Abstract
Basic knowledge of human reproduction can help youth prepare for puberty and make later classes focused on advanced reproductive health topics manageable. With the intention of potentially informing the creation of learning materials, we conducted a needs assessment among children ages 7 to 12 in our suburban Chicago community to ascertain their current understanding of, and beliefs and misconceptions about, human reproduction, and to determine their needs for additional reproductive health education. We held qualitative focus group interviews with local children. Participants primarily reported learning about these topics from their parents prior to receiving school-based education in fifth grade. Their level of understanding was relatively low. They had little knowledge of internal sexual organs, expressed a range of beliefs about conception ranging from inaccurate to accurate but incomplete, and voiced concerns about transitioning into adolescence. This suggests a need for additional resources that provide comprehensible descriptions of reproductive health processes and mitigate puberty-related concerns.
Keywords: reproduction, conception, puberty, reproductive anatomy, menstruation
Children first may begin exhibiting signs of puberty (e.g., pubic hair growth) at around ages 8 to 11 (Dixon-Mueller, 2008; J. D. G. Goldman, 2011; Himes, 2006). Youth who enter puberty with a strong understanding of human reproduction are more emotionally and intellectually equipped for impending physical changes (Brooks-Gunn, 1984; Winn, Roker, & Coleman, 1995) and later sexual health decision-making (J. D. G. Goldman, 2011; Koo, Rose, Bhaskar, & Walker, 2011; United Nations Educational, Scientific and Cultural Organization [UNESCO], 2009; Winn et al., 1995). Unfortunately, many existing youth-targeted educational materials fail to provide sufficiently detailed information on all relevant topics (Erchull, Chrisler, Gorman, & Johnston-Robledo, 2002; Fields, 2008; Whiteley, Mello, Hunt, & Brown, 2012). Improving the quality of these materials is challenging because much of the research on children’s knowledge in these areas is fairly dated (e.g., Bernstein & Cowan, 1975; R. J. Goldman & Goldman, 1982; Whisnant & Zegans, 1975).
An interdisciplinary team at our university is developing more extensive and comprehensive educational materials to teach children ages 7 to 12 in our community (suburban Chicago, Illinois) about reproductive health. To support the development of these materials, we conducted a needs assessment (see Rossi, Lipsey, & Freeman, 2003) to determine if the children in our community are in need of additional reproductive health education by better understanding the experiences they already have had learning about these topics and the knowledge they have gained from these experiences.
Children’s Experiences Learning About Reproductive Health
Many policymakers and educational experts are becoming increasingly supportive of providing prepubescent children with human reproduction education. In fact, the U.S. federal government has increased the amount of funding provided for reproductive health education exponentially over the past decade (Sexuality Information and Education Council of the United States [SIECUS], 2010), with over US$250 million in federal monies spent on sexual education programs in 2014 alone (SIECUS, 2014).
In conjunction with increased funding, numerous groups such as the United Nations Organization for Education, Science, and Culture (UNESCO, 2009), the Sexuality Information and Education Council of the United States (SIECUS, 2004), and the Future of Sex Initiative (Future of Sex Education Initiative [FoSE], 2012), have created K-12 sexual health learning standards. These guidelines recommend that between the ages of 5 and 8, children learn basic information about reproductive anatomy (FoSE, 2012; SIECUS, 2004; UNESCO, 2009), changes that occur during puberty (SIECUS, 2004; UNESCO, 2009), and the role sperm and ova play in conception (SIECUS, 2004; UNESCO, 2009). By age 12, the standards suggest children should understand the processes of menstruation and sperm production (SIECUS, 2004; UNESCO, 2009), be accepting of individual differences in pubertal timing, and know where to find medically accurate information about these topics (FoSE, 2012). They recommend teachers find ways to make instruction personally relevant to students (FoSE, 2012) and procure learning materials to help students achieve standards (FoSE, 2012; SIECUS, 2004; UNESCO, 2009). There is much variance in terms of how school curricula reflect these standards: Some U.S. school districts use K-12 reproductive health curricula (e.g., Chicago Public Schools, 2013), others provide limited information to children in select district-determined grades, and still others do not offer any sexual or reproductive health education (Guttmacher Institute, 2015; Landry, Singh, & Darroch, 2000). Nationally, by the time they reach the age of 15, only about half of youth report having taken a class covering reproductive health or other health topics (Wartella, Rideout, Zupancic, Ryan, & Lauricella, 2015).
Preceding or complementing these school-based efforts, many parents teach their children about human reproduction. Indeed, both experts (American Academy of Pediatrics, 2001) and parents themselves (KRC Research & Consulting, 1991b) believe that parents should be children’s first sexual education teachers before they receive formal education in schools. Accordingly, some parents begin teaching their children about topics such as menarche and sexual intercourse as young as age 2 (Haglund, 2006), with most parents believing such conversations should be initiated around age 9 (El-Shaieb & Wurtele, 2009; Haglund, 2006). Nonetheless, many parents feel uncomfortable talking to their children about reproductive health, which may in part be attributable to parents themselves not being confident in their own reproductive health knowledge (Fisher, 1986; UNESCO, 2009), and which may limit their effectiveness as sexual health educators (El-Shaieb & Wurtele, 2009).
Conceptual Understanding of Puberty and Human Reproduction
Preadolescent children’s knowledge and concerns about puberty and human reproduction may vary greatly, especially in light of how variable sexual educational experiences are in the United States. Unfortunately, the body of literature reviewing children’s knowledge of and concerns about reproductive health topics is quite small, perhaps because it can be challenging to recruit for studies in this domain, particularly in the United States (J. D. G. Goldman, 1994). With a few exceptions (e.g., R. J. Goldman & Goldman, 1982; KRC Research & Consulting, 1991a), most studies on this topic were conducted at one time point in single communities, with small samples in the range of approximately 10 to 40 participants per community. Moreover, the majority of studies on this topic are rather dated; almost every study we review was conducted during the late 20th century before recent increases in Internet access among families with school-age children (Rideout, Foehr, & Roberts, 2010) and funding as described above (SIECUS, 2010). Although the present study is plagued by some similar limitations, our results can help to triangulate and build on existing research.
Reproductive Anatomy
Scholarship in human biology education suggests having familiarity with body structures is integral to having a holistic understanding of body system functionality (Hmelo-Silver & Azevedo, 2006). In addition, experts in human reproduction education specifically recommend that children begin learning about reproductive anatomy by age 8, prior to being exposed to more advanced topics in this domain (UNESCO, 2009).
According to past scholarship, children’s understanding of reproductive anatomy varied across the reproductive system. They were more familiar with certain organs such as the penis (Gartrell & Mosbacher, 1984; KRC Research & Consulting, 1991a; Schor & Sivan, 1989) compared with other areas like the vulva (Gartrell & Mosbacher, 1984). It might be that parents privileged terms such as “penis” over other labels for genitalia (Martin, Verduzco Baker, Torres, & Luke, 2011). Sometimes children’s knowledge of these terms lacked specificity; for example, some were taught that the word “vagina” refers to the urethral opening or vulva (Gartrell & Mosbacher, 1984). And children exhibited confusion over the exact location and appearance of various components of the reproductive tract (Gartrell & Mosbacher, 1984; R. J. Goldman & Goldman, 1982; KRC Research & Consulting, 1991a; Whisnant & Zegans, 1975). Familiarity with other internal body parts may have been even lower than these articles indicate; we are unaware of any study that has questioned children about parts such as the cervix or urethra.
Puberty and Menstruation
The average age of menarche is 12 and spermarche 13, with first signs of puberty beginning a few years in advance of these milestones (Jorgensen, Keiding, & Skakkebaek, 1991; Walvoord, 2010). Research suggests that the onset of puberty and major pubertal milestones can be anxiety-provoking, especially for girls (KRC Research & Consulting, 1991a; Stubbs, 2008; Stubbs, Rierdan, & Koff, 1989; Whisnant & Zegans, 1975). Girls who achieve menarche earlier than their peers are at greater risk for depression and anxiety (Carter, 2014; Walvoord, 2010), which may stem in part from these girls entering puberty before fully understanding what is happening to their bodies (Brooks-Gunn, 1984; Walvoord, 2010). Therefore, experts recommend that children possess relatively detailed knowledge about puberty and some knowledge about menstruation by age 12 (e.g., UNESCO, 2009).
In prior scholarship, prepubescent children knew more about puberty than other aspects of reproductive health (Winn et al., 1995). That said, not all third to sixth graders in those studies were even familiar with the term puberty (KRC Research & Consulting, 1991a). Those who did know the term associated it with primary sexual changes such as menarche and secondary sexual developments such as voice changes for males, hair growth, and acne (KRC Research & Consulting, 1991a). Concerning menarche specifically, girls understood that menstruation involves unfertilized ova (Stubbs, 2008; Whisnant & Zegans, 1975). However, many were unaware of the nuances of related processes, such as the timing of menarche (Whisnant & Zegans, 1975).
Conception
Experts recommend that children learn basic information about human conception between the ages 5 and 8 (e.g., SIECUS, 2004). After all, as with reproductive anatomy, experts believe that learning the mechanics of human fertilization and conception can facilitate later learning about more advanced topics, such as the efficacy of abstinence and various methods of contraception (UNESCO, 2009). Moreover, in the United States, interest in teaching children about human reproduction has in large part historically been linked to concerns about unplanned adolescent pregnancy (SIECUS, 2010), and therefore many individuals in the United States may assume that education in human reproduction at any age will at least touch on topics such as fertilization, conception, and pregnancy.
Children’s understanding of conception has received more scholarly attention than other aspects of human reproduction. Some of children’s explanations about human conception in prior studies were completely inaccurate. For example, some children thought mothers must eat something special to begin growing babies in their stomachs (Berends & Caron, 1994). In contrast, many children understood that a sexual act was involved in the conception of a baby (Bernstein & Cowan, 1975; R. J. Goldman & Goldman, 1982; KRC Research & Consulting, 1991a), and some understood that sperm fertilize ova (Berends & Caron, 1994; Bernstein & Cowan, 1975; R. J. Goldman & Goldman, 1982; KRC Research & Consulting, 1991a). However, many children were unable to articulate the precise relationship between sexual acts, sperm, and ova; that is, they did not understand exactly what a sexual act entails, how sperm enter females, and/or where ova are located (Bernstein & Cowan, 1975; R. J. Goldman & Goldman, 1982; Haglund, 2006; KRC Research & Consulting, 1991a).
Current Study
To gain a better understanding of the experiences children ages 7 to 12 in our community have had learning about human reproduction, and to inform the potential development of learning materials and future scholarship in this domain, we conducted qualitative focus group interviews with children ages 7 to 12 in our community, segmenting groups by age and gender. These groups addressed the following research questions:
Research Question 1: How do children ages 7 to 12 in our suburban Chicago community learn about human reproduction? From whom do they learn this information: teachers, friends, parents, other relatives, or some combination of these sources?
Research Question 2: What do children in our community know about (a) reproductive anatomy, (b) puberty and menstruation, and (c) human conception?
Method
Because the goal of this study was exploratory and because of the potentially sensitive nature of these topics, we conducted qualitative focus group interviews stratified by age and gender to increase comfort. Focus group interviews have been recommended as an ideal methodology for needs assessment in general (Rossi et al., 2003), and focus group interviews segmented by age and gender have been suggested in previous scholarship on related topics (KRC Research & Consulting, 1991a; UNESCO, 2009).
Participants
A total of 19 children ages 7 to 12 participated in four qualitative focus group interviews (see Table 1). This was a convenience sample, with suburban Chicago families recruited through flyers, Craigslist postings, personal referrals, and commercial lists. An effort was made to recruit throughout our community so that the racial composition of our sample would roughly mirror the racial composition of our community (43% Caucasian according to the U.S. Census Bureau). As compensation for their participation in the study, children received US$50 Visa gift cards, and their parents received US$25 Visa gift cards.
Table 1.
Demographic Composition of Each Focus Group Interview.
| Group | n | Age
|
No. of children in home
|
Parent race-ethnicitya | Parent educationa | ||
|---|---|---|---|---|---|---|---|
| X̄ | SD | X̄ | SD | ||||
| Girls ages 7–9 | 5 | 8.28 | 1.01 | 2.20 | 0.45 | 2 Caucasians, 2 Latinos, 1 African American | 3 college degrees, 3 post-college |
| Girls ages 10–12 | 5 | 10.74 | 0.67 | 2.00 | 1.22 | 2 Caucasians, 2 Latinos, 1 African American | 1 associates degree, 2 college degrees |
| Boys ages 7–9b | 5 | 8.81 | 0.70 | 2.67 | 0.55 | 2 Caucasians, 3 Latinos | 1 less than college, 3 college degrees |
| Boys ages 10–12 | 4 | 12.16 | 0.62 | 2.00 | 0.00 | 3 Caucasians, 1 African American | 1 less than college, 3 post-college |
Note. Means and standard deviations for age (in years) and number of children in household for each group and tallies of race-ethnicity and parent education.
This is the race and highest level of parent education achieved by the parent who provided consent for the child; we do not have demographic data on spouses/partners.
One parent of a child in this group did not provide her highest level of education.
Measures
Parent questionnaire
The research team created a brief, multiple-choice questionnaire for parents to complete, covering their attitudes toward education on reproductive health topics, perceptions of the education their children had received, and basic demographic information. Although we collected some demographic information from all parents, only 16 completed the full questionnaire.
Focus group interview guideline
The researchers developed a list of open-ended questions and probes, in consultation with members of the Oncofertility Consortium program (http://oncofertility.northwestern.edu) and based on the literature reviewed above. Questions focused on children’s experiences learning about human reproduction and their understanding of reproductive anatomy, puberty, menstruation, and conception/fertilization.
Procedure and Stimuli
Prior to the study, families were informed that the focus group interviews would be recorded for research purposes. Children were assured their parents would not have access to the tapes of their groups, and parents were informed that the researchers would not share with them what their children said during the sessions. Parents provided consent for children to participate and completed the parent questionnaire. Children completed an assent form for their own participation.
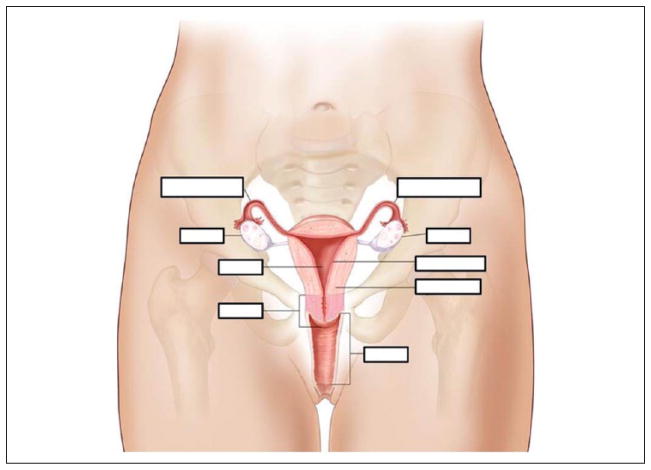
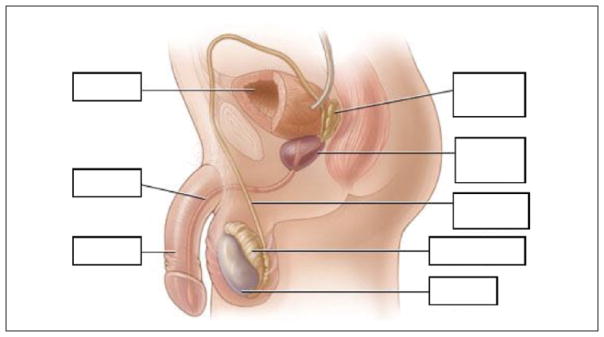
Sessions were conducted in late winter 2014. Only one group was held at a time so the same experienced researcher could lead all groups and so the first author could observe and take notes in real time. The researcher asked children what they knew about each reproductive health topic, providing verbal prompts and 11″ × 7″ diagrams of the female (see Figure 1) and male (see Figure 2) reproductive systems to facilitate discussion when relevant. In light of prior work indicating materials used to teach children about these topics often present inaccurate or inexact depictions of anatomy (e.g., Erchull et al., 2002), the team chose fairly detailed diagrams to use as stimuli. However, as shown in Figures 1 and 2, we removed the labels from these diagrams to facilitate testing children’s organ recall. Throughout the focus group interviews, the researcher leading the sessions made an effort to ensure all children participated and were engaged throughout each session. However, to maintain a relatively conversational tone and to ensure all children were comfortable discussing what might be sensitive topics for them, the researcher did not require every child to answer every question. Sessions lasted approximately 60 to 90 minutes. Approval for the study was obtained from our university institutional review board (IRB).
Figure 1.
Diagram of the female reproductive system used to facilitate discussion.
Source. Adapted from T. Winslow. For the National Cancer Institute © 2009 Terese Winslow, U.S. government has certain rights.
Note. Clockwise starting from the upper-right-hand corner, this diagram highlights a fallopian tube, an ovary, the endometrium, the myometrium, the vagina, the cervix, the uterus, another ovary, and another fallopian tube.
Figure 2.
Diagram of the male reproductive system used to facilitate discussion.
Source. Adapted from Healthwise, Incorporated. Copyright by Healthwise, Incorporated.
Note. Clockwise starting from the upper-right-hand corner, this diagram highlights the seminal vesicle, the prostate gland, the vas deferens, the epididymis, a testicle, the penis, the urethra, and the bladder.
Thematic Coding
Members of the research team transcribed the recordings of all focus group interview sessions. Based on observations made during the sessions, while watching the videos, and following multiple readings of the transcripts, two researchers independently created analytic memos (Tracy, 2013) describing significant themes, subthemes, and age/gender differences. In these memos, researchers summarized participants’ experiences learning about human reproduction and commonly held beliefs and misconceptions about reproductive anatomy, puberty, and human conception, and identified quotations representing the general set of comments expressed by children. During this memo-writing process, researchers consulted the focus group interview discussion guideline to ensure their memos covered all topic areas addressed in the sessions. The open-ended nature of focus group interview discussion meant that some children did not answer every question and certain points emerged spontaneously and were discussed in some groups but not others. Thus, our analysis focused on reporting salient themes that emerged across the data. While the open-ended nature of the focus group interview discussion made it infeasible to give precise counts of responses across all participants, researchers instead used terminology such as “a few” (referring to minority beliefs or opinions voiced by two or three children) and “most” (referring to beliefs or opinions voiced by all but one or two children in the sample at large or in a given demographic group, such as older girls) when describing the prevalence of each experience and belief across the total sample of children. The researchers discussed their separate memos until reaching a consensus about each point. For the most part, the two researchers’ initial memos were in agreement; however, each researcher also noted nuances not initially identified by the other researcher.
Results
Below, we describe children’s experiences learning about human reproduction, and their understanding of reproductive anatomy, puberty, menstruation, and conception. When relevant, we provide corroborating parent questionnaire data.
Throughout the sessions, the youngest group of boys was much rowdier and less engaged than the other three groups. Based on their affect and demeanor, it seemed as if three of these boys were uninterested in most of the topics discussed. All other children were comparatively much more animated, focused, and engaged.
Experiences Learning About Human Reproduction
A little over half of the parents who completed the questionnaire (n = 9, 56%) were sure that their children had learned something about human reproduction, while a considerable number of parents (n = 6, 38%) were unsure if their children knew anything about these topics. Of the parents who believed their children had learned about human reproduction, almost all (n = 8, 89%) reported teaching their children themselves, and many reported that their child’s other parent taught him or her about these topics (n = 6, 67%). Only three parents reported being sure that their children had taken a sexual education class in school.
Children themselves felt they had received a modest amount of instruction on human reproduction, and they reported primarily learning about these topics from family members, especially mothers and older siblings. As one boy (age 12) noted, “really your parents are the only people that you know that you’re comfortable with asking, and you know would know [accurate information].” Indeed, about half of the children in the two older groups described their parents as gatekeepers to their human reproduction education, with one girl (age 11) explaining,
Parents, like from generation to generation, like they always have to tell [their children if they think they are mature enough to learn about reproductive health]. So you should like ask them first, like, “Oh, can I go learn about this? Am I ready for this?” Like stuff like that.
For participants, school provided another source of information about human reproduction. A few children indicated that their schools offered formal sexual education classes in fifth (when children are about ages 10–11) and seventh grade (when children are about ages 12–13), sometimes segmented by gender. No child mentioned learning about reproductive health topics in class prior to fifth grade. Accordingly, only about one quarter of the sample already had taken a formal school-based class on these topics. Children also explained that reproductive health topics often were fodder for lunchroom and schooltime informal chatter among peers.
Many children were interested in learning about these topics, explaining that instruction should be age-appropriate, accurate, and moderately detailed. One boy (age 12) explained, “I want to understand it on some level, but I don’t need to know every single detail of every single thing that is going on. But I like to know the basics.” A few boys suggested that learning about human reproduction might make puberty less frightening to children their age, although at least one child in every group expressed that learning about these topics could be uncomfortable for some children—as could learning about anatomy and the body more generally. Nonetheless, very few children reported proactively searching for information (e.g., engaging in self- initiated Internet searches).
Conceptual Understanding and Misconceptions About Puberty/Human Reproduction
Reproductive anatomy
The majority of parents (n = 14, 88%) agreed or strongly agreed that it was important for their children to learn about reproductive anatomy. That said, only about half of parents who were certain their children had received sexual education were confident that this instruction covered the female (n = 5, 56%) and male (n = 4, 44%) reproductive systems.
Perhaps because only a portion of the sample had received any relevant instruction, children, especially those under the age of 11, demonstrated fairly limited knowledge of the female and male reproductive tracts. In fact, many of the younger children initially appeared and reported feeling uncomfortable looking at and labeling the reproductive anatomy diagrams, although they became more at ease as the groups progressed.
Female reproductive system
Children demonstrated minimal knowledge of the female reproductive tract. Roughly one third of the sample, including a few girls, initially failed to recognize that Figure 1 represents female anatomy. After children came to a consensus that the stimulus does indeed depict a female body, they struggled to precisely label the various organs. For example, about half the sample labeled the entire diagram the “vagina.” A few of the younger children knew that “eggs” were housed somewhere in the female body, although they were unfamiliar with ovaries and/or thought the entire ovary was an “egg.” In contrast, about half of the older children had heard of ovaries, could distinguish “ovaries” from “eggs,” and were accurately able to label the ovaries on the diagram. The oldest boys in the sample (ages 11 and 12) who had taken sexual education classes in school also noted many components of the female reproductive system not mentioned by other participants, including the cervix, uterus, and fallopian tube. But by and large, these boys could not accurately identify which areas of the diagram correspond to these verbal labels or describe in detail the function of these components.
Male reproductive system
Children’s knowledge of the male reproductive system was comparatively stronger although still fairly limited. Most children easily recognized that Figure 2 represents male anatomy, likely due to the prominence of the penis. However, children, especially the girls and younger boys, had minimal knowledge of the rest of the male system. For instance, a few of the 9-year-old boys and 9- to 11-year-old girls assumed that sperm must be housed somewhere that appeared hollow, although many could not identify where specifically. These girls and younger boys did not explicitly label the urethra, but a few described the “tube” in the diagram as probably facilitating the expulsion of urine and perhaps sperm from the male body. Only the oldest boys correctly labeled the testicle visible on the diagram, noted that sperm are found in this body part, and differentiated between the testicles and scrotum. A few of the older boys labeled the urethra accurately, albeit not confidently, and described how urine and sperm “come out” through this “passage.”
Puberty and menstruation
The majority of parents believed it was appropriate for their children to learn about female puberty (n = 13, 82%), male puberty (n = 14, 88%), and menstruation (n = 14, 88%) between the ages of 7 and 12. And indeed, of the parents who were confident their children had received some education around human reproduction, most (n = 7, 78%) were sure that this instruction covered puberty although only about half (n = 4, 44%) believed their children had learned about menstruation.
Despite parental support of education about these topics across the sample, children’s familiarity with puberty and menstruation varied greatly by age. Participants in the younger two groups (ages 7–9) knew very little about these topics and expressed very few puberty-related concerns. About half of the younger children had never even heard the term “puberty.” When discussing what happens as children enter adolescence, these children cited mostly secondary sexual changes, such as growth spurts, voice changes, and hair growth. The girls in the younger group arrived at the conclusion that both genders go through puberty, while the younger boys thought the term “puberty” only applies to males and a different term they could not recall is used for females. None of these younger children had heard the term “menstruation,” although three or four of the 8- and 9-year-olds were familiar with “periods” as a female bodily process involving “blood” and unfertilized “eggs.” For example, one girl (age 9) explained, “Like you have eggs when you have like your baby, and like as it sheds. It’s like your blood…. The egg sheds and that’s the blood that’s your period.” These children seemed to conceive of menstruation in very binary terms: having a “period” signified the lack of pregnancy, and the lack of “period” signified pregnancy. One or two of the 9-year-old boys also referred to “periods” as occurring once a month.
Children in the older groups (ages 10–12) demonstrated much stronger knowledge of puberty and menstruation, but even they evinced some misconceptions. They were largely familiar with the term “puberty” and could name relevant primary sexual changes, such as spermarche (when “the sperm comes out”; referenced only by the older boys) and menarche (when “the menstrual cycle like can happen,” according to one 10-year-old girl), in addition to the secondary sexual changes also listed by the younger children. All of the older participants understood that both boys and girls go through puberty and unique subsequent physiological changes. A few of these children had heard the term “menstruation,” and all knew of “periods.” Like their younger peers, they explained that menstruation occurs only in females and involves unfertilized “eggs” and “blood.” Nonetheless, their understanding was imperfect/incomplete. For example, they seemed largely unaware of how long menstruation lasts or of individual differences in cycle length and menarche onset. One girl (age 10) told the group, “If we have eggs right now, and this is the last day of February, the egg could then travel,” while her fellow group member (age 10) explained, “my mom said that your period can last from 1 to 4 days.”
In contrast to the younger children who expressed hardly any puberty-related concerns, the older children (here we refer to children ages 9 and up) mentioned worries they or their peers have about this transition. Girls seemed more concerned than boys. As an illustration, one girl (age 10) commented, “You get older, and your body changes and everything starts getting weird and shocked about how you’re starting puberty.” And when talking about menstruation, these girls seemed quite fretful about learning how to use potentially uncomfortable and “nasty” tampons, with one girl (age 11) remarking, “[Using a tampon is] kind of like … taking out an earring for the first time that’s infected.” Interestingly, the boys named concerns their peers might hypothetically have about transitioning to puberty but avoided identifying these concerns as their own. For example, one boy (age 12) explained that others might be “scared … ‘cause all the voice cracks that you get,” though he presented himself as fairly unconcerned.
Conception
All but one parent (n = 15, 94%) believed it was important for their children to know about human conception although only about half of parents who knew their children had received instruction in human reproduction believed it covered fertilization (n = 4, 44%) or pregnancy (n = 5, 56%).
Also mirroring the results above, children’s knowledge of human fertilization and conception varied greatly by age. About a third of the youngest children would not even venture guesses about how conception occurs. Another one-third explained that embryos grow in women’s stomachs and offered other very unscientific accounts of this process, as illustrated in the following exchange:
Girl (age 7): Like a crumb comes out … comes in and then bursts out something, and then it grows bigger and bigger and bigger, and then it becomes a baby.
Researcher: Where does the crumb come from?
Girl (age 7): Like when you eat something.
However, the remaining children in the younger groups vaguely seemed to understand that conception involves “sperms,” “eggs,” and a sexual act (“woohoo”) among post-pubescent males and females. For example, one boy (age 9) explained,
[Sperm are] a really really small thing um that when you have sex … it goes into the um woman. And it finds the egg. And when it goes through … That’s what—that’s what forms the baby because the sperm holds the man’s DNA, and the um egg holds the woman’s DNA.
That said, even those children struggled to articulate why prepubescent children cannot conceive. As an illustration, one boy (age 9) told the group, “[8-year-olds can’t have babies] because um, I think it’s like bad for a woman to have a baby … too young, and I think puberty has to do something with that.”
By comparison, all of the children in the older groups demonstrated a much more accurate level of understanding. They seemed to know that conception involves the sperm of a post-pubescent male “swimming” to the “egg” of a post-pubescent female. Nonetheless, these children exhibited confusion about where specifically the sperm penetrates the ovum, with many incorrectly pointing on the female diagram to the uterus as the location where this occurs.
Discussion
The findings of our needs assessment suggest that, despite parental support, the 7- to 12-year-olds who participated in our study were ill-informed about reproductive health. In fact, their beliefs and concerns regarding these topics were highly reminiscent of beliefs and concerns reported in prior research conducted 20 to 30 years ago (e.g., R. J. Goldman & Goldman, 1982; KRC Research & Consulting, 1991a). They could label few components of the male and female reproductive tracts, were unfamiliar with terms such as “menstruation” and even “puberty,” and espoused incomplete conceptual understanding of human conception. This is surprising given recent increases in Internet (Rideout et al., 2010) and funding for reproductive health education (SIECUS, 2010) and potentially problematic considering that possessing strong knowledge of these topics may help children be cognitively and emotionally prepared for the onset of puberty (Brooks-Gunn, 1984) and for later, more advanced health classes (UNESCO, 2009). The present focus group interview discussions shed insight into how our target population learns, conceptualizes, and theorizes about reproductive health topics, with support from parents and teachers.
Despite recommendations that children know where to find medically accurate information on these topics by the time they complete fifth grade (FoSE, 2012), the overwhelming majority of children in our sample never proactively searched for reproductive health information. It may be that youth do not feel a need to engage in such searches if they do not have any unanswered questions about these topics (e.g., Wartella et al., 2015; Mitchell, Ybarra, Korchmaros, & Kosciw, 2014). Parents and teachers therefore may need to be advised to share facts and broach conversations about reproductive health with children to ensure that children do indeed learn about these topics, even if children do not think to ask questions themselves. Much of the responsibility of teaching children about these topics may initially fall on parents as sexual education in our community is not taught until fifth grade. Given that parents, at least those in our community willing to allow their children to participate in this study, seemed supportive of their children learning about these topics, such an agenda might be realistic.
That said, the younger boys in our sample were not particularly interested in discussing reproductive health topics, and all of the 7- and 8-year-olds (both boys and girls) exhibited very low levels of knowledge on all topics. The same experienced researcher moderated all groups, suggesting the difference in levels of engagement likely reflected genuine differences in children’s interest in these topics, as opposed to methodological idiosyncrasies. Topics such as puberty and conception may have been so removed from the lived experiences of the 7- and 8-year-old children in our sample that they were uninterested in discussing these topics and might not have retained much factual information even in cases when caregivers had initiated reproductive health-related conversations. Experts suggest children learn reproductive health lessons most easily when material is made relevant to their daily experiences (FoSE, 2012). Those wishing to engage children before the onset of puberty may therefore need to be especially assiduous in brainstorming ways to make conversations interesting and relevant to this set.
Turning more specifically to the individual topics discussed, it is not surprising that children across our entire sample were only familiar with a handful of reproductive organs, given that only about a third of the sample had previously been taught about reproductive anatomy. Not unlike prior research (e.g., Bernstein & Cowan, 1975), our younger participants primarily focused on more familiar body parts such as the penis. Older participants, especially the boys who had already taken sexual education classes in school, could name a variety of reproductive organs but struggled to label them on the medically accurate stimuli diagrams. Nonetheless, children across the sample hypothesized about reproductive anatomy by linking relevant vocabulary they were able to recall to the visuals in the diagrams. For example, those who knew about sperm guessed they might be housed in one of the hollow areas in the diagram and might flow through the “tube” (i.e., the urethra). The use of the diagrams in this study thus allowed children to reason and allude to knowledge about reproductive anatomy (e.g., the sperm are contained in seminal fluid, and this fluid must traverse the male system) in ways not captured in prior studies that provided no stimuli (e.g., Whisnant & Zegans, 1975). However, not all of children’s guesses were accurate (e.g., the younger boys and older girls debated whether the hollow-looking bladder held sperm or urine). Aligned with prior literature on children’s learning about human biology (Allen, 2010), our results underscore the potential of incorporating accurate diagrams into sexual education. For the purposes of this study, we chose medically exact diagrams without labels, although labeling diagrams would be more appropriate in an educational setting.
Although children were more knowledgeable about puberty than other topics discussed, there nonetheless were age-related differences in knowledge and attitudes about impending transitions, again mirroring prior research (e.g., KRC Research & Consulting, 1991a; Whisnant & Zegans, 1975; Winn et al., 1995). Given that about half of the younger children were entirely unfamiliar with the term “puberty,” it is not shocking that they also were largely unfamiliar and unconcerned with primary sexual changes. Even though the older children were comparatively more knowledgeable than their younger counterparts, they did not seem on track to meet educational guidelines (UNESCO, 2009). As reflected in prior research (e.g., KRC Research & Consulting, 1991a), older girls also seemed more concerned about transitioning to puberty in general and menarche specifically.
These puberty- and menstruation-related findings point to a need for additional education. In light of research suggesting that the onset of puberty can have negative mental health ramifications for those who achieve major milestones precociously with limited topical knowledge (Walvoord, 2010), it may be appropriate to begin teaching children about some of these topics at an earlier age. Moreover, because girls ages 9 to 12 in particular were quite uneasy about menarche, it may be helpful to provide them with additional knowledge about these so that they might feel less anxious about impending milestones (Brooks-Gunn, 1984). Specifically, emphasizing individual differences in terms of the timing of processes such as menstruation (FoSE, 2012) and providing children, especially girls, detailed information about feminine hygiene products and/or describing alternatives to traditional products (Stubbs, 2008) might help elevate their level of knowledge and alleviate some of the specific concerns mentioned during the sessions.
Children’s knowledge about conception was remarkably similar to previously documented developmental trajectories on conception-related knowledge: Several of the youngest children espoused completely inaccurate beliefs, while the oldest children at least knew the major components involved in this process (e.g., Bernstein & Cowan, 1975; R. J. Goldman & Goldman, 1982). According to the national/international learning standards, this level of knowledge (i.e., knowing that conception involves sperm and unfertilized ova) may be sufficient for children in this age range (SIECUS, 2004; UNESCO, 2009). That said, if those teaching children about reproductive health wish to include lessons on human conception—and indeed the parents in our sample seemed overwhelmingly supportive of their children learning about this topic—these lessons perhaps should be mainly targeted to children ages 9 and above. The oldest children in the sample seemed more interested in discussing distal milestones such as conceiving, possibly reflecting greater maturity or stronger abstract reasoning skills relative to the younger participants.
Across all topic areas, children frequently used informal language and were unfamiliar with medically accurate terminology. For instance, children’s familiarity with the term period was higher than menstruation, and one of the most knowledgeable boys in the sample (age 12) said he thought “Testes sounds slang.” Also, when attempting to label the diagrams, children often labeled the organs they were unfamiliar with as “thingies.” In the context of the research setting, by allowing children to use their own words to describe their understanding of reproductive phenomena, we believe we yielded richer data than we would have had we restricted children’s language. When it comes to teaching children about these topics, our study calls into question the value of materials that over-rely on medical jargon, at least when delivering initial lessons (Whisnant, Brett, & Zegans, 1975).
Limitations
The results of this study should be interpreted in light of limitations. Because our study, like many others in this domain, was qualitative with a small, convenience sample, results may not generalize to other populations. More conservative parents do not always give their children permission to participate in studies of this nature (R. J. Goldman & Goldman, 1982), and children with high levels of puberty-related anxiety may proactively request not to participate. Accordingly, we may overestimate normative knowledge or underestimate concerns. However, as it did not seem as if any of our participants attended schools with K-12 human reproduction curricula (e.g., Chicago Public Schools, 2013), they might have been less knowledgeable than peers who have received annual topical education. Likewise, given previously documented cultural/regional differences in human reproduction knowledge (e.g., R. J. Goldman & Goldman, 1982), it is plausible that children in other communities might demonstrate differing levels of understanding. Furthermore, even though our stimulus materials had the advantage of being medically accurate, we nonetheless only provided one female and one male stimulus drawn in 3D effect. Children might have reflected different conceptual understanding had they viewed the reproductive systems from different or multiple angles, in black-and-white, or in 2D. Finally, our data only represent a snapshot of children’s knowledge. While we have made speculative comparisons between our data and data collected in prior studies and allude to potential educational priorities or tactics that might have had the potential to affect children’s knowledge, longitudinal work in this area is needed.
Conclusion
The current research indicates that children today (at least in our community) know as much about human reproduction as children did nearly 30 years ago. It may be that previous research truly reflected normative understanding, and shifts in technology and information access have not affected what children know and are interested in knowing. Or it may be that parents and educators, at least in this region, have not made measurable strides to truly enhance the quality and depth of the information they provide children in this age range. Our research suggests there may be a need in our community for visually rich educational aids that rely on parents and teachers as intermediaries and that use age-appropriate language, engage younger learners, and dispel concerns of older learners. Likewise, it is key that anyone assessing the effectiveness of any already existing or future learning aids allow children to discuss these topics in their own words (e.g., avoid creating tests dependent on familiarity with terms such as “uterus”) and scaffold their knowledge with the support of visual aids. If we accept the premise that teaching prepubescent children about human reproduction helps them be prepared for the onset of primary sexual changes (Brooks-Gunn, 1984; Winn et al., 1995), get the most out of the later reproductive health classes (UNESCO, 2009), and be equipped to make responsible sexual decisions as adolescents and adults (e.g., Koo et al., 2011), we must continue to work to enhance children’s early reproductive health learning experiences.
Acknowledgments
The authors thank Eden Schoofs for her help in transcribing a portion of the data, members of the Woodruff Lab for their focus group interview guideline input, and the members of the Center on Media and Human Development for their assistance with recruitment for and transitions between focus group interview sessions and for their feedback on drafts of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by Northwestern University Center for Reproductive Health After Disease, Grant P50 HD076188, from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD) National Centers for Translational Research in Reproduction and Infertility (NCTRI).
Biographies
Lisa B. Hurwitz is a doctoral candidate at Northwestern University. Her research investigates children’s conceptual development and experiences using electronic media.
Alexis R. Lauricella is associate director at the Center on Media and Human Development and a lecturer in the communication studies department at Northwestern University. Her research lies at the intersection of child development, education, and communication, and is done with the intention of informing policy and practice.
Brianna Hightower is a researcher at the Center for Children and Technology, Education Development Center, New York, NY. She received a bachelor’s degree from the Department of Communication Studies at Northwestern University in 2014.
Iris Sroka is founder and principal of Paradigm Research & Consulting. She is a child development expert specializing in the areas of educational media development, social values and attitudes, and child care and educational practices and attitudes.
Teresa K. Woodruff is the Thomas J. Watkins Professor of Obstetrics & Gynecology (OB/GYN), the vice chair of research (OB/GYN), the chief of the Division of Reproductive Science in Medicine, Feinberg School of Medicine, and professor of molecular biosciences at the Weinberg College of Arts and Sciences at Northwestern University. She is an expert in ovarian biology and coined the term oncofertility to describe the merging of oncology and fertility. She heads the Oncofertility Consortium, an interdisciplinary team of biomedical and social scientists.
Ellen Wartella is the Sheikh Hamad bin Khalifa Al-Thani Professor of Communication, professor of psychology and professor of human development and social policy at Northwestern University. She also directs the university’s Center on Media and Human Development. She researches the effects of media on children and adolescents.
Footnotes
Declaration of Conflicting Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
References
- Allen M. Misconceptions in primary science. New York, NY: Open University Press; 2010. [Google Scholar]
- American Academy of Pediatrics. Sexuality, contraception, and the media. Pediatrics. 2001;107:191–194. doi: 10.1542/peds.107.1.191. [DOI] [PubMed] [Google Scholar]
- Berends MM, Caron SL. Children’s understanding and knowledge of conception and birth: A developmental approach. Journal of Sex Education & Therapy. 1994;20:18–29. [Google Scholar]
- Bernstein AC, Cowan PA. Children’s concepts of how people get babies. Child Development. 1975;46:77–91. doi: 10.2307/1128836. [DOI] [Google Scholar]
- Brooks-Gunn J. The psychological significance of different pubertal events to young girls. The Journal of Early Adolescence. 1984;4:315–327. doi: 10.1177/0272431684044003. [DOI] [Google Scholar]
- Carter R. Anxiety symptoms in African American youth: The role of puberty and biological sex. The Journal of Early Adolescence. 2014;35:281–307. doi: 10.1177/0272431614530809. [DOI] [Google Scholar]
- Chicago Public Schools. Chicago public schools policy manual: Sexual health education. 2013 Retrieved from http://policy.cps.edu/download.aspx?ID=57.
- Dixon-Mueller R. How young is “too young”? Comparative perspectives on adolescent sexual, marital, and reproductive transitions. Studies in Family Planning. 2008;39:247–262. doi: 10.1111/j.1728-4465.2008.00173.x. [DOI] [PubMed] [Google Scholar]
- El-Shaieb M, Wurtele SK. Parents’ plans to discuss sexuality with their young children. American Journal of Sexuality Education. 2009;4:103–115. doi: 10.1080/15546120903001357. [DOI] [Google Scholar]
- Erchull MJ, Chrisler JC, Gorman JA, Johnston-Robledo I. Education and advertising: A content analysis of commercially produced booklets about menstruation. The Journal of Early Adolescence. 2002;22:455–474. doi: 10.1177/027243102237192. [DOI] [Google Scholar]
- Fields J. Risky lessons: Sex education and social inequality. Piscataway, NJ: Rutgers University Press; 2008. [Google Scholar]
- Fisher TD. Parent-child communication about sex and young adolescents’ sexual knowledge and attitudes. Adolescence. 1986;21:517–527. [PubMed] [Google Scholar]
- Future of Sex Education Initiative (FoSE) National sexuality education standards: Core content and skills, K-12. 2012 (A special publication of the Journal of School Health). Retrieved from https://web.archive.org/web/20160314044936/http://futureofsexeducation.org/documents/josh-fose-standards-web.pdf.
- Gartrell N, Mosbacher D. Sex differences in the naming of children’s genitalia. Sex Roles. 1984;10:869–876. doi: 10.1007/BF00288510. [DOI] [Google Scholar]
- Goldman JDG. Some methodological problems in planning, executing and validating a cross-national study of children’s sexual cognition. International Journal of Intercultural Relations. 1994;18:1–27. doi: 10.1016/0147-1767(94)90002-7. [DOI] [Google Scholar]
- Goldman JDG. An exploration in health education of an integrated theoretical basis for sexuality education pedagogies for young people. Health Education Research. 2011;26:526–541. doi: 10.1093/her/cyq084. [DOI] [PubMed] [Google Scholar]
- Goldman RJ, Goldman JDG. How children perceive the origin of babies and the roles of mothers and fathers in procreation: A cross-national study. Child Development. 1982;53:491–504. doi: 10.2307/1128992. [DOI] [Google Scholar]
- Guttmacher Institute. Sex and HIV education. 2015 Retrieved from http://www.guttmacher.org/statecenter/spibs/spib_SE.pdf.
- Haglund K. Recommendations for sexuality education for early adolescents. Journal of Obstetric, Gynecologic, & Neonatal Nursing. 2006;35:369–375. doi: 10.1111/j.1552-6909.2006.00048.x. [DOI] [PubMed] [Google Scholar]
- Himes JH. Examining the evidence for recent secular changes in the timing of puberty in US children in light of increases in the prevalence of obesity. Molecular and Cellular Endocrinology. 2006;254–255:13–21. doi: 10.1016/j.mce.2006.04.013. [DOI] [PubMed] [Google Scholar]
- Hmelo-Silver CE, Azevedo R. Understanding complex systems: Some core challenges. Journal of the Learning Sciences. 2006;15:53–61. doi: 10.1207/s15327809jls1501_7. [DOI] [Google Scholar]
- Jorgensen M, Keiding N, Skakkebaek NE. Estimation of spermarche from longitudinal spermaturia data. Biometrics. 1991;47:177–193. doi: 10.2307/2532505. [DOI] [PubMed] [Google Scholar]
- Koo HP, Rose A, Bhaskar B, Walker LR. Relationships of pubertal development among early adolescents to sexual and nonsexual risk behaviors and caregivers’ parenting behaviors. The Journal of Early Adolescence. 2011;32:589–614. doi: 10.1177/0272431611409746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- KRC Research & Consulting. 3-2-1 Contact research: Children’s understanding of puberty, sex and human reproduction. New York, NY: KRC Research & Consulting and Children’s Television Workshop; 1991a. [Google Scholar]
- KRC Research & Consulting. 3-2-1 Contact sexual education research with parents. New York, NY: KRC Research & Consulting and Children’s Television Workshop; 1991b. [Google Scholar]
- Landry DJ, Singh S, Darroch JE. Sexuality education in fifth and sixth grades in U.S. public schools, 1999. Family Planning Perspectives. 2000;32:212–219. doi: 10.2307/2648174. [DOI] [PubMed] [Google Scholar]
- Martin K, Verduzco Baker L, Torres J, Luke K. Privates, pee-pees, and coochies: Gender and genital labeling for/with young children. Feminism & Psychology. 2011;21:420–430. [Google Scholar]
- Mitchell KJ, Ybarra ML, Korchmaros JD, Kosciw JG. Accessing sexual health information online: Use, motivations and consequences for youth with different sexual orientations. Health Education Research. 2014;29:147–157. doi: 10.1093/her/cyt071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rideout V, Foehr UG, Roberts DF. Generation M2: Media in the lives of 8- to 18-year-olds. Menlo Park, CA: Kaiser Family Foundation; 2010. [Google Scholar]
- Rossi PH, Lipsey MW, Freeman HE. Evaluation: A systematic approach. 7. Thousand Oaks, CA: SAGE; 2003. [Google Scholar]
- Schor DP, Sivan AB. Interpreting children’s labels for sexrelated body parts of anatomically explicit dolls. Child Abuse & Neglect. 1989;13:523–531. doi: 10.1016/0145-2134(89)90056-2. [DOI] [PubMed] [Google Scholar]
- Sexuality Information and Education Council of the United States. Guidelines for comprehensive sexuality education: Kindergarten through 12th grade. 3. Washington, DC: Author; 2004. [Google Scholar]
- Sexuality Information and Education Council of the United States. A brief history of federal funding for sex education and related programs. 2010 Retrieved from http://www.siecus.org/index.cfm?fuseaction=page.viewPage&pageID=1341&nodeID=1.
- Sexuality Information and Education Council of the United States. Fact sheet: Federal programs cheat sheet. 2014 Retrieved from http://siecus.org/_data/n_0001/resources/live/ProgramFactsheet.pdf.
- Stubbs ML. Cultural perceptions and practices around menarche and adolescent menstruation in the United States. Annals of the New York Academy of Sciences. 2008;1135:58–66. doi: 10.1196/annals.1429.008. [DOI] [PubMed] [Google Scholar]
- Stubbs ML, Rierdan J, Koff E. Developmental differences in menstrual attitudes. The Journal of Early Adolescence. 1989;9:480–498. doi: 10.1177/0272431689094008. [DOI] [Google Scholar]
- Tracy SJ. Qualitative research methods: Collecting evidence, crafting analysis, communicating impact. Malden, MA: Wiley-Blackwell; 2013. [Google Scholar]
- United Nations Educational, Scientific and Cultural Organization. International technical guidance on sexuality education: An evidence-informed approach for schools, teachers and health educators. 1–2. Paris, France: Author; 2009. [Google Scholar]
- Walvoord EC. The timing of puberty: Is it changing? Does it matter? Journal of Adolescent Health. 2010;47:433–439. doi: 10.1016/j.jadohealth.2010.05.018. [DOI] [PubMed] [Google Scholar]
- Wartella E, Rideout V, Zupancic H, Ryan LB, Lauricella AR. Teens, health, and technology: A national study. Evanston, IL: Center on Media and Human Development, School of Communication, Northwestern University; 2015. [Google Scholar]
- Whisnant L, Brett E, Zegans L. Implicit messages concerning menstruation in commercial educational materials prepared for young adolescent girls. American Journal of Psychiatry. 1975;132:815–820. doi: 10.1176/ajp.132.8.815. [DOI] [PubMed] [Google Scholar]
- Whisnant L, Zegans L. A study of attitudes toward menarche in white middle-class American adolescent girls. American Journal of Psychiatry. 1975;132:809–814. doi: 10.1176/ajp.132.8.809. [DOI] [PubMed] [Google Scholar]
- Whiteley LB, Mello J, Hunt O, Brown LK. A review of sexual health web sites for adolescents. Clinical Pediatrics. 2012;51:209–213. doi: 10.1177/0009922811423311. [DOI] [PubMed] [Google Scholar]
- Winn S, Roker D, Coleman J. Knowledge about puberty and sexual development in 11–16 year-olds: Implications for health and sex education in schools. Educational Studies. 1995;21:187–201. doi: 10.1080/0305569950210204. [DOI] [Google Scholar]