Version Changes
Revised. Amendments from Version 1
Amendment of version 1 1. Method: Enterovirus D68 detection and whole genome sequencing: - deleted reference (14) and replaced references (15) after "....D68 viral specific PCR" - changed from "EV-D68 real time specific reverse-transcriptase PCR was carried out as previously described" to " EV-D68 real time ........(RT-PCR) was performed using D68 AN887 primers, D68 AN890 probe and SuperScript III One-Step RT-PCR system with Platinum Taq (Invitrogen, Carlsbad,CA, USA). PCR amplification was carried out as described in the original publication (15). In brief, in a total reaction volume of 20 μl, the PCR mixture consisted of 5 μl of template RNA, 0.6 μM of primers D68 AN887 and 0.8 μM probe D68 AN890, 10 μl of Platinum PCR supermix (Invitrogen) and 0.4ul enzyme SuperScript III One-Step RT-PCR. The thermal cycling condition consisted of 1 cycle of 50 °C for 30 min, 1 cycle of 95 °C for 2 min followed by 45 cycles of 95 °C for 15s, 55 °C for 1 min and 72 °C for 10 sec. All RT-PCR reactions were performed in a LightCycler480 II (Roche Diagnostics, Mannheim, Germany)" - changed from " EV-D68 positive specimens with .......as previously described" to " EV-D68 positive specimens with a Ct-value of 32 or less were whole-genome sequenced using........were sequenced in a single run" 2. Discussion: - After " ....account for 5% of respiratory illness in Viet Nam (21)" we added "The EV-D68 specific RT-PCR used in the present.........strains from Asia, Europe and the US" 3. Author contributions - Added " TTT, LAN" 4. Figure legends - Deleted "Table 2"
Abstract
Background: Since 1962, enterovirus D68 (EV-D68) has been implicated in multiple outbreaks and sporadic cases of respiratory infection worldwide, especially in the USA and Europe with an increasing frequency between 2010 and 2014. We describe the detection, associated clinical features and molecular characterization of EV-D68 in central and southern Viet Nam between 2009 and 2015.
Methods: Enterovirus/rhinovirus PCR positive respiratory or CSF samples taken from children and adults with respiratory/central nervous system infections in Viet Nam were tested by an EV-D68 specific PCR. The included samples were derived from 3 different observational studies conducted at referral hospitals across central and southern Viet Nam 2009 2015. Whole-genome sequencing was carried out using a MiSeq based approach. Phylogenetic reconstruction and estimation of evolutionary rate and recombination were carried out in BEAST and Recombination Detection Program, respectively.
Results: EV-D68 was detected in 21/625 (3.4%) enterovirus/rhinovirus PCR positive respiratory samples but in none of the 15 CSF. All the EV-D68 patients were young children (age range: 11.8 – 24.5 months) and had moderate respiratory infections. Phylogenetic analysis suggested that the Vietnamese sequences clustered with those from Asian countries, of which 9 fell in the B1 clade, and the remaining sequence was identified within the A2 clade. One intra sub-clade recombination event was detected, representing the second reported recombination within EV-D68. The evolutionary rate of EV-D68 was estimated to be 5.12E -3 substitutions/site/year. Phylogenetic analysis indicated that the virus was imported into Viet Nam in 2008.
Conclusions: We have demonstrated for the first time EV-D68 has been circulating at low levels in Viet Nam since 2008, associated with moderate acute respiratory infection in children. EV-D68 in Viet Nam is most closely related to Asian viruses, and clusters separately from recent US and European viruses that were suggested to be associated with acute flaccid paralysis.
Keywords: Enterovirus D68, respiratory infections, VIZIONS, next generation sequencing, Vietnam
Introduction
Enterovirus D68 (EV-D68) is a genotype of Enterovirus D, a species within the genus Enterovirus, family Picornaviridae. It was initially isolated in 1962 from children with bronchitis/pneumonia in California, USA 1. EV-D68 shares numerous properties with rhinoviruses, including its association with respiratory rather than systemic infections and, unlike other enterovirus A–D genotypes, its 5’ untranslated region (5’ UTR) end 2, 3. EV-D68 can be further divided into clades A, B and C and these can be further divided into subclades (e.g A1, A2).
Since 1962, EV-D68 has been implicated in multiple small outbreaks and sporadic cases of respiratory infection worldwide, with the associated clinical syndromes ranging in severity from mild to severe. However, between 2010 and 2014 EV-D68 was reported to the Centres of Disease Control and Prevention in the USA (USCDC) at much higher frequency than in previous years: 1153 cases were confirmed, predominantly among children and often in a context of asthma and wheezing. A simultaneous increase in numbers of cases of acute flaccid paralysis was reported, and although an epidemiological link seems possible, a virological association between these events has not yet been proven 4, 5. Genomic investigation of the causative viruses of those outbreaks in the USA showed that the EV-D68 belonged to the subclade B1 4. Increased detections of EV-D68 were also reported in both children and adults from Europe and the Asia-Pacific region during the 2014–2015 period 6– 10.
Given the emergence and potential public health threat of EV-D68, improving our knowledge about the geographic distribution, evolution and associated clinical phenotypes of the virus is essential for future intervention strategies and outbreak response. Here we describe the detection, associated clinical features and molecular characterization of EV-D68 infection, using respiratory and cerebrospinal fluid (CSF) samples from children in central and southern Viet Nam between 2009 and 2015.
Methods
Clinical samples
Clinical samples were selected from three different studies previously conducted in Viet Nam. The first cohort involved children under two years of age with lower respiratory tract infections admitted to two large paediatric hospitals (Children’s Hospital 1 and 2, Ho Chi Minh City) between 2009 and 2010 [n=632, median age: 7 months, interquartile range (IQR): 4 – 12] 11. The second cohort involved children with respiratory infections visiting the outpatient department of Children’s Hospital 1 between 2009 and 2010 (n=563; median age: 1.96 years, IQR: 1.05 – 3.18) 12. The third cohort involved adults and children hospitalised with respiratory or central nervous system infections, admitted to five major hospitals in central and southern Viet Nam between 2013 and 2016 13, with respiratory samples (n= 3791, median age: 2 years, IQR: 1 – 4) and CSF samples (n= 877, median age: 17 years, IQR: 5 – 44) being taken. The five hospitals in Viet Nam included: i) Dong Thap General Hospital, Dong Thap province, ii) Hue Central Hospital, Hue City, iii) Dak Lak General Hospital, Ban Me Thuot City, iv) Khanh Hoa General Hospital, Nha Trang City, and v) Hospital for Tropical Diseases, Ho Chi Minh City.
Ethics
All studies were approved by the corresponding institutional review board of the local hospitals in Viet Nam where patients were enrolled:
-
(i)
Children Hospital 1, Ho Chi Minh City (approval numbers 430BVNĐ and 146/BVNĐ1-KHKT);
-
(ii)
Hue Central Hospital, Hue City (77/25/05/12);
-
(iii)
Dak Lak General Hospital, Ban Me Thuot City (489/BVT-KHTH);
-
(iv)
Khanh Hoa General Hospital, Nha Trang City (356/BVĐKT);
-
(v)
Hospital for Tropical Diseases, Ho Chi Minh City (136/BVBNĐ – KH);
-
(vi)
Children Hospital 2, Ho Chi Minh City,
-
(vii)
Dong Thap General Hospital, Dong Thap province (approval number not available; signed date: 5/6/12.
The study was also approved by the Oxford Tropical Research Ethics Committee (31-08, 44-08 and 15-12).
Written informed consent was obtained from either the participant, or the participant’s parent or legal guardian.
Enterovirus D68 detection and whole genome sequencing
From the above described cohorts, archived respiratory samples and CSF were screened using a 5’ UTR PCR 14, those that were enterovirus or rhinovirus PCR positive were selected for further testing by EV-D68 viral specific PCR 15. EV-D68 real time specific reverse-transcriptase PCR (RT-PCR) was performed using D68 AN887 primers, D68 AN890 probe and SuperScrip III One-Step RT-PCR system with Platinum Taq (Invitrogen, Carlsbad, CA, USA). PCR amplification was carried out as described in the original publication 15. In brief, in a total reaction volume of 20 μl, the PCR mixture consisted of 5 μl of template RNA, 0.6 μM of primers D68 AN887 and 0.8 μM probe D68 AN890, 10 μl of Platinum PCR supermix (Invitrogen) and 0.4 μl enzyme SuperScript III One-Step RT-PCR. The thermal cycling condition consisted of 1 cycle of 50°C for 30 min, 1 cycle of 95°C for 2 min followed by 45 cycles of 95°C for 15sec, 55°C for 1 min and 72°C for 10sec. All RT-PCR reactions were performed in a LightCycler480 II (Roche Diagnostics, Mannheim, Germany).
EV-D68 positive specimens with a Ct-value of 32 or less were whole-genome sequenced using an in-house non-ribosomal random PCR and MiSeq based approach 16, 17. All the experiments were carried out as previously described 17. In short, extracted viral nucleic acids from nuclease-treated clinical samples were randomly amplified using non-ribosomal random PCR. The resulting PCR products were quantified by QIAquick PCR purification kit (QIAgen GmbH, Hilden, Germany) and measured by Qubit dsDNA HS kit (Invitrogen). One nanogram of the purified DNA was then subjected to library preparation using the Nextera XT DNA sample preparation kit (Illumina, San Diego, CA, USA), each sample was allocated to a barcode sequence using the Nextera XT Index Kit (Illumina). Sequencing of the prepared library was carried out using the MiSeq reagent kit V3 in an Illumina Miseq platform (Illumina). A total of 96 samples were sequenced in a single run.
Sequence analysis
The generated sequencing data from Illumina MiSeq was first subjected to a primer removing step using standard parameters available in Geneious software version 8.1.5 (Biomatters, Ltd, Auckland, New Zealand) 17, 18. A reference based mapping approach was then employed to assemble the viral genomes, followed by manual editing of the obtained consensuses using Geneious. Samples where the full VP1 regions or whole genomes were successfully sequenced proceeded to recombination detection and phylogenetic analysis.
Recombination detection and phylogenetic analysis
All sequence alignment was carried out using MUSCLE, available in Geneious (Biomatters).
Recombination was inferred using a combination of methods (Chimera, GENECONV, Maxchi, Bootscan and Siscan) within RDP4 (Recombination Detection Program, version 4) 19, with recombination supported if more than three methods showed significant values. The recombination event was then confirmed by constructing a neighbor-joining tree using the group D enterovirus sequences. Identified recombined samples were removed from further phylogenetic analysis.
The origin, evolution rate and divergence time of EV-D68 were estimated by using representatives of VP1 sequences (n=124) and whole genome sequences (n=58), downloaded from GenBank ( Supplementary Table 1 and Supplementary Table 2) alongside the Vietnamese sequences recovered in the present study. All analyses were carried out in BEAST version 1.8.3 20 using the General Time Reversible (GTR) with gamma 4 nucleotide substitution model and the strict molecular clock model and support for individual nodes was assessed using a bootstrap produce (1000 replicates). The molecular model was selected using Bayes factor. The Bayesian MCMC chain lengths were 100 million generations with sampling every 1000 generations.
Sequence accession numbers
The sequences of EV-D68 obtained in this study were submitted to NCBI under accession numbers MF045413–MF045423.
Results
Of a total 5863 samples (4986 respiratory samples and 877 CSF), 639 (624 respiratory, 15 CSF) were positive for enterovirus or rhinovirus by PCR on initial screening. EV-D68 was subsequently detected in 21 of 624 (3.4%) of enterovirus/ rhinovirus positive respiratory samples, while no CSF samples were positive for EV-D68. Overall, EV-D68 was detected in 0.4% of 5863 tested samples, and 3.3% of 639 enterovirus/ rhinovirus positive respiratory/CSF samples. The earlier EV-D68 PCR positive sample was collected on the 4th December 2009.
Demographics and clinical features
Table 1 briefly summarises the demographics, presenting features and outcomes for all 21 EV-D68 PCR positive patients. All 21 patients in whom EV-D68 was detected were aged 2 years or less, with a median age of 17 months at time of presentation. Three were admitted to the outpatient department of Children’s Hospital 1 (the second cohort), and the remaining 18 were inpatients enrolled into the first and the third cohorts. One patient had a pre-existing neurological comorbidity; the remaining 20 children were healthy at baseline.
Table 1. Demographics, clinical features and outcome for 21 patients with EV-D68 PCR positive respiratory specimens.
Categorical data were presented as n (%). Continuous variables were presented as median (range).
| Characteristics | |
|---|---|
| Male | 13 (61.9) |
| Female | 8 (38.1) |
| Age (months) | 17.2 (11.8-24.5) |
| Clinical features | |
| Acute respiratory illness | 21 (100) |
|
Duration of symptoms prior to admission
(days) |
2 (2-3) |
| Fever | 13 (61.9) |
| Temperature at presentation | 38.0 (37.5-38.4) |
| Haematology results | |
| Haemoglobin (g/dL) | 11.2 (10.3-12.0) |
| Leucocyte count ×10 9/L | 13.6 (10.9-16.5) |
| Neutrophils % total | 57.3 (37.8-64.9) |
| Lymphocytes % total | 30.45 (22.5-43) |
| Eosinophils % total | 0.25 (0.2-1.9) |
| Platelets | 347 (316-377) |
| Discharge outcome* | |
| Complete recovery | 16 (76.2) |
| Residual symptoms | 5 (23.8) |
| Death | 0 (0) |
All 21 patients presented with an acute respiratory illness of short duration (median onset 2 days prior to admission), and the median temperature at presentation was 38°C (range: 37.5°C – 38.4°C) ( Table 1). No patient required admission to intensive care. All of the patients survived their infection, and 16 (76%) had recovered completely at the time of discharge. The nature of the residual symptoms in the remaining 5 patients was not available. There were no reported cases of acute flaccid paralysis in this case series.
Whole genome sequencing
In total, 15 samples were processed for whole genome sequencing; of these, 9 samples gave genome coverage of over 89%, with the uncovered sections being mainly confined to the 5’ end of the genome. Two additional samples gave complete coverage of the VP1 region.
Recombination detection
One recombination event was detected, in sample EVD68-VN5, with the recombination being intra sub-clade, within B1 ( Figure 1). The recombination event occurred between nucleotide 3500 and 6300, with the sequence assembly depth remaining at about 1000 across the whole genome and phylogenetic tree, with a change in topological position within the B1 clade supported by the recombination event ( Figure 1C). Sample EVD68-VN5 was therefore removed from subsequent phylogenetic inference.
Figure 1. Recombination analysis of EVD68-VN9.
( A) Similarity plot analysis of EVD68-VN5 against the two heterogenic parents, EVD68-VN3 (blue) and EVD68-VN7 (purple). The x-axis indicates the number of nucleotides along the alignment, the y-axis indicates percentage similarity. ( B) Bootscan plot analysis supporting for the recombination event of EVD68-VN5 detected by similarity plot analysis in ( A). The y-axis indicates the percentage of bootstrap values. ( C) Phylogenetic analyses of nonrecombinant fragments of representatives of clade B1; the putative recombinant strain is in red.
Phylogenetic analysis and evolutionary rate of EV-D68
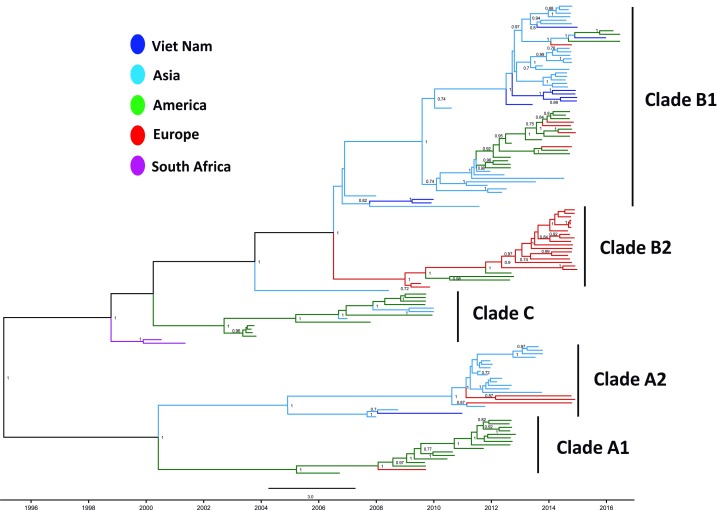
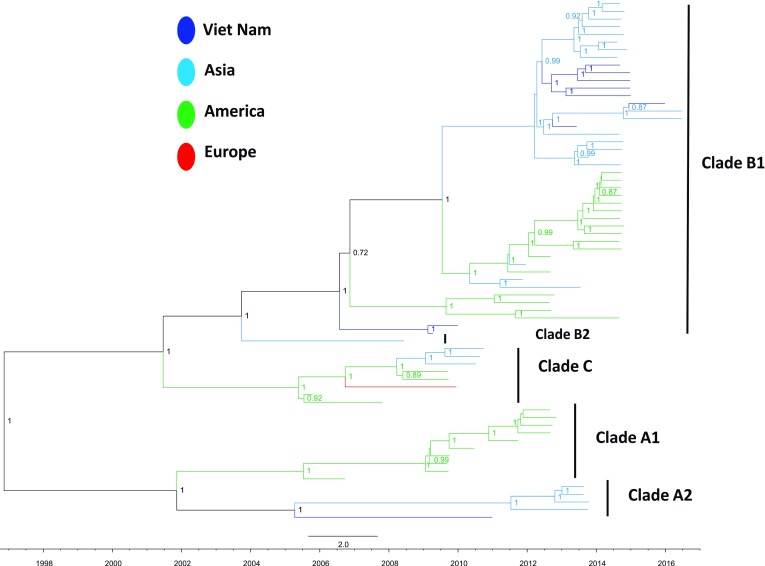
9 out of 10 Vietnamese EV-D68 VP1 sequences fell in the B1 clade ( Figure 2), and the remaining sequence was identified within the A2 clade. In all cases, the Vietnamese sequences clustered with Asian viruses. Whilst the Vietnamese viruses were not monophyletic, seven of the B1 sequences had other Vietnamese sequences as their closest relatives. Phylogenetic analysis also suggests that the analysis was carried out at whole genome level ( Figure 3), with the exception that a single sequence from the A2 clade was introduced earlier (2006).
Figure 2. MCC tree from Bayesian timescale phylogenetic analysis based on complete VP1 nucleotide sequence (927nt) of EV-D68 including Vietnamese strains obtained from this study (dark blue) and global representatives retrieved from GenBank.
Figure 3. MCC tree from Bayesian timescale phylogenetic analysis based on complete genomes of EV-D68 including Vietnamese strains obtained from this study (dark blue) and global representatives retrieved from GenBank.
The rate of evolution of EV-D68 was calculated from the VP1 data as 5.12E -3 substitutions/site/year. Bayesian analysis suggests that the EV-D68 origin lies in late 1960, and the common ancestor of the lineages under-investigation arose in 1994.
Discussion
Herein we have described for the first time the clinical presentation and phylogenetic characterization of EV-D68 in Viet Nam for the period 2009 to 2015.
Of 639 patients whose nasopharyngeal or CSF sample tested positive for enterovirus or rhinovirus on multiplex PCR, 21 (3.2%) respiratory samples were found to be positive for EV-D68 on specific RT-PCR. Overall, of 4986 respiratory samples screened, 0.4% were positive for EV-D68. This indicates that EV-D68 has been circulating at low levels in Viet Nam between 2009 and 2015; however, it does not represent a major contribution to the burden of acute respiratory illness in the region, in line with findings by Nguyen et al. that show enteroviruses only account for 5% of respiratory illness in Viet Nam 21. The EV-D68 specific RT-PCR used in the present study has been shown to have a sensitivity and specificity of 98.6% and 97.5% respectively 15, however evaluation of assay performance has only taken place in the United States. Therefore, the assay sensitivity and specificity on South-Easrt Asian clades of EV-D68 remain unknown and thus some may have been missed in our cohort, although as originally designed, the assay should be able to detect all EV-D68 strains from Asia, Europe and the US.
All of 21 EV-D68 positive patients were aged less than 2 years, presented with a respiratory illness of short duration and none needed admission to intensive care units. This is consistent with the findings of Xiang et al. 22 who reported that EV-D68 infection predominantly caused non-severe respiratory illness in children in China between 2006 and 2014, but differs from reports from Thailand and Cambodia, where EV-D68 positive patients were mostly older children and adults, respectively 23, 24. It should be noted, however, that the majority of our patients were children, which may explain the difference. Likewise, it has recently been reported in the Netherlands that EV-D68 was associated with severe respiratory infection in young children, however most of these patients had pulmonary co-morbidity at baseline 25.
Our phylogenetic analysis puts the identified Vietnamese EV-D68 in a global context and shows that the EV-D68 viruses circulating in Viet Nam belong to subclade B1, which includes EV-D68 viruses sampled across various continents including Asia, Europe and America. Our Vietnamese viruses are, however, most closely related to other Asian strains, and cluster separately within subgroup B1 from those which have been associated with epidemic outbreaks and implicated in acute flaccid paralysis in the USA in children with a median age of 8 years 4. It should however be noted that to date there has been no definitive link between specific EV-D68 strains and clinical phenotypes. Likewise, the causative role of EV-D68 in acute flaccid paralysis remains unproven.
Interestingly, we report herein a recombination event within our EV-D68 whole genome data set. This represents the second reported recombination within EV-D68 26, although recombination is a common phenomenon of enterovirus evolution.
The non-monophyletic clustering pattern suggests that EV-D68 was introduced in Viet Nam multiple times, while the low-level clustering suggests some persistence within Viet Nam, with no outbreak reported until now. Our data agrees with other published estimations of the origin and evolution rate of EV-D68 23, 27.
Conclusion
We have demonstrated that EV-D68 has been circulating at low levels in Viet Nam in the period of 2009 to 2015, and is associated with a moderate acute respiratory infection in healthy children in our cohorts. EV-D68 in Viet Nam is most closely related to other circulating Asian strains, and clusters separately from those implicated to be associated with acute flaccid paralysis in the USA and Europe.
Data availability
The sequences of EV-D68 obtained in this study were submitted to NCBI under accession numbers MF045413–MF045423.
Acknowledgements
The VIZIONS Consortium members (alphabetical order by surname), from the Oxford University Clinical Research Unit are: Bach Tuan Kiet, Stephen Baker, Alessandra Berto, Maciej F. Boni, Juliet E. Bryant, Bui Duc Phu, James I. Campbell, Juan Carrique-Mas, Dang Manh Hung, Dang Thao Huong, Dang Tram Oanh, Jeremy N. Day, Dinh Van Tan, H. Rogier van Doorn, Duong An Han, Jeremy J. Farrar, Hau Thi Thu Trang, Ho Dang Trung Nghia, Hoang Bao Long, Hoang Van Duong, Huynh Thi Kim Thu, Lam Chi Cuong, Le Manh Hung, Le Thanh Phuong, Le Thi Phuc, Le Thi Phuong, Le Xuan Luat, Luu Thi Thu Ha, Ly Van Chuong, Mai Thi Phuoc Loan, Behzad Nadjm, Ngo Thanh Bao, Ngo Thi Hoa, Ngo Tri Tue, Nguyen Canh Tu, Nguyen Dac Thuan, Nguyen Dong, Nguyen Khac Chuyen, Nguyen Ngoc An, Nguyen Ngoc Vinh, Nguyen Quoc Hung, Nguyen Thanh Dung, Nguyen Thanh Minh, Nguyen Thi Binh, Nguyen Thi Hong Tham, Nguyen Thi Hong Tien, Nguyen Thi Kim Chuc, Nguyen Thi Le Ngoc, Nguyen Thi Lien Ha, Nguyen Thi Nam Lien, Nguyen Thi Ngoc Diep, Nguyen Thi Nhung, Nguyen Thi Song Chau, Nguyen Thi Yen Chi, Nguyen Thieu Trinh, Nguyen Thu Van, Nguyen Van Cuong, Nguyen Van Hung, Nguyen Van Kinh, Nguyen Van Minh Hoang, Nguyen Van My, Nguyen Van Thang, Nguyen Van Thanh, Nguyen Van Vinh Chau, Nguyen Van Xang, Pham Ha My, Pham Hong Anh, Pham Thi Minh Khoa, Pham Thi Thanh Tam, Pham Van Lao, Pham Van Minh, Phan Van Be Bay, Maia A. Rabaa, Motiur Rahman, Corinne Thompson, Guy Thwaites, Ta Thi Dieu Ngan, Tran Do Hoang Nhu, Tran Hoang Minh Chau, Tran Khanh Toan, Tran My Phuc, Tran Thi Kim Hong, Tran Thi Ngoc Dung, Tran Thi Thanh Thanh, Tran Thi Thuy Minh, Tran Thua Nguyen, Tran Tinh Hien, Trinh Quang Tri, Vo Be Hien, Vo Nhut Tai, Vo Quoc Cuong, Voong Vinh Phat, Vu Thi Lan Huong, Vu Thi Ty Hang, and Heiman Wertheim; from the Centre for Immunity, Infection, and Evolution, University Of Edinburgh: Carlijn Bogaardt, Margo Chase-Topping, Al Ivens, Lu Lu, Dung Nyugen, Andrew Rambaut, Peter Simmonds, and Mark Woolhouse; from The Wellcome Trust Sanger Institute, Hinxton, United Kingdom: Matthew Cotten, Bas B. Oude Munnink, Paul Kellam, and My Vu Tra Phan; from the Laboratory of Experimental Virology, Department of Medical Microbiology, Center for Infection and Immunity Amsterdam (CINIMA), Academic Medical Center of the University of Amsterdam, Amsterdam, the Netherlands: Martin Deijs, Lia van der Hoek, Maarten F. Jebbink, and Seyed Mohammad Jazaeri Farsani; and from Metabiota, CA: Karen Saylors and Nathan Wolfe.
Funding Statement
This work was supported by the Wellcome Trust, UK [101104/Z/13/Z, 106680/B/14/Z, 093724/Z/10/Z and 204904/Z/16/Z].
The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
[version 2; referees: 3 approved]
Supplementary materials
Supplementary Table 1: Accession numbers, locations and sampling dates of representatives of VP1 sequences.References
- 1. Schieble JH, Fox VL, Lennette EH: A probable new human picornavirus associated with respiratory diseases. 1967;85(2):297–310. 10.1093/oxfordjournals.aje.a120693 [DOI] [PubMed] [Google Scholar]
- 2. Blomqvist S, Savolainen C, Råman L, et al. : Human rhinovirus 87 and enterovirus 68 represent a unique serotype with rhinovirus and enterovirus features. United States;2002;40(11):4218–23. 10.1128/JCM.40.11.4218-4223.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Oberste MS, Maher K, Schnurr D, et al. : Enterovirus 68 is associated with respiratory illness and shares biological features with both the enteroviruses and the rhinoviruses. England;2004;85(Pt 9):2577–84. 10.1099/vir.0.79925-0 [DOI] [PubMed] [Google Scholar]
- 4. Greninger AL, Naccache SN, Messacar K, et al. : A novel outbreak enterovirus D68 strain associated with acute flaccid myelitis cases in the USA (2012–14): a retrospective cohort study. Elsevier Ltd;2015;15(6):671–82. 10.1016/S1473-3099(15)70093-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Sejvar JJ, Lopez AS, Cortese MM, et al. : Acute Flaccid Myelitis in the United States, August-December 2014: Results of Nationwide Surveillance. 2016;63(6):737–745. 10.1093/cid/ciw372 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bal A, Schuffenecker I, Casalegno JS, et al. : Enterovirus D68 nosocomial outbreak in elderly people, France, 2014. England;2015;21(8):e61–2. 10.1016/j.cmi.2015.05.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Furuse Y, Chaimongkol N, Okamoto M, et al. : Molecular epidemiology of enterovirus D68 from 2013 to 2014 in Philippines. 2015;53(3):1015–8. 10.1128/JCM.03362-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Levy A, Roberts J, Lang J, et al. : Enterovirus D68 disease and molecular epidemiology in Australia. 2015;69:117–21. 10.1016/j.jcv.2015.06.079 [DOI] [PubMed] [Google Scholar]
- 9. Vongpunsawad S, Prachayangprecha S, Chansaenroj J, et al. : Genome sequence of enterovirus D68 and clinical disease, Thailand. 2015;21(2):384. 10.3201/eid2102.141742 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Zhang T, Ren L, Luo M, et al. : Enterovirus D68-associated severe pneumonia, China, 2014. 2015;21(5):916–8. 10.3201/eid2105.150036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Do LA, Bryant JE, Tran AT, et al. : Respiratory Syncytial Virus and Other Viral Infections among Children under Two Years Old in Southern Vietnam 2009–2010: Clinical Characteristics and Disease Severity. Schildgen O, editor. Public Library of Science;2016;11(8):e0160606. 10.1371/journal.pone.0160606 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Ngoc N, Minh Q: Outpatient Antibiotic Use in Acute Respiratory Infections.2014. Reference Source [Google Scholar]
- 13. Rabaa MA, Tue NT, Phuc TM, et al. : The Vietnam Initiative on Zoonotic Infections (VIZIONS): A Strategic Approach to Studying Emerging Zoonotic Infectious Diseases. Springer US;2015;12(4):726–35. 10.1007/s10393-015-1061-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jansen RR, Schinkel J, Koekkoek S, et al. : Development and evaluation of a four-tube real time multiplex PCR assay covering fourteen respiratory viruses, and comparison to its corresponding single target counterparts. 2011;51(3):179–85. 10.1016/j.jcv.2011.04.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Zhuge J, Vail E, Bush JL, et al. : Evaluation of a Real-Time Reverse Transcription-PCR Assay for Detection of Enterovirus D68 in Clinical Samples from an Outbreak in New York State in 2014. 2015;53(6):1915–20. 10.1128/JCM.00358-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. de Vries M, Deijs M, Canuti M, et al. : A sensitive assay for virus discovery in respiratory clinical samples. 2011;6(1):e16118. 10.1371/journal.pone.0016118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Nguyen AT, Tran TT, Hoang VM, et al. : Development and evaluation of a non-ribosomal random PCR and next-generation sequencing based assay for detection and sequencing of hand, foot and mouth disease pathogens. 2016;13(1):125. 10.1186/s12985-016-0580-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Kearse M, Moir R, Wilson A, et al. : Geneious Basic: an integrated and extendable desktop software platform for the organization and analysis of sequence data. 2012;28(12):1647–9. 10.1093/bioinformatics/bts199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Martin DP, Murrell B, Golden M, et al. : RDP4: Detection and analysis of recombination patterns in virus genomes. 2015;1(1):vev003. 10.1093/ve/vev003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Drummond AJ, Suchard MA, Xie D, et al. : Bayesian phylogenetics with BEAUti and the BEAST 1.7. 2012;29(8):1969–73. 10.1093/molbev/mss075 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Nguyen DN, Mai le Q, Bryant JE, et al. : Epidemiology and etiology of influenza-like-illness in households in Vietnam; it’s not all about the kids! Elsevier B.V;2016;82:126–32. 10.1016/j.jcv.2016.07.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Xiang Z, Xie Z, Liu L, et al. : Genetic divergence of enterovirus D68 in China and the United States. England;2016;6: 27800. 10.1038/srep27800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Linsuwanon P, Puenpa J, Suwannakarn K, et al. : Molecular epidemiology and evolution of human enterovirus serotype 68 in Thailand, 2006–2011. United States;2012;7(5):e35190. 10.1371/journal.pone.0035190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Ly N, Tokarz R, Mishra N, et al. : Multiplex PCR analysis of clusters of unexplained viral respiratory tract infection in Cambodia. England;2014;11:224. 10.1186/s12985-014-0224-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Knoester M, Schölvinck EH, Poelman R, et al. : Upsurge of Enterovirus D68, the Netherlands, 2016. 2017;23(1):140–3. 10.3201/eid2301.161313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tan Y, Hassan F, Schuster JE, et al. : Molecular Evolution and Intraclade Recombination of Enterovirus D68 during the 2014 Outbreak in the United States. 2015;90(4):1997–2007. 10.1128/JVI.02418-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Du J, Zheng B, Zheng W, et al. : Analysis of Enterovirus 68 Strains from the 2014 North American Outbreak Reveals a New Clade, Indicating Viral Evolution. United States;2015;10(12):e0144208. 10.1371/journal.pone.0144208 [DOI] [PMC free article] [PubMed] [Google Scholar]