Abstract
Background:
More and more studies conduct to compare intramedullary fixation (IMF) with arthroplasty in treating intertrochanteric hip fractures, but it remains controversy. The aim of this meta-analysis was to find out whether IMF or arthroplasty was more appropriate for treating intertrochanteric hip fractures in elderly patients.
Methods:
Relevant studies were searched in the electronic databases of PubMed, Embase, and The Cochrane Central Register of Controlled Trials from January 1980 to September 2016 with English language restriction. Surgical information and postoperative outcomes were analyzed using RevMan 5.3 version.
Results:
A total of 1239 patients from 11 studies which satisfied the eligibility criteria were included. Compared with IMF, the use of arthroplasty reduced implant-related complications (odds ratio [OR]: 2.05, P = .02) and reoperation rate (OR: 7.06, P < .001), and had similar length of hospital stay (weighted mean difference [WMD]: −0.41, P = .63). However, IMF reduced blood loss (WMD: −375.01, P = .001) and transfusion requirement (OR: 0.07, P < .001), shorter operation time (WMD: −18.92, P = .010), higher Harris hip score (WMD: 4.19, P < .001), and lower rate of 1-year mortality (OR: 0.67, P = .02) compared with arthroplasty.
Conclusion:
The main treatment of intertrochanteric hip fractures is internal fixation using IMF. In the absence of concrete evidence, arthroplasty should be undertaken with caution in carefully selected patient and surgeon should be aware of the increased complexity of doing the arthroplasty in these elderly patients. Further high-quality randomized controlled trials (RCTs) are needed to provide robust evidence and evaluate the treatment options.
Keywords: arthroplasty, intertrochanteric hip fractures, intramedullary fixation, meta-analysis
1. Introduction
The morbidity of intertrochanteric hip fractures is displaying a rising trend.[1] Surgical treatment with rigid fixation, which allows early mobilization and reduces complications, has gradually become preferred.[2] Extramedullary fixations have been the standard internal fixation in treating trochanteric fractures.[3] However, when compared with the intramedullary implants, it has a nonnegligible biomechanical disadvantage especially for unstable fractures.[4] Therefore, intramedullary fixations (IMF) become the most commonly used internal device for intertrochanteric fractures.[5] But, internal fixation may fail, particularly in unstable frail fractures. This has led some surgeons to try hip arthroplasty as a primary option in treating intertrochanteric hip fractures. Many reports in the literature consider that prosthetic replacement is the preferred treatment for selected unstable comminuted intertrochanteric fractures in the elderly.[6,7]
Several randomized controlled trials (RCTs) and non-RCTs have been conducted to compare IMF with arthroplasty in treating intertrochanteric hip fractures. However, no consensus has been reached regarding which one leads to superior results and better clinical outcomes. Hence, the purpose of this meta-analysis is to evaluate the evidence from the RCT and non-RCT studies that have compared the safety and efficacy of IMF and arthroplasty for treating patients with intertrochanteric hip fractures.
2. Materials and methods
2.1. Search strategy
In order to aggregate all of the relevant published studies, Preferred Reporting Items for Systematic Reviews and Meta-Analyses-compliant searches were used for all peer-reviewed studies published from January1980 to September 2016 that compared IMF with arthroplasty for treating intertrochanteric hip fractures. We conducted a literature search in PubMed, Embase, and The Cochrane Central Register of Controlled Trials using the following keywords: intertrochanteric, or pertrochanteric, or trochanteric, or extracapsular hip fractures; intramedullary fixation, or cephalomedullary nail; and hip arthroplasty, or hip replacement, or endoprothesis. The “related article” function was also used during the search; the references for retrieved articles were manually searched to avoid initial misses.
2.2. Inclusion and exclusion criteria
Included studies had to fulfill the following inclusion criteria: studies were designed as interventional studies (RCTs or non-RCTs); comparison of IMF with arthroplasty techniques in patients treated for intertrochanteric hip fractures; patients older than 60 years; and the articles were restricted to the English language.
Exclusion criteria: type of literature as a “review” and “digest,” “talk,” “letters,” “commentary,” and “case report”; cadaver or model studies; data were duplicated or overlapped; and patients had a metastasis or myeloma, infection, or congenital deformity.
2.3. Data extraction
All the titles and abstracts of the relevant studies were first independently categorized by 2 reviewers, and then the full-text articles that met the eligibility criteria were read and selected for inclusion. Whenever necessary, we contacted the authors of the articles to obtain missing data or further information. The detailed data included the title, year of publication, design of study, sample size, age and sex of participants, blinding method, surgical procedures, types of fixation implants, duration of follow-up, and outcome parameters.
2.4. Quality assessment
We assessed the risk of bias of RCTs using a modified version of the Cochrane Collaboration's tool.[8] Other non-RCTs were assessed with the Methodological Index for Nonrandomized Studies.[9] According to the Cochrane Collaboration recommendations, the methodological quality of eligible clinical trials was independently assessed by 2 reviewers. Any disagreements encountered were resolved by discussion. When no consensus could be achieved, a 3rd reviewer was consulted for reconciliation.
2.5. Statistical analysis
Weighted mean differences (WMDs) or odds ratios (ORs) and corresponding 95% confidence interval (CI) were estimated and pooled across studies to assess the discrepancy between the 2 methods with a value of P < .05 as statistically significant. Heterogeneity was assessed using the I2 value and Chi-square test. When the heterogeneity test was P ≥ .05, or I2 < 50% indicating low statistical heterogeneity, a fixed effect model was used; otherwise, a random effect model was chosen. Sensitivity analysis was evaluated by determining whether the remaining results would be markedly affected after removing outlier studies one by one. Publication bias was not assessed due to the relatively fewer studies included for any variable. All of the meta-analyses were performed with Review Manager software (RevMan Version 5.3, The Nordic Cochrane Center, The Cochrane Collaboration, Copenhagen, Denmark).
2.6. Ethical approval
This article does not contain any studies with human participants performed by any of the authors.
3. Results
3.1. Search results
A total of 532 articles were preliminarily reviewed, and the search and exclusion criteria details were displayed in a flow diagram (Fig. 1). Finally, 11 studies satisfied the eligibility criteria, including 3 RCTs[10–12] and 8 non-RCTs[13–20] associated with IMF versus arthroplasty in treating intertrochanteric hip fractures for senile were identified.
Figure 1.
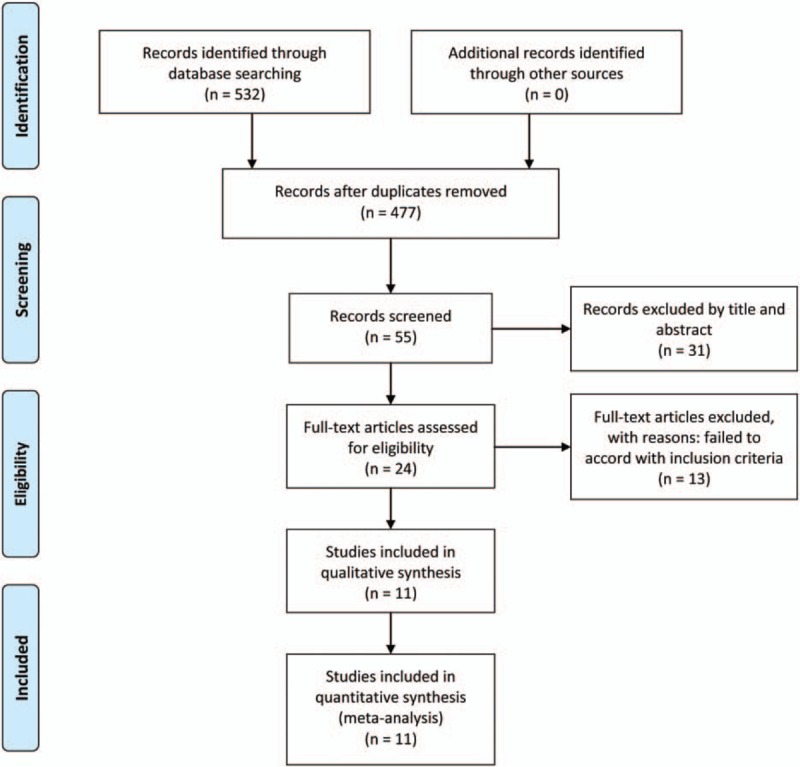
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram of study selection.
3.2. Quality assessment
The Cochrane Collaboration Risk of Bias Tool applied to evaluate the quality of the RCTs (Fig. 2), and the Methodological Index for Nonrandomized Studies assessment was used for non-RCTs (Table 1). The quality of the RCTs was acceptable, all the RCTs had reported their methods of randomization. Two RCTs[10,11] were conducted through the computer-generated list, and the remaining through a sealed opaque equivalent envelope.[12] None of the included RCTs reported blinding of the surgeons, participants, or assessors, though 1 study mentioned that the randomization list was concealed from the surgeon. All of the studies provided results for a minimum of 95% of the included patients.
Figure 2.
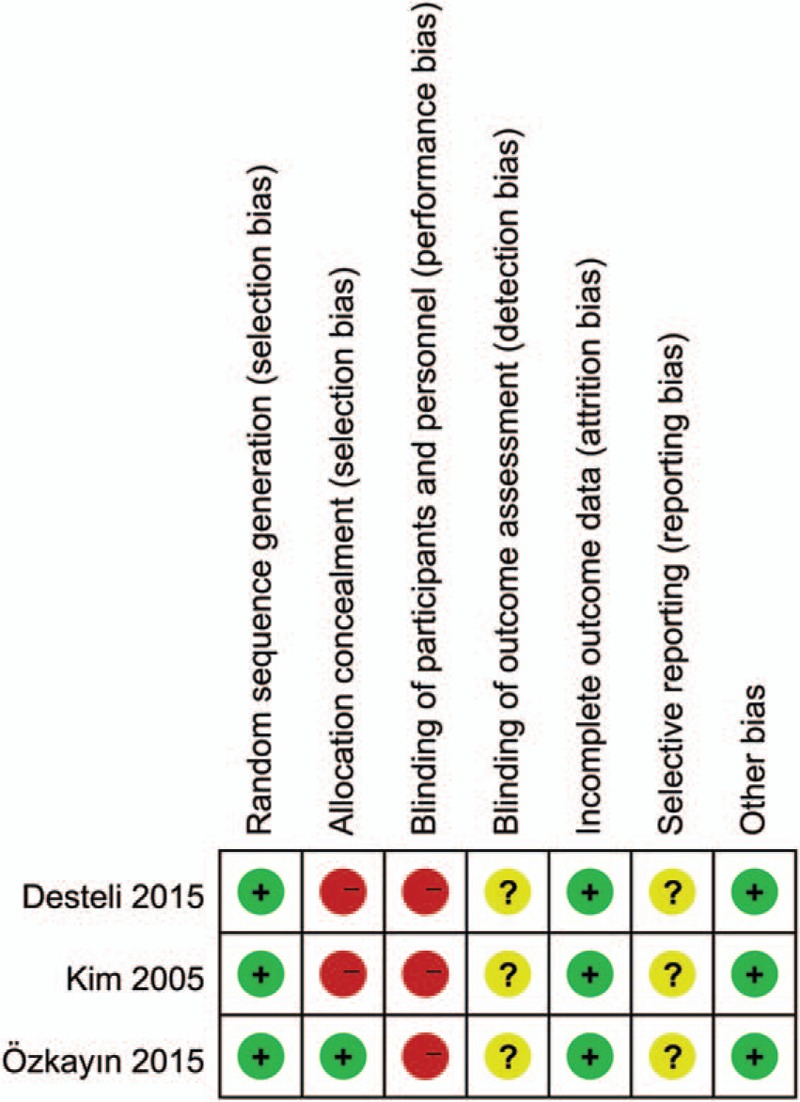
Risk of bias assessment summary of randomized controlled trials.
Table 1.
Quality assessment of nonrandomized studies (methodological index for nonrandomized studies).

3.3. Demographic characteristics
A total of 1239 patients from 11 studies were included. The demographic characteristics are summarized in Table 2. There were 552 patients who underwent IMF and 528 patients who received arthroplasty to treat intertrochanteric hip fractures. The other 159 patients from 2 studies[14,16] underwent extramedullary fixations. Four studies were from Turkey, 3 from Korea, and the others were from France, Germany, China, and Canada, respectively.
Table 2.
Characteristics of included studies.

3.4. Duration of operation
Eight studies[10–12,14,15,17–19] provided data of operation time, but just 5 studies[10–12,14,18] including 515 fractures were eligible in the form of mean and standard deviation. The pooled results indicated that there was a statistical difference in operation time between the 2 groups (WMD: −18.92, 95% CI: −33.26 to −4.57, P = .010) with significant heterogeneity (Chi2 = 251.19, P < .001, I2 = 98%, Fig. 3). However, the result of sensitive analysis by excluding the outlier study[11] did not alter significance, suggesting the result reliable.
Figure 3.
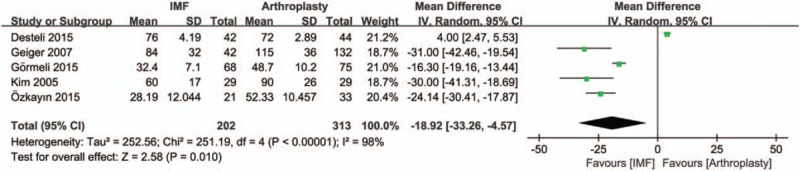
Forest plot diagram of operation time compared between intramedullary fixation and arthroplasty.
3.5. Blood loss and transfusion
There were 3 articles[10,14,18] involving 375 fractures which provided data of intraoperative blood loss. The heterogeneity test indicated there was a statistical heterogeneity (Chi2 = 190.17, P < .001, I2 = 99%), and the outcome shows a significant difference between the 2 groups (WMD: −375.01, 95% CI: −604.60 to −145.41, P = .001, Fig. 4). However, no sensitivity test was necessary because significant difference was observed in each trial, indicating the result reliable. Blood transfusion was documented in 2 articles.[10,18] The pooled data indicated the rate for blood transfusion significantly favored IMF (OR: 0.07, 95% CI: 0.03–0.16, P < .001) without any heterogeneity (Chi2 = 0.20, P = .65, I2 = 0%, Fig. 5).
Figure 4.
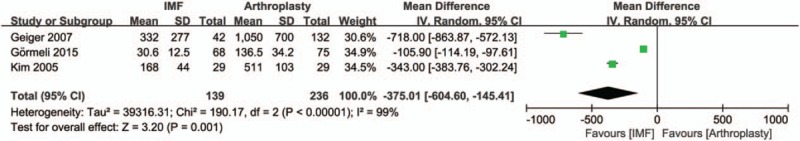
Forest plot diagram of blood loss compared between intramedullary fixation and arthroplasty.
Figure 5.
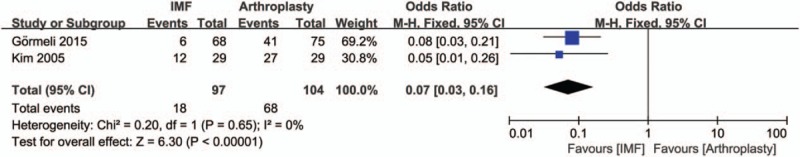
Forest plot diagram of transfusion compared between intramedullary fixation and arthroplasty.
3.6. Hospital stay
Three studies[10,11,18] reported data of hospital stay. There were a total of 287 patients, with 139 patients in IMF group and 148 in arthroplasty group. There was no statistical difference in hospital stay between IMF and arthroplasty (WMD: −0.41, 95% CI: −2.09 to 1.26, P = .63) with significant heterogeneity (Chi2 = 24.25, P < .001, I2 = 92%, Fig. 6). A sensitivity analysis found that there was no significant change when any 1 study was omitted.
Figure 6.
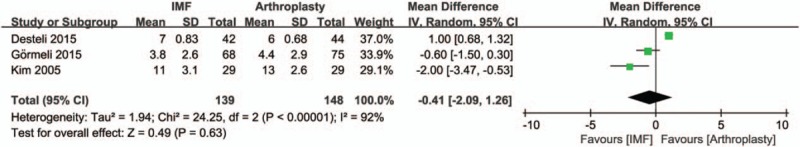
Forest plot diagram of hospital stay compared between intramedullary fixation and arthroplasty.
3.7. Harris hip score of the latest follow-up
Six studies[10,12,15,16,18,20] provided data of Harris hip score and were eligible in the form of standard deviation. There were 594 fractures included, 295 patients with the IMF and 299 with the arthroplasty. The difference between IMF and arthroplasty was significant (WMD: 4.19, 95% CI: 2.48–5.91, P < .001) with slight heterogeneity (Chi2 = 6.94, P = .23, I2 = 28%, Fig. 7).
Figure 7.
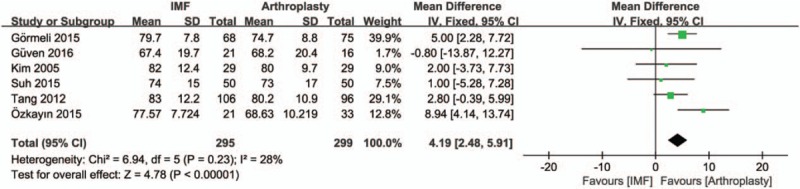
Forest plot diagram of Harris hip score of the latest follow-up compared between intramedullary fixation and arthroplasty.
3.8. Mortality within 1-year
Mortality within 1-year was documented in 6 studies.[10,13–15,17,18] There were 977 fractures included, 422 patients with the IMF and 555 with the arthroplasty. A fixed effects model was applied because no statistical heterogeneity was found between the studies (Chi2 = 2.73, P = .74, I2 = 0%). The results indicated that the rate for mortality within 1-year significantly favored IMF (OR: 0.67, 95% CI: 0.48–0.93, P = .02, Fig. 8).
Figure 8.
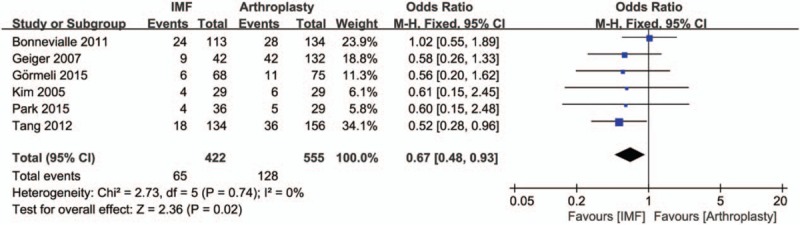
Forest plot diagram of mortality within 1-year compared between intramedullary fixation and arthroplasty.
3.9. Implant-related complications
Eight articles[10,12,13,15–19] provided data of implant-related complications, while one showed no implant-related complication,[16] which mainly included: femoral shaft fracture, cut-out, barrel loosening, shortening, protrusion of neck screw, fracture of the lateral femoral wall, and breakage of the screw. The pooled data indicated the implant-related complications significantly favored arthroplasty (OR: 2.05, 95% CI: 1.11–3.82, P = .02) without any heterogeneity (Chi2 = 5.03, P = .54, I2 = 0%, Fig. 9).
Figure 9.
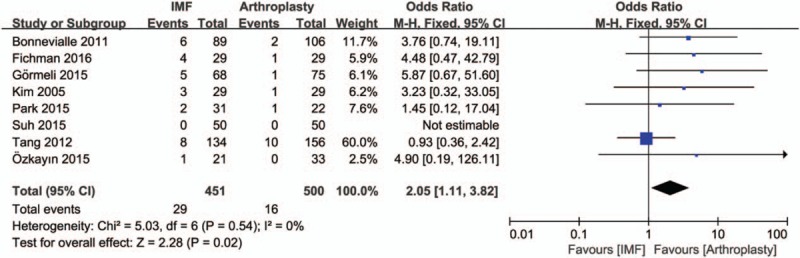
Forest plot diagram of implant-related complications compared between intramedullary fixation and arthroplasty.
3.10. Reoperation
The reasons for reoperation mainly caused by cut-out of femoral head, breakage of the implant, nonunion, and infection. Seven articles[10,12–14,17–19] provided data of reoperation, while one showed no reoperation occur.[12] The pooled results showed no significant heterogeneity (Chi2 = 3.54, P = .62, I2 = 0%), and a fixed effects model was used. The available data demonstrated that the reoperation was significantly lower in the arthroplasty group compared with IMF group (OR: 7.06, 95% CI: 3.24–15.36, P < .001, Fig. 10).
Figure 10.
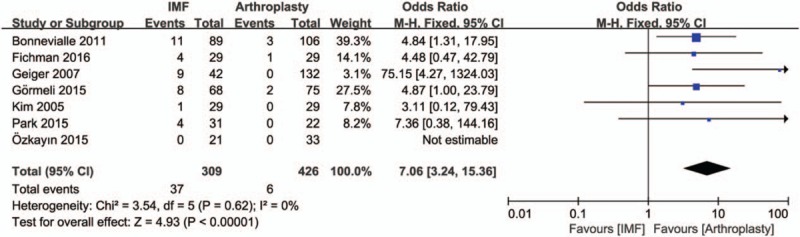
Forest plot diagram of reoperation compared between intramedullary fixation and arthroplasty.
4. Discussion
The goals of care for patients with intertrochanteric hip fractures include prompt and safe surgical stabilization to enable rapid mobilization and avoidance of medical complications. Currently, intramedullary nails are widely used in treating fractures because of a biological advantage, minimally invasive approach, and easy manipulation.[21] However, in the treatment of unstable intertrochanteric fractures in elderly patients with osteoporotic bones, the internal fixation may fail, which result in poor function and remain problems.[22] In order to allow an earlier postoperative weight-bearing and a rapid recovery and to avoid excessive collapse at the fracture site, some surgeons have turned the treatment regimen into hip prosthetic replacements as the primary treatment method of unstable intertrochanteric fractures.[22,23] Nevertheless, there is no clear evidence from clinical research to indicate that hip arthroplasty is more effective than IMF and vice versa. Therefore, we performed this meta-analysis to compare the advantages and disadvantages of the 2 devices to provide reliable evidence for clinicians in selecting the optimal treatment.
The meta-analysis showed that the IMF group had significantly shorter operation time compared with the arthroplasty group. Same result was shown in the previous study.[15] But there was a notable heterogeneity, which could probably be explained by the different levels of experience of surgeons, and the duration of IMF could be shortened as surgical skills improved. Meanwhile, the arthroplasty for intertrochanteric fractures typically required a more complex surgical procedure,[24] and this could be another probable reason to enlarge the gap of duration.
For blood loss and the rate for blood transfusion, both were reduced significantly in IMF compared with arthroplasty. Same results were shown in previous studies.[15,17] The more complex surgical procedure and more osteotomy during the operation might contribute a more blood loss in arthroplasty group.[25] The number of blood transfusion was consistent with blood loss during operation.[26] Our study showed the same result. In practice, various counting methods of intraoperative blood loss were used in different hospitals, and surgeons usually estimate it. That could explain the significant heterogeneity for blood loss.
Our meta-analysis found that hospital stay was similar in both IMF and arthroplasty group statistically. A sensitivity test was performed, which showed that, in hospital stay, the 2 groups were still similar. Furthermore, the hospital stay was more depend on prevailing medical/economic/social conditions. And the varied physical status and fracture types of patients should also be taken into consideration. That could explain the statistic significant difference of heterogeneity.
In our study, we used Harris hip score of the latest follow-up to show results of hip joint function. And the IMF had significantly higher Harris hip score compared with the arthroplasty. Same result was shown in previous study.[17] Among the above studies, there were 2 studies[12,17] recorded it in different follow-up periods. Özkayın et al[12] reported that the difference between 2 groups was statistically significant in favor of the arthroplasty until 6 months, after that time point, this difference became reverse to the IMF. Although Park et al[17] showed that there was no difference between the groups until 12 months, yet scores were significantly better in IMF group when measured 24 months after the surgery. Delayed full weight-bearing activity in IMF group might explain the reason why Harris hip scores in IMF group were not higher than arthroplasty group in early follow-up periods.
The mortality rate within 1-year in the IMF was reduced significantly compared with the arthroplasty. Hip fractures were associated with a significantly increased mortality risk in 6 to 12 months after the injury, and it became similar to that patients without hip fracture after the 1st year.[27] Hossain et al[28] showed that cement use itself in arthroplasty could lead to an increased embolic load and thus trigger cardiovascular adverse effects causing hypotension and even collapse and death of the patient. Thus, cement used in arthroplasty seemed to be a risk factor affected mortality rate within 1-year.
In our study, the IMF had significantly higher implant-related complication cases compared with the arthroplasty. The frequent problems in patients treated with IMF were cut-out of the hip screw and the 2nd fracture, while dislocation was the major complication in the arthroplasty. Results from recent reports demonstrated that primary bipolar hemiarthroplasty allowed patients to ambulate earlier with a low failure ratio.[29,30] And cut-out complication rates with newer design intramedullary nails were lower.[31] Although the technology of the IMF was continuously improved, the systematical review by Norris et al[32] reported that the incidence of a 2nd fracture after IMF was approximately 1.7%.
Our meta-analysis showed the reoperation rate was consistent with the implant-related complications. IMF had higher reoperation rate than arthroplasty. Aros et al[33] does not support routine use of an IMF for management of all intertrochanteric hip fractures in light of the higher revision surgery rate. And hip arthroplasty was advocated as the main treatment option for salvage.[34,35] Moreover, when patients treated with arthroplasty complained about hip discomfort, we handled it with observation usually. Reoperation rate was also dependent on prevailing medical/economic/social conditions. All these affected the reoperation rate.
Undoubtedly, there were several potential limitations in this meta-analysis. First, the number of studies included was not so sufficient which only 11 publications met the eligibility criteria. Second, the quality of the trials was generally low, except for 3 RCTs and 1 prospective nonrandomized trial, the other 7 studies were retrospective comparative study, and in some of the trials, the demographic characteristics were unclear, which might introduce bias into the results. Third, our inclusion criteria focused on studies in English, which led to selection or allocation biases, affected the results of our meta-analysis. Fourth, different follow-up duration of included studies also reduced the power of our research. Furthermore, the existence of publication bias, which was common to all meta-analyses, might have been unavoidable in our study.
However, to the best of our knowledge, this is the 1st meta-analysis to compare the strengths and weaknesses of IMF and arthroplasty in treating intertrochanteric hip fractures. High-quality clinical trials are required to compare the optimality between IMF and arthroplasty. To some extent, the present study is meaningful for both clinical decision making and fundamental research.
5. Conclusion
Based on this meta-analysis, we find that compared with IMF, the use of arthroplasty can reduce implant-related complications and reoperation rate, but has no obvious statistical difference in terms of hospital stay. However, IMF results in reducing blood loss and transfusion requirement, shorter operation time, higher Harris hip score, and lower rate of 1-year mortality. The mainstay of treatment of intertrochanteric hip fractures is internal fixation using IMF. In the absence of concrete evidence, arthroplasty should be undertaken with caution in carefully selected patient and surgeon should be aware of the increased complexity of doing the arthroplasty in these elderly patients. We suggest that arthroplasty may be considered as a primary treatment in patients with highly unstable factures with poor bone quality, ipsilateral hip arthritis, or other conditions with a higher risk for early failure.
Acknowledgments
The authors thank Huaxiang Rao, PhD for kindly providing statistical consultation for the study.
Footnotes
Abbreviations: CI = confidence interval, IMF = intramedullary fixation, OR = odds ratio, RCT = randomized controlled trials, WMD = weighted mean difference.
The authors have no funding and conflicts of interest to disclose.
References
- [1].Court-Brown CM, Caesar B. Epidemiology of adult fractures: a review. Injury 2006;37:691–7. [DOI] [PubMed] [Google Scholar]
- [2].Teague DC, Ertl WJ, Hickerson L, et al. What's new in orthopaedic trauma. J Bone Joint Surg Am 2016;98:1142–9.27385688 [Google Scholar]
- [3].Huang X, Leung F, Xiang Z, et al. Proximal femoral nail versus dynamic hip screw fixation for trochanteric fractures: a meta-analysis of randomized controlled trials. ScientificWorldJournal 2013;2013:805805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Bonnaire F, Lein T, Bula P. [Trochanteric femoral fractures: anatomy, biomechanics and choice of implants]. Unfallchirurg 2011;114:491–500. [DOI] [PubMed] [Google Scholar]
- [5].Sambandam SN, Chandrasekharan J, Mounasamy V, et al. Intertrochanteric fractures: a review of fixation methods. Eur J Orthop Surg Traumatol 2016;26:339–53. [DOI] [PubMed] [Google Scholar]
- [6].Haentjens P, Casteleyn PP, De Boeck H, et al. Treatment of unstable intertrochanteric and subtrochanteric fractures in elderly patients. Primary bipolar arthroplasty compared with internal fixation. J Bone Joint Surg Am 1989;71:1214–25. [PubMed] [Google Scholar]
- [7].Chan KC, Gill GS. Cemented hemiarthroplasties for elderly patients with intertrochanteric fractures. Clin Orthop Relat Res 2000;371:206–15. [DOI] [PubMed] [Google Scholar]
- [8].Higgins F J.P.T.GSe. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0 [updated March 2011]. The Cochrane CollaborationAvailable from www.cochrane-handbook.org. Accessed March 20, 2011. [Google Scholar]
- [9].Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (minors): development and validation of a new instrument. ANZ J Surg 2003;73:712–6. [DOI] [PubMed] [Google Scholar]
- [10].Kim SY, Kim YG, Hwang JK. Cementless calcar-replacement hemiarthroplasty compared with intramedullary fixation of unstable intertrochanteric fractures. A prospective, randomized study. J Bone Joint Surg Am 2005;87:2186–92. [DOI] [PubMed] [Google Scholar]
- [11].Desteli EE, Imren Y, Erdogan M, et al. Quality of life following treatment of trochanteric fractures with proximal femoral nail versus cementless bipolar hemiarthroplasty in elderly. Clin Invest Med 2015;38:E63–72. [DOI] [PubMed] [Google Scholar]
- [12].Özkayın N, Okcu G, Aktuglu K. Intertrochanteric femur fractures in the elderly treated with either proximal femur nailing or hemiarthroplasty: a prospective randomised clinical study. Injury 2015;46(Suppl 2):S3–8. [DOI] [PubMed] [Google Scholar]
- [13].Bonnevialle P, Saragaglia D, Ehlinger M, et al. Trochanteric locking nail versus arthroplasty in unstable intertrochanteric fracture in patients aged over 75 years. Orthop Traumatol Surg Res 2011;97(6 Suppl):S95–100. [DOI] [PubMed] [Google Scholar]
- [14].Geiger F, Zimmermann-Stenzel M, Heisel C, et al. Trochanteric fractures in the elderly: the influence of primary hip arthroplasty on 1-year mortality. Arch Orthop Trauma Surg 2007;127:959–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Tang P, Hu F, Shen J, et al. Proximal femoral nail antirotation versus hemiarthroplasty: a study for the treatment of intertrochanteric fractures. Injury 2012;43:876–81. [DOI] [PubMed] [Google Scholar]
- [16].Suh YS, Nho JH, Kim SM, et al. Clinical and radiologic outcomes among bipolar hemiarthroplasty, compression hip screw and proximal femur nail antirotation in treating comminuted intertrochanteric fractures. Hip Pelvis 2015;27:30–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Park BJ, Cho HM, Min WB. A comparison of internal fixation and bipolar hemiarthroplasty for the treatment of reverse oblique intertrochanteric femoral fractures in elderly patients. Hip Pelvis 2015;27:152–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Gormeli G, Korkmaz MF, Gormeli CA, et al. Comparison of femur intertrochanteric fracture fixation with hemiarthroplasty and proximal femoral nail systems. Ulusal Travma Acil Cerrahi Derg 2015;21:503–8. [DOI] [PubMed] [Google Scholar]
- [19].Fichman SG, Makinen TJ, Safir O, et al. Arthroplasty for unstable pertrochanteric hip fractures may offer a lower re-operation rate as compared to cephalomedullary nailing. Intern Orthop 2016;40:15–20. [DOI] [PubMed] [Google Scholar]
- [20].Guven M, Kocadal O, Akman B, et al. Proximal femoral nail shows better concordance of gait analysis between operated and uninjured limbs compared to hemiarthroplasty in intertrochanteric femoral fractures. Injury 2016;47:1325–31. [DOI] [PubMed] [Google Scholar]
- [21].Jiang X, Wang Y, Ma X, et al. Proximal femoral nail antirotation versus reverse less invasive stabilization system-distal femur for treating proximal femoral fractures: a meta-analysis. Medicine 2016;95:e3168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Kumar Gn K, Meena S, Kumar NVSM, et al. Bipolar hemiarthroplasty in unstable intertrochanteric fractures in elderly: a prospective study. J Clin Diagn Res 2013;7:1669–71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Rodop O, Kiral A, Kaplan H, et al. Primary bipolar hemiprosthesis for unstable intertrochanteric fractures. Int Orthop 2002;26:233–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Kaplan K, Miyamoto R, Levine BR, et al. Surgical management of hip fractures: an evidence-based review of the literature. II: intertrochanteric fractures. J Am Acad Orthop Surg 2008;16:665–73. [DOI] [PubMed] [Google Scholar]
- [25].Makinen TJ, Gunton M, Fichman SG, et al. Arthroplasty for pertrochanteric hip fractures. Orthop Clin North Am 2015;46:433–44. [DOI] [PubMed] [Google Scholar]
- [26].Hou G, Zhou F, Tian Y, et al. Predicting the need for blood transfusions in elderly patients with pertrochanteric femoral fractures. Injury 2014;45:1932–7. [DOI] [PubMed] [Google Scholar]
- [27].Kilci O, Un C, Sacan O, et al. Postoperative mortality after hip fracture surgery: a 3 years follow up. PloS One 2016;11:e0162097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Hossain M, Andrew JG. Is there a difference in perioperative mortality between cemented and uncemented implants in hip fracture surgery? Injury 2012;43:2161–4. [DOI] [PubMed] [Google Scholar]
- [29].Park MS, Cho HM, Kim JH, et al. Cementless bipolar hemiarthroplasty using a rectangular cross-section stem for unstable intertrochanteric fractures. Hip Int 2013;23:316–22. [DOI] [PubMed] [Google Scholar]
- [30].Grimsrud C, Monzon RJ, Richman J, et al. Cemented hip arthroplasty with a novel cerclage cable technique for unstable intertrochanteric hip fractures. J Arthroplasty 2005;20:337–43. [DOI] [PubMed] [Google Scholar]
- [31].Xu Y, Geng D, Yang H, et al. Treatment of unstable proximal femoral fractures: comparison of the proximal femoral nail antirotation and gamma nail 3. Orthopedics 2010;33:473. [DOI] [PubMed] [Google Scholar]
- [32].Norris R, Bhattacharjee D, Parker MJ. Occurrence of secondary fracture around intramedullary nails used for trochanteric hip fractures: a systematic review of 13,568 patients. Injury 2012;43:706–11. [DOI] [PubMed] [Google Scholar]
- [33].Aros B, Tosteson AN, Gottlieb DJ, et al. Is a sliding hip screw or im nail the preferred implant for intertrochanteric fracture fixation? Clin Orthop Relat Res 2008;466:2827–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Shi X, Zhou Z, Yang J, et al. Total hip arthroplasty using non-modular cementless long-stem distal fixation for salvage of failed internal fixation of intertrochanteric fracture. J Arthroplasty 2015;30:1999–2003. [DOI] [PubMed] [Google Scholar]
- [35].Karampinas PK, Kollias G, Vlamis J, et al. Salvage of failed hip osteosynthesis for fractures with modular hip prosthesis. Eur J Orthop Surg Traumatol 2015;25:1039–45. [DOI] [PubMed] [Google Scholar]


