Abstract
Objectives
To evaluate the effectiveness of clinical pharmacists and community health workers (CHWs) in improving glycemic control within a low-income, ethnic minority population.
Methods
In a two-arm, 2-year, crossover trial, 179 African-American and 65 Hispanic adult patients with uncontrolled diabetes mellitus (hemoglobin A1c [HbA1c] ≥ 8%) were randomized to CHW support either during the first or second year of the study. All participants received clinical pharmacist support for both years of the study. The primary outcome was change in HbA1c over 1 and 2 years.
Results
Similar HbA1c declines were noted after receiving the 1-year of CHW support: −0.45% [95% confidence interval [CI] −0.96, 0.05] with CHW versus −0.42% [95% CI −0.93, 0.08] without CHW support. In addition, there were no differences in change on secondary outcome measures, including body mass index (BMI), systolic blood pressure (SBP), high-density lipoprotein (HDL)-, and low-density lipoprotein (LDL)-cholesterol, quality of life, and perceived social support. A difference in diastolic blood pressure change was noted: 0.80 mm Hg [95% CI −1.92, 3.53] with CHW versus −1.85 mm Hg [95% CI −4.74, 1.03] without CHW support (p=0.0078). Patients receiving CHW support had more lipid-lowering medication intensifications (0.39 [95% CI 0.27, 0.52]) compared to those without CHW support (0.26 [95% CI 0.14, 0.38]; p<.0001). However, no significant differences in intensification of antihyperglycemic and antihypertensive medications were observed between patients receiving CHW support and those without CHW support. Patients with low health literacy completed significantly more encounters with the pharmacist and CHW than those with high health literacy; although outcomes were comparable.
Conclusions
No significant differences were noted between a clinical pharmacist-CHW team and clinical pharmacist alone in improving glycemic control within a low-income, ethnic minority population.
Keywords: diabetes complications, disparities, adherence with treatment, community health, pharmacist, randomized clinical trial
Introduction
Approximately 9% of American adults are diagnosed with type 2 diabetes mellitus; although individuals living in poverty and ethnic minorities are disproportionately affected.1 Current health care delivery approaches for these vulnerable groups, particularly African-American and Hispanic/Latino, are inadequate.2 A range of interventions with primary care providers, nurses, dieticians, pharmacists, and community health workers (CHWs) designed to improve glucose and cardiovascular control in diverse patient populations have resulted in mixed results.3, 4 However, the most effective interventions studied to date consist of multidisciplinary teams providing a range of components.3 Within the routine clinical environment, these interventions are most consistent with the patient-centered medical home framework.5 This model of care typically involves coordinated, team-based disease management that considers patient context, including family and community. Clinical pharmacists and CHWs are often involved in medical home teams working with patients on chronic disease management.6
Clinical pharmacists provide expertise in medication-related issues (e.g., drug interactions and cost), encourage adherence, provide patient education, and adjust therapy in collaboration with providers resulting in improvements in a range of clinical outcomes.7–9 A recent meta-analysis of diabetes outcomes with clinical pharmacy support identified 35 studies and found a moderate effect representing a mean reduction in hemoglobin A1c (HbA1c) of 1.1% (95% confidence interval [CI] 0.88, 1.27) with pharmacist care in the ambulatory setting.4 Pharmacist involvement varied from providing patient education to medication adjustment via prescriptive authority.
Community health workers are uniquely prepared to work with vulnerable populations. Patients trust CHWs who understand their socio-cultural barriers, provide social support, speak the same language, and can increase the relevancy of disease self-management for individuals who are often struggling to manage competing priorities. Importantly, mounting evidence suggests that CHW involvement can contribute to improvement in diabetes self-management as well as significant decreases in HbA1c that have ranged from 0.5% to 0.9%.10–14
A pilot study partnering clinical pharmacists with CHWs to serve minority patients with poorly-controlled type 2 diabetes mellitus demonstrated feasibility of this collaborative approach.15 In the pilot, nine Latino patients with HbA1c values of 8% or higher were recruited from within a general medicine clinic. During a 6-month period, a bilingual Latina CHW provided self-management guidance, medical follow-up assistance, and support for increased medication adherence during home and clinic visits along with telephone contact. Additionally, pharmacists met in-person with the patient and the CHW to conduct medication therapy management. Although this pilot study was small and without a comparison group, mean HbA1c values among participants declined from 9.6% to 9.0%. Building on this work, the present randomized-controlled trial explored the effectiveness of a clinical pharmacist-CHW team compared to clinical pharmacy services alone in improving HbA1c (primary outcome), lipids, and blood pressure within a high-risk group of Hispanic/Latino and African-American patients with type 2 diabetes mellitus. The crossover design investigated the benefit derived from adding CHW support following receipt of clinical pharmacist services for 1 year and the maintenance of any HbA1c improvement after phasing out CHW support.
Materials and Methods
The University of Illinois (UI) at Chicago Institutional Review Board approved the study protocol. Details of the design of this randomized, two-arm, two-period crossover study were published previously (including sample size determination).16
Inclusion criteria were: (i) self-identified as Hispanic/Latino or African-American; (ii) verbal fluency in English or Spanish; (iii) 21 years of age or older; (iv) existing diagnosis of type 2 diabetes mellitus; (v) HbA1c of 8% or higher in the past year; (vi) received primary care through UI Health during the past year; and (vii) prescribed at least one oral medication for diabetes or hypertension. Exclusion criteria were: (i) inability to verbalize comprehension of study or evidence of impaired decision making (e.g., dementia); (ii) resided outside of the Chicago area 3 or more months of the year or planned to move from the Chicago area; (iii) had a household member already participating in same study; or (iv) currently pregnant or trying to become pregnant.
Recruitment and Randomization
A convenience sample was recruited from four primary care ambulatory sites within an academic medical setting that provides care for a diverse, low-income population in Chicago. Research assistants (RAs) fluent in the participants’ preferred language (English or Spanish) worked with clinic staff to identify patients with type 2 diabetes presenting for a regularly scheduled visit. The RAs screened interested patients for initial eligibility and provided study details when appropriate. Patients’ provided telephone numbers to be contacted for study enrollment pending confirmation of HbA1c of 8% or higher in the past year by a physician investigator who reviewed each patient’s electronic medical record (EMR). Upon arrival, RAs obtained written informed consent and Health Insurance Portability and Accountability Act (HIPAA) authorization followed by a computer-assisted personal interview. A nurse conducted venipuncture for HbA1c and lipid profile, and measured height, weight, and sitting blood pressure. Laboratory values were entered into the EMR by a study physician and forwarded to the primary care physician (PCP) and pharmacist. Follow-up data were similarly collected at 12- and 24-months with $40 compensation for each data collection.
After baseline data collection, RAs scheduled an initial pharmacist encounter and determined sequence assignment. Randomization was blocked by gender, ethnicity, and site using a computer-generated random order of sequence assignments. One sequence received only clinical pharmacist visits during the first year with the CHW added during the second year. The second sequence received a clinical pharmacist plus CHW during the first year but only the pharmacist in year 2. The project coordinator independently applied randomization, maintained concealment, and logged the information separately. Those randomized to a CHW met her face-to-face and scheduled an initial home visit. In rare instances when a CHW introduction was not possible, patients received a written welcome letter from the CHW (with her photograph) and the CHW contacted the patient within 24 hours to schedule a visit.
Pharmacist Intervention
Pharmacists provided medication and disease management services to patients following an established Pharmacist Management Protocol,16 which included a comprehensive needs assessment, health promotion, patient-centric goal setting and education, interventions to encourage behavioral change, and collaboration with the PCP. The CHWs were present during pharmacist encounters when schedules allowed, and often translated for Spanish-speaking patients. The initial pharmacist encounter included medication reconciliation, identification of therapeutic goals (particularly HbA1c and blood pressure), formulation of a PCP-approved plan of care, and documentation of the plan in the EMR. The CHWs worked with patients to maintain a record of home glucose and blood pressure monitoring data, which was encouraged and reviewed by pharmacists when available. The PCPs and pharmacists used medication intensification algorithms based on national guidelines.17, 18 Per guidelines, less stringent goals were implemented for patients with a history of severe hypoglycemia, limited life expectancy, advanced micro- or macrovascular disease, or extensive comorbid conditions. In collaboration with CHWs, pharmacists assessed common barriers to medication adherence including poor memory, lack of diabetes knowledge, health beliefs, cost, medication burden, physical disabilities, and social barriers. Pharmacists also addressed medications (name and purpose of medications; time, strength, and method of administration); drug interactions and side effects; goals of therapy; basic lifestyle modifications; and use of pillboxes, low-literacy medication lists, or other adherence aids. Communication between the pharmacist and CHW included secure emails, telephone contact, and face-to-face discussion before or after patient encounters.
Community Health Worker (CHW) Intervention
Though college-educated, the CHWs otherwise shared many sociodemographic characteristics with the patient population served including ethnic background and language (there was ethnic concordance between patients and CHWs). Standardized CHW training included two educational curricula: the Diabetes Empowerment Education Program19 and the adapted Training Curriculum for Health Coaches.20 Additional training was provided by a licensed clinical dietician with certification in diabetes health education (3 hours), an endocrinologist (1 hour), motivational interviewing certified trainer (4 hours), pharmacist (2 hours), clinical health psychologist (3 hours), and PCP (2 hours). CHWs shadowed pharmacists to observe pharmacist-patient interactions in the UI Health Medication Therapy Management Clinic for 2 days to gain insight into routine clinical pharmacist activities. CHW competencies in counseling and diabetes-related clinical skills were assessed with feedback in structured patient simulations.
CHWs visited patients in their homes and communicated with them by telephone. They attempted to meet with patients monthly for the first 3 to 4 months to establish a relationship; however, the number of home visits per year varied based on patient availability and willingness. With patients’ permission, CHWs accompanied them to PCP and pharmacist encounters. These interactions included preparing questions for providers and identifying goals for each visit beforehand. After visits, information was reinforced (e.g., provider instructions, scheduling tests and appointments, medication changes, etc.). Specific CHW activities were individualized based on patient preferences, needs, and values. Examples included social support, diabetes self-management education, problem-solving skill building, health care navigation, translation, and referrals to resources (e.g., food pantries and housing shelters). As mentioned, CHWs and pharmacists communicated with each other in-person, by telephone, and through secure email to coordinate patient management. CHWs participated in weekly face-to-face supervision facilitated by a study PCP and health psychologist throughout the study period. During these weekly team meetings, they discussed patients seen during the past week, those unable to be reached, and individuals with challenging and complex psychological and social problems. The meetings ensured CHWs followed the protocol, minimizing drift in intervention delivery. Team meetings also offered CHWs psychological support as they managed patients with severe poverty and stressful life events.
Outcomes and Measurements
The primary outcome was change in HbA1c. The secondary outcomes were changes in systolic and diastolic blood pressure, high-density lipoprotein (HDL) cholesterol, low-density lipoprotein (LDL) cholesterol, body mass index (BMI), quality of life, and perceived social support. Alverno Laboratory (Hammond, IN; NGSP certified) processed all blood testing. Blood pressure was measured after participants sat quietly for 5 minutes (Welch Allyn Spot Vital Signs LXi). Height was obtained via stadiometer, and weight was measured with light clothing and without shoes. The surveys included validated measures of diabetes-specific quality of life (4-item Diabetes Distress Scale);21 social support from friends, family, and healthcare team (selected 4 items);22 health literacy (3-item health literacy screen);23 diabetes knowledge (Spoken Knowledge in Low Literacy in Diabetes scale);24 depression (Patient Health Questionnaire-2 screen);25 a single-item global health status26 (self-reported); and demographics. These survey measures were considered as potential covariates in mixed-effect modeling.
Medical Record Abstraction
At the end of the study, EMRs were abstracted to capture number of pharmacist encounters and number of intensifications of diabetes, hypertension, and/or hyperlipidemia medications. Medication changes were considered intensification events when a progress note indicated an increase in the number of agents (a new therapeutic class), an increase in the medication dosage, or a change to a different agent.
The number of intensification events, as well as percentage of patients with any intensification events were reported. In addition, CHW contact records with participants were tabulated. Face-to-face contact was defined as a home visit or encounter within the health care setting before or after a scheduled provider visit.
Statistical Analyses
All analyses were intention-to-treat. Descriptive statistics for continuous variables were expressed as mean ± standard deviation (SD), whereas categorical variables were expressed as frequencies and proportions. P-values of less than 0.05 were considered to be statistically significant. To detect differences in baseline characteristics, intensification events, and outcome measures between the two sequence arms, two-sample t tests or nonparametric Wilcoxon rank-sum tests were used for continuous variables, and χ2 tests or Fisher exact tests for categorical variables. Gender, ethnicity, and site were included as control variables in the models initially, but are not shown because the results were unchanged. Given the crossover design of this study, mixed-effect modeling was performed on primary and secondary outcomes. The mixed-effect model with random intercept controls for repeated measurement and produces correct standard errors of estimates. Each outcome was analyzed as a measure at each time point and as a change within each time period. For the crossover design, treatment was defined as receipt of CHW support (true or false), period as year in time (1 or 2), and sequence as year receiving CHW support (1 or 2). The final model included fixed-effects for design variables (treatment, period, and sequence), demographic characteristics (age, gender, race, insurance, health literacy), and baseline HbA1c with random effects for subject. These variables were selected because they were clinically relevant and/or statistically associated with the outcome (p<0.1). All statistical analyses were conducted by SAS version 9.4 (SAS Institute Inc., Cary, NC, USA).
Treatment of Missing Data
Missing HbA1c data were obtained from the EMR when available. HbA1c values near the targeted data collection date were identified in 28 instances. For the remaining missing data, multiple imputation followed by fitting of the mixed-effect model on the imputed data was conducted. The reported estimated means and mean changes were combined from 20 imputed datasets. As a secondary analysis, extreme changes of HbA1c values were truncated and the same analyses were repeated. The main results did not differ with the additional EMR data, imputation, or truncation of extreme values. Missing data for the additional outcomes were addressed with the same multiple imputation procedures. To explore the unexpected finding of diastolic blood pressure change between treatments, multiple imputation was conducted with a worst-case scenario where missing values were replaced with the worst observed value during the study period. The same mixed-effects model was then applied with no difference in result.
Results
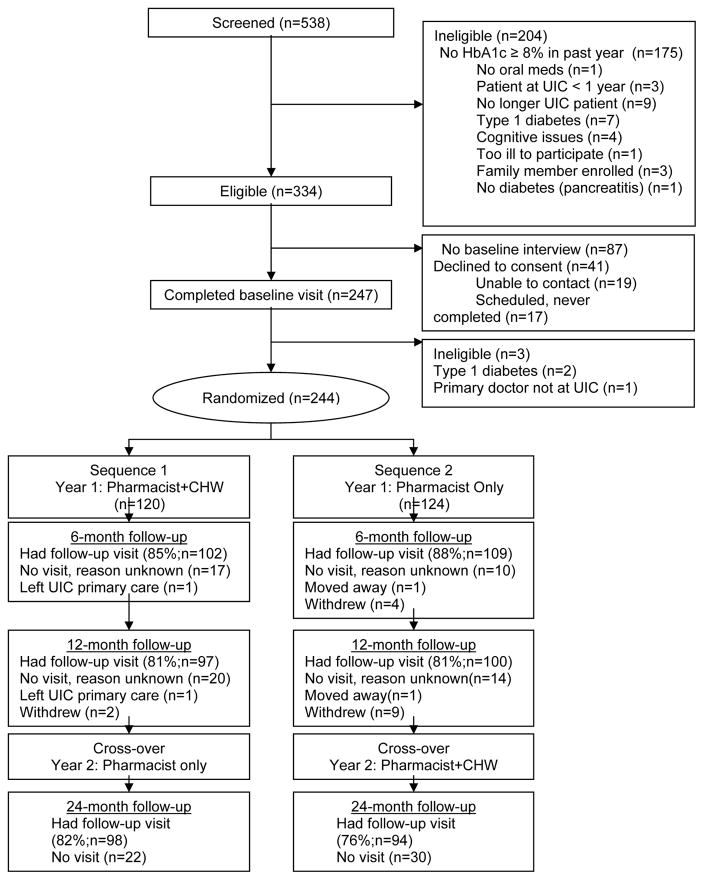
Figure 1 describes screening, randomization, and participant flow during the 24-month study period. Of the 538 patients screened, 334 were deemed eligible for the study (62%) and 247 completed baseline data collection. However, three of those patients were subsequently deemed ineligible resulting in a final sample of 244 patients. For year 1, 124 patients were randomized to initially receive only pharmacist support, and 120 to receive both pharmacist and CHW support. Baseline characteristics were balanced between the two randomly assigned sequence groups (Table 1).
Figure 1. Study Design and Randomization.
Study design and randomization. CHW, community health workers; HbA1c, Hemoglobin A1c; UIC, University of Illinois at Chicago.
Table 1.
Demographic Characteristics at Baseline
| Characteristic | Sequence 1 Pharmacist+CHWa (N=120) | Sequence 2 Pharmacist Onlya (N=124) | Both Groups Combined (N=244) | Between-Group Difference P-value |
|---|---|---|---|---|
| Age in years; mean (SD) | 53.83 (10.5) | 54.57 (11.7) | 54.21 (11.15) | 0.61 |
| Gender N (%) | 0.52 | |||
| Female | 83 (69.2) | 81 (65.3) | 164 (67.2) | |
| Male | 37 (30.8) | 43 (34.7) | 80 (32.8) | |
| Race/Ethnicity N (%) | 0.99 | |||
| African American/Black | 88 (73.3) | 91 (73.4) | 179 (73.4) | |
| Hispanic/Latino | 32 (26.7) | 33 (26.6) | 65 (26.6) | |
| Income Level b N (%) | 0.35 | |||
| < $10,000 | 46 (46.5) | 40 (36.7) | 86 (41.4) | |
| $10,000–$20,000 | 25 (25.3) | 31 (28.4) | 56 (26.9) | |
| >$20,000 | 28 (28.3) | 38 (34.86) | 66 (27.1) | |
| Highest Education Level N (%) | 0.74 | |||
| Less than high school | 33 (27.5) | 39 (31.5) | 72 (29.5) | |
| High school diploma/GED | 58 (48.3) | 59 (47.6) | 117 (48.0) | |
| Some college/graduated college | 29 (24.2) | 26 (21) | 55 (22.5) | |
| Employment Status N (%) | 0.46 | |||
| Disabled and unable to work | 61 (50.8) | 56 (45.5) | 117 (48.2) | |
| Retired | 14 (11.7) | 21 (17.1) | 35 (14.4) | |
| Out of work/unemployed | 18 (15.0) | 13 (10.6) | 31 (12.8) | |
| Work (full- or part-time) | 25 (21.2) | 28 (23.7) | 53 (21.7) | |
| Marital Status N (%) | 0.90 | |||
| Single, never married | 50 (41.7) | 54 (43.6) | 104 (42.6) | |
| Married or living with partner | 34 (28.3) | 36 (29.0) | 70 (28.7) | |
| Widowed/separated/divorced | 36 (30.0) | 34 (27.4) | 70 (28.7) | |
| Health Insurance N (%) | 0.30 | |||
| None | 4 (3.3) | 9 (7.4) | 13 (5.4) | |
| Public aid/Medicaid/Medicare | 96 (80) | 89 (73.6) | 185 (75.8) | |
| HMO/PPO | 20 (16.7) | 23 (19.0) | 43 (17.8) | |
| Health Status N (%) | 0.96 | |||
| Excellent/Very Good/Good | 47 (39.2) | 49 (39.5) | 96 (39.3) | |
| Fair/Poor | 73 (60.8) | 75 (60.5) | 148 (60.7) | |
| Diabetes duration; mean yrs (SD) | 13.24 (8.7) | 13.66 (8.9) | 13.45 (8.8) | 0.71 |
| Health literacy; mean (SD) | 6.43 (3.4) | 6.59 (3.5) | 6.51 (3.42) | 0.73 |
| Diabetes knowledge; mean (SD) | 5.29 (1.8) | 5.45 (1.9) | 5.37 (1.8) | 0.50 |
| Diabetes social support; mean (SD) | 15.73 (4.2) | 15.94 (3.9) | 15.83 (4.1) | 0.69 |
| Quality of life; mean (SD) | 13.77 (6.3) | 13.38 (5.7) | 13.57 (6.0) | 0.61 |
| Depression (PHQ-2); mean (SD) | 1.90 (2.0) | 1.80 (1.9) | 1.85 (2.0) | 0.69 |
| Physiologic | ||||
| HbA1c (%); mean (SD) | 9.43 (2.0) | 9.57 (1.8) | 9.50 (1.9) | 0.57 |
| SBP (mm Hg); mean (SD) | 134.18 (20.5) | 134.17 (17.9) | 134.17 (19.2) | 0.99 |
| DBP (mm Hg); mean (SD) | 79.08 (13.7) | 80.25 (12.1) | 79.67 (12.9) | 0.48 |
| BMI (kg/m2); mean (SD) | 35.74 (8.9) | 36.81 (9.6) | 36.29 (9.3) | 0.37 |
| LDL (mg/dL); mean (SD) | 98.19 (41.3) | 91.90 (33.4) | 94.97 (37.5) | 0.20 |
| HDL (mg/dL); mean (SD) | 48.7 2(14.3) | 47.90 (12.7) | 48.30 (13.5) | 0.64 |
Notes:
Initial treatment assignment in year 1;
Income in sequence 1 missing (N=21) and sequence 2 missing (N=15).
BMI, body mass index; CHW, community health workers; DBP, diastolic blood pressure; GED, general education diploma; HbA1c, hemoglobin A1c; HDL, high-density lipoprotein; LDL, low-density lipoprotein; PHQ-2, patient health questionnaire-2; SBP, systolic blood pressure; SD, standard deviation; UIC, University of Illinois at Chicago; HMO, health maintenance organization; PPO, preferred provider organization; yrs, years.
Utilization of Interventions
Clinical pharmacist and CHW contact varied among participants. During the study period, 83.6% of the 244 participants had at least one pharmacist encounter, with a mean of 7.1 (SD=8.2) per participant over 2 years. Pharmacist utilization was greater during year 1 than year 2 (1162 vs. 564 encounters, p<0.001), but there were no differences in the number of encounters between treatment groups (6.7 for pharmacist only vs. 7.4 with CHW, p=0.504). The number of pharmacist encounters did not differ by ethnic group. However, those with low health literacy completed on average 9.7 (SD=10.4) pharmacist visits compared to 7.2 (SD=7.7; p<0.05) among those with high literacy.
Overall, 77.5% of participants completed at least one CHW encounter. However, 91.7% of those with CHW support during year 1 completed at least one encounter versus 63.7% receiving CHW support in year 2 (p<0.0001). In addition, there was a significant difference in the number of CHW encounters between groups. On average, those who received CHW in year 1 completed 6.5 (SD=5.3) encounters compared to 3.4 (SD=4.1; p<0.001) with CHW support in year 2. Patients with low health literacy had a mean 8.4 (SD=7.0) CHW visits compared to 6.5 CHW visits (SD=5.2; p=0.012) in those with high health literacy.
Glycemic Control and Secondary Outcomes
Of the 244 patients enrolled, 197 (81%) completed 12-month and 192 (79%) completed 24-month data collection. Both treatments showed a similar decline in HbA1c (Table 2). Patients receiving pharmacist plus CHW support had an average decrease of HbA1c of −0.45% (95% CI [−0.96, 0.05]) compared to −0.42% (95% CI [−0.93, 0.08]) in those receiving only pharmacist support. There were no differences between treatments in change in secondary outcomes including BMI, systolic blood pressure, HDL- and LDL-cholesterol, self-reported medication adherence, quality of life, and perceived social support. Change in diastolic blood pressure was 0.80 mm Hg (95% CI [−1.92, 3.53]) for pharmacist plus CHW compared with. −1.85 mm Hg (95% CI [−4.74, 1.03]) for pharmacist only (p=0.0078).
Table 2.
Results of Crossover (Mixed-Effect Model) Analysis
| Outcome | Pharmacist + CHW | Pharmacist only | Difference | |||
|---|---|---|---|---|---|---|
|
| ||||||
| Estimate [95%CI] | Estimate [95%CI] | Estimate | SD | 95%CI | P-value | |
|
| ||||||
| HbA1c (%) | ||||||
| Change | −0.45 [−0.96, 0.05] | −0.42 [−0.93, 0.08] | −0.03 | 0.15 | −0.32,−0.26 | 0.84 |
| Raw | 8.84 [ 8.36, 9.32] | 8.89 [ 8.40, 9.38] | −0.05 | 0.13 | −0.31, 0.22 | 0.72 |
|
| ||||||
| SBP (mmHg) | ||||||
| Change | 1.26 [−3.15, 5.67] | −1.00 [−5.64, 3.62] | 2.27 | 1.61 | −0.90, 5.43 | 0.16 |
| Raw | 133.0 [128.76, 137.24] | 132.78 [128.53, 137.02] | 0.22 | 1.31 | −2.34, 2.79 | 0.86 |
|
| ||||||
| DBP (mmHg) | ||||||
| Change | 0.80 [−1.92, 3.53] | −1.85 [−4.74, 1.03] | 2.65 | 0.99 | 0.70, 4.61 | 0.0078 |
| Raw | 78.38 [75.93, 80.83] | 77.77 [75.32, 80.22] | 0.61 | 0.82 | −1.00, 2.21 | 0.46 |
|
| ||||||
| BMI (kg/m2) | ||||||
| Change | −0.20 [−1.15, 0.74] | −0.22 [−1.17, 0.73] | 0.02 | 0.20 | −0.38, 0.41 | 0.93 |
| Raw | 35.91 [35.00, 36.83] | 36.16 [35.23, 37.08] | −0.24 | 0.19 | −0.62, 0.14 | 0.21 |
|
| ||||||
| LDL (mg/dl) | ||||||
| Change | −2.93[−10.60, 4.74] | −2.66[−9.79, 4.467] | −0.27 | 2.76 | −5.70, 5.16 | 0.92 |
| Raw | 91.34[82.99, 99.70] | 91.08[82.87, 99.28] | 0.266 | 2.05 | −3.74, 4.28 | 0.90 |
|
| ||||||
| HDL (mg/dl) | ||||||
| Change | −0.82 [−3.14, 1.49] | −1.61 [−3.87, 0.65] | 0.79 | 0.79 | −0.77, 2.34 | 0.32 |
| Raw | 46.63 [44.83, 48.43] | 46.96 [45.17, 48.76] | −0.34 | 0.58 | −1.47, 0.80 | 0.56 |
|
| ||||||
| Social support | ||||||
| Change | 0.53 [−0.30, 1.36] | 0.64 [−0.22, 1.50] | −0.11 | 0.26 | −0.63, 0.41 | 0.65 |
| Raw | 16.58 [15.59, 17.57] | 16.53 [15.53, 17.52] | 0.06 | 0.21 | −0.35, 0.46 | 0.79 |
|
| ||||||
| Quality of life | ||||||
| Change | −1.51 [−2.89, −0.13] | −1.59 [−2.95, −0.22] | 0.08 | 0.43 | −0.78, 0.93 | 0.86 |
| Raw | 11.46 [10.26, 12.67] | 11.60 [10.37, 12.83] | −0.14 | 0.36 | −0.85, 0.58 | 0.71 |
Overall (pooled) estimates of main outcomes for pharmacist and pharmacist plus CHW interventions from multiple imputed data. Pharmacist + CHW and Pharmacist columns represent the estimated effect of the intervention adjusted for sequence, period, and covariates. The difference column represents the estimated difference between the two treatments (with and without CHW).
BMI, body mass index; CHW, community health workers; confidence interval, CI; DBP, diastolic blood pressure; HbA1c, hemoglobin A1c; HDL, high-density lipoprotein; LDL, low-density lipoprotein; SBP, systolic blood pressure, SD, standard deviation.
The final crossover design mixed-effects model showed no significant treatment or sequence effects. However, there was a greater reduction in HbA1c during year 1 compared to year 2 (p<.0001) with baseline HbA1c (p<.0001) negatively associated with the mean change in HbA1c. No other covariates were significant. Additional exploratory analyses showed no difference between having a pharmacist-CHW team compared to a pharmacist alone in terms of the number of patients reaching goal in HbA1c (either ≤7% or ≤8%), at either 12 or 24 months.
Medication Intensification
The number of intensification events was similar across treatments for antihyperglycemic and antihypertensive medications (Table 3). However, there were more intensifications in lipid-lowering medications when working with pharmacist plus CHW (0.39 (95% CI [0.27, 0.52])) compared to the pharmacist alone (0.26 (95% CI ([0.14, 0.38]), p<.0001). Similarly, a comparable percentage of patients working with a CHW and pharmacist versus pharmacist only had any antihyperglycemic or antihypertensive medication intensifications, whereas significantly more patients working with a CHW and pharmacist had intensifications in antilipid medication compared to those working with only a pharmacist (Table 4).
Table 3.
Number of Medication Intensifications
| Intensification | Pharmacist + CHW | Pharmacist | Difference | |||
|---|---|---|---|---|---|---|
| Estimate [95%CI] | Estimate [95%CI] | Estimate | SE | 95% CI | P-value | |
| Antihyperglycemic | 1.51 [0.83, 2.18] | 1.60 [0.93, 2.28] | −0.09 | 0.11 | −0.31, 0.12 | 0.38 |
| Antihypertensive | 0.49 [0.20, 0.78] | 0.40 [0.11, 0.69] | 0.09 | 0.06 | −0.02, 0.21 | 0.11 |
| Antilipid | 0.39 [0.27, 0.52] | 0.26 [0.14, 0.38] | 0.13 | 0.03 | 0.08, 0.19 | <0.0001 |
CHW, community health workers; CI, confidence interval; SE, standard error.
Table 4.
Percentage of Patients with Medication Intensification by Year
| Intensification | Year 1 | Year 2 | ||||
|---|---|---|---|---|---|---|
| Pharmacist + CHW (%) | Pharmacist (%) | P-value | Pharmacist + CHW (%) | Pharmacist (%) | P-value | |
| Antihyperglycemic | 70.83 | 70.97 | 0.98 | 56.45 | 54.17 | 0.72 |
| Antihypertensive | 35.00 | 31.45 | 0.56 | 31.45 | 24.17 | 0.20 |
| Antilipid | 29.17 | 15.32 | 0.01 | 20.16 | 10.00 | 0.03 |
CHW, community health workers.
Discussion
Patients receiving pharmacist management, with or without CHW support, demonstrated improvement in HbA1c. The magnitude of change may be clinically significant with an estimated mean decrease of 0.42% to 0.45% over 2 years.27–29 Secondary outcomes were unchanged with the exception of diastolic blood pressure (participants with pharmacist-only intervention experienced slightly lower diastolic pressure, possibly a spurious relationship). Finally, significantly more intensifications of lipid-lowering medication were noted when participants were working with the CHW compared to the pharmacist alone. A recent study of diabetic Latinos receiving CHW support also demonstrated an increase in lipid-lowering intensification.13 The reason for this effect is unclear. It is conceivable that CHW-pharmacist communication, including medication reconciliation, created more opportunities to restart or intensify statin prescriptions. Although a CHW intervention with patients experiencing acute coronary syndrome did result in lower LDL and total cholesterol, similar outcomes have not extended to CHW interventions and patients with diabetes.13, 14, 30
From a process standpoint, it was noteworthy that patients randomized to receive CHW support during their first year had more face-to-face visits with CHWs than those who received CHW support after 1 year of pharmacist-only support. Several factors might account for this pattern of engagement. Introducing CHWs to patients immediately following data collection was challenging, particularly mid-study because patients were accustomed to leaving immediately after data collection. Many patients reported reasons for why they could not stay to meet with CHWs (e.g., need to get to work, a ride cannot wait, etc.). Relatedly, there was limited change in HbA1c during the second year overall, possibly due to lower patient motivation, less patient-pharmacist contact, and some patients reaching their therapeutic goals.
As is common with behavioral interventions, some patients were engaged more than others. Specifically, patients with low health literacy had more visits with both CHWs and pharmacists than those with high health literacy, and Hispanics/Latinos had more CHW visits than African Americans. Low health literacy is a known barrier to diabetes self-management.31 Furthermore, mistrust of health care providers is more common among patients with diabetes and low health literacy than those with adequate health literacy.32 The higher incidence of visits with pharmacists among the patients with low health literacy may relate to the fact that the CHWs accompanied patients to pharmacy visits and translated for Spanish-speaking patients. The CHW model is uniquely suited to patients with low health literacy, mistrust, and poor communication with providers. Unfortunately, more visits did not translate into improved outcomes when compared to those with high health literacy. Notably, many Hispanic/Latino patients appreciated having a Spanish-speaking advocate within the clinical setting where language barriers were prevalent. Indeed, language discordance between patient and provider contributes to poor glycemic control.33 However, the small number of Hispanic/Latino patients with limited English proficiency reduced the ability to make meaningful comparisons by ethnic groups.
Overall, the 2-year improvement in HbA1c was comparable to other CHW-driven intervention studies, yet slightly less than other pharmacist-collaborator models, which average a 1.1% decrease in HbA1c over 6 to 12 months.4, 25, 34–36 In comparison, the improvement in HbA1c over the first 12 months was 0.87% in this study. As is commonly found in pharmacist-led chronic disease programs,9 our study provided frequent follow-up encounters to conduct medication monitoring and patient education. Although it may be anticipated that prescriptive authority could result in greater improvement in HbA1c, other factors must be considered. For example, a lack of reliable transportation represents an important barrier to care access among our population and reportedly limited the number of pharmacist visits.37
This study has several limitations. First, all participants received pharmacist support making it impossible to know what change might have occurred with routine medical care alone. Specifically, regression towards the mean38 cannot be excluded. Second, individuals were randomized within clinics (not cluster randomized). It is possible, though unlikely, that patients receiving CHW support may have influenced those in the other condition, consequently reducing between-treatment differences in outcomes. Also, carryover remains a potential issue in crossover design. The CHWs’ contributions were mostly immediate and within the period of CHW exposure, such as problem solving and direct support. However, it is possible that CHWs also conveyed knowledge or modeled how to resolve problems, some of which sequence-1 participants may have partially retained, so there could have been a degree of carryover effect as well into year 2. Third, these results might not generalize to other practices and settings. The pharmacist-CHW teams were implemented in several sites within a single academic medical center and the effectiveness of the pharmacist-CHW team likely varied. Pharmacist and CHW communication about patient care was challenging outside of pharmacist encounters, despite the fact that the pharmacists reported positive experiences working with CHWs and felt that patients likely benefited from their involvement.39 Work-related scheduling conflicts prevented consistent and on-going collaboration. The “intervention dose” provided by the CHW and pharmacist varied across patients, as is common in similar studies.13 For example, whereas some patients completed monthly face-to-face encounters with the CHW and pharmacist, others may have had only a few pharmacist encounters or preferred telephone contact with the CHWs. The relatively low engagement by some patients, particularly in year 2, may further reduce the probability of detecting changes in outcomes between treatments and may affect differences detected between time periods, following our intention-to-treat analysis. Also, it is important to note that a relationship between the number of CHW encounters and HbA1c improvement was not detected in analyses. Although some may conclude that CHWs truly offer no additional benefit to clinical pharmacy support in terms of HbA1c control, this conclusion may be premature. The population under study had numerous comorbid health conditions along with complicated psychosocial challenges and other serious barriers (e.g., death of loved ones, housing instability, and exacerbation of other chronic illness).40 The CHWs reported that these contextual issues challenged patients’ ability to focus on diabetes self management. Documentation from CHWs’ visits suggested that they often spent time providing psychological support and resources to patients. A number of patients lacked basic access to adequate food, a safe environment, or sufficient finances. The CHWs were trained to assess the patient’s life context and then work with them to increase their diabetes self-management skills within the reality of that context. It is possible that some patients engaged with the CHW component more for the resources and advocacy for their daily needs than for the diabetes-related self-management support.
The CHWs reported that several patients refused to engage in on-going pharmacist support because of the need for transportation to attend an additional visit and waiting room time. A randomized study is currently being conducted to evaluate whether the use of remote clinical pharmacist video conferencing and text messaging can address these barriers. Video conferencing, where CHWs provide Internet-enabled iPads to patient homes, will allow patient interactions with clinical pharmacists routinely without need for transportation. Text messaging will further promote patient-CHW communication, including patient reminders for self-care activities and other forms of support. These intervention enhancements, in addition to the study comparing patients who do not receive pharmacist or CHW support, may further the understanding of this unique model of diabetes care.
In conclusion, no significant differences were found between a clinical pharmacist-CHW team and clinical pharmacist alone in improving glycemic control in this sample of low-income African-American and Hispanic/Latino patients with uncontrolled diabetes. The magnitude of HbA1c change may be considered clinically meaningful at the end of the study period. Collaboration between pharmacists and CHWs did result in greater intensification of lipid-lowering medication (but without effect on LDL). There was differential patient engagement with the pharmacists and CHWs suggesting that future research should explore which patients most benefit from such services.
Acknowledgments
Funding: This project was supported by grants from the National Center for Research Resources and the National Institute of Diabetes and Digestive and Kidney Diseases. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Center for Research Resources, the National Center for Advancing Translational Sciences, or the National Institutes of Health. Trial registration NCT01498159. The funding sources had no role in study design, conduct, analysis, or decision to submit findings for publication.
We wish to acknowledge the following individuals who substantially contributed to study procedures: Linda Schiffer, Lauren Rapacki, Aida Rodriguez, Sylvia Morales, Monique Walker, ZsaZsa Brown, Vairneke Westmoreland, Enrique Rojas, Shikhi Bansari, Samina Syed, and Oksana Pugach. In addition, the authors express appreciation for all of the study participants.
References
- 1.Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington (DC): National Academies Press (US); 2003. Institute of Medicine (US) Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health Care. [PubMed] [Google Scholar]
- 2.Harris MI. Racial and ethnic differences in health care access and health outcomes for adults with type 2 diabetes. Diabetes Care. 2001;3:454–9. doi: 10.2337/diacare.24.3.454. [DOI] [PubMed] [Google Scholar]
- 3.Seidu S, Walker NS, Bodicoat DH, Davies MJ, Khunti K. A systematic review of interventions targeting primary care or community based professionals on cardio-metabolic risk factor control in people with diabetes. Diabetes Research and Clinical Practice. 2016:1–13. doi: 10.1016/j.diabres.2016.01.022. [DOI] [PubMed] [Google Scholar]
- 4.Fazel MT, Bagalagel A, Lee JK, Martin JR, Slack MK. Impact of Diabetes Care by Pharmacists as Part of Health Care Team in Ambulatory Settings: A Systematic Review and Meta-analysis. The Annals of Pharmacotherapy. 2017;10:890–907. doi: 10.1177/1060028017711454. [DOI] [PubMed] [Google Scholar]
- 5.Bojadzievski T, Gabbay RA. Patient-centered medical home and diabetes. Diabetes Care. 2011;4:1047–53. doi: 10.2337/dc10-1671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smith M, Bates DW, Bodenheimer T, Cleary PD. Why pharmacists belong in the medical home. Health Affairs (Project Hope) 2010;5:906–13. doi: 10.1377/hlthaff.2010.0209. [DOI] [PubMed] [Google Scholar]
- 7.Choe HM, Mitrovich S, Dubay D, Hayward RA, Krein SL, Vijan S. Proactive case management of high-risk patients with type 2 diabetes mellitus by a clinical pharmacist: a randomized controlled trial. The American Journal of Managed Care. 2005;4:253–60. [PubMed] [Google Scholar]
- 8.Wubben DP, Vivian EM. Effects of pharmacist outpatient interventions on adults with diabetes mellitus: a systematic review. Pharmacotherapy. 2008;4:421–36. doi: 10.1592/phco.28.4.421. [DOI] [PubMed] [Google Scholar]
- 9.Greer N, Bolduc J, Geurkink E, et al. Pharmacist-led Chronic Disease Management: A Systematic Review of Effectiveness and Harms Compared With Usual Care. Annals of Internal Medicine. 2016;1:30. doi: 10.7326/M15-3058. [DOI] [PubMed] [Google Scholar]
- 10.Kane EP, Collinsworth AW, Schmidt KL, et al. Improving diabetes care and outcomes with community health workers. Family Practice. 2016;5:523–8. doi: 10.1093/fampra/cmw055. [DOI] [PubMed] [Google Scholar]
- 11.Shah M, Kaselitz E, Heisler M. The role of community health workers in diabetes: update on current literature. Current Diabetes Reports. 2013;2:163–71. doi: 10.1007/s11892-012-0359-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Aponte J, Jackson TD, Wyka K, Ikechi C. Health effectiveness of community health workers as a diabetes self-management intervention. Diabetes & Vascular Disease Research. 2017;4:316–26. doi: 10.1177/1479164117696229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Carrasquillo O, Lebron C, Alonzo Y, Li H, Chang A, Kenya S. Effect of a Community Health Worker Intervention Among Latinos With Poorly Controlled Type 2 Diabetes: The Miami Healthy Heart Initiative Randomized Clinical Trial. JAMA Internal Medicine. 2017;7:948–54. doi: 10.1001/jamainternmed.2017.0926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Spencer MS, Rosland AM, Kieffer EC, et al. Effectiveness of a community health worker intervention among African American and Latino adults with type 2 diabetes: a randomized controlled trial. American Journal of Public Health. 2011;12:2253–60. doi: 10.2105/AJPH.2010.300106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gerber BS, Cano AI, Caceres ML, et al. A pharmacist and health promoter team to improve medication adherence among Latinos with diabetes. The Annals of Pharmacotherapy. 2010;1:70–9. doi: 10.1345/aph.1M389. [DOI] [PubMed] [Google Scholar]
- 16.Gerber BS, Rapacki L, Castillo A, et al. Design of a trial to evaluate the impact of clinical pharmacists and community health promoters working with African-Americans and Latinos with diabetes. Bio Med Central Public Health. 2012;1:891. doi: 10.1186/1471-2458-12-891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Inzucchi SE, Bergenstal RM, Buse JB, et al. Management of hyperglycemia in type 2 diabetes: a patient-centered approach: position statement of the American Diabetes Association (ADA) and the European Association for the Study of Diabetes (EASD) Diabetes Care. 2012;6:1364–79. doi: 10.2337/dc12-0413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Chobanian AV, Bakris GL, Black HR, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension (Dallas, Tex: 1979) 2003;6:1206–52. doi: 10.1161/01.HYP.0000107251.49515.c2. [DOI] [PubMed] [Google Scholar]
- 19.Castillo A, Giachello A, Bates R, et al. Community-based Diabetes Education for Latinos: The Diabetes Empowerment Education Program. The Diabetes Educator. 2010;4:586–94. doi: 10.1177/0145721710371524. [DOI] [PubMed] [Google Scholar]
- 20.Ghorob A, Vivas MM, De Vore D, et al. The effectiveness of peer health coaching in improving glycemic control among low-income patients with diabetes: protocol for a randomized controlled trial. BMC Public Health. 2011;1:208. doi: 10.1186/1471-2458-11-208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Fisher L, Glasgow RE, Mullan JT, Skaff MM, Polonsky WH. Development of a brief diabetes distress screening instrument. Annals of Family Medicine. 2008;3:246–52. doi: 10.1370/afm.842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Tang TS, Brown MB, Funnell MM, Anderson RM. Social support, quality of life, and self-care behaviors amongAfrican Americans with type 2 diabetes. The Diabetes Educator. 2008;2:266–76. doi: 10.1177/0145721708315680. [DOI] [PubMed] [Google Scholar]
- 23.Chew LD, Bradley KA, Boyko EJ. Brief questions to identify patients with inadequate health literacy. Family Medicine. 2004;8:588–94. [PubMed] [Google Scholar]
- 24.Rothman RL, Malone R, Bryant B, et al. The Spoken Knowledge in Low Literacy in Diabetes scale: a diabetes knowledge scale for vulnerable patients. The Diabetes Educator. 2005;2:215–24. doi: 10.1177/0145721705275002. [DOI] [PubMed] [Google Scholar]
- 25.Lowe B, Kroenke K, Grafe K. Detecting and monitoring depression with a two-item questionnaire (PHQ-2) Journal of Psychosomatic Research. 2005;2:163–71. doi: 10.1016/j.jpsychores.2004.09.006. [DOI] [PubMed] [Google Scholar]
- 26.Krause NM, Jay GM. What do global self-rated health items measure? Medical Care. 1994;9:930–42. doi: 10.1097/00005650-199409000-00004. [DOI] [PubMed] [Google Scholar]
- 27.Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;7258:405–12. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Sherwani SI, Khan HA, Ekhzaimy A, Masood A, Sakharkar MK. Significance of HbA1c Test in Diagnosis and Prognosis of Diabetic Patients. Biomarker Insights. 2016:95–104. doi: 10.4137/BMI.S38440. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Little RR, Rohlfing CL, Sacks DB. Status of hemoglobin A1c measurement and goals for improvement: from chaos to order for improving diabetes care. Clinical Chemistry. 2011;2:205–14. doi: 10.1373/clinchem.2010.148841. [DOI] [PubMed] [Google Scholar]
- 30.Xavier D, Gupta R, Kamath D, et al. Community health worker-based intervention for adherence to drugs and lifestyle change after acute coronary syndrome: a multicentre, open, randomised controlled trial. The Lancet Diabetes & Endocrinology. 2016;3:244–53. doi: 10.1016/S2213-8587(15)00480-5. [DOI] [PubMed] [Google Scholar]
- 31.Rothman RL, DeWalt DA, Malone R, et al. Influence of patient literacy on the effectiveness of a primary care-based diabetes disease management program. JAMA. 2004;14:1711–6. doi: 10.1001/jama.292.14.1711. [DOI] [PubMed] [Google Scholar]
- 32.White RO, Chakkalakal RJ, Presley CA, et al. Perceptions of Provider Communication Among Vulnerable Patients With Diabetes: Influences of Medical Mistrust and Health Literacy. Journal of Health Communication. 2016;(sup2):127–34. doi: 10.1080/10810730.2016.1207116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Fernandez A, Schillinger D, Warton EM, et al. Language barriers, physician-patient language concordance, and glycemic control among insured Latinos with diabetes: the Diabetes Study of Northern California (DISTANCE) Journal of General Internal Medicine. 2011;2:170–6. doi: 10.1007/s11606-010-1507-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gerber BS, Brodsky IG, Lawless KA, et al. Implementation and evaluation of a low-literacy diabetes education computer multimedia application. Diabetes Care. 2005;7:1574–80. doi: 10.2337/diacare.28.7.1574. [DOI] [PubMed] [Google Scholar]
- 35.Rochon J. Application of GEE procedures for sample size calculations in repeated measures experiments. Statistics in Medicine. 1998;14:1643–58. doi: 10.1002/(sici)1097-0258(19980730)17:14<1643::aid-sim869>3.0.co;2-3. [DOI] [PubMed] [Google Scholar]
- 36.Lavori PW, Dawson R, Shera D. A multiple imputation strategy for clinical trials with truncation of patient data. Statistics in Medicine. 1995;17:1913–25. doi: 10.1002/sim.4780141707. [DOI] [PubMed] [Google Scholar]
- 37.Syed ST, Gerber BS, Sharp LK. Traveling towards disease: transportation barriers to health care access. Journal of Community Health. 2013;5:976–93. doi: 10.1007/s10900-013-9681-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bland J, Altman D. Regression towards the mean. BMJ: British Medical Journal. 1994;6942:1499. doi: 10.1136/bmj.308.6942.1499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rojas E, Gerber BS, Tilton J, Rapacki L, Sharp LK. Pharmacists’ perspectives on collaborating with community health workers in diabetes care. Journal of the American Pharmacists Association : JAPhA. 2015;4:429–33. doi: 10.1331/JAPhA.2015.14123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Bonevski B, Randell M, Paul C, et al. Reaching the hard-to-reach: a systematic review of strategies for improving health and medical research with socially disadvantaged groups. BMC Medical Research Methodology. 2014:42. doi: 10.1186/1471-2288-14-42. [DOI] [PMC free article] [PubMed] [Google Scholar]