Abstract
A 78-year-old man with a history of benign prostatic hyperplasia presented with double vision, facial pain, altered taste and headache for 7 weeks. Neurological exam was notable for palsies of the right V, VI, VII and XII cranial nerves. An expansive clival mass and multiple lesions in the vertebra were found on MRI. Radionuclide studies showed extensive tumour burden in his liver and peritoneum. His serologies showed normal carcinoembryonic antigen and carbohydrate antigen 19-9 levels and modestly elevated prostate-specific antigen, which was a red herring. Biopsy of his omentum was consistent with metastatic adenocarcinoma with immunostaining indicating an upper gastrointestinal primary tumour. The patient underwent several cycles of radiation therapy, but ultimately elected to pursue hospice care. This case demonstrates the presentation of multiple cranial neuropathies from a clival mass and an unusual primary source from an upper gastrointestinal tumour.
Keywords: cranial nerves, neurooncology
Background
The clivus is a bony structure of the skull base located at the junction of the occipital and sphenoid bones and is in close proximity to the long course of the abducens nerve. The typical presentation of a clival lesion is double vision from an abducens nerve palsy.1 Clival tumours are exceedingly rare, and the most common primary tumours, chordomas and chondrosarcomas, each comprise only 0.1%–0.2% of all intracranial tumours.2–4 Metastatic tumours to the clivus are even rarer with prostate (26.4%), thyroid (11.7%) and hepatocellular (11.7%) being the most common primary malignancies.1 Upper gastrointestinal tumours metastasising to the clivus are reported in only five cases.5 This case illustrates the neurological manifestations associated with clival mass lesions and serves as a rare case of a clival metastasis from an upper gastrointestinal tumour.
Case presentation
A 78-year-old man with a history of benign prostatic hyperplasia presented with double vision for 7 weeks. Additional symptoms included right facial pain, altered taste sensation and headaches worse when lying flat. General physical examination revealed lower abdominal lymphadenopathy. On neurological examination, he had reduced abduction of the right eye with horizontal diplopia on rightward gaze, numbness within the right mouth, decreased taste sensation in the right anterior tongue and rightward protrusion of the tongue, indicating palsies of the right V, VI, VII and XII cranial nerves.
Investigations
A clival mass involving the right petrous apex, occipital condyle, Dorello’s canal, hypoglossal canal and Meckel’s cave was discovered on brain MRI (see figure 1). Multiple vertebral bodies and the iliac on spine imaging also had destructive lesions. Positron emission tomography and CT showed extensive fludeoxyglucose-avid tumour burden involving the liver, bones, peritoneum and abdominal lymph nodes consistent with a cholangiocarcinoma (see figure 2). Pertinent serological studies included normal carcinoembryonic antigen and carbohydrate antigen 19-9 levels and an elevated prostate-specific antigen (PSA) level of 18.8 ng/mL (ref 0.0–4.0).
Figure 1.
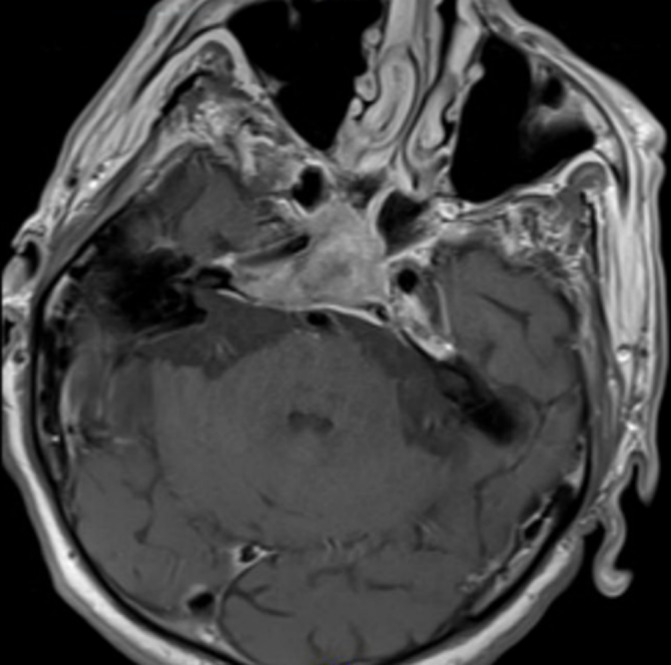
Brain MRI showing a destructive and expansive mass of the clivus.
Figure 2.
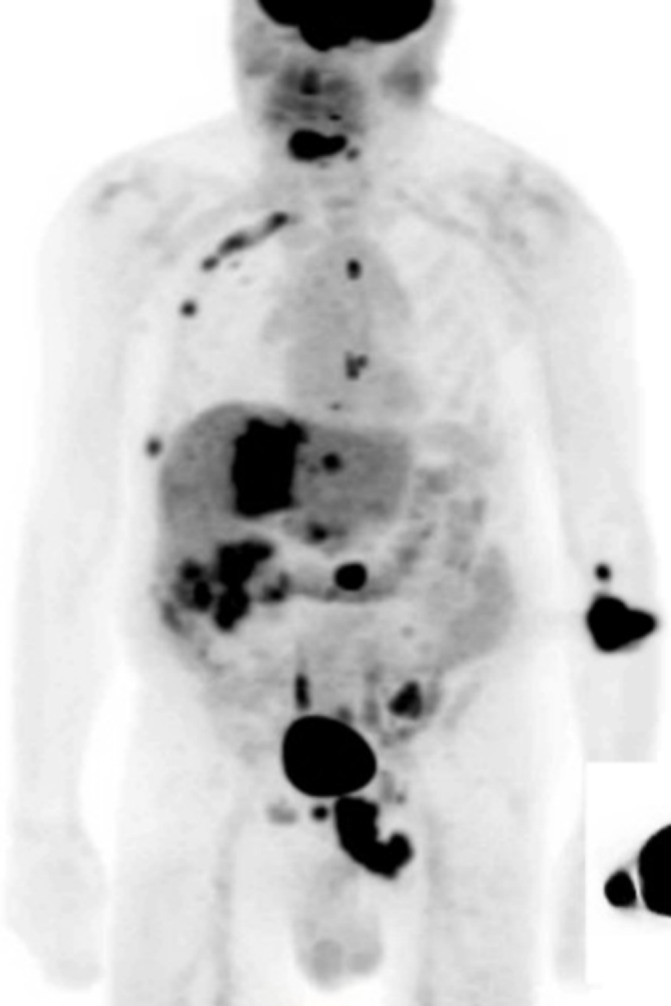
Positron emission tomography and CT showing extensive, fludeoxyglucose-avid signal involving the liver, bones, peritoneum and upper abdominal lymph nodes, consistent with a metastatic gastrointestinal malignancy.
Biopsy of an omental mass showed metastatic adenocarcinoma, compatible with a pancreaticobiliary or upper gastrointestinal primary tumour. Prostate or lung origins were not favoured due to absence of typical immunoreactivity patterns
Outcome and follow-up
The patient was diagnosed with an upper gastrointestinal adenocarcinoma with metastases to the abdomen, peritoneum and bone, particularly the clivus. He was initially treated with radiation therapy to the skull base and cervical spine, but this was stopped when the patient elected to pursue hospice care.
Discussion
This patient developed multiple cranial neuropathies as a result of nerve compression from a clival mass lesion. Most prominent was his diplopia, which was caused by a right cranial nerve VI palsy, a common cranial nerve finding in patients with clival tumours (seen in over 40% of cases).5 Initially, prostate cancer was suspected to be the primary source, as it is the most common cause of clival metastases and the patient’s PSA was modestly elevated.1 5 However, both radiological and histopathological studies were most consistent with gastrointestinal adenocarcinoma.
There have been five reported cases of upper gastrointestinal malignancies with clival metastasis, including three cases of gastric carcinoma,6–8 one gastrointestinal stromal tumour9 and one duodenal adenocarcinoma.5 Of these five cases, only two were new diagnoses of primary malignancies.8 9 This case highlights the importance of considering clival pathology as the cause of an abducens palsy or multiple cranial neuropathies. It is also an example of the rare manifestation of upper gastrointestinal adenocarcinoma metastasising to the clivus and highlights the need to consider this aetiology when a clival metastasis of an unknown primary malignancy is suspected.
Learning points.
Clival tumours are rare and can present as multiple cranial neuropathies, typically with involvement of the abducens nerve and resultant double vision.
The most commonly reported primary malignancies resulting in clival metastases are prostate cancer, followed by thyroid and hepatocellular malignancies.
Clival metastases can also rarely result from primary upper gastrointestinal adenocarcinomas, and these malignancies should be considered in cases of an unknown primary tumour and especially when accompanied by consistent abdominal imaging.
Footnotes
Contributors: CL, JMT and AD: conception, analysis and interpretation of data. CL: drafting the article. JMT and AD: revising it critically for important intellectual content. CL, JMT and AD: final approval of the version to be published. All authors read and approved the final manuscript.
Competing interests: None declared.
Patient consent: Obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Pallini R, Sabatino G, Doglietto F, et al. Clivus metastases: report of seven patients and literature review. Acta Neurochir 2009;151:291–6. 10.1007/s00701-009-0229-1 [DOI] [PubMed] [Google Scholar]
- 2.Deconde AS, Sanaiha Y, Suh JD, et al. Metastatic disease to the clivus mimicking clival chordomas. J Neurol Surg B Skull Base 2013;74:292–9. 10.1055/s-0033-1348027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Korten AG, ter Berg HJ, Spincemaille GH, et al. Intracranial chondrosarcoma: review of the literature and report of 15 cases. J Neurol Neurosurg Psychiatry 1998;65:88–92. 10.1136/jnnp.65.1.88 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sen C, Triana A. Cranial chordomas: results of radical excision. Neurosurg Focus 2001;10:1–7. 10.3171/foc.2001.10.3.4 [DOI] [PubMed] [Google Scholar]
- 5.Dekker SE, Wasman J, Yoo KK, et al. Clival metastasis of a duodenal adenocarcinoma: a case report and literature review. World Neurosurg 2017;100:62–8. 10.1016/j.wneu.2016.12.078 [DOI] [PubMed] [Google Scholar]
- 6.Hirai O, Kikuchi H, Hashimoto N. Skull base metastasis from gastric cancer--case report. Neurol Med Chir 1992;32:908–10. 10.2176/nmc.32.908 [DOI] [PubMed] [Google Scholar]
- 7.Fukushima M, Katayama Y, Shigemori Y, et al. Clivus metastasis from gastric signet ring cell carcinoma after a 10-year disease-free interval--case report. Neurol Med Chir 2012;52:751–3. 10.2176/nmc.52.751 [DOI] [PubMed] [Google Scholar]
- 8.Harada S, Toya S, Iisaka Y, et al. [Basal skull metastasis of stomach cancer presenting with Garcin’s syndrome--a case report]. No Shinkei Geka 1987;15:765–9. [PubMed] [Google Scholar]
- 9.Baeg MK, Bae SH, Lee KH, et al. Diplopia as a presenting symptom in a gastric gastrointestinal stromal tumor. Jpn J Clin Oncol 2011;41:265–8. 10.1093/jjco/hyq176 [DOI] [PubMed] [Google Scholar]


