it under Differences between protocol and review. Insufficient data prevented us from carrying out qualitative analysis of intervention characteristics and limited the conclusions that could be drawn from quantitative analyses. We attempted to contact study authors to request additional outcome data and intervention characteristics but were able to contact only the authors of Bell 2000 and Bruzzese 2006. We could not obtain data from authors of the Henry 2004 study, as the primary investigator has since retired; we failed to make contact with the authors of Kawafha 2015 and McCann 2006. Any data forthcoming after publication of this review will be filed appropriately for future updates of this review.
Agreements and disagreements with other studies or reviews
A recent systematic review (Soo 2013) collated randomised and non‐randomised evidence (two and eight studies, respectively) on staff asthma education provided to improve pharmacological management of acute asthma in schools; both of the randomised trials considered in this previous review are included in the present review (Bell 2000; McCann 2006). Soo 2013 focused on younger children and excluded studies that included only high‐school‐aged children and adolescents. Results presented by Soo 2013 are very much in agreement with our finding that education effectively increases asthma knowledge among school staff, but evidence is limited regarding how such knowledge can be applied in practice. Inclusion in the former review of non‐randomised evidence, which we also collated for review but not for inclusion, further supports this finding.
Jaramillo 2015 collated nine primary studies that assessed teacher knowledge and adherence to asthma policies in US schools and found high reliance on school nurses and gaps in knowledge about how to guide asthma management. The latter theme runs through the literature in various countries (Abdel Gawwad 2007; Olympia 2005) and is supported by baseline characteristics and observations reported by our included studies. Unfortunately, interventions assessed thus far in randomised trials do not show that education addresses this problem effectively.
Non‐randomised studies have reported varying success of different types of asthma education programmes for school staff, ranging from information pamphlets or presentations (Abdel Gawwad 2007; Snow 2004) to more complex educational interventions (Korta Murua 2012) and partnerships between schools and healthcare providers (NCT00005736; Olympia 2005). Findings focus on misgivings of current asthma knowledge in the schools or on ways to improve staff knowledge but do not show a measurable effect on important outcomes for children. The non‐randomised evidence is based on a similar range of interventions, and most findings are consistent with those based on randomised evidence.
Authors' conclusions
Implications for practice.
Asthma education for school staff increases asthma knowledge and preparedness, but studies are varied and all evidence is of low quality. Studies have not yet captured whether this improvement in knowledge has appreciable benefit over a short or longer term for the safety and health of children with asthma in school. Randomised evidence does not contribute to our understanding of what content or attributes of interventions lead to best outcomes, nor what resources are required for successful implementation.
Implications for research.
Studies are needed to address the evidence gap in this field. Future studies should recognise the unique context of educational research if they are to identify not only whether an intervention is effective, but what key content is associated with effectiveness. Publications of educational research should include a full description of intervention content and resources required to allow feasibility assessments and replication. This applies to both randomised and non‐randomised studies, although the latter may be better placed to observe important clinical outcomes such as exacerbations and mortality over the longer term.
Acknowledgements
We would like to thank study authors who took the time to respond to our requests for additional information: James McElnay and Heather Bell regarding Bell 2000, Peter Gibson with regard to Henry 2004 and Jean‐Marie Bruzzese for Bruzzese 2006.
We are very grateful to teaching staff who provided invaluable feedback on the manuscript: Hannah Rye, Helen Woolley, Jeremy Finch and Mark Fanchi.
The Background and Methods sections of this review are based on a standard template used by the Cochrane Airways Group. We are very grateful to Elizabeth Stovold for designing the search strategy, and to all other Cochrane Airways Group staff members for editorial support provided.
Rebecca Normansell was the Editor for this review and commented critically on the review.
Appendices
Appendix 1. Sources and search methods for the Cochrane Airways Group Specialised Register (CAGR)
Electronic searches: core databases
| Database | Frequency of search |
| CENTRAL | Monthly |
| MEDLINE (Ovid) | Weekly |
| Embase (Ovid) | Weekly |
| PsycINFO (Ovid) | Monthly |
| CINAHL (EBSCO) | Monthly |
| AMED (EBSCO) | Monthly |
Handsearches: core respiratory conference abstracts
| Conference | Years searched |
| American Academy of Allergy, Asthma and Immunology (AAAAI) | 2001 onwards |
| American Thoracic Society (ATS) | 2001 onwards |
| Asia Pacific Society of Respirology (APSR) | 2004 onwards |
| British Thoracic Society Winter Meeting (BTS) | 2000 onwards |
| Chest Meeting | 2003 onwards |
| European Respiratory Society (ERS) | 1992, 1994, 2000 onwards |
| International Primary Care Respiratory Group Congress (IPCRG) | 2002 onwards |
| Thoracic Society of Australia and New Zealand (TSANZ) | 1999 onwards |
MEDLINE search strategy used to identify trials for the CAGR
Asthma search
1. exp Asthma/
2. asthma$.mp.
3. (antiasthma$ or anti‐asthma$).mp.
4. Respiratory Sounds/
5. wheez$.mp.
6. Bronchial Spasm/
7. bronchospas$.mp.
8. (bronch$ adj3 spasm$).mp.
9. bronchoconstrict$.mp.
10. exp Bronchoconstriction/
11. (bronch$ adj3 constrict$).mp.
12. Bronchial Hyperreactivity/
13. Respiratory Hypersensitivity/
14. ((bronchial$ or respiratory or airway$ or lung$) adj3 (hypersensitiv$ or hyperreactiv$ or allerg$ or insufficiency)).mp.
15. ((dust or mite$) adj3 (allerg$ or hypersensitiv$)).mp.
16. or/1‐15
Filter to identify RCTs
1. exp "clinical trial [publication type]"/
2. (randomized or randomised).ab,ti.
3. placebo.ab,ti.
4. dt.fs.
5. randomly.ab,ti.
6. trial.ab,ti.
7. groups.ab,ti.
8. or/1‐7
9. Animals/
10. Humans/
11. 9 not (9 and 10)
12. 8 not 11
The MEDLINE strategy and RCT filter are adapted to identify trials in other electronic databases.
Appendix 2. Search strategy to identify relevant trials from the CAGR
#1 AST:MISC1
#2 MeSH DESCRIPTOR Asthma Explode All
#3 asthma*:ti,ab
#4 #1 or #2 or #3
#5 MeSH DESCRIPTOR Schools Explode All
#6 MeSH DESCRIPTOR Teaching
#7 MeSH DESCRIPTOR School Health Services
#8 MeSH DESCRIPTOR School Nursing
#9 teacher*
#10 classroom* NEXT assistant*
#11 teaching* NEXT assistant*
#12 school* NEAR nurs*
#13 (school* or teach*) NEAR (staff* or personnel*)
#14 (school*) NEAR (intervention* or program* or project* or promotion* or campaign*)
#15 #5 or #6 or #7 or #8 or #9 or #10 or #11 or #12 or #13 or #14
#16 #4 AND #15
[Note: in search line #1, MISC1 denotes the field in the record where the reference has been coded for condition, in this case, asthma]
Appendix 3. Supplementary database searches
Web of Science
TOPIC: (asthma*) AND TOPIC: (school* or teacher* or teaching*) AND TOPIC: (random*)
Refined by: TOPIC: (staff)
ClinicalTrials.gov
| Study type: | interventional |
| Condition: | asthma |
| Intervention | staff education |
Data and analyses
Comparison 1. Staff asthma education versus control.
| Outcome or subgroup title | No. of studies | No. of participants | Statistical method | Effect size |
|---|---|---|---|---|
| 1 Visits to ED/hospital (mean per child) | Other data | No numeric data | ||
| 2 Asthma control ‐ quality of life (PAQLQ) | 2 | Mean Difference (IV, Random, 95% CI) | Subtotals only | |
| 2.1 Main follow‐up (6 to 12 months) | 2 | 1005 | Mean Difference (IV, Random, 95% CI) | 0.14 [‐0.03, 0.31] |
| 2.2 24‐month follow‐up | 1 | 368 | Mean Difference (IV, Random, 95% CI) | ‐0.20 [‐0.52, 0.12] |
| 3 Adherence to asthma policies | 2 | Odds Ratio (M‐H, Random, 95% CI) | Subtotals only | |
| 3.1 Policy ownership | 2 | 57 | Odds Ratio (M‐H, Random, 95% CI) | 4.45 [1.38, 14.30] |
| 3.2 Improvement in measures to prevent attacks | 1 | 29 | Odds Ratio (M‐H, Random, 95% CI) | 9.33 [1.65, 52.68] |
| 3.3 Ability to administer salbutamol | 1 | 33 | Odds Ratio (M‐H, Random, 95% CI) | 20.22 [3.45, 118.65] |
| 4 Absenteeism related to asthma (mean per child) | Other data | No numeric data | ||
| 5 Staff preparedness ‐ asthma knowledge | 3 | 640 | Std. Mean Difference (IV, Random, 95% CI) | 0.74 [0.33, 1.16] |
1.5. Analysis.
Comparison 1 Staff asthma education versus control, Outcome 5 Staff preparedness ‐ asthma knowledge.
Characteristics of studies
Characteristics of included studies [ordered by study ID]
Bell 2000.
| Methods |
Study design: parallel cluster‐RCT Length of observation: 4 weeks Setting: 10 primary schools (5 matched pairs) in Northern Ireland, UK (English language) |
|
| Participants |
Population: 5 schools were randomised to receive the intervention (53 teachers; 36 had data at baseline and at follow‐up) and 5 to serve as the control group (60 teachers; 45 had data at baseline and at follow‐up) Age group: primary school Socioeconomic status: not reported Baseline characteristics No details about children. Study reports number of years teaching, age of class taught, number of children with asthma in class, previous training in asthma, personal or family/friends' diagnosis of asthma. A large proportion of the intervention group (91.7%) said they had received previous training in asthma (62.2% in control group) Inclusion criteria: teachers at randomly selected primary schools in Northern Ireland. 91 primary schools from a single Education Board were placed in matched pairs according to numbers of teachers, pupil numbers and locations (postal code). Schools were randomly assigned to control or intervention. 16 pairs of schools then were randomly selected and were asked to participate. 5 pairs (10 schools) agreed to participate Exclusion criteria: any school that had previously been asked to complete a questionnaire on asthma knowledge |
|
| Interventions |
Intervention Summary of content: “The training session provided information about the pathophysiology of asthma, symptoms and trigger factors of asthma, differences between reliever and preventer medication used in the treatment of the condition, inhaler devices, and action to be taken in an emergency” Number/duration of sessions: 1 session lasting approximately 30 to 40 minutes Delivered by/to: by a “project facilitator” (pharmacist) to all teaching staff Follow‐up: 4 weeks Control Teachers completed baseline and follow‐up questionnaires at 4 weeks. No training was given until after evaluation had taken place |
|
| Outcomes | Mean score on Newcastle Asthma Knowledge Questionnaire (NAKQ) at baseline visit and 4 weeks later | |
| Notes |
Trial registration: not reported Funding: not described Note: The study also reports results of the NAKQ sent to 73 out of 150 primary schools randomly selected in Northern Ireland. The intervention study is relevant to this review |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | The primary schools were all from one Education and Library Board. All schools were placed in matched pairs excluding those that had participated in the questionnaire portion of the study. After matching, schools were randomly put in control or intervention groups but details are not provided. Sixteen pairs of schools were then randomly telephoned to ask if they would participate; 5 pairs agreed |
| Allocation concealment (selection bias) | High risk | The method and order in which allocation and selection took place would not have controlled adequately for biased allocation to groups |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not possible for those delivering or receiving the intervention; this may have, intentionally or unintentionally, affected how participants and study staff in each group behaved. The risk is not necessarily high for all outcomes, so we considered the possible effect of performance bias separately for each outcome when applying GRADE |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | The main outcome measure was knowledge self‐reported on the Newcastle Asthma Knowledge Questionnaire (NAKQ), which might have been biased by teachers’ knowledge of the group to which they belonged |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 17/53 (32%) teachers in the intervention group and 15/60 (25%) teachers in the control group did not fill out the 4‐week questionnaire |
| Selective reporting (reporting bias) | Unclear risk | The NAKQ is reported fully, but the paper states that the attitudes questionnaire is not reported, and that no associated trial protocol or registration is available against which to check for other measured outcomes |
Bruzzese 2006.
| Methods |
Study design: parallel cluster‐RCT Length of observation: most outcomes at 12 months; telephone interviews at 24 months; absences at 2.5 years Setting: 44 schools in New York (English language) |
|
| Participants |
Population: Schools were randomised. 307 families were included in the intervention group and 284 in the control group. Dropout was 20.5% and 19.7% in intervention and control groups at 12 months and was 36.5% and 39.1% at 24 months Age group: kindergarten to grade 5, i.e. primary‐aged children up to age 11 Socioeconomic status: lower socioeconomic status population: “more than 50% of students receiving free lunch and more than 67% being ethnic minorities”…“chosen to ensure reaching low‐income ethnic minority families, the target of our intervention” Baseline characteristics Intervention: mean age 7.8 years (SD 1.5); % male 57.8; 47.4% Hispanic; 37.5% black; 20.7% white; 41.8% other, including biracial; 3.3 symptom days/wk; 2.5 night awakenings/2 wk Control: mean age 7.8 years (SD 1.4); % male 59.4; 48.2% Hispanic; 34.2% black; 20.6% white; 45.2% other, including biracial; 3.6 symptom days/wk; 3.2 night awakenings/2 wk Inclusion criteria: Eligible schools had “more than 50% of students receiving free lunch and more than 67% being ethnic minorities”…“chosen to ensure reaching low‐income ethnic minority families, the target of our intervention”. Eligible families were “those with a child diagnosed with asthma and symptoms of persistent asthma” according to NHLBI criteria. Children with prior persistent asthma diagnosis with 3 or more days of symptoms per week or night‐time awakening 3 or more times a month Exclusion criteria: not reported |
|
| Interventions |
Intervention Summary of content: 3‐day workshop for school health team to train teachers in a 45‐minute session. Additional training for primary care providers (PCPs), and preventive care activities with caregivers from nurses and physicians. The session delivered to teachers by the school health team covered asthma and their role in helping children manage asthma in school. Training by university staff and study physicians given to students' PCPs covered preventive therapy, communication, patient education and procedures for establishing medication plans in schools using the Physician Asthma Care Education (PACE) programme. Preventive care activities were given by nurses and physicians to caregivers of children with asthma, including assessing child asthma severity and needs, providing asthma education as needed, presenting sample treatment plans to PCPs, encouraging caregivers/PCPs to complete school medication forms when required and referring families for medical care when needed. Nurses also conveyed instructions from management plans to teachers School health team implemented preventive care with investigator support for 2 years via monthly visits from the nurse educator. An additional year of support was provided if needed to sustain the intervention Number/duration of sessions: single 3‐day workshop for school health team and one 45‐minute session for teachers plus ongoing monthly support from school health team Delivered by/to: by school health team (full‐time school nurse, school physician (2 days a month), public health assistant (2 to 3 days a week), schoolteacher or administrator and a parent) who were themselves trained by Columbia University staff. Delivered to teachers, primary care providers and students Follow‐up: 2 to 3 years Control Received intervention only after evaluation |
|
| Outcomes | By interview at 12 and 24 months: caregiver reports of frequency of daytime symptoms, night‐time awakening and days with activity limitation in the past 2 weeks and the past 6 months; urgent use of healthcare services and medication over the past year; caregiver PAQLQ School absences from records for baseline to 2.5 years post intervention Nurse logs of time spent on asthma‐related tasks |
|
| Notes |
Trial registration: not reported Funding: grant from National Heart Lung and Blood Institute (HL56348); W.T. Grant Foundation; Frances L & Edwin L Cummings Memorial Fund; New York Community Trust; United Hospital Fund; New York City Department of Health and Mental Hygiene Note: Open Airways for Schools (OAS) was delivered to NYC schools during this study, including those in the control group. “Approximately half of our sample met the age criteria to receive OAS. Participation levels in the intervention and control groups were comparable” |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | Method of sequence generation not described |
| Allocation concealment (selection bias) | High risk | “schools were paired by size and borough to control for potential borough differences. Schools were randomly assigned in each pair either to “intervention” or to “control” status; control schools received the intervention after the evaluation”. This method of pairing may have introduced an allocation bias |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not possible for those delivering or receiving the intervention, which may have, intentionally or unintentionally, affected how participants and study staff in each group behaved. The risk is not necessarily high for all outcomes, so we considered the possible effect of performance bias separately for each outcome when applying GRADE |
| Blinding of outcome assessment (detection bias) All outcomes | Low risk | “NERI, an independent research company blind to treatment status, conducted caregiver telephone interviews at baseline and at 12‐ and 24‐months post‐baseline” |
| Incomplete outcome data (attrition bias) All outcomes | High risk | 591 children were in the study at baseline ‐ 307 in the intervention arm and 284 in the control arm. The intervention arm provided data for 244 (79.5%) and 195 (63.5%) children at 12 and 24 months, respectively. The control group provided data for 228 (80.3%) and 173 (60.9%) children, respectively. Report states “We followed the intent‐to‐treat principle”. The level of retention over the 2 years was similar across groups and intent‐to‐treat analyses were performed, but the quantity of missing data (and hence the quantity that had to be imputed) was high, especially by 2 years (38% missing for caregivers;around the same for children) |
| Selective reporting (reporting bias) | Unclear risk | Named outcomes appear to be well reported at the time points described but no trial registration is available to check |
Henry 2004.
| Methods |
Study design: parallel cluster‐RCT Length of observation: 6 to 8 months Setting: 33 high schools in Newcastle, New South Wales, Australia (English language: predominantly Caucasian population with very few children from non‐English‐speaking backgrounds) |
|
| Participants |
Population: 16 schools (688 teachers) were randomised to the intervention and 17 schools to the control (416 teachers) Age group: high school, year 8. Aged 12 to 13 Socioeconomic status: not reported Baseline characteristics Intervention: % male 52.4; 23.7% met the definition for asthma Control: % male 52.9; 20.8% met the definition for asthma Age not reported, but all in year 8, so between 12 and 13 years of age; 42% of the asthma population across both groups had ever taken ICS and 22% were current smokers Inclusion criteria: state schools run by the Department of School Education, schools run by the Catholic Education Office and independent private schools. Targeted at year 8 students, i.e. those in their second year of high school education. Asthma was defined with the quality of life questionnaire Exclusion criteria: not reported |
|
| Interventions |
Intervention Summary of content: Three‐session Living With Asthma Package about asthma delivered to a school representative, who was then provided with the Living With Asthma teaching kit. Three‐session package designed to be taught within the Personal Development/Health/Physical Education (PD/H/PE) strand of the school curriculum. Full details of the package, developed as a joint exercise between school teachers and health professionals, are published here. Each intervention school was invited to send a representative to a 1‐day in‐service seminar. This covered health and educational principles of asthma education among adolescents, highlighting important features about asthma and its management and indicating the way in which the package was consistent with the educational principles espoused in the PD/H/PE curriculum Number/duration of sessions: 1 seminar followed by 3 in‐school teacher‐led sessions Delivered by/to: by “those who had been involved in the development of the package”, to a school representative at the seminar (then subsequently to teachers and students) Follow‐up: questionnaires were undertaken between 6 and 8 months after baseline data were collected. Five years later, in 1999, a questionnaire was sent to head teachers to ascertain whether the Living With Asthma programme was still being taught Control All schools were instructed that a community asthma educator could be contacted for assistance with staff training in management and policy development in the school setting. Control schools were offered the package and teacher training after the study |
|
| Outcomes | Follow‐up data were collected from students and teachers from August to October 1993 by questionnaire. In addition, we recorded requests for assistance from teachers. Baseline and follow‐up questionnaires measured asthma knowledge (Newcastle Asthma Knowledge Questionnaire, slightly modified for adolescents, score 0 to 31), attitudes, symptoms (based on internal locus of control model, 6‐point Likert scales for which higher scores represented stronger attitudes). Students with asthma additionally filled out a quality of life questionnaire (based on the Juniper AQLQ) and an 18‐item questionnaire concerning their personal history of asthma symptoms, use of asthma treatments and school absenteeism due to asthma. School requests for assistance were documented |
|
| Notes |
Trial registration: not reported Funding: National Health and Medical Research Council, Australia; Hunter Community Asthma Project Note: some outcomes reported for all participants rather than just for those who had asthma |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | "Schools were randomized to control or intervention, with an attempt to obtain similar demographic mixes in the two groups…" No details about the how the sequence was generated |
| Allocation concealment (selection bias) | High risk | “with an attempt to obtain similar demographic mixes in the two groups” suggests that allocation may not have been concealed in an attempt to keep the groups balanced for some confounding factors |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not possible for those delivering or receiving the intervention, which may have, intentionally or unintentionally, affected how participants and study staff in each group behaved. The risk is not necessarily high for all outcomes, so we considered the possible effect of performance bias separately for each outcome when applying GRADE |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Outcomes were collected via questionnaires filled in by teachers and students, and so could not be controlled for detection bias |
| Incomplete outcome data (attrition bias) All outcomes | High risk | "Complete questionnaires were returned by 4,161/4,475 (93%) of the year 8 students at baseline and by 3,837 at follow‐up. However, only 3,443 of the students (1,787 intervention; 1,656 control) were matched with their first survey. Thus 76.7% of all eligible students and 82.7% of students who were recruited into the initial phase contributed to the data analysis, with similar response rates in intervention and control adolescents” A lot of missing data for teachers: “Of the 1,815 teachers (688 intervention and 416 control), 1,104 (60.8%) completed asthma knowledge and attitudes questionnaires at baseline and 621 at follow‐up (310 intervention and 311 control). The consent process meant that many teachers completed the forms anonymously, and paired data were available for only 260 teachers from intervention schools and 225 from control schools” |
| Selective reporting (reporting bias) | Unclear risk | All named outcomes appear to be reported well, but no trial registration was cited against which we could check |
Kawafha 2015.
| Methods |
Study design: pre‐test/post‐test cluster‐RCT Length of observation: 3 months Setting: A cluster random sample was obtained from the entire public primary schools in the north of Jordan (Arabic language) |
|
| Participants |
Population: 40 teachers were randomised to the intervention group and 40 to the control group Age group: 6 to 12, i.e. primary Socioeconomic status: The areas were selected (Irbid, Jarash and Ajlon regions) for high population density and because they consisted of urban and rural populations with different socio‐economic status Baseline characteristics Intervention: mean age of teachers 36 (SE 0.89); all female Control: mean age of teachers 34 (SE 0.88); all female Paper specifically states that no children with asthma were included in the classes of teachers who participated in the study Inclusion criteria: teachers at public primary schools over 18 years of age who agreed to participate in the study. Schoolchildren were females from 6 to 12 years of age Exclusion criteria: teachers with asthma, teachers who attended an educational programme about asthma in the past and all non‐Jordonian nationality teachers |
|
| Interventions |
Intervention Summary of content: Education covered general information about asthma, etiology, pathophysiology, severity, signs and symptoms, asthma attacks, triggers, management of asthma (including how to use inhalers and treat symptoms) and asthma and sport. Teachers were then given CDs and pamphlets summarising the session content. Based on Smeltzer 2011 textbook Content was reviewed by 2 respiratory specialists Number/duration of sessions: 3 sessions (approximately 1 hour each) conducted in schools Delivered by/to: by primary researcher with nursing degree, trained by 2 respiratory specialists (lecture discussion and PowerPoint presentation). Delivered to primary school teachers. Follow‐up: after 1 week, and then 3 months later Control No intervention. Assessed at beginning and end |
|
| Outcomes | Structured questionnaire with demographic data and the Asthma General Knowledge Questionnaire for Adults (AGKQA – Allen and Jones 1998, 0 to 31, higher = better) | |
| Notes |
Trial registration: not reported Funding: “The author(s) received no financial support for the research, authorship, and/or publication of this article” Note: “None of the teachers had received an educational session or workshop about asthma in the past. All were Muslims and did not have asthma or family members with asthma. No children with asthma were in the classes of teachers in the selected sample" |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “The primary researcher generated the random allocation sequence, enrolled participants, and assigned participants to intervention” “Eighty teachers were randomly selected and were then randomly allocated either to the experimental or the control group to have 40 in each” Report describes a multi‐level sampling procedure but does not describe how the sequence was generated |
| Allocation concealment (selection bias) | High risk | “The primary researcher generated the random allocation sequence, enrolled participants, and assigned participants to intervention.” Slips of paper were used, and the same person completed all steps of randomisation, which may have introduced bias |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | Blinding was not possible for those delivering or receiving the intervention, which may have, intentionally or unintentionally, affected how participants and study staff in each group behaved “The teachers who completed the pre‐test did not know their group assignments, but the researcher knew the groups in which they were included. Teachers were made aware of their groups prior to the beginning of the education implementation." The risk is not necessarily high for all outcomes, so we considered the possible effect of performance bias separately for each outcome when applying GRADE |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Teachers filled in the questionnaires at the start and end of the study, which may have introduced detection bias “A code number was given to each teacher in both groups to mask their participation and keep their data confidential”. This likely would have at least masked the analysis of the data |
| Incomplete outcome data (attrition bias) All outcomes | Low risk | “Eighty teachers were randomly allocated either to the experimental or the control group to have 40 in each”. Abstract reports 36 and 38 in each arm, suggesting that 4 were not included in the experimental group (10%) and 2 were not included in the control group (5%) |
| Selective reporting (reporting bias) | Unclear risk | The study mentions only 1 outcome, which is reported at the 2 time points described. No associated protocol is available to check whether other outcomes were measured and not reported |
McCann 2006.
| Methods |
Study design: parallel cluster‐RCT Length of observation: 12 months Setting: 24 primary/junior schools in the south of England, UK (English language) |
|
| Participants |
Population: 12 schools (106 pupils with asthma) were randomised to the intervention group and 12 schools (113 pupils with asthma) to the control group Age group: primary – ages 7 to 9 (years 3 and 4) Socioeconomic status: No differences were found between NI and IV groups at baseline in markers of social deprivation (baseline info not available) Baseline characteristics Intervention: % male 52.8; 21.5% had at least 1 parent who smokes Control: % male 58.4; 30% had at least 1 parent who smokes All between 7 and 9 years of age Inclusion criteria: primary schools in the south of England. Families of children in years 3 and 4 were invited “on the basis of information relating to a current diagnosis of asthma, the use of asthma medication and symptoms of wheeze over a previous 12‐month period” Exclusion criteria: not reported |
|
| Interventions |
Intervention Summary of content: Nurse‐led intervention consisted of a staff training session (duration 45 minutes) and an asthma workshop for pupils (duration 45 minutes). A model asthma policy related to care and management of asthma was offered to schools based on examples used in previous studies [17] and the National Asthma Campaign information pack for schools [23], as well as further support and advice for writing of their own policies. The class teacher was present at nurse‐led pupil workshops In IV schools, these workshops focused on asthma as a cause of cough and wheeze, a description of the respiratory system consistent with the Science National Curriculum for pupils 7 to 9 years of age and what it feels like to have asthma and how to help a friend who is coughing and finding it difficult to breathe. The latter involved a role‐play with a school nurse as the teacher, in which the importance of taking the teacher to a coughing child, rather than the child to the teacher, was emphasised. Pupils with asthma were invited to participate as experts if they wished but were not compelled to do so Number/duration of sessions: 1 staff training session (45 minutes) and an asthma workshop for pupils (45 minutes) Delivered by/to: by a nurse to staff (teachers, lunchtime supervisors, caretakers and secretaries) and pupils in years 3 and 4 Follow‐up: children and staff followed up for 1 year Control Children (not teachers) in NI schools took part in a workshop (45 minutes) about the respiratory system and how the body defends itself against infection, also consistent with the National Curriculum. No mention was made of asthma during this NI workshop |
|
| Outcomes | School absences (primary), establishment of asthma policies and procedures, staff asthma knowledge, pupil asthma knowledge, prescribed medication according to BTS steps, asthma symptom reporting, quality of life, perceived self‐competence and self‐esteem | |
| Notes |
Trial registration: not reported Funding: National Health Service Research and Development (Project AM1/08/008) administered by the National Asthma Campaign (Asthma UK); Merck, Sharp & Dohme (UK) Ltd |
|
| Risk of bias | ||
| Bias | Authors' judgement | Support for judgement |
| Random sequence generation (selection bias) | Unclear risk | “Pairs of schools were matched on demographic characteristics and randomly assigned in pairs to the non‐intervention (NI) group and the intervention (IV) group” No description of the random sequence |
| Allocation concealment (selection bias) | High risk | Matching schools into pairs would not have allowed the sequence to be fully concealed |
| Blinding of participants and personnel (performance bias) All outcomes | High risk | It was not possible to blind participants and personnel to treatment assignment. The risk is not necessarily high for all outcomes, so we considered the possible effect of performance bias separately for each outcome when applying GRADE |
| Blinding of outcome assessment (detection bias) All outcomes | High risk | Most of the outcomes were self‐rating scales completed by staff and pupils who were aware of the group to which they belonged |
| Incomplete outcome data (attrition bias) All outcomes | High risk | “A total of 23 out of 24 (95.8%) schools completed the study (fig. 1). One school withdrew as the result of a change in head teacher. In total, 20 children moved out of the area and a further six children were withdrawn from the study because they or their school withdrew. A total of 193 out of 219 (88.1%) children with asthma completed the study” 13 children from each arm did not complete the study (12.3% and 11.5% for intervention and control groups, respectively), which is balanced “Absence data were available for 186 out of 193 (96.4%) study children with asthma” However, missing data were substantial for some outcomes, particularly staff asthma knowledge: “While 481 members of staff completed a questionnaire pre‐intervention, only 149 (31%) of these staff members completed post‐intervention questionnaires” |
| Selective reporting (reporting bias) | High risk | Data for several outcomes of interest to the review were not reported in a way that allowed them to be included in a meta‐analysis. The focus was on associations with treatment modifiers (e.g. sex, pet ownership, social deprivation) rather than on overall treatment effects versus the control group. Some outcomes were just reported, as “no effect of the intervention was found” (e.g. absence) |
AGKQA: Asthma General Knowledge Questionnaire for Adults
AQLQ: Asthma Quality of Life Questionnaire
BTS: British Thoracic Society
ICS: inhaled corticosteroid
IV: intervention
NAKQ: Newcastle Asthma Knowledge Questionnaire
NI: non‐intervention
PACE: Physician Asthma Care Education
PAQLQ: Paediatric Asthma Quality of Life Questionnaire
PCP: primary care physician
PD/H/PE: personal development/health/physical education
RCT: randomised controlled trial
SD: standard deviation
SE: standard error
Characteristics of excluded studies [ordered by study ID]
| Study | Reason for exclusion |
|---|---|
| Abdel Gawwad 2007 | Not an RCT ‐ pre‐post experimental research design. Summarised in discussion |
| Al‐Sheyab 2015 | Population does not match the inclusion criteria ‐ intervention aimed at school students, not staff |
| Bruzzese 2011 | Population does not match the inclusion criteria ‐ intervention aimed at school students with symptoms but no diagnosis of asthma (n = 30) |
| Bruzzese 2011a | Population and intervention do not match the inclusion criteria ‐ aimed at students and healthcare providers, not school staff |
| Bruzzese 2014 | Population and intervention do not match the inclusion criteria ‐ aimed at school students with symptoms but no diagnosis of asthma (n = 399) |
| Bush 2014 | Population does not match the inclusion criteria ‐ intervention aimed at school students, not staff, and publication is assessing the level of agreement between student and parent scores |
| Cicutto 2003 | Population does not match the inclusion criteria ‐ intervention aimed at students and parents, not staff |
| Cicutto 2013 | Population and intervention do not match the inclusion criteria ‐ focus of the intervention is the Roaring Adventure of Puff programme for students |
| Clark 2004 | Population and intervention do not match inclusion criteria ‐ main focus of the intervention was educating students rather than staff |
| Clark 2013 | Study design does not match the inclusion criteria ‐ not an intervention study |
| Francis 2000 | Intervention does not match the inclusion criteria ‐ offering an asthma review at school rather than at the GP surgery office |
| Gallefoss 1997 | Population does not match the inclusion criteria ‐ intervention aimed at students, not staff |
| Gerald 2006 | Population and intervention do not match inclusion criteria ‐ main focus of the intervention was educating students rather than staff |
| Gibson‐Young 2014 | Study design does not match the inclusion criteria ‐ survey, not RCT |
| Halterman 2012 | Population and intervention do not match inclusion criteria ‐ web‐based system for healthcare providers to monitor children in school, not aimed at educating staff |
| Hazell 1995 | Not an RCT ‐ teachers attended a seminar but were not randomised. Summarised in discussion |
| Henry 2006 | Not an intervention study ‐ national policy paper |
| Horspool 2013 | Population and intervention do not match the inclusion criteria ‐ aimed at parents to prevent exacerbations at school, not staff |
| Kintner 2009 | Population and intervention do not match the inclusion criteria ‐ aimed at students and parents, not school staff |
| Kintner 2015 | Population does not match the inclusion criteria ‐ aimed at students, and teachers participated in delivering the intervention rather than receiving it |
| Korta Murua 2012 | Study design does not match the inclusion criteria ‐ not an RCT. Described as a "before and after quasi‐experimental study". Summarised in discussion |
| McGhan 2000 | Population does not match the inclusion criteria ‐ aimed at students, not school staff |
| Monforte 2012 | Population does not match the inclusion criteria ‐ aimed at students, not school staff |
| Murray 2007 | Study design does not match the inclusion criteria ‐ systematic review |
| NCT00005736 | Design and intervention do not match the inclusion criteria ‐ observational study aimed primarily at children, with a lesser focus on parents, peers and school staff (unclear if the same study as NCT00005735) |
| NCT00304304 | Population does not match the inclusion criteria ‐ intervention primarily aimed at very young children 1 to 5 years of age, not at staff. Also cross‐over design |
| NCT01607749 | Population does not match the inclusion criteria ‐ intervention delivered through teachers to children, not for staff |
| Olympia 2005 | Study design does not match the inclusion criteria ‐ survey, not RCT |
| Perry 2015 | Population and intervention do not match the inclusion criteria ‐ asthma education delivered via telemedicine to children with asthma, their caregivers and school nurses as part of a comprehensive telemonitoring system in schools |
| Snow 2004 | Study design does not match the inclusion criteria ‐ inception cohort and historical controls |
| Soo 2013 | Study design does not match the inclusion criteria ‐ systematic review |
| Splett 2006 | Intervention does not match the inclusion criteria ‐ partnership between schools, healthcare providers and parents to improve adoption of asthma guidelines |
| Tapp 2011 | Intervention does not match the inclusion criteria ‐ the school‐based care arm does not mention specific training to be provided to staff, rather "an electronic data capture system to a robust CDC funded school‐based intervention to assist with evaluation and to link the school‐based care team with primary care providers" |
| Wong 2004 | Study design does not match the inclusion criteria ‐ survey, not RCT |
GP: general practitioner
RCT: randomised controlled trial
Differences between protocol and review
We were not able to carry out qualitative analysis as planned because information on the interventions provided was insufficient. We attempted to contact study authors to ask for more information, but they were unable to provide it, or we were not able to make contact. We were also unable to conduct some of the planned quantitative syntheses, particularly subgroup and sensitivity analyses, because usually only one or two studies reported each outcome; we have explained this in greater detail in the Effects of interventions section.
Contributions of authors
As planned in the protocol, KK screened all references, extracted data and assessed risk of bias for all studies. RC and TD shared duplication of these tasks, and all review authors contributed to final decisions about study inclusion. KK performed the meta‐analyses and led the write‐up, with support from all review authors.
Sources of support
Internal sources
-
Kayleigh M Kew, UK.
Supported by St George's, University of London
External sources
-
National Institute for Health Research, UK.
Evidence to guide care in adults and children with asthma, 13/89/14
This project was supported by the National Institute for Health Research (NIHR), via Cochrane Infrastructure, Cochrane Programme Grant or Cochrane Incentive funding to the Airways Group. The views and opinions expressed therein are those of the review authors and do not necessarily reflect those of the Systematic Reviews Programme, NIHR, NHS or the Department of Health.
Declarations of interest
Kayleigh Kew: none known.
Robin Carr: none that are relevant to the interventions considered in this review. I am a part‐time Partnership GP. I work as the long‐term conditions lead for the Oxfordshire Clinical Commissioning Group for respiratory illness and was the medical director of the Somerset COPD service until October 2014. I have received a salary from each of these employers. I have organised primary care education for over 20 years and have received honoraria from GSK, BI, AZ and Chiesi over the past 36 months for lectures presented to primary care staff. I received travel reimbursement for attending a Cochrane Airways Group meeting in 2014 and in 2015.
Tim Donovan: none known.
Morris Gordon: none that are relevant to the interventions considered in this review. I have received travel and educational grants from various companies over the past three years, including Ferring, Danone/Nutricia, Abbott, Biogaia and Clinova. None of these companies were involved in the planning, design, execution or write‐up of this review.
New
References
References to studies included in this review
Bell 2000 {published data only}
- Bell HM, McElnay JC, Hughes CM, Gleadhill I. Primary schoolteachers' knowledge of asthma: the impact of pharmacist intervention. Journal of Asthma 2000;37(7):545‐55. [0277‐0903] [DOI] [PubMed] [Google Scholar]
Bruzzese 2006 {published data only}
- Bruzzese JM, Evans D, Wiesemann S, Pinkett‐Heller M, Levison MJ, Du Y, et al. Using school staff to establish a preventive network of care to improve elementary school students' control of asthma. Journal of School Health 2006;76(6):307‐12. [0022‐4391] [DOI] [PubMed] [Google Scholar]
Henry 2004 {published data only}
- Henry RL, Gibson PG, Vimpani GV, Fanccis JL, Hazell J. Randomized controlled trial of a teacher‐led asthma education program. Pediatric Pulmonology 2004;38(6):434‐42. [DOI] [PubMed] [Google Scholar]
Kawafha 2015 {published data only}
- Kawafha MM, Tawalbeh LI. The effect of asthma education program on knowledge of school teachers: a randomized controlled trial. Western Journal of Nursing Research 2015;37(4):425‐40. [1552‐8456] [DOI] [PubMed] [Google Scholar]
McCann 2006 {published data only}
- McCann DC, McWhirter J, Coleman H, Calvert M, Warner JO. A controlled trial of a school‐based intervention to improve asthma management. European Respiratory Journal 2006;27(5):921‐8. [DOI] [PubMed] [Google Scholar]
- McWhirter J, McCann D, Coleman H, Calvert M, Warner J. Can schools promote the health of children with asthma?. Health Education Research 2008;23(6):917‐30. [0268‐1153] [DOI] [PubMed] [Google Scholar]
References to studies excluded from this review
Abdel Gawwad 2007 {published data only}
- Abdel Gawwad ESA, El‐Herishi S. Asthma education for school staff in Riyadh city: effectiveness of pamphlets as an educational tool. Journal of the Egyptian Public Health Association 2007;82(1‐2):147‐71. [PubMed] [Google Scholar]
Al‐Sheyab 2015 {published data only}
- Al‐Sheyab N, Alomari M, Shah S, Gallagher R. 'Class smoke‐free' pledge impacts on nicotine dependence in male adolescents: a cluster randomized controlled trial. Tropical Medicine & International Health 2015;20:255‐6. [Google Scholar]
Bruzzese 2011 {published data only}
- Bruzzese J‐M, Cespedes A, Kingston S, Sheares BJ, Sadeghi H, Su Z, et al. Feasibility and preliminary outcomes of a school‐based intervention for inner‐city, ethnic minority adolescents with undiagnosed asthma. Patient Education and Counseling 2011;85(2):290‐4. [0738‐3991] [DOI] [PMC free article] [PubMed] [Google Scholar]
Bruzzese 2011a {published data only}
- Bruzzese JM, Sheares BJ, Vincent EJ, Du Y, Sadeghi H, Levison MJ, et al. Effects of a school‐based intervention for urban adolescents with asthma. A controlled trial. American Journal of Respiratory and Critical Care Medicine 2011;183(8):998‐1006. [DOI] [PMC free article] [PubMed] [Google Scholar]
Bruzzese 2014 {published data only}
- Bruzzese JM, Cespedes A, Kingston S, Sheares BJ, Sadeghi H, Su Z, et al. Immediate efficacy of a school‐based intervention for urban adolescents with undiagnosed asthma: a randomized control trial (Abstract). American Journal of Respiratory and Critical Care Medicine 2014;189:A4022. [Google Scholar]
Bush 2014 {published data only}
- Bush JS, Waller JL, Ownby DR, TIngen MS. Do parents influence health literacy and impact asthma self‐management in rural Georgia high school students?. Annals of Allergy, Asthma & Immunology 2014;113(5):A20. [Google Scholar]
Cicutto 2003 {published data only}
- Cicutto L, Murphy S, Coutts D, O'Rourke J, Lang G, Chapman C, et al. Evaluating an elementary school based asthma education program: effects on quality of life and self efficacy [abstract]. American Thoracic Society 99th International Conference; 2003 May 16‐21; Seattle. 2003:C024 Poster 120.
Cicutto 2013 {published data only}
- Cicutto L, To T, Murphy S. A randomized controlled trial of a public health nurse‐delivered asthma program to elementary schools. Journal of School Health 2013;83(12):876‐84. [0022‐4391] [DOI] [PubMed] [Google Scholar]
- Cicutto L, To T, Murphy S. Cicutto, To, and Murphy respond: a randomized controlled trial of a public health nurse‐delivered asthma program to elementary schools... Kahan BC, Morris TP. The consequences of randomizing schools rather than children. Journal of School Health 2014; Vol. 84, issue 6:350. [0022‐4391] [DOI] [PubMed]
- Kahan BC, Morris TP. Letter: The consequences of randomizing schools rather than children... Cicutto L, To T, Murphy S. A randomized controlled trial of a public health nurse delivered asthma program to elementary schools. Journal of School Health 2014;84(6):349. [0022‐4391] [Google Scholar]
Clark 2004 {published data only}
- Controlling Asthma at School. https://clinicaltrials.gov/ct2/show/NCT00005735 (accessed 6 Sept 2016).
- Clark NM, Brown R, Joseph CL, Anderson EW, Liu M, Valerio MA. Effects of a comprehensive school‐based asthma program on symptoms, parent management, grades, and absenteeism. Chest 2004;125(5):1674‐9. [DOI] [PubMed] [Google Scholar]
Clark 2013 {published data only}
- Clark BR, Burkett SA, Andridge RR, Buckley TJ. Evidence of high rates of undiagnosed asthma in central Ohio elementary school children. Journal of School Health 2013;83(12):896‐906. [0022‐4391] [DOI] [PubMed] [Google Scholar]
Francis 2000 {published data only}
- Francis C. Asthma care in a school environment. Nursing Times 2000;96(37):43‐5. [0954‐7762] [PubMed] [Google Scholar]
Gallefoss 1997 {published data only}
- Gallefoss F, Bakke P, Kjaersgaard P. Effect of a randomized controlled asthma school intervention on consultation and hospitalization rates, days off work and their costs [abstract]. European Respiratory Journal 1997;10:421S. [Google Scholar]
Gerald 2006 {published data only}
- Gerald LB, Redden D, Wittich AR, Hains C, Turner‐Henson A, Hemstreet MP, et al. Outcomes for a comprehensive school‐based asthma management program. Journal of School Health 2006;76(6):291‐6. [0022‐4391] [DOI] [PMC free article] [PubMed] [Google Scholar]
Gibson‐Young 2014 {published data only}
- Gibson‐Young L, Martinasek MP, Clutter M, Forrest J. Are students with asthma at increased risk for being a victim of bullying in school or cyberspace? Findings from the 2011 Florida Youth Risk Behavior Survey. Journal of School Health 2014;84(7):429‐34. [0022‐4391] [DOI] [PubMed] [Google Scholar]
Halterman 2012 {published data only}
- Halterman J, Sauer J, Fagnano M, Montes G, Fisher S, Tremblay P, et al. Working toward a sustainable system of asthma care: development of the School‐Based Preventive Asthma Care Technology (SB‐PACT) trial. Journal of Asthma 2012;49(4):395‐400. [0277‐0903] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Halterman JS, Fagano M, Montes G, Fisher S, Tremblay P, Tajon R, et al. The school‐based preventive asthma care trial: results of a pilot study. Journal of Pediatrics 2012;161(6):1109‐15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noyes K, Bajorska A, Fisher S, Sauer J, Fagnano M, Halterman JS. Cost‐effectiveness of the School‐Based Asthma Therapy (SBAT) program. Pediatrics 2013;131(3):e709‐17. [DOI] [PMC free article] [PubMed] [Google Scholar]
Hazell 1995 {published data only}
- Hazell J, Henry RL, Francis JL, Halliday JA. Teacher initiated improvement of asthma policy in schools. Journal of Paediatrics and Child Health 1995;31(6):519‐22. [1440‐1754] [DOI] [PubMed] [Google Scholar]
Henry 2006 {published data only}
- Henry RL, Lough S, Mellis C, Australasian Paediatric Respiratory Group. National policy on asthma management for schools. Journal of Paediatrics and Child Health 2006;42(9):491‐5. [1440‐1754] [DOI] [PubMed] [Google Scholar]
Horspool 2013 {published data only}
- Horspool, MJ, Julious SA, Boote J, Bradburn MJ, Cooper CL, Davis S, et al. Preventing and lessening exacerbations of asthma in school‐age children associated with a new term (PLEASANT): study protocol for a cluster randomised control trial. Trials 2013;14(1):297. [DOI] [PMC free article] [PubMed] [Google Scholar]
Kintner 2009 {published data only}
- Kintner EK, Sikorskii A. Randomized clinical trial of a school‐based academic and counseling program for older school‐age students. Nursing Research 2009;58(5):321‐31. [1538‐9847] [DOI] [PMC free article] [PubMed] [Google Scholar]
Kintner 2015 {published data only}
- Kintner E, Cook G, Marti CN, Stoddard D, Gomes M, Harmon P, et al. Comparative effectiveness on cognitive asthma outcomes of the SHARP academic asthma health education and counseling program and a non‐academic program. Research in Nursing & Health 2015;38(6):423‐35. [1098‐240X] [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kintner EK, Cook G, Marti CN, Allen A, Stoddard D, Harmon P, et al. Effectiveness of a school‐ and community‐based academic asthma health education program on use of effective asthma self‐care behaviors in older school‐aged students. Journal for Specialists in Pediatric Nursing 2015;20(1):62‐75. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kintner EK, Cook G, Marti CN, Gomes M, Meeder L, Egeren LA. Effectiveness of a school‐based academic asthma health education and counseling program on fostering acceptance of asthma in older school‐age students with asthma. Journal for Specialists in Pediatric Nursing 2015; Vol. 20, issue 1:49‐61. [DOI] [PMC free article] [PubMed]
Korta Murua 2012 {published data only}
- Korta Murua J, Pérez‐Yarza EG, Pértega Díaz S, Aldasoro Ruiz A, Sardón Prado O, López‐Silvarrey Varela A, et al. [Impact of an asthma educational intervention programme on teachers]. Anales de Pediatria 2012;77(4):236‐46. [1695‐9531] [DOI] [PubMed] [Google Scholar]
McGhan 2000 {published data only}
- McGhan S, Jhangri G, Wells H, Wong E, Boechler V, Befus D, et al. Results of a controlled study of a school based asthma education program [abstract]. American Journal of Respiratory and Critical Care Medicine 2000;161(3):A903. [Google Scholar]
Monforte 2012 {published data only}
- Monforte SE, Gleason M, Covar R, Cicutto L, Szelfer SJ. Reducing health disparities for asthma with a school based asthma education program [Abstract]. Journal of Allergy and Clinical Immunology 2012;129(2):AB41 [156]. [Google Scholar]
Murray 2007 {published data only}
- Murray NG, Low BJ, Hollis C, Cross AW, Davis SM. Coordinated school health programs and academic achievement: a systematic review of the literature. Journal of School Health 2007;77(9):589‐600. [0022‐4391] [DOI] [PubMed] [Google Scholar]
NCT00005736 {published data only}
- Interventions to improve asthma management/prevention at school. https://clinicaltrials.gov/ct2/show/NCT00005736 (accessed 6 Sept 2016).
NCT00304304 {published data only}
- Community‐based asthma intervention in subsidized preschools. https://clinicaltrials.gov/show/NCT00304304 (accessed 6 Sept 2016).
NCT01607749 {published data only}
- Study for asthma education in primary schools. https://clinicaltrials.gov/show/NCT01607749 (accessed 6 Sept 2016).
Olympia 2005 {published data only}
- Olympia RP, Wan E, Avner JR. The preparedness of schools to respond to emergencies in children: a national survey of school nurses. Pediatrics 2005;116(6):e738‐45. [DOI] [PubMed] [Google Scholar]
Perry 2015 {published data only}
- Perry TT, Halterman JS, Brown RH, Hunter CR, Randle SM, Tilford JM, et al. Breath connection: a school‐based telemedicine program for rural children with asthma. Journal of Allergy and Clinical Immunology 2015;135(2):AB169. [Google Scholar]
Snow 2004 {published data only}
- Snow R, Kimball S, Ozuah PO. Helping teachers breathe easier: Improving asthma knowledge and competencies among elementary school teachers. Pediatric Research 2004;55(4):266A. [Google Scholar]
Soo 2013 {published data only}
- Soo YY, Saini B, Moles RJ. Can asthma education improve the treatment of acute asthma exacerbation in young children?. Journal of Paediatrics and Child Health 2013;49(5):353‐60. [1440‐1754] [DOI] [PubMed] [Google Scholar]
Splett 2006 {published data only}
- Splett PL, Erickson CD, Belseth SB, Jensen C. Evaluation and sustainability of the healthy learners asthma initiative. Journal of School Health 2006;76(6):276‐82. [0022‐4391] [DOI] [PubMed] [Google Scholar]
Tapp 2011 {published data only}
- Tapp H, Hebert L, Dulin M. Comparative effectiveness of asthma interventions within a practice based research network. BMC Health Services Research 2011;11:188. [1472‐6963] [DOI] [PMC free article] [PubMed] [Google Scholar]
Wong 2004 {published data only}
- Wong IC, Awolowo T, Gordon K, Mo YW. Survey of administration of medicines to pupils in primary schools within the London area. Archives of Disease in Childhood 2004;89(11):998‐1001. [DOI] [PMC free article] [PubMed] [Google Scholar]
Additional references
Asthma UK
- Asthma UK. Asthma at school. https://www.asthma.org.uk/advice/living‐with‐asthma/school/ (accessed 11 Feb 2016).
Bates 2004
- Bates R. A critical analysis of evaluation practice: the Kirkpatrick model and the principle of beneficence. Evaluation and Program Planning 2004;27(3):341‐7. [Google Scholar]
Baverstock 2010
- Baverstock M, Woodhall N, Maarman V. Do healthcare professionals have sufficient knowledge of inhaler techniques in order to educate their patients effectively in their use?. Thorax 2010;65:A117‐8. [Google Scholar]
BTS/SIGN 2014
- British Thoracic Society/Scottish Intercollegiate Guidelines Network. BTS/SIGN British guideline on the management of asthma, October 2014. www.brit‐thoracic.org.uk/guidelines‐and‐quality‐standards/asthma‐guideline/ (accessed 11 Feb 2016).
Cicutto 2014
- Cicutto L, Gleason M, Szefler SJ. Establishing school‐centred asthma programs. Journal of Allergy and Clinical Immunology 2014;134(6):1223‐30. [DOI] [PubMed] [Google Scholar]
Cochrane 1999
- Cochrane GM, Horne R, Chanez I. Compliance in asthma. Respiratory Medicine 1999;93:763‐9. [DOI] [PubMed] [Google Scholar]
Coffman 2009
- Coffman JM, Cabana MD, Yelin EH. Do school‐based asthma education programs improve self‐management and health outcomes?. Pediatrics 2009;124(2):729‐42. [DOI] [PMC free article] [PubMed] [Google Scholar]
Department for Health 2015
- Department for Health, UK. Supporting pupils at school with medical conditions: statutory guidance for governing bodies of maintained schools and proprietors of academies in England. https://www.gov.uk/government/uploads/system/uploads/attachment_data/file/484418/supporting‐pupils‐at‐school‐with‐medical‐conditions.pdf (accessed 19 Feb 2016).
Department of Health 2014
- Department of Health. Guidance: emergency asthma inhalers for use in schools. https://www.gov.uk/government/publications/emergency‐asthma‐inhalers‐for‐use‐in‐schools (accessed 11 Feb 2016).
Fowler 1992
- Fowler MG, Davenport MG, Garg R. School functioning of US children with asthma. Pediatrics 1992;90(6):939‐44. [PubMed] [Google Scholar]
GINA 2015
- Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention, Global Initiative for Asthma (GINA) 2015. www.ginasthma.org/ (accessed 11 Feb 2016).
Global Asthma Report 2014
- Global Asthma Network Steering Group. The Global Asthma Report 2014. http://www.globalasthmanetwork.org/publications/Global_Asthma_Report_2014.pdf (accessed 11 Feb 2016).
Gordon 2011
- Gordon M, Findley R. Educational interventions to improve handover in health care: a systematic review. Medical Education 2011;45(11):1081‐9. [DOI] [PubMed] [Google Scholar]
Gordon 2013
- Gordon M. Non‐technical skills training to enhance patient safety. The Clinical Teacher 2013;10:170‐5. [DOI] [PubMed] [Google Scholar]
GRADEpro GDT [Computer program]
- Brozek J, Oxman A, Schünemann H. GRADEpro GDT. Version accessed 14 March 2016. Hamilton (ON): GRADE Working Group, McMaster University, 2014.
Hanania 1994
- Hanania NA, Wittman R, Kesten S, Chapman KR. Medical personnel's knowledge of and ability to use inhaling devices. Metered‐dose inhalers, spacing chambers, and breath‐actuated dry powder inhalers. Chest 1994;105(1):111‐6. [DOI] [PubMed] [Google Scholar]
Higgins 2011
- Higgins JPT, Green S (editors). Cochrane Handbook for Systematic Reviews of Interventions Version 5.1 [updated March 2011]. The Cochrane Collaboration, 2011. www.cochrane‐handbook.org.
Hillemeier 2006
- Hillemeier MM, Gusic ME, Bai Y. Rural and urban children with asthma: are school health services meeting their needs?. Pediatrics 2006;118(3):1097‐103. [DOI] [PubMed] [Google Scholar]
Jaramillo 2015
- Jaramillo Y, Reznik M. Do United States' teachers know and adhere to the national guidelines on asthma management in the classroom? A systematic review. Scientific World Journal 2015;Article ID 624828:epub 2015. [DOI] [PMC free article] [PubMed] [Google Scholar]
Martinez 2008
- Martinez FD. Trends in asthma prevalence, admission rates, and asthma deaths. Respiratory Care 2008;53(5):561‐5. [PubMed] [Google Scholar]
Meng 2012
- Meng MY, Babey SH, Wolstein J. Asthma related school absenteeism and school concentration of low income students in California. Preventing Chronic Disease 2012;9:E98. [DOI] [PMC free article] [PubMed] [Google Scholar]
Moher 2009
- Moher D, Liberati A, Tetzlaff J, Altman D. Preferred reporting items for systematic reviews and meta‐analyses: the PRISMA statement. PLoS Medicine 2009;6(7):e1000097. [DOI: 10.1371/journal.pmed.1000097] [DOI] [PMC free article] [PubMed] [Google Scholar]
Murphy 2006
- Murphy KR, Hopp RJ, Kittelson EB, Hansen G, Windle ML, Walburn JN. Life‐threatening asthma and anaphylaxis in schools: a treatment model for school‐based programs. Annals of Allergy, Asthma & Immunology 2006;96(3):398‐405. [DOI] [PubMed] [Google Scholar]
NAEPP 2014
- National Asthma Education and Prevention Program, National Heart, Lung and Blood Institute. Managing Asthma: A Guide for Schools. http://www.nhlbi.nih.gov/files/docs/resources/lung/NACI_ManagingAsthma‐508%20FINAL.pdf (accessed 26 May 2016).
Norcini 2011
- Norcini J, Anderson B, Bollela V, Burch V, Costa MJ, Duvivier R, et al. Criteria for good assessment: consensus statement and recommendations from the Ottawa 2010 conference. Medical Teacher 2011;33(3):206‐14. [DOI] [PubMed] [Google Scholar]
NRAD 2015
- National Review of Asthma Deaths. Why asthma still kills. https://www.rcplondon.ac.uk/projects/outputs/why‐asthma‐still‐kills (accessed 11 Feb 2016).
RevMan 2014 [Computer program]
- The Nordic Cochrane Centre, The Cochrane Collaboration. Review Manager (RevMan). Version 5.3. Copenhagen: The Nordic Cochrane Centre, The Cochrane Collaboration, 2014.
Reznik 2015
- Reznik M, Bauman LJ, Okelo SO, Halterman JS. Asthma identification and medication administration forms in New York City schools. Annals of Allergy, Asthma and Immunology 2015;114(1):67‐8. [DOI] [PMC free article] [PubMed] [Google Scholar]
Ring 2015
- Ring N, Booth H, Wilson C, Hoskins G, Pinnock H, Sheikh A, et al. The 'vicious cycle' of personalised asthma action plan implementation in primary care: a qualitative study of patients and health professionals' views. BMC Family Practice 2015;16(145):[epub]. [DOI] [PMC free article] [PubMed] [Google Scholar]
Smeltzer 2011
- Smeltzer S, Bare B, Hinkle J, Cheever K. Brunner and Suddarth's Textbook of Medical Surgical Nursing. 12th Edition. Baltimore, MD: Lippincott Williams & Wilkins, 2011. [Google Scholar]
Williams 1998
- Williams MV, Baker DW, Honig EG, Lee TM, Nowlan A. Inadequate literacy is a barrier to asthma knowledge and self‐care. Chest 1998;114(4):1008‐15. [DOI] [PubMed] [Google Scholar]
Wu 1998
- Wu F, Hill J. An allergy and asthma educational outreach program for school nurses and staff. Allergy and Asthma Proceedings 1998;19(5):307‐10. [DOI] [PubMed] [Google Scholar]
References to other published versions of this review
Kew 2016
- Kew KM, Carr R, Donovan T, Gordon M. Asthma education for school staff. Cochrane Database of Systematic Reviews 2016, Issue 6. [DOI: 10.1002/14651858.CD012255] [DOI] [PMC free article] [PubMed] [Google Scholar]


