Abstract
The relative importance and use of motor evaluation to diagnose carpal tunnel syndrome (CTS) is not clear. Because the ulnar nerve is not affected in CTS, we evaluated comparing the strength of the median-nerve innervated muscles to the ulnar innervated muscles in the same patient, through manual muscle testing (MMT) and a handheld dynamometer. Our purpose was to evaluate whether this method, which takes into account patient-dependent factors that would affect both groups of muscles equally, can provide better assessment of CTS. A retrospective case-control review of MMT and dynamometer-measured strength for CTS was performed. The study was performed retrospectively but prior to surgery or other treatment. There were 28 cases (CTS) and 14 controls (without CTS). Positive nerve conduction tests defined cases. MMT of the thenar musculature was found to be unreliable as a test for CTS. Comparisons to ulnar nerve innervated muscle strength did not improve sensitivity or specificity of the MMT examination. Use of the dynamometer improved sensitivity and specificity of motor testing in CTS over MMT. Motor evaluation is important for the diagnosis of CTS, but further study is warranted, specifically to define the method of motor evaluation and delineate the subgroup of patients (predominantly thenar motor presentation) that would benefit most from motor testing and motor-focused treatment.
Keywords: carpal tunnel syndrome, diagnosis, dynamometer, motor examination, ulnar
Introduction
The diagnosis of carpal tunnel syndrome (CTS) may remain challenging despite the ubiquity of the condition and the plethora of studies attempting to improve our ability to accurately detect it. 1 2 Various objective, clinical, and electrophysiological tests are used as an aid in diagnosis. 3 4 5 Various diagnostic tools are also required to assess the degree of involvement, need for therapy or surgery, and to document the response to conservative and surgical management. 6
A weak abductor pollicis brevis (APB) in CTS has been reported in up to 94% of patients. 7 8 However, relatively few studies support the motor and muscle strength examination as being better, or at least as good as the sensory examination in defining and quantifying CTS. 6 7 8 9
Some studies defined patients with CTS and a predominantly motor presentation as a separate subgroup of CTS; others believe that motor symptoms appear later than sensory symptoms. Not all cases of CTS actually present with thenar muscle weakness, but it remains unclear whether these are indeed separate groups and whether there is a common natural history. 10 11 12
Manual muscle testing (MMT) of the APB is most often compared with the muscle in the other hand. The nature of the examination renders it examiner dependent, subject to inherent interuser variability, and the APB strength of one hand may not be comparable to the contralateral hand as the strength in the dominant hand may be greater than that in nondominant hand. 13 14 15 Some studies have evaluated interobserver agreement of grip and pinch strengths such as the study by Mathiowtz et al. 16 A study by Brandsma et al evaluated inter- and intraobserver reliability in measuring the intrinsic muscles of the hand. They found that intraobserver reliabilities ranged from 0.71 to 0.96 and interobserver reliabilities from 0.72 to 0.93, depending on the muscle group that was evaluated. Multiple attempts have been made to trial more “objective” manometers to evaluate muscle strength. 17 18 19 20
Because CTS is caused by pressure on the median nerve in the carpal tunnel and the ulnar nerve is not affected, we evaluated comparing MMT of the median-nerve-innervated APB to MMT of the first dorsal interosseous (FDI), supplied by the ulnar nerve, in the same patient. This may take into account patient-dependent factors that would affect both groups of muscles equally and provide better evaluation of CTS. A previous study evaluated quantitative testing of APB strength, using a commercially available handheld strength-testing device in patients with CTS. 21 22
The purpose of this study was to evaluate the specificity and sensitivity of MMT in CTS when comparing the median nerve innervated muscles (thenar musculature) to the ulnar nerve innervated muscles (FDI) in the same hand and to evaluate the utility of the handheld strength-testing device in CTS when comparing the median to the ulnar nerve in the same hand. We hypothesized that comparing muscles innervated by different nerves in the same hand will be more sensitive and specific to diagnose CTS than MMT of the APB in the involved hand alone and that the use of the handheld device would be more sensitive and specific to identify CTS than MMT.
Methods
A review of a cohort of patients with suspected CTS was performed. Fifty-one consecutive adult patients who presented to the hand clinic with a history that was suspicious for CTS were included in the study. Incomplete charts, history of hand surgery, and other injuries to the ulnar or median nerves were excluded from the study as well as evidence of any other neurologic or nerve-related diagnoses. Patients with bilateral symptoms were also excluded. All the patients were evaluated by an experienced board-certified hand surgeon and hand therapist. The diagnosis of CTS was made on the basis of symptomatology, including nighttime numbness and pain, morning stiffness, and by clinical findings including Phalen's test, compression tests, and thenar muscle weakness as well as electrodiagnostic testing. Patients with positive nerve conduction tests (NCTs) and typical signs and symptoms were considered as suffering from CTS whereas those with a negative NCT were considered as not having CTS (controls). Twenty-eight patients had unilateral CTS and 14 patients were used as controls (negative NCT and no typical symptomatology).
Background information obtained for each patient included age, sex, affected side, hand dominance, duration of symptoms, occupation, general medical conditions, and history of any previous diagnosis and/or treatment involving the affected hand. APB strength was tested using the commercially available handheld strength-testing device (Digitrack, J Tech Medical Industries, Heber City, Utah) attached to a portable computerized data storage device (Commander PowerTrack II, J Tech Medical Industries, Heber City, Utah). The instrument was calibrated and certified at the manufacturer with serialized weights traceable to the National Institute of Standards and Technology (NIST). During the period of testing for this study, a calibrated weight was applied to the instrument on a weekly basis to check for any possible error in calibration.
Quantitative APB testing was administered according to standard testing procedures and instructions established in a previous study. 21 The examiner stabilized the hand, while the thumb was positioned in maximum palmar abduction and ulnar rotation in a plane perpendicular to the palm. At the beginning of each trial, the examiner placed the curved aluminum pad of the Digitrack on the radial aspect of the interphalangeal (IP) joint of the thumb, checking for proper placement; that is, that the concave pad was properly placed along the convex part of the radial (lateral) side of the thumb directly at the IP joint. The patient was asked to push against the resistance supplied by the tester with maximal force. During the testing period, the examiner exerted a gradually increasing force against abduction and ulnar rotation until the position of the thumb could no longer be maintained. Duration of testing time was controlled at 3 seconds using audible cues from the testing device. Time between trials was standardized at 10 seconds. During testing, both patient and tester were blinded to the test values. After both the hands were tested, the assessor read and recorded the data stored in the Commander, which included the results of each trial and coefficients of variation (CV). The temporal reproducibility of the test has been established in a previous study. 21 The ulnar nerve was evaluated using the same method but evaluating abduction of the index (FDI muscle) instead of the thumb.
MMT was performed using the index finger of the physician opposing the patients' thumb abduction or index finger abduction (FDI muscle). The same (evaluating) physician performed all tests. MMT was graded using a scale based on resistance only from 0 to 5 (0–1 no resistance, 2–4 decreased resistance, 5 normal).
The sample included 26 females and 16 males, with an age range of 26 to 57 years (54.52 ± 15.4 years). Thirty-seven patients were right-hand dominant, and five were left-hand dominant. Symptoms were present for over 1 year in 56 (90%) of hands tested. Thirty cases were covered under workers' compensation (71%). Most patients were employed; 94% were currently working, and 6% were out of work. Forty percent were employed primarily in computer-related work; 22% were manual workers; and 38% were employed in other types of work, including administrative, sales, health care, and education.
Fourteen patients had right-handed CTS, 14 had left-handed CTS, and 14 patients had a negative NCT and no symptoms typical of CTS as outlined in the methods, and were therefore considered without CTS. The CTS and non-CTS groups are compared in Table 1 . The two groups differed in age but not in any other demographic characteristics. All patients in the CTS group were offered treatment. Our general policy is to trial night splinting in patients with short-term symptoms and surgery when the symptoms have been long standing.
Table 1. Characteristics of study participants with and without CTS as defined by NCT and EMG results.
| CTS n = 28 |
Non-CTS n = 14 |
p Value | |
|---|---|---|---|
| Age | 58.46 ± 16.0 | 46.64 ± 10.6 | 0.017 |
| Sex = male (%) | 10 (36%) | 6 (43%) | 0.653 |
| Occupation = heavy Labor/heavy use of the hands (%) |
14 (50%) | 3 (21.4%) | 0.075 |
| Hand dominance (%) | 25 (89.3%) | 12 (85.7%) | 0.59 |
Abbreviations: CTS, carpal tunnel syndrome; NCT, nerve conduction test.
Note: When the groups are compared, there is a trend toward a difference between the two groups in occupation type with heavy laborers marginally more common in the CTS group.
Statistical Analysis
Data analysis was performed using the SPSS statistical package version 21 (SPSS, Chicago, Illinois, United States). The relationships between categorical characteristics and clinical variables and CTS (as defined by positive NCT) were analyzed with chi-square test.
Continuous variables were evaluated using the t -test or Mann-Whitney tests. Receiver-operating characteristic (ROC) curve was used to determine the DYN APB-level that differed most between positive and negative NCT. The area under the ROC curve (AUC) was computed, and a cutoff point was chosen to have the highest possible sensitivity and specificity.
Logistic regression was performed to evaluate the relative contribution of the different variables to the outcome of CTS. Odds ratios (ORs) with 95% confidence interval (CI) were calculated.
All p values were two-sided, and statistical significance was defined as p < 0.05.
Results
The associations between the different tests and the results of NCT (the gold standard for CTS) are depicted in Table 2 . MMT of the APB of the affected side/unaffected side was not significantly associated with CTS, but the comparison of measurements using the dynamometer was significant when comparing thenar strength between the affected and unaffected side as well as when comparing thenar to ulnar (FDI) strength on the affected side. The association of MMT with NCT results is shown in Table 3 . These values were not statistically significant but seemed to trend toward significance.
Table 2. Relationships between the clinical test and NCT results.
| CTS n = 28 |
Non-CTS n = 14 |
p Value (affected vs. unaffected) | |
|---|---|---|---|
| Mean ± SD median |
Mean ± SD median |
||
| MMT APB-only | 4.51 ± 0.58 5.0 |
4.78 ± 0.42 5.0 |
0.224 |
| MMT FDI-only | 4.55 ± 0.75 5.0 |
4.78 ± 0.42 5.0 |
0.488 |
| MMT APB/FDI ratio | 1.01 ± 0.15 1.0 |
1.0 ± 0.09 1.0 |
0.88 |
| DYN APB-only |
11.46 ± 5.45
b
10.17 |
16.25 ± 5.36
c
16.02 |
0.01 a |
| DYN FDI-only |
14.10 ± 6.91
b
13.58 |
17.68 ± 5.90
c
17.12 |
0.106 |
| DYN APB/FDI ratio | 0.90 ± 0.42 0.83 |
0.98 ± 0.33 0.97 |
0.84 |
Abbreviations: APB, abductor pollicis brevis muscle indicating thenar strength; DYN, use of the dynamometer to evaluate thenar strength; FDI, first dorsal interosseous muscle indicating ulnar strength; MMT, manual muscle testing; NCT, nerve conduction testing; SD, standard deviation.
A significant relationship: dynamometer for thenar strength affected versus unaffected side.
Comparisons within the same hand:
DYN APB versus DYN FDI within Affected Hand: p = 0.007.
DYN APB versus DYN FDI within the unaffected hand: p = 0.28.
It is possible that we were underpowered to detect differences.
Table 3. Association of MMT with NCT results.
| Affected hand-only | Unaffected | p Value (affected vs. unaffected) | |
|---|---|---|---|
| MMT APB-only | |||
| < 5 | 12 (43.0%) | 3 (21.4%) | 0.172 |
| = 5 | 16 (57.0%) | 11 (78.6%) | |
| MMT FDI-only | |||
| < 5 | 9 (32.0%) | 3 (21.4%) | 0.470 |
| = 5 | 19 (68.0%) | 11 (78.6%) | |
Abbreviations: APB, abductor pollicis brevis muscle indicating thenar strength; FDI, first dorsal interosseous muscle indicating ulnar strength; MMT, manual muscle testing; NCT, nerve conduction testing.
Note: MMT was graded using a scale based on resistance only from 0 to 5 (0–1 no resistance, 2–4 decreased resistance, 5 normal).
The ROC analysis is illustrated in Fig. 1 . The area under the curve was 0.75 ± 0.075, 95% CI (0.61–0.90), p = 0.008. Logistic regression was performed for thenar motor evaluation by the dynamometer adjusted for age and sex. The cutoff point to give optimal sensitivity and specificity using the ROC curve was found to be 14 lb; a thenar measured strength of ≥ 14 lb was found to be significantly related to CTS (OR = 5.53 95% CI: 1.01–30.3) ( p = 0.49).
Fig. 1.
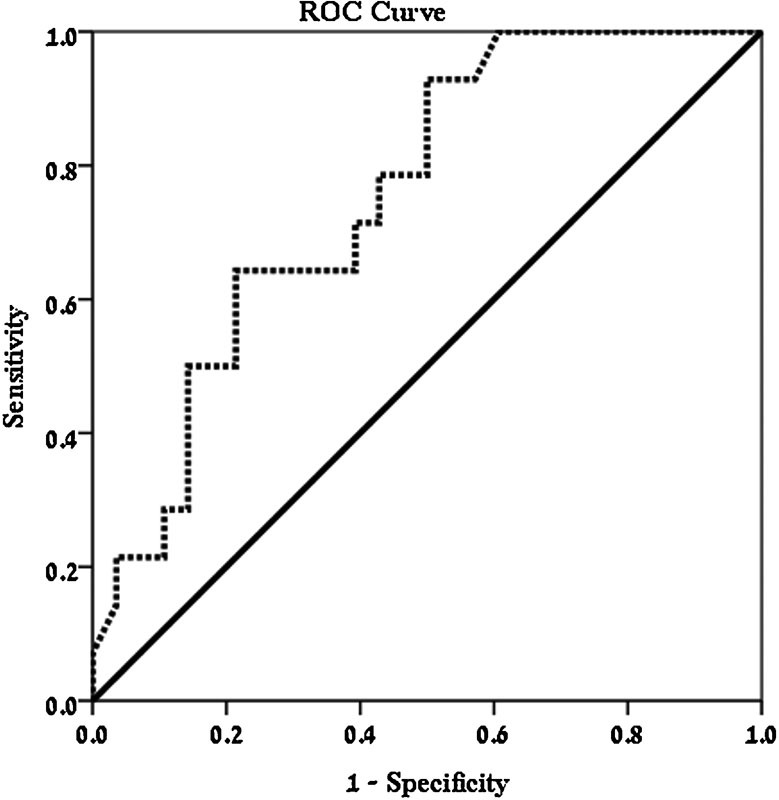
The receiver-operating characteristic (ROC) analysis of the results.
Discussion
Because CTS is so common and causes significant morbidity, it is especially relevant to physicians and hand surgeons, in particular, to try and optimize its diagnosis and treatment. Recently, multiple studies have been performed evaluating the cost-effectiveness of anesthesia and surgical procedure type in the treatment of CTS. 23 24 25 Other studies have evaluated the effect of accurate diagnosis. 26
The best method to diagnose CTS has long been debated in the literature. 27 28 Sometimes considered an occupational condition, the need for a standardized, objective, and reliable diagnostic tool has not consistently been met. NCT and electromyography (EMG), though considered the gold standard for the diagnosis of CTS, have significant limitations and are even considered by some researchers as unnecessary in the face of clear and characteristic clinical symptoms and signs. 3 Multiple studies have examined methods for improving the specificity and sensitivity of NCT and EMG, whereas others have examined different modalities such as ultrasonography and magnetic resonance imaging (MRI). 11 29 30 31 32 Ultrasound has recently been used, allowing the technician to demonstrate flattening of the median nerve within the carpal tunnel. Some studies have supported its use to indicate surgery when there are persisting pain and dysesthesia despite conservative measures and a normal NCT and EMG. 33 34 Other studies have targeted clinical evaluation methods and provocative testing. 35 36
In this study MMT of the thenar musculature was found to be unreliable as a test for CTS. Furthermore, comparisons to ulnar nerve innervated strength did not improve the sensitivity or specificity of the MMT examination ( Table 3 ). Though we did not find significance, it is possible that this study was underpowered to find differences in MMT. However, in tandem with our findings, Brown et al found minimal clinical thenar motor loss despite a significant loss in motor neurons. 37 Because we did find a significant relationship with motor testing using the dynamometer (even when correcting for age and gender), it is not clear whether the lack of relationship of MMT stems from the fact that motor evaluation in general is not always sensitive or specific for CTS or whether the reason lies with the way MMT was performed in this study. Because MMT subjectively compares thenar strength to the examiner's strength, it may not be a good test for detecting CTS. Furthermore, this may not be reliable in patients with concomitant median and ulnar nerve compression. Handheld dynamometer assessment also does not take into account thumb CMC symptoms (sometimes asymptomatic OA), which may affect thenar muscle power testing while FDI strength would remain unaffected. The existence of aberrant connections between the ulnar and median nerves (e.g., Riche-Cannieu and Martin Gruber) would affect the clinical presentation as well as the examination. We did not have any cases as identified by NCT and EMG examinations.
Mondelli et al finding predominant loss of motor fibers in vineyard workers actually classified these as a different type of CTS. 38 We believe that it is most likely that some patients present with predominantly motor signs and symptoms whereas others present with a more sensory presentation. If indeed there is a separate “predominantly motor” subgroup, perhaps a different therapeutic approach may be indicated, such as exercises that have been described to decompress the carpal tunnel by pulling the lumbricals out of the carpal tunnel or exercises aimed at muscle strengthening. 39 40 However, the characterization of each group has not yet been elucidated.
The handheld dynamometer used in this study has been validated in previous studies. 21 41 The potential disadvantage of this dynamometer is that it is handheld and therefore possibly includes examiner/operator factors in the results. Schrama et al found that results of intraexaminer reliability across multiple studies using handheld dynamometry for the upper extremity were not consistently acceptable. 42 Other dynamometers have also been examined, such as the Rotterdam Intrinsic Hand Myometer (RIHM), and found to be reliable and comparable in accuracy to other strength dynamometers in distinct populations such as children. 43 44
The comparison of APB strength (median) to FDI (ulnar) testing was helpful in detecting CTS only when performing the comparison in the affected hand using the dynamometer. This comparison may be helpful clinically in identifying a subgroup of patients with significant motor weakness, as well as quantifying the amount of motor loss. 26
The main limitations of this study stem from its retrospective nature. We had 36% males since the study was performed in a “blue collar” area with a relatively high percentage of laborers. This is a high percentage of males compared with some studies, but younger male laborers are also considered at risk for the development of CTS and so we assume our population was representative of most CTS populations. 45 46 47 48 We also did not always have information regarding severity of CTS according to examination and NCT/EMG. Furthermore, the testing was done in different places by different examiners so it is not clear what value there would be to a comparison.
Though the order of the examination was usually the same (the history was taken first, then the manual examination and then the testing using the manometer) and though most patients in the study were sent by the physician for NCT and EMG testing, it is possible that some of the patients presented with an NCT and EMG examination at their first encounter, causing a bias that we were unable to identify due to the retrospective nature of the study. We also did not have information in this study to evaluate any correlations between weakness and thenar muscle wasting. Isolated thenar muscle wasting and weakness should warrant a search for a cause other than CTS with only motor signs, such as osteoarthritis or neurological disease.
CTS is commonly bilateral though not necessarily at the same time or to the same degree. Padua et al found an 87% incidence and Goyal et al found 91.4% bilaterality in their series of patients with CTS. 49 50 This study only identified patients with unilateral CTS at the time of presentation. It is possible that this affected our MMT and dynamometer comparisons between both hands of the patients, but it is uncertain that muscle weakness precedes the appearance of symptoms and positive findings on NCT and EMG.
Though our gold standard of NCT and EMG is considered the most sensitive and specific for the existence of CTS, it is still a limited examination, sometimes being at odds with the patient's physical examination and history. It is possible that using NCT and EMG results to differentiate between cases and controls affects our results as pertaining to the true occurrence of CTS and consequently the utility of the physical examinations. Furthermore, this examination does not supply qualifying information on characteristics such as severity and anatomical distribution. As already stated, it is possible that the comparison to ulnar innervated muscles adds sensitivity and specificity to the test only when performed in the affected hand with a dynamometer, but it may add qualifying information such as severity even when performed manually. For example, a thenar MMT of 4/5 in a hand with ulnar MMT of 4/5 is conceivably less severe than finding a thenar MMT of 45 in a hand with 5/5 ulnar MMT.
In summary, the use of motor testing in the diagnosis of CTS is beneficial, but it warrants further study, specifically to define the subgroups that would benefit most from motor testing as well as to define those patients who may profit most from treatment, both surgical and therapeutic, to strengthen the intrinsic musculature. This distinction may be important especially because motor recovery may be more limited and more time sensitive than sensory recovery. In general, this knowledge can help improve our ability to objectively diagnose this multifactorial and common condition.
References
- 1.Foresti C, Quadri S, Rasella M, Tironi F, Viscardi M, Ubiali E. Carpal tunnel syndrome: which electrodiagnostic path should we follow? A prospective study of 100 consecutive patients. Electromyogr Clin Neurophysiol. 1996;36(06):377–384. [PubMed] [Google Scholar]
- 2.Shimizu S, Tachibana S, Fujii K. Difficulty of pinching behind the back: an atypical symptom of carpal tunnel syndrome related to a specific wrist position. Two case reports. Neurol Med Chir (Tokyo) 2012;52(04):229–230. doi: 10.2176/nmc.52.229. [DOI] [PubMed] [Google Scholar]
- 3.Spindler H A, Dellon A L. Nerve conduction studies and sensibility testing in carpal tunnel syndrome. J Hand Surg Am. 1982;7(03):260–263. doi: 10.1016/s0363-5023(82)80176-7. [DOI] [PubMed] [Google Scholar]
- 4.Sohn M W, Whittle J, Pezzin L E, Miao H, Dillingham T R. Electrodiagnostic consultation and identification of neuromuscular conditions in persons with diabetes. Muscle Nerve. 2011;43(06):812–817. doi: 10.1002/mus.22003. [DOI] [PubMed] [Google Scholar]
- 5.Visser L H, Smidt M H, Lee M L. High-resolution sonography versus EMG in the diagnosis of carpal tunnel syndrome. J Neurol Neurosurg Psychiatry. 2008;79(01):63–67. doi: 10.1136/jnnp.2007.115337. [DOI] [PubMed] [Google Scholar]
- 6.Fowler J R, Munsch M, Huang Y, Hagberg W C, Imbriglia J E. Pre-operative electrodiagnostic testing predicts time to resolution of symptoms after carpal tunnel release. J Hand Surg Eur Vol. 2016;41(02):137–142. doi: 10.1177/1753193415576248. [DOI] [PubMed] [Google Scholar]
- 7.Rozmaryn L M, Bartko J J, Isler M L.The Ab-Adductometer: a new device for measuring the muscle strength and function of the thumb J Hand Ther 20072004311–324., quiz 325 [DOI] [PubMed] [Google Scholar]
- 8.Geere J, Chester R, Kale S, Jerosch-Herold C.Power grip, pinch grip, manual muscle testing or thenar atrophy—which should be assessed as a motor outcome after carpal tunnel decompression? A systematic review BMC Musculoskelet Disord 20078114. Doi: 10.1186/1471-2474-8-114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Keith M W, Masear V, Chung K et al. Diagnosis of carpal tunnel syndrome. J Am Acad Orthop Surg. 2009;17(06):389–396. doi: 10.5435/00124635-200906000-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mondelli M, Aretini A, Ginanneschi F, Padua L. Thenar motor neuropathy electrophysiological study of 28 cases. J Clin Neurophysiol. 2010;27(05):344–349. doi: 10.1097/WNP.0b013e3181f386a6. [DOI] [PubMed] [Google Scholar]
- 11.Inukai T, Uchida K, Kubota C, Takamura T, Nakajima H, Baba H. Second lumbrical-interossei nerve test predicts clinical severity and surgical outcome of carpal tunnel syndrome. J Clin Neurosci. 2013;20(09):1224–1227. doi: 10.1016/j.jocn.2012.10.041. [DOI] [PubMed] [Google Scholar]
- 12.Danoff J R, Birman M V, Rosenwasser M P. Transfer of the flexor carpi radialis to the abductor pollicis brevis tendon for the restoration of tip-pinch in severe carpal tunnel syndrome. J Hand Surg Eur Vol. 2014;39(02):175–180. doi: 10.1177/1753193413481303. [DOI] [PubMed] [Google Scholar]
- 13.de Krom M C, Knipschild P G, Kester A D, Spaans F.Efficacy of provocative tests for diagnosis of carpal tunnel syndrome Lancet 1990335(8686):393–395. [DOI] [PubMed] [Google Scholar]
- 14.Bohannon R W. Manual muscle testing: does it meet the standards of an adequate screening test? Clin Rehabil. 2005;19(06):662–667. doi: 10.1191/0269215505cr873oa. [DOI] [PubMed] [Google Scholar]
- 15.Bohannon R W. Internal consistency of manual muscle testing scores. Percept Mot Skills. 1997;85(02):736–738. doi: 10.2466/pms.1997.85.2.736. [DOI] [PubMed] [Google Scholar]
- 16.Mathiowetz V, Weber K, Volland G, Kashman N. Reliability and validity of grip and pinch strength evaluations. J Hand Surg Am. 1984;9(02):222–226. doi: 10.1016/s0363-5023(84)80146-x. [DOI] [PubMed] [Google Scholar]
- 17.Bohannon R W. Hand-held compared with isokinetic dynamometry for measurement of static knee extension torque (parallel reliability of dynamometers) Clin Phys Physiol Meas. 1990;11(03):217–222. doi: 10.1088/0143-0815/11/3/004. [DOI] [PubMed] [Google Scholar]
- 18.Bohannon R W, Andrews A W. Interrater reliability of hand-held dynamometry. Phys Ther. 1987;67(06):931–933. doi: 10.1093/ptj/67.6.931. [DOI] [PubMed] [Google Scholar]
- 19.Brandsma J W, Schreuders T A, Birke J A, Piefer A, Oostendorp R. Manual muscle strength testing: intraobserver and interobserver reliabilities for the intrinsic muscles of the hand. J Hand Ther. 1995;8(03):185–190. doi: 10.1016/s0894-1130(12)80014-7. [DOI] [PubMed] [Google Scholar]
- 20.Brandsma J W, Schreuders T A. Sensible manual muscle strength testing to evaluate and monitor strength of the intrinsic muscles of the hand: a commentary. J Hand Ther. 2001;14(04):273–278. doi: 10.1016/s0894-1130(01)80005-3. [DOI] [PubMed] [Google Scholar]
- 21.Liu F, Carlson L, Watson H K. Quantitative abductor pollicis brevis strength testing: reliability and normative values. J Hand Surg Am. 2000;25(04):752–759. doi: 10.1053/jhsu.2000.6462. [DOI] [PubMed] [Google Scholar]
- 22.Liu C W, Chen T W, Wang M C, Chen C H, Lee C L, Huang M H. Relationship between carpal tunnel syndrome and wrist angle in computer workers. Kaohsiung J Med Sci. 2003;19(12):617–623. doi: 10.1016/S1607-551X(09)70515-7. [DOI] [PubMed] [Google Scholar]
- 23.Rhee P C, Fischer M M, Rhee L S, McMillan H, Johnson A E. Cost savings and patient experiences of a clinic-based, wide-awake hand surgery program at a military medical center: a critical analysis of the first 100 procedures. J Hand Surg Am. 2017;42(03):e139–e147. doi: 10.1016/j.jhsa.2016.11.019. [DOI] [PubMed] [Google Scholar]
- 24.Ren Y M, Wang X S, Wei Z Jet al. Efficacy, safety, and cost of surgical versus nonsurgical treatment for carpal tunnel syndrome: a systematic review and meta-analysis Medicine (Baltimore) 20169540e4857. Doi: 10.1097/MD.0000000000004857 [DOI] [PMC free article] [PubMed] [Google Scholar] [Retracted]
- 25.Zhang S, Vora M, Harris A H, Baker L, Curtin C, Kamal R N. Cost-minimization analysis of open and endoscopic carpal tunnel release. J Bone Joint Surg Am. 2016;98(23):1970–1977. doi: 10.2106/JBJS.16.00121. [DOI] [PubMed] [Google Scholar]
- 26.Conlon C, Asch S, Hanson M et al. Assessing the value of high-quality care for work-associated carpal tunnel syndrome in a large integrated health care system: study design. Perm J. 2016;20(04):87–95. doi: 10.7812/TPP/15-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Vahdatpour B, Khosrawi S, Chatraei M.The role of median nerve terminal latency index in the diagnosis of carpal tunnel syndrome in comparison with other electrodiagnostic parameters Adv Biomed Res 20165110. Doi: 10.4103/2277-9175.183671 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ten Cate D F, Glaser N, Luime J J et al. A comparison between ultrasonographic, surgical and histological assessment of tenosynovits in a cohort of idiopathic carpal tunnel syndrome patients. Clin Rheumatol. 2016;35(03):775–780. doi: 10.1007/s10067-014-2720-1. [DOI] [PubMed] [Google Scholar]
- 29.Yagci I, Gunduz O H, Sancak S, Agirman M, Mesci E, Akyuz G. Comparative electrophysiological techniques in the diagnosis of carpal tunnel syndrome in patients with diabetic polyneuropathy. Diabetes Res Clin Pract. 2010;88(02):157–163. doi: 10.1016/j.diabres.2010.02.011. [DOI] [PubMed] [Google Scholar]
- 30.Zalaffi A, Mariottini A, Carangelo B et al. Wrist median nerve motor conduction after end range repeated flexion and extension passive movements in carpal tunnel syndrome. Pilot study. Acta Neurochir Suppl (Wien) 2005;92:47–52. doi: 10.1007/3-211-27458-8_11. [DOI] [PubMed] [Google Scholar]
- 31.Yildiz N, Atalay N S, Gungen G O, Sanal E, Akkaya N, Topuz O. Comparison of ultrasound and ketoprofen phonophoresis in the treatment of carpal tunnel syndrome. J Back Musculoskeletal Rehabil. 2011;24(01):39–47. doi: 10.3233/BMR-2011-0273. [DOI] [PubMed] [Google Scholar]
- 32.Watanabe T, Ito H, Morita A et al. Sonographic evaluation of the median nerve in diabetic patients: comparison with nerve conduction studies. J Ultrasound Med. 2009;28(06):727–734. doi: 10.7863/jum.2009.28.6.727. [DOI] [PubMed] [Google Scholar]
- 33.Lee K M, Kim H J. Relationship between electrodiagnosis and various ultrasonographic findings for diagnosis of carpal tunnel syndrome. Ann Rehabil Med. 2016;40(06):1040–1047. doi: 10.5535/arm.2016.40.6.1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kolovos S, Tsiotas D. Ultrasonographic diagnosis of carpal tunnel syndrome: introducing a new approach. Eur J Orthop Surg Traumatol. 2016;26(02):167–175. doi: 10.1007/s00590-015-1728-9. [DOI] [PubMed] [Google Scholar]
- 35.Makanji H S, Becker S J, Mudgal C S, Jupiter J B, Ring D. Evaluation of the scratch collapse test for the diagnosis of carpal tunnel syndrome. J Hand Surg Eur Vol. 2014;39(02):181–186. doi: 10.1177/1753193413497191. [DOI] [PubMed] [Google Scholar]
- 36.Boland R A, Kiernan M C. Assessing the accuracy of a combination of clinical tests for identifying carpal tunnel syndrome. J Clin Neurosci. 2009;16(07):929–933. doi: 10.1016/j.jocn.2008.09.004. [DOI] [PubMed] [Google Scholar]
- 37.Brown W F. Thenar motor unit count estimates in the carpal tunnel syndrome. J Neurol Neurosurg Psychiatry. 1973;36(02):194–198. doi: 10.1136/jnnp.36.2.194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mondelli M, Baldasseroni A, Aretini A, Ginanneschi F, Padua L. Prevalent involvement of thenar motor fibres in vineyard workers with carpal tunnel syndrome. Clin Neurophysiol. 2010;121(08):1251–1255. doi: 10.1016/j.clinph.2010.02.150. [DOI] [PubMed] [Google Scholar]
- 39.Cobb T K, An K N, Cooney W P, Berger R A. Lumbrical muscle incursion into the carpal tunnel during finger flexion. J Hand Surg [Br] 1994;19(04):434–438. doi: 10.1016/0266-7681(94)90206-2. [DOI] [PubMed] [Google Scholar]
- 40.Baker N A, Moehling K K, Rubinstein E N, Wollstein R, Gustafson N P, Baratz M. The comparative effectiveness of combined lumbrical muscle splints and stretches on symptoms and function in carpal tunnel syndrome. Arch Phys Med Rehabil. 2012;93(01):1–10. doi: 10.1016/j.apmr.2011.08.013. [DOI] [PubMed] [Google Scholar]
- 41.Liu F, Watson H K, Carlson L, Lown I, Wollstein R. Use of quantitative abductor pollicis brevis strength testing in patients with carpal tunnel syndrome. Plast Reconstr Surg. 2007;119(04):1277–1283. doi: 10.1097/01.prs.0000254498.49588.2d. [DOI] [PubMed] [Google Scholar]
- 42.Schrama P P, Stenneberg M S, Lucas C, van Trijffel E. Intraexaminer reliability of hand-held dynamometry in the upper extremity: a systematic review. Arch Phys Med Rehabil. 2014;95(12):2444–2469. doi: 10.1016/j.apmr.2014.05.019. [DOI] [PubMed] [Google Scholar]
- 43.Molenaar H M, Selles R W, Schreuders T A, Hovius S E, Stam H J. Reliability of hand strength measurements using the Rotterdam Intrinsic Hand Myometer in children. J Hand Surg Am. 2008;33(10):1796–1801. doi: 10.1016/j.jhsa.2008.07.018. [DOI] [PubMed] [Google Scholar]
- 44.Molenaar H M, Selles R W, de Kraker M, Stam H J, Hovius S E. The added value of measuring thumb and finger strength when comparing strength measurements in hypoplastic thumb patients. Clin Biomech (Bristol, Avon) 2013;28(08):879–885. doi: 10.1016/j.clinbiomech.2013.07.011. [DOI] [PubMed] [Google Scholar]
- 45.Jenkins P J, Srikantharajah D, Duckworth A D, Watts A C, McEachan J E. Carpal tunnel syndrome: the association with occupation at a population level. J Hand Surg Eur Vol. 2013;38(01):67–72. doi: 10.1177/1753193412455790. [DOI] [PubMed] [Google Scholar]
- 46.Raman S R, Al-Halabi B, Hamdan E, Landry M D.Prevalence and risk factors associated with self-reported carpal tunnel syndrome (CTS) among office workers in Kuwait BMC Res Notes 20125289. Doi: 10.1186/1756-0500-5-289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Abumunaser L A. Demographic pattern of carpal tunnel syndrome in western Saudi Arabia. Neurosciences (Riyadh) 2012;17(01):44–47. [PubMed] [Google Scholar]
- 48.Mondelli M, Giannini F, Giacchi M. Carpal tunnel syndrome incidence in a general population. Neurology. 2002;58(02):289–294. doi: 10.1212/wnl.58.2.289. [DOI] [PubMed] [Google Scholar]
- 49.Goyal V, Bhatia M, Padma M V, Jain S, Maheshwari M C. Electrophysiological evaluation of 140 hands with carpal tunnel syndrome. J Assoc Physicians India. 2001;49:1070–1073. [PubMed] [Google Scholar]
- 50.Padua L, Padua R, Nazzaro M, Tonali P. Incidence of bilateral symptoms in carpal tunnel syndrome. J Hand Surg [Br] 1998;23(05):603–606. doi: 10.1016/s0266-7681(98)80010-7. [DOI] [PubMed] [Google Scholar]


