Highlights
-
•
Intestinal duplications cysts are rare congenital anomalies that can occur throughout the gastrointestinal tract.
-
•
Isolated intestinal duplication cysts can present with vague abdominal complaints.
-
•
Diagnosis can be challenging even with imaging.
-
•
Our clinical workup was suggestive of a mucinous cystic neoplasm (MCN) of the pancreas.
-
•
This represents the first reported case of an enteric duplication cyst that mimicked an MCN of the pancreas.
Abbreviations: CT, computed tomography; EUS, endoscopic ultrasound; FNA, fine-needle aspiration; MCN, mucinous cystic neoplasm; MRI, magnetic resonance imaging; CEA, carcinoembryonic antigen; GI, gastrointestinal
Keywords: Enteric, Intestinal, Isolated duplication cyst
Abstract
Introduction
Enteric duplication cysts presenting in adulthood are rare. Isolated enteric duplication cysts, which lack a connection to the GI tract or the adjacent mesenteric vasculature, have only been cited in six previous case reports.
Case presentation
A 48-year-old female presented with a four-year history of intermittent nausea, vomiting and abdominal pain. Computed tomography (CT) scan of the abdomen revealed a 7 cm multi-lobular, calcified, cystic lesion intimately involved with the pancreas. Endoscopic ultrasound (EUS)-guided fine-needle aspiration (FNA) was non-diagnostic; however, the cyst fluid Carcinoembryonic Antigen (CEA) level was significantly elevated leading to a presumed diagnosis of a mucinous cystic neoplasm (MCN) of the pancreas. Intraoperatively, the cystic mass was identified and notably did not have any true attachments to the neighboring pancreas, gastrointestinal tract or vasculature. Final pathology demonstrated an isolated small bowel duplication cyst.
Discussion
In this case a patient presented with a clinical picture consistent with an MCN of the pancreas. However, intraoperatively and on final pathology the mass was found to be an isolated enteric duplication cyst. This represents only the seventh such case report in an adult.
Conclusion
Although rare, isolated enteric duplication cysts can be considered in a patient presenting with chronic abdominal pain and an abdominal mass on imaging. In this case we demonstrate that an isolated enteric duplication cyst can clinically mimic an MCN of the pancreas.
1. Introduction
Intestinal duplications cysts are rare congenital anomalies that can occur throughout the gastrointestinal tract, but are most commonly found in the small intestine. Although usually detected in infancy and childhood, duplication cysts can occasionally be found in adulthood. Duplication cysts typically have some connection to the gastrointestinal tract (GI) as well as the local blood supply to that region. However, in rare cases the cysts can be completed isolated from the GI tract and in these cases often have a separate vascular pedicle. Here we report a case of an isolated intestinal duplication cyst surrounding the pancreas that was initially suggestive of a pancreatic mucinous cystic neoplasm (MCN). This work has been reported in line with the SCARE criteria [1].
2. Case presentation
A 48-year-old female patient presented with intermittent nausea, vomiting and abdominal pain. She reported that these symptoms had persisted over the past four years. Clinical examination did not demonstrate any reproducible abdominal pain. Her past medical and surgical history was unremarkable. Family and social history were also non-contributory.
After evaluation, she underwent a contrast-enhanced computed tomography (CT) scan, which revealed a 7.3 × 6.7 cm multi-lobular, calcified, cystic lesion intimately involved with the pancreas (Fig. 1). Magnetic resonance imaging (MRI) was subsequently performed to better characterize the mass, which again showed a multi-lobulated cystic lesion with peripheral calcifications involving the body and tail of the pancreas (Fig. 2).
Fig. 1.
CT demonstrates a 7.3 × 6.7 cm cystic lesion (red arrow).
Fig 2.
MRI demonstrates a multi-lobulated cystic lesion.
The decision was made to perform an endoscopic ultrasound (EUS) with fine-needle aspiration (FNA) to obtain a tissue diagnosis. EUS demonstrated a 6.3 cm, partially calcified multi-loculated, cystic lesion in the body of the pancreas with thick irregular walls and without any clear communication to the main pancreatic duct. FNA was non-diagnostic and demonstrated histiocytes in a granular background. The cyst fluid was aspirated and sent for Carcinoembryonic Antigen (CEA) and amylase. Her cyst CEA level was significantly elevated at 10,758 ng/mL and cyst amylase was 558 units/L. A presumed diagnosis of a mucinous cystic neoplasm (MCN) was made. After an extensive discussion in clinic the patient agreed to undergo an exploratory laparotomy with planned resection of the mass.
The patient was taken to the operating room by a surgical oncologist who primarily specialized in pancreatic resections and had been in practice for over 10 years. Upon laparotomy, the gastrocolic ligament was divided and the lesser sac was entered to expose the body and tail of the pancreas. We subsequently identified a portion of the cystic structure just posterior to the pancreas and situated directly beneath the splenic artery. On further dissection, the cystic structure was clearly separate from the pancreas and was relatively shelled out without requiring resection of any adjacent structures. We did not identify a dominant feeding vessel to the cyst.
The patient had an uneventful post-operative course. She was discharged home on post-operative day 5. Final pathology of the cyst demonstrated a small bowel duplication cyst with cystic and calcified components (Fig. 3). During the patient’s initial post-operative visit she was counseled that we identified an enteric duplication cyst without any evidence of malignancy. On subsequent follow-up the patient reported resolution of her abdominal symptoms.
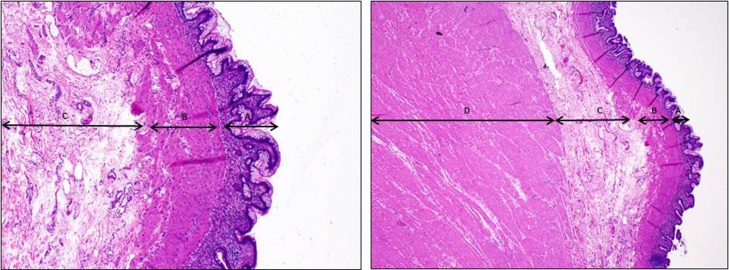
Fig. 3.
Duplication cyst most compatible with jejunum.
3. Discussion
Intestinal duplication cysts are rare, seen in approximately 1/100,000 births [2], [3]. These enteric cysts can occur throughout the gastrointestinal tract and have a predilection for the jejunum and ileum (47–70%), but can also be found in the colon (20%), esophagus (17%), stomach (8%) and duodenum (2–12%) [4]. These cysts are predominantly found on the mesenteric side of the bowel [5]. Enteric duplication cysts typically have some connection to the GI tract as well as to the local blood supply to that region; however, in rare cases, the cyst can be completed isolated from the GI tract and typically have a separate vascular pedicle [6], [7]. Intestinal duplications cysts which are completed isolated from the GI tract have been characterized in only a few case reports [8]. Here we report a case of an isolated intestinal duplication cyst surrounding the pancreas in an adult.
Histologically, enteric duplication cysts are similar in structure and histomorphology to the normal bowel wall and usually contain all layers (mucosa, submucosa, muscularis propria and serosa). These are most frequently found in intimate association with the normal adjacent GI tract [9]. Embryologically, the GI tract canalizes and becomes a hollow viscus between weeks 6–8 of fetal development. Enteric duplication cysts have been identified and reported as early as 12 weeks into fetal development [10]. Several theories have been proposed on the etiology of enteric duplication cysts: 1) aberrant luminal recanalization theory, which postulates that duplication cysts form as an aberrancy of the developmental canalization process and result in a parallel tract to the normal lumen, 2) abortive twinning theory that represents incomplete twinning during fetal development 3), split notochord theory, 4) persistent embryologic diverticula theory, and 5) sequestration of part of the fetal gut [4], [11].
Duplication cysts rarely communicate directly with the intestinal lumen despite often being attached to the intestine and occasionally even sharing a common wall. These cysts typically share the same mesenteric blood supply as the adjacent bowel. However, completed isolated enteric duplication cysts have no attachments to the intestinal wall and usually have their own vascular supply [12], [13]. The blood supply to these cysts becomes relevant from a surgical perspective, as a shared blood supply with neighboring bowel will often necessitate a bowel resection. In the case of an isolated duplication cyst without a shared blood supply, as seen in our patient, division of the vascular supply with subsequent resection of the cyst does not compromise the vasculature to any normal bowel.
The differential diagnosis of an intra-abdominal cystic mass is broad and includes mesenteric and omental cysts, ovarian cysts when found in the pelvis, mucinous cystic neoplasms of the pancreas and pancreatic pseudocysts more commonly seen in the setting of recurrent pancreatitis. The patient featured in this case report presented with imaging consistent with a peri-pancreatic mass in the setting of a fluid aspirate with a high CEA level. This presentation initially raised our concern for a diagnosis of a mucinous cystic neoplasm (MCN) of the pancreas. However, our intraoperative findings demonstrated a clearly isolated cystic structure, and final pathology confirmed an enteric duplication cyst.
Typically, these cysts are found in infants before the first year of life and can manifest pre-natally on screening ultrasound, or post-natally as small bowel obstruction, perforation or hemorrhage [14], [15]. When not found in infancy, these cysts can be asymptomatic, thereby evading diagnosis [8]. When found incidentally on CT, enteric duplication cysts typically appear as well-circumscribed, fluid-filled, round structures with a thin, enhancing wall [12].
Isolated duplication cysts in adults are exceedingly rare, and this case represents only the seventh such case report that has been described. The previous cases were equally split between men and women. Five of the six prior case reports involved the mesentery of either the small or large bowel. Two of the cases were found incidentally. One case presented with a palpable mass. The remaining three cases presented with either abdominal pain or abdominal fullness [8]. The patient in our case report presented with intermittent GI symptoms and abdominal pain, consistent with the most commonly presenting symptom in the prior case reports (Table 1).
Table 1.
Total case reports of isolated enteric duplication cyst.
| Reference | Age | Gender | Clinical Feature | Dimensions (cm) | Site | Mucosal Type |
|---|---|---|---|---|---|---|
| Blank et al. [17] | 51 | M | Incidental | 10 × 4 | Mesentery of the ileum | Villi, crypts, numerous mucous cells |
| Kim et al. [20] | 28 | M | Incidental | Not mentioned | Mesentery of the ligament of Treitz | Gastric |
| Nichols et al. [21] | 27 | F | Abdominal fullness | 9 × 6 x 1 | Mesentery of the descending colon | Simple columnar epithelium |
| Lee et al. [22] | 21 | F | Palpable mass | 3.5 × 2.5 | Mesentery in the vicinity of the round ligament | No epithelial lining |
| Kyriakos et al. [23] | 20 | M | Abdominal pain and fever | 7 × 4 | Lateral region of the ascending colon | Not mentioned |
| Park et al. [8] | 36 | F | Abdominal pain | 12 × 8.5 × 6 | Mesentery of the terminal ileum | Mixed |
| Present case | 48 | F | Abdominal pain | 6.5 × 4.5 × 2.5 | Retropancreatic | Jejunal |
There is no clear consensus on how to treat intestinal duplication cysts. However, it should be emphasized that given the difficulty in establishing a preoperative diagnosis, symptomatology should and often does dictate surgical management. In a patient with abdominal pain where other causes have been sufficiently ruled out (i.e. peptic ulcer disease, pancreatitis, etc.), it is our opinion that resection is merited. Additionally, there have been instances of underlying carcinoma found in enteric duplication cysts in adults [16], [17], [18]. Therefore, it is further justified to choose resection over surveillance in the management of enteric duplication cysts. Open as well as laparoscopic approaches have been described in the surgical management of enteric duplication cysts, which are generally resectable [19]. The location of the tumor with attention to the adjacent anatomic structures involved (i.e. mesenteric, peri-pancreatic, etc.) as well as surgeon preference should help guide the operative approach.
4. Conclusion
Isolated enteric duplication cysts in adults are exceedingly rare, and this case represents only the seventh such case report. The majority of these case presentations were characterized by abdominal symptoms, such as abdominal pain or fullness. Unique to this case, the preoperative imaging and laboratory studies were concerning for a mucinous cystic neoplasm of the pancreas. However, intraoperatively we identified a cystic structure that was not adherent to the pancreas or GI tract and final pathology demonstrated an isolated enteric duplication cyst.
Conflicts of interest
No conflicts of interest.
Funding
No sources of funding.
Ethical approval
For case reports, the University of South Florida IRB does not require IRB oversight/approval per their policy #311. This applies to case reports on three (3) patients or less. Anything over 3 patients requires IRB approval.
Additionally, there is no identifiable patient health information associated with the case report.
Consent
Informed consent has been obtained from the patient and all identifying details have been omitted.
Authors contribution
All authors listed on the paper were involved in the data analysis, interpretation and writing of the paper.
Guarantor
Evan Weitman, MD.
Acknowledgement
Not Applicable.
Contributor Information
Evan Weitman, Email: evan.weitman@moffitt.org.
Sameer Al Diffalha, Email: drsameerdif@yahoo.com.
Barbara Centeno, Email: Barbara.Centeno@moffitt.org.
Pamela Hodul, Email: pamela.hodul@moffitt.org.
References
- 1.Agha R.A. A protocol for the development of reporting criteria for surgical case reports: the SCARE statement. Int. J. Surg. 2016;27:187–189. doi: 10.1016/j.ijsu.2016.01.094. [DOI] [PubMed] [Google Scholar]
- 2.Hata H. Carcinoid tumor arising in a duplication cyst of the duodenum. Pathol. Int. 2006;56(5):272–278. doi: 10.1111/j.1440-1827.2006.01957.x. [DOI] [PubMed] [Google Scholar]
- 3.Prasad T.R., Tan C.E. Duodenal duplication cyst communicating with an aberrant pancreatic duct. Pediatr. Surg. Int. 2005;21(4):320–322. doi: 10.1007/s00383-005-1369-x. [DOI] [PubMed] [Google Scholar]
- 4.Tsai S.D., Sopha S.C., Fishman E.K. Isolated duodenal duplication cyst presenting as a complex solid and cystic mass in the upper abdomen. J. Radiol. Case Rep. 2013;7(11):32–37. doi: 10.3941/jrcr.v7i11.1785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Segal S.R. Ultrasonographic features of gastrointestinal duplications. J. Ultrasound Med. 1994;13(11):863–870. doi: 10.7863/jum.1994.13.11.863. [DOI] [PubMed] [Google Scholar]
- 6.Chen J.J. Meta-analysis: the clinical features of the duodenal duplication cyst. J. Pediatr. Surg. 2010;45(8):1598–1606. doi: 10.1016/j.jpedsurg.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 7.You H.S. A case of duodenal duplication cyst manifested by duodenal polyp. Clin. Endosc. 2012;45(4):425–427. doi: 10.5946/ce.2012.45.4.425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Park J.Y. A completely isolated intestinal duplication cyst mimicking ovarian cyst torsion in an adult. World J. Gastroenterol. 2014;20(2):603–606. doi: 10.3748/wjg.v20.i2.603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Okamoto T. Completely isolated alimentary tract duplication in a neonate. Pediatr. Surg. Int. 2008;24(10):1145–1147. doi: 10.1007/s00383-008-2220-y. [DOI] [PubMed] [Google Scholar]
- 10.Chen M. Sonographic features of ileal duplication cyst at 12 weeks. Prenat. Diagn. 2002;22(12):1067–1070. doi: 10.1002/pd.468. [DOI] [PubMed] [Google Scholar]
- 11.Mandhan P. Noncommunicating multiple intra-abdominal enteric duplication cysts. Afr. J. Paediatr. Surg. 2014;11(3):276–278. doi: 10.4103/0189-6725.137344. [DOI] [PubMed] [Google Scholar]
- 12.Macpherson R.I. Gastrointestinal tract duplications: clinical, pathologic, etiologic, and radiologic considerations. Radiographics. 1993;13(5):1063–1080. doi: 10.1148/radiographics.13.5.8210590. [DOI] [PubMed] [Google Scholar]
- 13.Sinha A., Ojha S., Sarin Y.K. Completely isolated: noncontiguous duplication cyst. Eur. J. Pediatr. Surg. 2006;16(2):127–129. doi: 10.1055/s-2006-924004. [DOI] [PubMed] [Google Scholar]
- 14.Otter M.I., Marks C.G., Cook M.G. An unusual presentation of intestinal duplication with a literature review. Dig. Dis. Sci. 1996;41(3):627–629. doi: 10.1007/BF02282353. [DOI] [PubMed] [Google Scholar]
- 15.van Dam L.J. Case report: intra-uterine demonstration of bowel duplication by ultrasound. Eur. J. Obstet. Gynecol. Reprod. Biol. 1984;18(4):229–232. doi: 10.1016/0028-2243(84)90122-9. [DOI] [PubMed] [Google Scholar]
- 16.Jung K.H. Adenocarcinoma arising in a duplication of the cecum. Korean J. Intern. Med. 2012;27(1):103–106. doi: 10.3904/kjim.2012.27.1.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Blank G. Adenocarcinoma arising in a cystic duplication of the small bowel: case report and review of literature. World J. Surg. Oncol. 2012;10:55. doi: 10.1186/1477-7819-10-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Hsu H. Adenocarcinoma arising from colonic duplication cyst with metastasis to omentum: a case report. J. Clin. Ultrasound. 2011;39(1):41–43. doi: 10.1002/jcu.20739. [DOI] [PubMed] [Google Scholar]
- 19.Ford W.D. Laparoscopic excision of a gastric duplication cyst detected on antenatal ultrasound scan. J. Pediatr. Surg. 2004;39(10):e8–e10. doi: 10.1016/j.jpedsurg.2004.06.044. [DOI] [PubMed] [Google Scholar]
- 20.Kim S.K., Lim H.K., Lee S.J., Park C.K. Completely isolated enteric duplication cyst: case report. Abdom Imaging. 2003;28:12–14. doi: 10.1007/s00261-001-0138-0. [DOI] [PubMed] [Google Scholar]
- 21.Nichols K.C., Pollema T., Moncure M. Laparoscopically excised completely isolated enteric duplication cyst in adult female: a case report. Surg. Laparosc. Endosc. Percutan. Tech. 2011;21:e173–e175. doi: 10.1097/SLE.0b013e318216f301. [DOI] [PubMed] [Google Scholar]
- 22.Lee J.U., KIM J.O., KIM S.J., SUL H.J. Completely isolated enteric duplication cyst presenting as an inguinal hernia. Kor. J. Pathol. 2010;44:204–206. [Google Scholar]
- 23.Kyriakos N., Andreas C., Elena S., Charalampos A., Chrisanthos G. Infected completely isolated enteric duplication cyst management with percutaneous drainage and surgical excision after retreat of infection: a case report. Case. Rep. Surg. 2013;2013:108126. doi: 10.1155/2013/108126. [DOI] [PMC free article] [PubMed] [Google Scholar]