Abstract
Background: Metacarpal lengthening by distraction osteogenesis has been well documented in pediatric patients but limited in older patients. Fewer studies have assessed the success of the procedure through outcome measure scores. The purpose of this study is to assess the outcomes of distraction osteogenesis in skeletally mature adults with brachymetacarpia and patients’ perspectives on their satisfaction through outcome measure scores. Methods: Retrospective chart review of a consecutive series of metacarpal lengthenings for the treatment of brachymetacarpia was performed. Key parameters collected include starting metacarpal length, amount lengthened, range of motion of metacarpophalangeal joint, type of fixator used, distraction time, and total time in fixator. Relevant comorbidities and complications encountered were recorded as well. The Body Image Quality of Life Inventory (BIQLI) and Limb Deformity Modified Scoliosis Research Society (LD-SRS) score were given to evaluate patients’ perspectives on their satisfaction of surgery. Results: Seven metacarpal lengthenings were performed in 4 adult females (average age: 22.8 years) between 2005 and 2016. The average amount lengthened was 1.5 cm (range, 1.2-2.1 cm), corresponding to a mean percent lengthening of 44.4% (range, 33.3%-57.1%). The mean distraction rate was 0.432 mm/day (range, 0.286-0.724 mm/day). The mean distraction time was 38 days (range, 28-55 days). External fixation index was 71.8 days/cm (range, 53.5-99.2 days/cm). No functional loss was observed. Conclusions: Progressive distraction osteogenesis can obtain functionally successful results and improvement in aesthetics and body image without severe complications in skeletally mature adults with brachymetacarpia.
Keywords: brachymetacarpia, distraction osteogenesis, adults, outcome measure scores, metacarpal lengthening
Introduction
Brachymetacarpia is a rare congenital hand deformity resulting in abnormal shortening of the metacarpal(s). While the incidence is unknown, brachymetacarpia occurs more often in females than in males.13 The fourth metacarpal is the most frequently affected digit.10 The underdevelopment of the metacarpals is due primarily to the premature closure of the epiphyseal growth plate. This may be of congenital etiology or acquired from infection or trauma to the epiphysis.
Unlike other hand deformities, brachymetacarpia does not seriously compromise hand function. However, it can result in restriction of flexion at the metacarpophalangeal (MCP) joint.10 Severe shortening of the metacarpal(s) can alter the normal anatomy of the transverse metacarpal arch leading to weakness in grasping or difficulty in making a hard fist.1 Therefore, surgical treatment is mainly desired because of aesthetic and body image reasons. Patients are displeased with the altered curved line formed by the tips of the fingers and altered contour of the knuckles.12
In recent years, progressive distraction osteogenesis has been the preferred surgical intervention for brachymetacarpia. Progressive distraction osteogenesis is consider safer because the lengthening process is gradual, resulting in better outcomes and lower complication rates.2 Although several studies have reported its high success rate in treating patients with brachymetacarpia, all the studies described pediatric patients (average age: 16.0 years).2,3,7,8 Literature regarding metacarpal lengthening in older patients is limited.11 In addition, few assessed the success of the procedure through outcome measure scores. The purpose of this study is to evaluate the results of distraction osteogenesis in a uniform series of older patients (average age: 22.8 years), including patients’ perspectives on their satisfaction through outcome measure scores.
Materials and Methods
After obtaining institutional review board approval and informed consent from each patient, records of 4 patients who underwent 7 metacarpal lengthening for the treatment of brachymetacarpia were retrospectively reviewed by the lead author between 2005 and 2016. Patients’ medical charts and radiographs were reviewed. Information pertaining to the patients’ demographics, comorbidities, complications, and number of affected metacarpal(s) were recorded. Key parameters collected include range of motion (ROM) of the MCP joint, type of fixator used, distraction time and the total time in the fixator. Starting and ending metacarpal lengths were measured from patients’ radiographs. Patients completed the Body Image Quality of Life Inventory (BIQLI)4 and Limb Deformity Modified Scoliosis Research Society (LD-SRS) score5 both preoperatively and at the latest follow-up.
Based on the measurements from the radiographs, the amount lengthened and the percentage lengthening were calculated. The lengthening rate was determined by dividing the amount lengthened by the distraction time in days. Consolidation times were indirectly calculated based on the difference between the total time in fixator and the distraction time. External fixation index (EFI) for each patient was determined by dividing the total time in fixator by the amount lengthened. To objectively determine whether the optimal amount lengthened was achieved, the mathematical relationship between the different metacarpals determined by Aydinlioglu et al was used (second metacarpal = 1.06 × third metacarpal = 1.16 × fourth metacarpal = 1.26 × fifth metacarpal).1
Means were calculated for all variables. The nonparametric version Wilcoxon signed rank sum test (primary analysis approach) and paired t tests (secondary analysis approach) were used to analyze preoperative and postoperative values for the BIQLI and LD-SRS scores. Both tests were used because a sample size of 4 may not be sufficient to test the normality assumption required for paired t tests. P < .05 was considered statistically significant.
Surgical Technique
The upper extremity of the affected side was prepped and draped in the usual sterile fashion. With the help of biplanar fluoroscopy, a 1.6 mm treaded external fixation half pin was inserted into the most proximal aspect of the affected metacarpal. The pin was placed dorsal to palmar in the center of the bone and started in a slight ulnar direction to avoid the extensor tendon.
Using the Orthofix Minirail frame (Orthofix, Lewisville, Texas) as a guide, the most distal pin was placed on the distal pin clamp parallel to the first pin and at the most distal aspect of the bone, just proximal to the MCP capsule. With these 2 pins placed, the orientation of the fixator was established being parallel to the metacarpal bone. An additional half pin was placed in the proximal clamp and an additional half pin was placed in the distal clamp.
The external fixator was then removed from the external fixation pins and a 1.5 cm skin incision was made centered on the point just between the proximal and distal pin processes. Soft tissue dissection was carried down to the bone. The extensor tendon was retracted and the metacarpal was prepared for osteotomy using a multiple drill hole technique. A 0.045-inch Kirschner wire was used to make the multiple transverse drill holes while cooled with saline. A 3-mm thin osteotome was used to complete the osteotomy. The osteotomy was completed but was left nondisplaced.
The wound was irrigated, and the skin was closed with 3-0 nylon suture. The Orthofix Minirail frame was reapplied to the pins to stabilize the osteotomy and maintain it in a nondisplaced position. The MCP joint was checked to ensure that there was full ROM, from full extension to 90 of flexion, and there was no obstruction from the external fixation pins. The surgical wounds and pin sites were covered with Xeroform gauze and dry sterile dressings. The MCP joint was held in about a 60 flexed position with a Kling wrap.
The lengthening process began postoperative day 5 to allow for some early healing of the osteoplasty. Postoperative physical therapy focused on stretching, active and passive ROM of the MCP joint as it is easier to lose flexion than extension. When not performing ROM exercises, the MCP joint was maintained in about 70 of flexion with a resting splint. A representative case of Patient 1 with bilateral fourth metacarpal shortening before and after is shown in Figures 1 and 2.
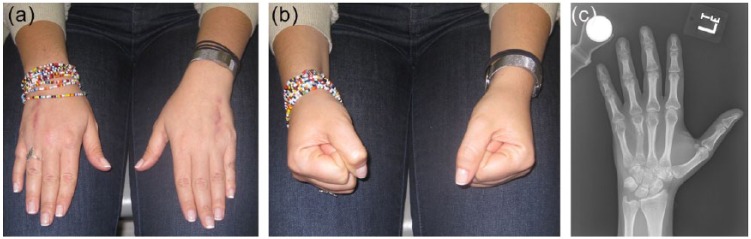
Figure 1.
(a) Front view of the left hand showing shortening of the fourth finger. (b) When in a fist position, the absence of the knuckle (arrow) and the metacarpal shortening is apparent. (c) AP x-ray of left hand showing fourth metacarpal shortening of about 13 mm (magnification marker is 25.4 mm or 1 inch).
Figure 2.
(a) Two months after removal of the second hand frame. (b) Patient demonstrates excellent function and range of motion of hand. (c) Anteroposterior radiograph of left hand showing bone union, restoration of the fourth metacarpal lengths, and satisfactory alignment.
Results
Four patients undergoing 7 cases of metacarpal lengthening for brachymetacarpia were identified (Table 1). All of the patients were healthy, skeletally mature, adult females with a mean age of 22.8 years (range, 16-30 years). Average follow-up was 35 months (range, 4-84 months).
Table 1.
Patient Demographics.
| Patient (n = 4) | Age (years) | Comorbidities | Affected metacarpal (n = 7) | Starting length (cm) |
|---|---|---|---|---|
| 1 | 23 | None | R. 4th | 3.2 |
| L. 4th | 3.3 | |||
| 2 | 22 | None | R. 5th | 3.4 |
| L. 3rd | 3.8 | |||
| L. 5th | 3.5 | |||
| 3 | 30 | None | L. 4th | 3.5 |
| 4 | 16 | None | L. 4th | 3.6 |
| Average | 22.8 | — | — | 3.5 |
All lengthening procedures were performed using the Orthofix Minirail frame. On average, the lengthening rate was 0.440 mm/day (range, 0.286-0.724 mm/day). The mean distraction time was 38 days (range, 28-55 days). Average EFI was 71.8 days/cm (Tables 2 and 3).
Table 2.
Surgical Outcomes.
| Patient (n = 4) | Affected metacarpal (n = 7) | Amount lengthened (cm) (% lengthened) | MCP ROM extension/flexion
(degrees) |
Complications | Follow-up (months) | |
|---|---|---|---|---|---|---|
| Pre-op | Post-op | |||||
| 1 | R. 4th | 1.5 (46.9) | 0/90 | 0/80 | Pin site infection | 36 |
| L. 4th | 1.5 (45.5) | 0/90 | 0/90 | Pin site infection | ||
| 2 | R. 5th | 1.2 (35.3) | 30/90 | 0/90 | Break through pain/tightness | 84 |
| L. 3rd | 2.1 (55.3) | 30/90 | 0/90 | Tightness | ||
| L. 5th | 1.3 (37.1) | 30/90 | 0/80 | Fracture at lengthening site | ||
| 3 | L. 4th | 2.0 (57.1) | 15/60 | 0/80 | Flexion deformity at osteotomy site Lack MCP flexion Lack prominent MCP on 4th finger |
15 |
| 4 | L. 4th | 1.2 (33.3) | 40/100 | 0/90 | Pin site infection × 2 | 4 |
| Average | 1.5 (44.4) | 21/87 | 0/86 | — | 35 | |
Note. MCP = metacarpophalangeal; ROM = range of motion.
Table 3.
Fixator Parameters.
| Patient | Affected metacarpal | Type of fixator | Lengthening rate (mm/day) | Distraction time (days) | Consolidation time (days) | Total time in fixator (days) | EFI (days/cm) |
|---|---|---|---|---|---|---|---|
| 1 | R. 4th | Orthofix Minirail | 0.375 | 40 | 60 | 100 | 66.7 |
| L. 4th | Orthofix Minirail | 0.536 | 28 | 70 | 98 | 65.3 | |
| 2 | R. 5th | Orthofix Minirail | 0.286 | 42 | 77 | 119 | 99.2 |
| L. 3rd | Orthofix Minirail | 0.724 | 29 | 90 | 119 | 56.7 | |
| L. 5th | Orthofix Minirail | 0.448 | 29 | 66 | 95 | 73.1 | |
| 3 | L. 4th | Orthofix Minirail | 0.364 | 55 | 68 | 123 | 53.5 |
| 4 | L. 4th | Orthofix Minirail | 0.293 | 41 | 65 | 106 | 88.3 |
| Average | 0.432 | 38 | 71 | 109 | 71.8 |
Note. EFI = external fixation index.
On average, the metacarpals were lengthened by 1.5 cm (range, 1.2-2.1 cm). Based on the mathematical relationship reported by Aydinlioglu et al, the average difference from the ideal length was 1.6 mm (range, 0.04-0.24 cm) (Table 4). This was within our acceptable range of ±0.2 cm for achieving correct length of the affected metacarpals. The second metacarpal was used as the reference point. This was because during the surgical planning, the senior authors estimated the amount needed to be lengthened based on what fitted the normal parabola of the hand formed by the tips of the fingers. In all cases, the second metacarpal was used as the reference point. The starting length, percent lengthened, and the difference between ideal length could not be calculated for Patient 3 because the radiographs were from an outside center and they were not calibrated. At the start, 3 of the 4 patients had trouble with extension, mean of 21° (range, 0°-40°). After the lengthening procedure, all patients were able to achieve full extension of their affected metacarpals. Similarly, flexion improved or was maintained at the normal degree of motion after the surgery for all patients except Patient 3.
Table 4.
Comparison Between Final Length Achieved and Ideal Metacarpal Length.
| Patient | Affected metacarpal | Before (cm) | After (cm) | Ideal (cm) | Difference (cm) |
|---|---|---|---|---|---|
| 1 | R. 4th | 3.2 | 4.7 | 4.91 | 0.21 |
| L. 4th | 3.3 | 4.8 | 4.91 | 0.11 | |
| 2 | R. 5th | 3.4 | 4.6 | 4.84 | 0.24 |
| L. 3rd | 3.8 | 5.9 | 5.75 | 0.15 | |
| L. 5th | 3.5 | 4.8 | 4.84 | 0.04 | |
| 4 | L. 4th | 3.6 | 4.8 | 5.00 | 0.20 |
| Average | 0.16 |
Overall, 5 of the 7 metacarpals healed without complications. Patient 2 had a fracture at the osteotomy site of the left fifth metacarpal during physical therapy after removal of the fixator. There was limitation of flexion of the MCP joint. This was resolved by open reduction and internal fixation with a dorsal plate and a dorsal capsulotomy of the MCP joint. After the additional surgery, patient went on to heal without further complications. In addition, Patient 3 experienced flexion deformity at the osteotomy site and was not able to achieve full flexion as compared with the other hand. While the metacarpal was lengthened to a clinically acceptable length, Patient 3 still had lack of a prominent knuckle on the fourth finger. At the latest follow-up, Patient 3 still experienced the same problem but stated that it did not affect the daily activities and did not want additional treatment.
The BIQLI questionnaire and LD-SRS scores were completed by 2 of the 4 patients. Two patients were lost to follow-up. Due to the small sample size, the nonparametric version Wilcoxon signed rank sum test and paired t tests could not be used to analyze the data. Of the 2 patients that completed the surveys, the patients reported a mean BIQLI score of 1.08 prior to the surgery. After the surgery, the mean BIQLI score improved to 1.55. Similarly, before the surgery, the patients reported a mean LD-SRS score of 3.8. After the surgery, the mean LD-SRS score improved to 4.2. Within the LD-SRS score, prior to the surgery, the patients reported a mean self-image/appearance score of 2.9. After the surgery, the mean self-image/appearance score improved to 4.1. The function/activity and pain scores before and after the surgery did not change, 4.2 and 4.4, respectively.
Discussion
Congenital shortening of the metacarpals is a rare deformity that affects women more than men. In contrast to other hand deformities, hand function is not seriously compromised. Surgery is indicated primarily for aesthetic and body image concerns. Various methods for lengthening the shortened metacarpals have been reported, including single-stage lengthening and fast distraction with bone graft. Single-stage lengthening has been reported to be limited to lengthening of less than 10 mm because of potential vascular compromise and complications include delay in union, malunion, and collapse of bone graft.6,9 Fast distraction with bone graft allows for lengthening of more than 10 mm but requires multiple surgical stages and can result in tendon imbalance and potential flexion deformities.6,7 Subsequently, an alternative surgical intervention is progressive distraction osteogenesis.
Progressive distraction osteogenesis has been preferred in recent years because the lengthening process is gradual, requires no bone graft, and results in less pain and better aesthetic outcomes. Although studies have documented positive results with progressive distraction osteogenesis, the literature review within the last 15 years yielded case series focusing primarily on pediatric patients (Table 5). Isolated case reports were found but were excluded in the literature review. Kato et al7 and Bulut et al3 were case series of patients with average age of 13.3 and 14.9 years, respectively. Both reported similar outcomes from the lengthening procedure, average lengthening and average percentage lengthening of 1.52 cm (43.8%) and 1.51 cm (44.2%), respectively. In both studies, several complications were reported, including problems with the fixator, finger contracture, and hypertrophic scarring. Bulut et al especially noted that the length of metacarpals and muscles that will be affected from lengthening should be considered when determining the daily rate of distraction. In contrast, Kawoosa et al8 documented no major complications except for mild pain and minor pin tract infection in their case series of 5 patients. In that case series, the average lengthening was 2.3 cm, which was the longest average lengthening of the 4 studies. Conversely, Bozan et al2 had the largest sample size of the 4 case series with 8 patients and 18 affected metacarpals. Similar to the other case series, they reported an average lengthening of 1.65 cm.
Table 5.
Literature Review.
| Authors | Year | No. of patients | No. of metacarpals | Average age | Type of fixator | Total time in fixator (weeks) | Length of distraction (mm) | % lengthened | EFI (* = HI) | Complications | Average follow-up (months) |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Kato et al | 2002 | 3 | 6 | 13.3 | Hoffmann Mini Lengthener & Orthofix | 13.9 | 15.2 | 43.8 | 62.3 days/cm | One needed bone graft Readjusting external fixator Hypertrophic scar |
45 |
| Kawoosa et al | 2004 | 5 | 5 | 17 | UMEX distractor | — | 23 | — | 1.3 mo/cm* | Mild Pain Minor pin tract infection |
— |
| Bozan et al | 2006 | 8 | 18 | 18.6 | Mini-type Semicircular Fixator & Unilateral External Fixator | 122.3 days | 16.5 | 55 | 74.1 days/cm | Pin tract infection | 23.6 |
| Bulut et al | 2013 | 4 | 7 | 14.9 | Unilateral External Fixator | 79.1 days | 15.1 | 44.2 | 51.7 day.cm | Finger contracture and pain Instability and malalignment due to fixator Pin tract infection |
34.6 |
Note. EFI = external fixation index; HI = healing index; UMEX = universal mini external fixator.
Bozan et al was the only study that included both pediatric and adult patients.2 When looking at factors that influenced the healing index, Bozan et al reported that there was a linear relationship between age and corresponding healing index.2 The healing index was defined as the time in days needed for consolidation per centimeter of distracted osteotomy site. The older the patients, the longer the healing index. In addition, both Bozan et al and Kato et al suggested that adolescence is the most appropriate time to perform distraction lengthening.2,7 Kato et al specifically recommended lengthening when patients are between ages 10 and 15 years.7 At that age, patients are motivated and able to safely manage the external fixator by themselves. More importantly, the final lengthening of the shortened metacarpal can be better estimated as the epiphyseal plates of the other metacarpals are almost closed.
In this present case series, a uniform series of skeletally mature adults, average age 22.8 years, were evaluated. Similar to the other 4 case series where all but 1 patient were females, all of the patients in this study were also females. The average amount lengthened, average percentage of lengthening, and average follow-up were also comparable to other case series. In fact, when comparing the average healing index (HI) using the definition given by Bozan et al, the average healing index in our patients was faster than the average healing index in older patients aged 19 to 30 years in the study by Bozan et al.2 The average healing index was 46.4 days/cm versus 58.7 days/cm. Furthermore, except for Bozan et al, where 7 of the 18 metacarpals lengthened used semicircular fixators, all other patients including this study used unilateral fixators. Unilateral fixators are preferred as they are not bulky and allow for the free use of the digit.
Like the other case series, several complications were encountered during the lengthening process in this study. Patient 2 experienced a fracture at the lengthening site at the left fifth metacarpal. This was because during the lengthening process, it is easier to lose flexion than extension. During physical therapy, the patient tried to work on flexion aggressively but resulted in a fracture. To avoid subsequent problems with loss of flexion, the patients’ hands were kept in flexion using a splint. From there, physical therapy was used to work on extension. Patient 3 experienced flexion deformity at the osteotomy site. This was attributed to early removal of frame. In addition, although the post distraction x-ray of Patient 1 in Figure 2c showed some anatomic axis angulation, the overall mechanical axis of the metacarpal was normal. No rotational deformity was present. As such, it did not adversely affect the ROM, function, or aesthetics of the patient.
One unique aspect of this case series was the attempt to assess the patient’s perspective in the satisfaction of the lengthening procedure using 2 different surveys, BIQLI questionnaire which measures body image and LD-SRS score which is a newly validated limb deformity score. Except for Bulut et al,3 none of the other case series evaluated patient’s satisfaction outcome. Bulut et al used the visual analog scale (VAS) to determine patient satisfaction of aesthetic outcome. Compared with preoperative and postoperative values, the VAS demonstrated a significant improvement in patient satisfaction. In this study, only 2 of the 4 patients returned the questionnaires. Therefore, the small sample size led to an inability to demonstrate statistical significance. However, of the 2 patients who responded to the surveys, both reported an increase in the scores. In the LD-SRS score, there was a marked increase in patient’s self-image/appearance, from 2.9 to 4.1. This is important as positive self-image is an integral component to the overall health of a patient. Interestingly, both the function/activity and pain scores were the same preoperatively and postoperatively, which supports the observation that brachymetacarpia does not impact hand function significantly, if at all, or cause significant pain. In this study, patients were asked to take the surveys twice, once as if before the surgery and once as if after the surgery. Although there is a possibility of recall bias, we believe the surveys were meaningful as they objectively gave the patients perspective of the surgery. If they were to do everything over again, both patients confirmed that they would choose to do the surgery. In the future, similar surveys should be used to extensively evaluate patient satisfaction with a much larger sample size.
Although brachymetacarpia is a congenital deformity, some patients might not elect to treat or have the means to treat the deformity until later in their lives. Most literature recommends lengthening of the metacarpals during adolescence. As this case series illustrates, distraction osteogenesis for the treatment of shortened metacarpal is not limited to younger patients. If proper precaution is taken to prevent MCP stiffness or fracture, distraction osteogenesis can obtain functionally successful results with improvement in body image and aesthetics without severe complications in skeletally mature adults with brachymetacarpia.
Footnotes
Ethical Approval: This study was approved by our institutional review board.
Statement of Human and Animal Rights: All procedures followed were in accordance with the ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2008.
Statement of Informed Consent: Informed consent was obtained from all individual participants included in the study.
Declaration of Conflicting Interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: AL declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article. ATF reports personal fees from Smith & Nephew, personal fees from NuVasive, personal fees from Synthes, outside the submitted work. SRR reports personal fees from Smith & Nephew, personal fees from NuVasive, personal fees from Stryker, outside the submitted work.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Aydinlioglu A, Akpinar F, Tosun N. Mathematical relations between the lengths of the metacarpal bones and phalanges: surgical significance. Tohoku J Exp Med. 1998;185(3):209-216. [DOI] [PubMed] [Google Scholar]
- 2. Bozan ME, Altinel L, Kuru I, et al. Factors that affect the healing index of metacarpal lengthening: a retrospective study. J Orthop Surg (Hong Kong). 2006;14(2):167-171. [DOI] [PubMed] [Google Scholar]
- 3. Bulut M, Ucar BY, Azboy I, et al. Lengthening by distraction osteogenesis in congenital shortening of metacarpals. Acta Orthop Traumatol Turc. 2013;47(2):79-85. [DOI] [PubMed] [Google Scholar]
- 4. Cash TF, Fleming EC. The impact of body image experiences: development of the Body Image Quality of Life Inventory. Int J Eat Disord. 2002;31(4):455-460. [DOI] [PubMed] [Google Scholar]
- 5. Fabricant PD, Borst EW, Green SA, et al. Validation of a modified Scoliosis Research Society instrument for patients with limb deformity: the Limb Deformity-Scoliosis Research Society (LD-SRS) score. J Limb Lengthen Reconstr. 2016;2(2):86-93. [Google Scholar]
- 6. Fultz CW, Lester DK, Hunter JM. Single stage lengthening by intercalary bone graft in patients with congenital hand deformities. J Hand Surg Br. 1986;11(1):40-46. [DOI] [PubMed] [Google Scholar]
- 7. Kato H, Minami A, Suenaga N, et al. Callotasis lengthening in patients with brachymetacarpia. J Pediatr Orthop. 2002;22(4):497-500. [PubMed] [Google Scholar]
- 8. Kawoosa AA, Mir NA, Badoo AR, et al. Metacarpal lengthening by distraction osteogenesis. JK-Practitioner. 2004;11(1):32-34. [Google Scholar]
- 9. Ogino T, Kato H, Ishii S, et al. Digital lengthening in congenital hand deformities. J Hand Surg Br. 1994;19(1):120-129. [DOI] [PubMed] [Google Scholar]
- 10. Rayan GM, Upton J., III Congenital Hand Anomalies and Associated Syndromes. Berlin, Germany: Springer;2014. [Google Scholar]
- 11. Rozbruch SR. Case 98: bilateral metacarpal lengthening for congenital brachymetacarpia. In: Rozbruch SR, Hamdy RC. eds. Limb Lengthening and Reconstruction Surgery Case Atlas: Adult Deformity, Tumor, Upper Extremity. Basel, Switzerland: Springer; 2015:673-679. [Google Scholar]
- 12. Saito H, Koizumi M, Takahashi Y, et al. One-stage elongation of the third or fourth brachymetacarpia through the palmar approach. J Hand Surg Am. 2001;26(3):518-524. [DOI] [PubMed] [Google Scholar]
- 13. Volpi AD, Fragomen AT. Percutaneous distraction lengthening in brachymetacarpia. Orthopedics. 2011;34(8):e424-e427. [DOI] [PubMed] [Google Scholar]