Abstract
Objective
In this study, we aimed to determine the success rate of nasoenteric tube (NET) insertion into the postpyloric area using ultrasonography (USG) and compare with the commonly used method direct abdominal graphy.
Methods
A single anaesthesiologist placed all the NETs. The NET was visualised by two radiologists simultaneously using USG. The localisation of the tube was confirmed using an abdominal graph in all patients.
Results
The blind bedside method was used for NET insertion into 34 patients. Eleven of the tubes were detected passing through the postpyloric area using USG. In one case, the NET could not be visualised in the postpyloric area using USG; however, it was detected in the postpyloric area through control abdominal radiography. In 22 patients, NETs were detected in the stomach using control abdominal radiography. The rate of imaging post pyloric using USG was 91.6%. When all cases were considered, catheter localisation was detected accurately using USG by 97% (33 in 34 patients).
Conclusion
USG is a reliable and practical alternative to radiography, which can be used to detect localisation of the nasogastric tube and NET.
Keywords: Nasoenteric tube, ultrasonography, radiography, enteral feeding, aspiration
Introduction
Enteral feeding may be maintained via the nasogastric tube (NGT) or nasoenteric tube (NET) for patients in the intensive care unit who are incapable of oral feeding (1–5).
There are many techniques for NET placement, such as blind bedside technique, air insuflation technique, metoclopramid and erythromycin treatment for motility stimulation, observing electromyography (EMG) signals and electromagnetic signals. The first-applied and best-known method is the blinding NET application. The success rates of the application vary significantly by the clinic (6–13). In addition, the classic endoscopy can be placed with transnasal endoscopy or fluoroscopy; however, it requires the equipment and trained personnel (14–16).
In association with the NET inserted for enteral feeding, some complications such as oesophagus, gastric and duodenal perforation; epistaxis; sinusitis; otitis media; and tracheobronchial trauma have been reported (3–6, 17, 18). The incorrect localisation of the NET and reflux-associated pulmonary aspiration is an important complication. It is important to determine the localisation of the distal end after the installation of the NET to avoid the complications (3–6).
The NET can be auscultated over the stomach by aerating after the placement; however, auscultation was shown to not be sufficiently safe due to the reverberation of sound in pulmonary-localised tube cases. The examination of the liquid withdrawn from the NET end may not always provide accurate results due to the antihistaminic medications used by patients (2–5).
Presently, ultrasonography (USG) has an extensive usage in intensive care units for both interventional medical practice and the examination of the thorax and abdomen. Detecting the location of the NET using abdominal radiography before starting enteral feeding is recommended in the current guidelines (2–5).
The detection of the position of the NET can be conducted by radiologists or experienced staff of the intensive care unit with a bedside USG, which is a noninvasive and radiation-free technique.
The aim of this study was to show the usability of the bedside USG for detecting the location of the NET in the intensive care unit patients as an alternative to abdominal radiography.
Methods
After obtaining approval of the Clinical Research Ethics Committee of Erciyes University University (21.03.2014 Decision No. 2014/186), the patients having the indication of NET placement in the Intensive Care for Adults, Ahi Evran University Education and Research Hospital were included in the study for enteral feeding. Written informed consent was obtained from the parents of the patients who participated in this study.
Nasoenteric tubes were installed by the same anaesthesiologist using the blind bedside method. No motive drug was used. The polyurethane was lubricated by applying the gel outside the weightless 8F NET (Bexen, Spain) and inside the guide wire and entered via the open nostril. After detection of the xiphoid distance between the mouth and the antitragus, the NET was advanced at least along this distance, and subsequently after hearing the voice on auscultation by aerating from the tube, it was advanced an additional 20–30 cm. The guide wire in the NET was extracted. Its location between the auscultation and the abdomen was confirmed by aerating from the catheter lumen. Thereafter, it was assessed simultaneously by the same two radiologists if the NET in the patient set to the supine position again with the aid of M5 portable USG (Mindray, PRC) device, 3,5 MHz convex probe and 7,5 MHz linear probe. The antropyloric area was detected on the head of the pancreas and choledochus. It was assessed in the axial, oblique axial and sagittal plane. The double linear echogenic foci (rail-like lines) having continuity in was based for the catheter detection in the antropyloric area. It was confirmed by real-time examination if a double linear echogenic focus is bound up to the catheter by giving 5 mL saline solutions to the NET lumen. The localisation of the NET in all patients was confirmed using abdominal radiography. The rate at which the NETs passed to the post pyloric area during the first placement and incorrect placements were recorded; the results were compared with that of abdominal radiography.
Results
In our study, the age of patients varied between 16 and 88 years, and the average age was 74.02±16.1 years. Seventeen patients were males and 17 females. Demographic data of the patients and their numbers by the reason for hospitalisation in intensive care are provided in Table 1. The NET was placed into 34 patients in our study using the blind bedside method. No NET was observed in antropyloric zone in USGs of 22 patients. It was detected in USG that these 22 patients had tubes in their stomachs. They were confirmed to be in the stomach in control graphs (Figure 1). It was detected that 11 of NETs we inserted were post pyloric with USG. Post pyloric NET USG images are provided in Figures 2 and 3. Although NET localisation could not be visualised post pyloric with USG in only one patient, it was found to be located post pylorically. The success rate of inserting the NET using the blind bedside method was 35%, and the rate of imaging post pyloric using USG was 91.6%. When all cases were considered, catheter localisation was detected correct with USG by 97% (33 in 34 patients).
Table 1.
Distribution of patients by their demographic data and reasons for hospitalisation in intensive care
| Age average, years | 74.02±16.1 |
| Gender (male/female) | 17/17 |
| Distribution of patients by diseases | Number |
| Cerebrovascular disease | 10 |
| Chronic obstructive disease and pneumonia | 8 |
| Traumatic intracranial bleeding | 5 |
| Renal failure | 5 |
| Heart failure | 2 |
| Sepsis | 2 |
| Liver failure | 1 |
| Status epilepticus | 1 |
Figure 1.

Control graphs
Figure 2.
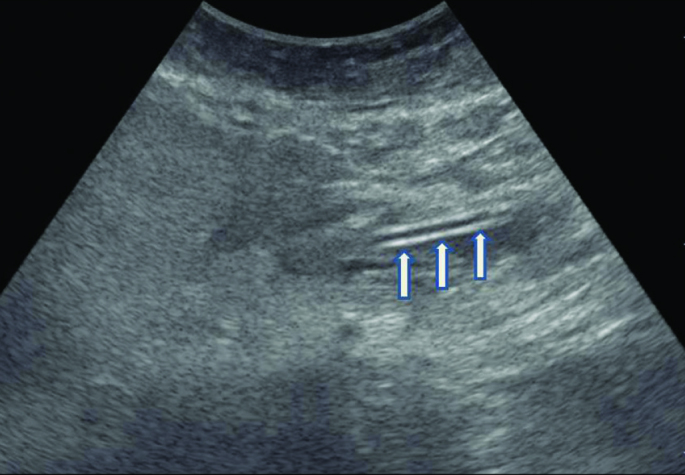
NET that forms double linear echogenic view is observed in the examination carried out with 3.5 MHz convex probe
Figure 3.

Axial section view of the NET is observed with 7.5 MHz linear probe
Discussion
Despite the fact that the well-known and preferred method is the blind bedside method, some techniques have been defined for the placement of the NET. Success rates with NET insertion are evaluated according to the post pyloric passage. The success rate of the blinding method is less compared to others. In literature, the blinding method success rates vary between 15% and 67% depending on the tube type (weighted-weightless) and use or nonuse of motility-enhancing medicine (6–8, 18, 19). In our study, we used weightless tubes and did not use motility-enhancing medicine considering the use of medications by patients in large quantities.
In the study by Hernandez-Socorro et al. (8) in which the NET was inserted accompanied with sonography, post pyloric insertion success rate was 84.6% in the USG group and 25.7% in the blinding technique group. The real-time examination during NET insertion was not performed in our study. We performed the examination on the same day following NET insertion. The success rate of the blinding technique was 35% in our study and is similar to that reported in literature.
Although there are some studies indicating that the auscultation, the following of pH, and colorimetric capnometry are successful techniques for detecting NET location, there are some restrictions (20–22).
Thus, the primarily preferred method for detecting localisation of NGT or NET is a standing direct abdominal radiograph. Endoscopy, fluoroscopy and USG are used for detecting localisation during or following insertion of the NET. The patient and intensive care personnel are subject to X-ray in bedside radiography and fluoroscopy implementation. Endoscopic implementation is not always practical and easily accessible method since it requires experienced personnel and equipment (23). USG is a practical method that does not involve X-ray and is cheap, easily accessible and repeatable. Moreover, it is more advantageous for real-time imaging compared to the USG radiography. USG must be preferred primarily since pregnant women and children are more sensitive to radiation. It is the disadvantage of sonography that obesity and abdomen gas distension limit imaging.
In our study, USG examination was performed after NET insertion and prior to radiography. Double linear echogenic view that extended to the post pyloric area and displayed continuity in the antropyloric area was evaluated as catheter. In a study that used USG for detecting NGT localisation, USG sensitivity was 97% (24). In our study, USG was found successful at a rate of 97% in detecting catheter localisation when all cases were considered. The rate of post pyloric imaging was 91.6%. One of 12 catheters extending to the post pyloric area could not be detected using ultrasound due to intensive gas distension in the patient. It was seen that the NET was located in the post pyloric area in radiography. In detecting localisation, the success rate with USG was close to that of radiography and complied with the literature. Radiography may be preferred in abdomen gas and obesity phenomena in which the antropyloric area cannot be visualised sufficiently.
The USG and X-ray techniques for detecting the location of the NGT tube was compared in a study by Kim et al. (25) they found high detection rates with USG, as in our study. No study regarding the USG technique for detecting the NET location has been found in the literature.
Study limitations
The planned case numbers could not be reached because of repair in the intensive care unit during the ethical board approval of the study. Therefore, this study can be considered a preliminary observational study. The blind bedside technique for the placement of NET is another limitation of this study. The placement rate is low in our study as in other studies in the literature using this technique. The objective of this study was to verify the placement of the NET at the bedside by the staff of intensive care units. The staff of the intensive care unit was experienced regarding the usage of USG for interventional medical practice and imaging of the thorax. However, they were inexperienced regarding abdominal USG. Hence, two radiologists were included to provide abdominal USG training support.
Conclusion
The detection of the NET location using USG requires appropriate training and experience. Detecting the location of NGT and NET tubes through bedside USG can be achieved by the intensive care unit staff after an education period of abdominal USG.
We concluded that USG is a noninvasive method that has no risk for radiation, a reliable option to detect NET localisation, and can be used bedside practically. Studies that are more comprehensive should be conducted to evaluate the success rate of USG, excluding the status, such as obesity and distension, which limit the usage of USG.
Footnotes
Ethics Committee Approval: Ethics committee approval was received for this study from the ethics committee of Erciyes University School of Medicine (No: 2014/186).
Informed Consent: Written informed consent was obtained from the parents of the patients who participated in this study.
Peer-review: Externally peer-reviewed.
Author Contributions: Concept – R.D.; Design – R.D., H.B., Y.D.; Supervision – R.D., Y.D., T.T.T.; Resources – R.D., H.B., Z.A.E.; Materials – R.D., Y.D.; Data Collection and/or Processing – R.D., Z.A.E., T.T.T.; Analysis and/or Interpretation – R.D., H.B., Y.D., T.T.T., Z.A.E.; Literature Search – R.D., T.T.T.; Writing Manuscript – R.D., Y.D.; Critical Review – R.D., H.B., Y.D., T.T.T., Z.A.E.; Other – R.D., Y.D., Z.A.E.
Conflict of Interest: No conflict of interest was declared by the authors.
Financial Disclosure: The authors declared that this study has received no financial support.
References
- 1.Marik PE, Zaloga GP. Early enteral nutrition in acutely ill patients: a systematic review. Crit Care Med. 2001;29:1495–501. doi: 10.1097/00003246-200112000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Stroud M, Duncan H, Nightingale J. Guidelines for enteral feeding in adult hospital patients. Gut. 2003;52(Suppl VII):vii1–vii12. doi: 10.1136/gut.52.suppl_7.vii1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kreymann KG, Berger MM, Deutz NEP, Hiesmayr M, Jolliet P, Kazandjiev G, et al. ESPEN Guidelines on Enteral Nutrition:Intensive care. Clin Nutr. 2006;25:210–23. doi: 10.1016/j.clnu.2006.01.021. https://doi.org/10.1016/j.clnu.2006.01.021. [DOI] [PubMed] [Google Scholar]
- 4.Bankhead R, Boullata J, Brantley S, Corkins M, Guanter P, Krenitsky J, et al. ASPEN Board of directors. Enteral Nutrition Practice Recommendations. J Parenter Enteral Nutr. 2009;33:122–67. doi: 10.1177/0148607108330314. https://doi.org/10.1177/0148607108330314. [DOI] [PubMed] [Google Scholar]
- 5.Kabaçam G, Özden A. Enteral Tüple Beslenme. Güncel Gastroenteroloji. 2009;13:201–10. [Google Scholar]
- 6.Kirby DF, Delegge MH, Fleming CR. American Gastroenterological Association Technical Review on Tube Feeding for Enteral Nutrition. Gasrtoenterology. 1995;108:1282–301. doi: 10.1016/0016-5085(95)90231-7. https://doi.org/10.1016/0016-5085(95)90231-7. [DOI] [PubMed] [Google Scholar]
- 7.Zaloga GP. Bedside method for placing small bowel feeding tubes in critically ill patients. A prospective study. Chest. 1991;100:1643–6. doi: 10.1378/chest.100.6.1643. [DOI] [PubMed] [Google Scholar]
- 8.Hernandez-Socorro CR, Marin J, Ruiz-Santana S, Santana L, Manzano JL. Bedside sonographic-guided versus blind nasoenteric feeding tube placement in critically ill patients. Crit Care Made. 1996;24:1690–4. doi: 10.1097/00003246-199610000-00015. https://doi.org/10.1097/00003246-199610000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Rees RG, Payne-James JJ, King C, Silk DB. Spontaneous transpyloric passage and performance of ‘fine bore’ polyuretane feeding tubes: a controlled clinical trial. JPEN J Parenter Enteral Nutr. 1988;12:469–72. doi: 10.1177/0148607188012005469. https://doi.org/10.1177/0148607188012005469. [DOI] [PubMed] [Google Scholar]
- 10.Lord LM, Weiser-Maimone A, Pulhamus M, Sax HC. Comparison of weighted vs unweighted enteral feeding tubes for efficacy of transpyloric intubation. JPEN J Parenter Enteral Nutr. 1993;17:271–3. doi: 10.1177/0148607193017003271. https://doi.org/10.1177/0148607193017003271. [DOI] [PubMed] [Google Scholar]
- 11.Paz HL, Weinar M, Sherman MS. Motility agents for the placement of weighted and unweighted feeding tubes in critically ill patients. Intensive Care Med. 1996;22:301–4. doi: 10.1007/BF01700450. https://doi.org/10.1007/BF01700450. [DOI] [PubMed] [Google Scholar]
- 12.Gabriel SA, Ackermann RJ, Castresana MR. A new technique for placement of nasoenteral feeding tubes using external magnetic guidance. Crit Care Med. 1997;25:641–5. doi: 10.1097/00003246-199704000-00014. https://doi.org/10.1097/00003246-199704000-00014. [DOI] [PubMed] [Google Scholar]
- 13.Keidan I, Gallagher TJ. Electrocardiogram-guided placement of enteral feeding tubes. Crit Care Med. 2000;28:2631–3. doi: 10.1097/00003246-200007000-00075. https://doi.org/10.1097/00003246-200007000-00075. [DOI] [PubMed] [Google Scholar]
- 14.Lorenzo-Zuniga V, Moreno de Vega V, Moreno P, Muchard J, Boix J. Endoscopic placement of postpyloric nasoenteric feeding tubes: The importance of the guidewire used. Clin Nutr. 2009;28:355–6. doi: 10.1016/j.clnu.2009.02.009. https://doi.org/10.1016/j.clnu.2009.02.009. [DOI] [PubMed] [Google Scholar]
- 15.Hashimoto A, Oya M, Iwano M, Fuse C, Inoue T, Yamada T, et al. A secure “double-check” technique of bedside post pyloric feeding tube placement using transnasal endoscopy. J Clin Biochem Nutr. 2012;51:213–5. doi: 10.3164/jcbn.12-35. https://doi.org/10.3164/jcbn.12-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hillard AE, Waddel JJ, Metzler MH, McAlpin D. Fluoroscopically guided nasoenteric feeding tube placement versus bedside placement. South Med J. 1995;88:425–8. doi: 10.1097/00007611-199504000-00008. https://doi.org/10.1097/00007611-199504000-00008. [DOI] [PubMed] [Google Scholar]
- 17.Kaufman JP, Hughes WB, Kerstein MD. Pneumothorax after nasoenteral feeding tube placement. Am Surg. 2001;67:772–3. [PubMed] [Google Scholar]
- 18.Marik PE, Zaloga GP. Gastric versus post-pyloric feeding: a systematic review. Crit Care Med. 2003;7:46–51. doi: 10.1186/cc2190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Huerta G, Puri VK. Nasogastric Versus Feeding Tubes in Critically Ill Patients. Nutrition. 2000;16:264–7. doi: 10.1016/s0899-9007(99)00307-x. https://doi.org/10.1016/S0899-9007(99)00307-X. [DOI] [PubMed] [Google Scholar]
- 20.Erzincanli S, Zaybak A, Güler A. Investigation of the efficacy of colorimetric capnometry method used to verify the correct placement of the nasogastric tube. Intensive and Critical Care Nursing. 2017;38:46–52. doi: 10.1016/j.iccn.2016.08.005. https://doi.org/10.1016/j.iccn.2016.08.005. [DOI] [PubMed] [Google Scholar]
- 21.Stock A, Gilbertson H, Babl FE. Confirming nasogastric tube position in the emergency department: pH testing is reliable. Pediatr Emerg Care. 2008;24:805–9. doi: 10.1097/PEC.0b013e31818eb2d1. https://doi.org/10.1097/PEC.0b013e31818eb2d1. [DOI] [PubMed] [Google Scholar]
- 22.Muslu B, Demircioglu RI, Gozdemir M, Usta B. Comparison of neck ultrasonography with a pH meter to confirm correct position of nasogastric tube. Clin Invest Med. 2016;39:27520. [PubMed] [Google Scholar]
- 23.Fang JC, Hilden K, Holubkov R, DiSario JA. Transnasal endoscopy vs fluoroscopy for the placement of nasoenteric feeding tubes in critically ill patients. Gasrointest Endosc. 2005;62:661–6. doi: 10.1016/j.gie.2005.04.027. https://doi.org/10.1016/j.gie.2005.04.027. [DOI] [PubMed] [Google Scholar]
- 24.Vigneau C, Baudel JL, Guidet B, Offenstadt G, Maury E. Sonography as an alternative to radiography for nasogastric feeding tube location. Intensive Care Med. 2005;31:1570–2. doi: 10.1007/s00134-005-2791-1. https://doi.org/10.1007/s00134-005-2791-1. [DOI] [PubMed] [Google Scholar]
- 25.Kim HM, So BH, Jeong WJ, Choi SM, Park KN. The effectiveness of ultrasonography in verifying the placement of a nasogastric tube in patients with low consciousness at an emergency center. Scand J Trauma Resusc Emerg Med. 2012;20:38. doi: 10.1186/1757-7241-20-38. https://doi.org/10.1186/1757-7241-20-38. [DOI] [PMC free article] [PubMed] [Google Scholar]


