Summary
Introduction.
Epidemiological studies are a key element in determining the evolution and spread of HIV infection among the world population. Knowledge of the epidemiological dynamics improves strategies for prevention and monitoring.
Methods.
We examined 2,272 subjects who voluntarily underwent HIV testing from January 1992 to December 2015. For each subject, an anonymous form was completed to obtain information on personal data, sexual habits and exposure to risk factors.
Results.
The number of subjects undergoing the screening test has increased over the years and the average age of the tested subjects has decreased over time. The main motivation for undergoing HIV testing is unprotected sex. Although heterosexual subjects taking the test were more numerous than homosexuals in this study, an increase in the latter over time should be highlighted.
Conclusions.
Although the number of tests performed has increased over the years, the persistence of unprotected sex shows an inadequate perception of risk. Therefore, it is necessary to implement programmes to increase the general awareness of HIV infection. It is also essential to undertake constant monitoring of behaviour, risk perception and the application of the screening test via surveillance systems in order to implement effective and efficient prevention.
Key words: HIV infection epidemiology, Unprotected sex, HIV testing, Risk behaviours, Prevention strategies
Introduction
Epidemiological HIV data are the most important element showing the evolution and diffusion of HIV infection among the world population. Moreover, epidemiological studies allow the planning of specific prevention strategies monitoring the spread of this infection [1-4]. The AIDS surveillance systems provide useful information on HIV epidemic dynamics [5-7]. For this reason, since 1988 several Italian provinces and regions (Lazio, Veneto, Friuli Venezia-Giulia, Trento, Modena, Sicilia) have established local surveillance systems for new HIV diagnoses [8, 9]. AIDS surveillance has three complementary objectives in HIV-infected individuals: (1) reducing high-risk sexual behaviours [10-13]; (2) reducing the use of injected and non-injected drugs [10, 14]; (3) improving clinical care [15]. The last objective aims to attain adherence to antiretroviral therapy, the suppression of HIV viral load and the prevention of the development of HIV drug resistance [15, 16]. At the Epidemiological Observatory, the Regional Registry (activated in Sicily in 1985) collects all cases of AIDS occurring among Sicilian residents or diagnosed in Sicily. The register is part of the National Register, which is maintained by the National Institute of Health and it collects all cases of AIDS occurring or diagnosed in all Italian regions. However, the monitoring of new cases of HIV infection has always been difficult to implement due to the significant problems related to privacy. Subsequently, following the issue of the Ministerial decree of 2008.03.31, a national surveillance system of HIV infection was established which included the notification of new cases; this system is similar to that used for cases of AIDS. For this purpose, the regional representatives of the Infectious Diseases Units have been specially appointed and a regional surveillance system has been implemented since 2010. In addition, since 2009 our laboratory has adhered to the system of regional surveillance, although it was already in place in the province of Messina from 1984. This system offers the screening test to all people who voluntarily request it after engaging in risk behaviours. Therefore, our study is a surveillance survey of the number of subjects who underwent a voluntary HIV test in the city and province of Messina from January 1992 to December 2015, monitoring in the territory risk behaviour, risk perception, HIV infection and the application of the screening test via surveillance systems in order to implement effective and efficient prevention.
Methods
Overall, 2,272 people, 1,554 males and 718 females, voluntarily underwent HIV testing from January 1992 to December 2015 at the HIV laboratory of the Policlinic G. Martino in Messina, which is one of the reference centres for monitoring HIV infection in Sicily. Messina lies on the north-eastern tip of Sicily and it has around 240,000 inhabitants. Before blood sample collection, the volunteers underwent counselling to ascertain the need for the test considering the risk factor and if the time between exposure and the test was sufficient to detect the presence of antibodies. During counselling, we collected information about gender, age, place of birth, occupation and sexual habits (heterosexual, homosexual or bisexual). We also asked about the motivation for coming and the kinds of risk to which the subjects may have been exposed recently, such as blood transfusion, dental visits, accidental punctures, drugs and/or alcohol use, piercing and/or tattoos and unprotected sex.
Comparisons and correlations were determined using the standard Pearson test and linear regression. Significance was assessed at the p < 0.05 level. All analyses were performed using the Prism 4.0 software.
Results
Table I shows information about gender, age, sexual habits, occupation and exposure to risk factors.
Tab. I.
Overview on subjects who voluntarily underwent HIV testing from January 1992 to December 2015.
| 1992 | 1993 | 1994 | 1995 | 1996 | 1997 | 1998 | 1999 | 2000 | 2001 | 2002 | 2003 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N° test | 8 | 14 | 37 | 29 | 10 | 5 | 25 | 122 | 100 | 82 | 53 | 105 |
| Male Female | 6 | 6 | 28 | 17 | 4 | 4 | 18 | 70 | 63 | 49 | 30 | 63 |
| 2 | 8 | 9 | 12 | 6 | 1 | 7 | 52 | 37 | 33 | 23 | 42 | |
| Mean age | 48 | 50 | 46 | 47 | 44 | 52 | 46 | 43 | 42 | 42 | 42 | 43 |
| Occupation | ||||||||||||
| Student | 3 | 7 | 15 | 11 | 7 | 1 | 11 | 51 | 51 | 35 | 25 | 49 |
| Employee | 0 | 2 | 7 | 3 | 1 | 0 | 4 | 23 | 17 | 18 | 5 | 18 |
| Freelancer | 0 | 1 | 0 | 4 | 0 | 0 | 3 | 2 | 2 | 3 | 2 | 6 |
| Workman | 0 | 0 | 0 | 4 | 0 | 1 | 3 | 7 | 3 | 5 | 2 | 5 |
| Housewife | 0 | 1 | 1 | 2 | 0 | 0 | 0 | 4 | 6 | 2 | 2 | 3 |
| Physician* | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 12 | 5 | 5 | 5 | 13 |
| Dealer | 2 | 1 | 4 | 2 | 0 | 1 | 2 | 6 | 7 | 2 | 0 | 2 |
| Police,army | 2 | 0 | 4 | 0 | 0 | 0 | 0 | 2 | 1 | 3 | 3 | 2 |
| Retired | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 1 | 1 | 1 | 0 | 0 |
| Prostitute | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 0 |
| Unemployed | 1 | 1 | 4 | 1 | 2 | 0 | 0 | 14 | 6 | 7 | 8 | 6 |
| Sexual habits | ||||||||||||
| Heterosexual | 7 | 13 | 33 | 29 | 10 | 4 | 21 | 104 | 85 | 69 | 44 | 96 |
| Homosexual | 1 | 0 | 2 | 0 | 0 | 1 | 3 | 5 | 7 | 3 | 3 | 3 |
| Bisexual | 0 | 0 | 1 | 0 | 0 | 0 | 1 | 4 | 1 | 3 | 1 | 6 |
| Transsexual | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Unresponsive | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 9 | 7 | 7 | 5 | 0 |
| Risk factor | ||||||||||||
| No risk reported | 0 | 0 | 1 | 1 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 |
| Unprotected sex | 6 | 9 | 22 | 18 | 5 | 4 | 20 | 85 | 64 | 46 | 28 | 71 |
| Prevention/control | 0 | 1 | 10 | 6 | 1 | 1 | 1 | 16 | 8 | 8 | 2 | 13 |
| Accidental injury | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 13 | 14 | 21 | 12 | 15 |
| Invasive practices$ | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 4 | 0 | 1 | 0 |
| Drug addicts/ partner drug addicts | 1 | 2 | 4 | 2 | 2 | 0 | 1 | 2 | 5 | 4 | 7 | 0 |
| Partners of HIV+ subjects | 0 | 1 | 0 | 1 | 0 | 0 | 1 | 4 | 4 | 2 | 3 | 5 |
| Transfused or dialysis patients | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Suspected diagnosis | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 2004 | 2005 | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N° test | 99 | 90 | 218 | 143 | 89 | 83 | 84 | 193 | 83 | 147 | 208 | 245 |
| Male Female | 69 | 62 | 144 | 96 | 65 | 63 | 60 | 124 | 55 | 97 | 164 | 197 |
| 30 | 28 | 74 | 47 | 24 | 20 | 24 | 69 | 28 | 50 | 44 | 48 | |
| Mean age | 41 | 41 | 38 | 36 | 36 | 40 | 34 | 31 | 35 | 32 | 33 | 32 |
| Occupation | ||||||||||||
| Student | 28 | 25 | 79 | 63 | 38 | 20 | 36 | 96 | 25 | 60 | 55 | 73 |
| Employee | 15 | 20 | 49 | 24 | 13 | 18 | 11 | 23 | 11 | 21 | 26 | 47 |
| Freelancer | 3 | 9 | 22 | 13 | 10 | 6 | 8 | 14 | 8 | 15 | 23 | 18 |
| Workman | 5 | 5 | 6 | 8 | 8 | 5 | 6 | 13 | 3 | 8 | 18 | 17 |
| Housewife | 2 | 2 | 1 | 0 | 2 | 3 | 5 | 4 | 2 | 2 | 5 | 2 |
| Physician* | 13 | 8 | 13 | 7 | 3 | 10 | 6 | 9 | 2 | 8 | 9 | 17 |
| Dealer | 3 | 0 | 10 | 8 | 2 | 2 | 4 | 1 | 2 | 4 | 6 | 2 |
| Police,army | 5 | 2 | 0 | 1 | 0 | 5 | 1 | 5 | 1 | 1 | 4 | 7 |
| Retired | 1 | 3 | 7 | 1 | 2 | 2 | 1 | 0 | 4 | 4 | 5 | 4 |
| Prostitute | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Unemployed | 23 | 16 | 30 | 17 | 10 | 11 | 4 | 28 | 24 | 23 | 56 | 58 |
| Sexual habits | ||||||||||||
| Heterosexual | 71 | 67 | 191 | 111 | 54 | 72 | 57 | 155 | 56 | 117 | 134 | 128 |
| Homosexual | 15 | 15 | 13 | 23 | 24 | 10 | 20 | 17 | 23 | 20 | 57 | 75 |
| Bisexual | 10 | 6 | 9 | 7 | 4 | 1 | 4 | 7 | 2 | 10 | 5 | 25 |
| Transsexual | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| Unresponsive | 3 | 2 | 5 | 2 | 7 | 0 | 3 | 14 | 2 | 0 | 12 | 17 |
| Risk factor | ||||||||||||
| No risk reported | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 6 | 1 | 0 | 2 | 5 |
| Unprotected sex | 68 | 64 | 144 | 115 | 76 | 68 | 69 | 127 | 68 | 106 | 158 | 186 |
| Prevention/control | 7 | 5 | 58 | 11 | 5 | 4 | 6 | 31 | 4 | 19 | 25 | 14 |
| Accidental injury | 17 | 12 | 13 | 14 | 8 | 9 | 6 | 4 | 10 | 11 | 9 | 10 |
| Invasive practices$ | 0 | 0 | 0 | 1 | 0 | 2 | 2 | 25 | 0 | 2 | 1 | 3 |
| Drug addicts/ partner drug addicts | 0 | 0 | 3 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 9 | 1 |
| Partners of HIV+ subjects | 7 | 8 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 4 | 0 | 14 |
| Transfused or dialysis patients | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 |
| Suspected diagnosis | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 3 | 4 | 11 |
physician, paramedic, dentist
surgery, dental care, tattoo, piercing
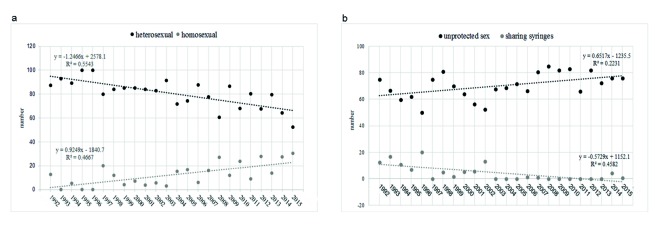
The analysis of the data collected from 1992 to 2015 clearly showed a statistically significant increase (p < 0.0001) in the number of HIV tests performed. The number of subjects undergoing the screening test has increased from 8 to 245 persons/year (Fig. 1).
Fig. 1.
Number of 2 screened for HIV from 1992 to 2015.
The data analysed by gender shows a predominance of male subjects who carried out the test (1,554 males vs. 718 females). As confirmed by the regression analysis, from 1992 to 2015, the mean age of the tested subjects steadily decreased from 48 to 32 (p < 0.0001) (Fig. 2).
Fig. 2.
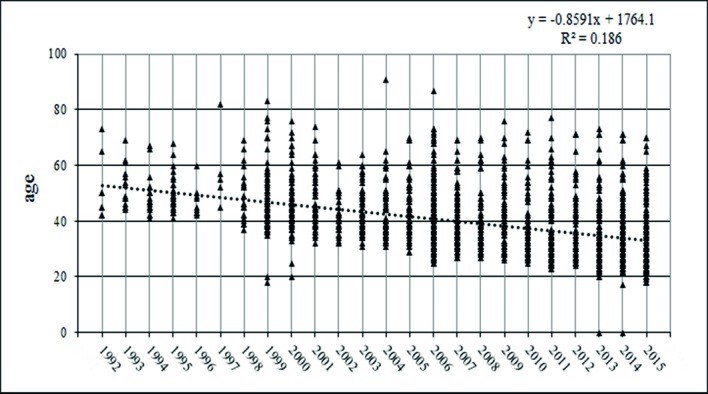
Regression analysis shows the distribution of subjects undergoing screening for HIV by age in the period 1992-2015.
Analysing the sample according to profession, most of the subjects in the study were students (38.13%), followed by employees (16.54%) and unemployed (15.52%). These categories were prevalent in all the years examined in this study. All categories were uniformly represented over the years under investigation, with the exception of the category "unemployed" and "retired" significantly more present in recent years (p = 0.0078 and p=0.0046 respectively), in contrast to the "dealer" category, most represented in the 1990s (p = 0.0076).
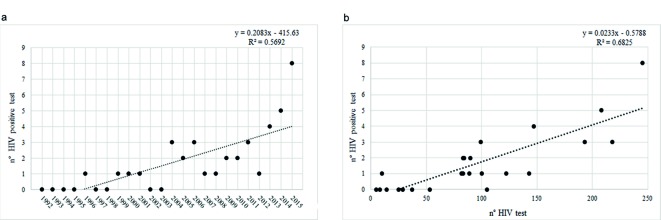
The information collected on sexual habits showed that, on average, 76.06% of the sample comprised heterosexual subjects, 14.96% homosexual subjects and 4.71% bisexual subjects. The statistical analysis showed a significant inverse correlation (p < 0.0001) between the number of heterosexual and homosexual subjects; in particular, the former decreased while the latter increased over the years (Fig. 3a).
Fig. 3.
Comparison between heterosexuals and homosexuals categories, (a) and the most involved risk factors (b).
The most common reason prompting the subjects to carry out the test was unprotected sex (71.17%). In addition, 9.95% of people were persuaded to take the test for prevention and 10.03% due to contact with potentially contaminated objects. The category of drug users, on average, accounted for 4.36% of the subjects examined. The comparison between the two risk factors most implicated – unprotected sex and the exchange of syringes among drug users – showed that the former increased significantly from 1992 to 2015, while the latter declined significantly over the years (Fig. 3b).
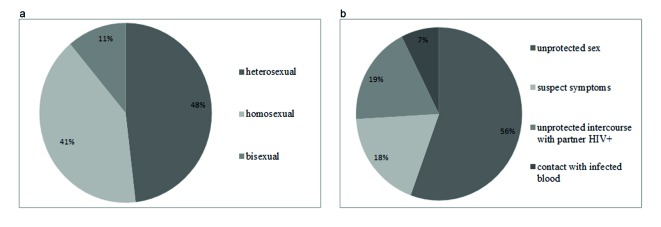
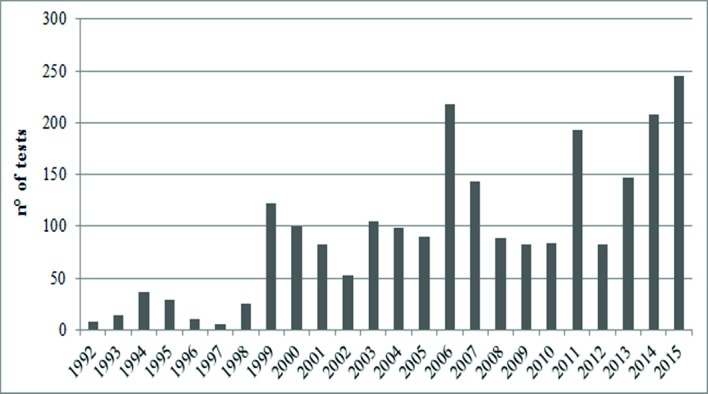
In all, 35 of 1,554 tested males (2.25%) were HIV positive and their average age was 35 ± 11.73. Only 4 female subjects out of 718 were HIV positive (0.5 %); they were on average 45 ± 11.21 years old. As shown in Figure 4a, the number of positive HIV tests increased over the years, especially from 2013 onwards, reaching 5.7 new cases of HIV infection per 100,000 residents in 2015. Furthermore, the number of positive HIV tests increases significantly with an increase in the number of tests performed (Fig.4b). Of the subjects who were positive on the test, 48% were heterosexual, 41% were homosexual and 11% were bisexual. Analysing the reasons that led the subjects to carry out the test, it was found that 56% of them did so because of occasional unprotected sex, 19% because of sexual contact with an HIV-positive partner, 18% because of apparent symptoms related to HIV and only 7% due to being drug users (Fig. 5a-b).
Fig. 4.
The scatterplots show the results of regression analysis to assess the increase in the number of tests during the years examined (a) and the relationship with the number of HIV tests performed in the same period (b) (1992–2015).
Fig. 5.
Sexual habits (a) and main cause of transmission (b) of the subjects who tested HIV positive.
Discussion
Our study is an observational survey that drew on epidemiological surveillance carried out in our laboratory from 1992 to 2015 among subjects who underwent a voluntary test. The Joint United Nations Programme on HIV/AIDS (UNAIDS)/World Health Organization (WHO) has defined second generation surveillance (SGS) [17, 18] as the "regular, systematic collection, analysis and interpretation of information for use in tracking and describing changes in the HIV/AIDS epidemic over time". This kind of surveillance provides an understanding of local epidemics, including sources of new infections over time, as well as the behavioural and biological factors driving epidemic spread. Most new transmission is still attributed to those with higher risk behaviours and their immediate sexual partners. The monitoring of risks related to the transmission of HIV provides a key source of information, not only to understand the drivers of epidemics, but also for advocacy and the planning and evaluation of preventive interventions [19, 20].
From the data described above, the greater presence of males than females could be attributed to the fact that men pay less attention to prevention than women and therefore their behaviours are less cautious. Alternatively, it could reflect a heightened perception of risk among men. The results showed that during the entire period of observation, the average age of the tested subjects consistently decreased, whereas the number of individuals who voluntarily took the test increased over time. This is an unequivocal sign that information has become more effective over the years. During the period observed, we highlight the increase in the number of those undergoing voluntary testing in the years 2006 and 2011. In these years, our laboratory, in collaboration with the Red Cross of Messina, organized prevention campaigns, with information points distributed in the main squares of the city, offering the chance to do an on-site test.
The results obtained show that from 1992 to 2015 individuals who requested testing and those who tested positive were predominantly subjects with at-risk sexual behaviours. Despite the fact that heterosexuals remain the category most represented, our results show that in recent years the number of heterosexuals voluntarily taking the test has decreased, while the number of homosexuals has increased. This can be attributed to greater awareness among the latter of the greater risk of transmission of HIV through anal intercourse [21], or perhaps finding it easier to declare their sexual orientation because the homosexuality taboo is greatly reduced in society. Some associations, particularly active in our city, help us in the field of sexual health and the prevention of HIV and sexually transmitted infections (STIs) to increase the promotion of testing in this group given the increased vulnerability of gay and bisexual men.
Only a few subjects belonged to the category of drug addicts, in contrast to the 1980s in Italy, when they were the predominant category in the spread of the virus [22, 23]. In addition, the prevalence of people who reported that they practised unprotected sex denotes a lack of knowledge of the risk, in particular evidence of inadequate risk perception, condom use and HIV testing, suggesting the need to implement programmes aimed at increasing the general awareness of HIV infection according to the guidelines issued at the European level [24].
Regarding the subjects who tested positive for HIV, our data show a lower incidence of HIV infection in women, in line with the latest data from the AIDS Operating Center (COA) of the National Institute of Health. Unlike women, only the age group of affected men is in line with the national figure, at 39 years for males and 36 for females.
The increase in the number of positive HIV tests could suggest an increase in the incidence of new diagnoses, but this would not be in line with current Italian data. According to the data provided by the COA in 2015, the incidence of new HIV infection diagnoses has decreased slightly from the previous three years, with 3,444 new HIV infection diagnoses equal to 5.7 new cases of HIV infection per 100,000 residents reported. As new diagnoses increase with the number of tests performed, we believe it plausible that the incidence of infection has not increased, but rather the increase in the number of tests has simply led to the discovery of infection that would otherwise be hidden.
Since the mid-1980s, the distribution of new HIV transmission diagnoses has changed dramatically: the proportion of IDUs declined from 76.2% to 3.2% in 2015, while the cases attributable to sexual transmission, in particular those attributable to heterosexual transmission, increased from 1.7% in 1985 to 44.9% in 2015 and cases attributable to homosexual transmission over the same period increased from 6.3% to 40.7%. Our data correlate with this trend, 48% of HIV-positive people were heterosexual and 41% were homosexual. Yet, our data show that the majority of new diagnoses of infection by HIV can be attributed to unprotected sexual intercourse at a rate of 83%, in line with COA data that attributes 85.5% of all cases to unprotected sexual intercourse [25, 26].
Conclusions
Data from the National Institute of Health in Italy (the AIDS Operating Center) show that the distribution of HIV methods of transmission has undergone remarkable changes in recent years. As the major cause of the risk of HIV exposure is represented by unprotected sex, we believe it is essential to promote knowledge about diseases and their complications. Since students are more vulnerable to unprotected sex, it is clear that there is an urgent need to introduce sex education as a proper subject in Italian schools in order to promote the practice of sexual relationships in safe and responsible manner and to enhance awareness of the risk of contracting and transmitting STIs [27].
It is essential to undertake constant monitoring of behaviour and risk perception, as well as the application of the screening test in Italy and other countries via a surveillance system and other methods in order to implement effective and efficient prevention [28, 29].
In agreement with other studies [7, 30], we affirm that the changed pattern of the HIV epidemic in Italy highlights the need for a nation-wide surveillance system for HIV infection, aimed also at the allocation of adequate economic resources and the planning of specific prevention.
Over the last decade, the proportion of late presenters or those with indications of advanced infection has increased, from 20.5% in 2006 to 74.5% in 2015. This means that these individuals are diagnosed only when their immune system is already failing. There is no cure for HIV, but early diagnosis allows access to lifesaving treatment that prolongs healthy life.
The above provides an understanding of the importance of promoting HIV testing. This is important because it allows the emergence of previously hidden non-diagnosed cases of HIV infection; later diagnosis of HIV is worse for the immune system, while timely diagnosis helps manage the infection effectively. Providing antiretroviral therapy in the early stages of HIV infection allows people with HIV to live longer and healthier lives. It also reduces costs for the healthcare system and above all reduces the risk of transmitting HIV to others.
ACKNOWLEDGMENTS
The study was not supported by other entities. The authors declare no conflict of interest.
References
- 1.Kilmarx PH. Global epidemiology of HIV. Curr Opin HIV AIDS. 2009;4:240–246. doi: 10.1097/COH.0b013e32832c06db. [DOI] [PubMed] [Google Scholar]
- 2.Camoni L, Regine V, Stanecki K, Salfa MC, Raimondo M, Suligoi B. Estimates of the number of People Living with HIV in Italy. BioMed Research International. 2014;2014:209619–209619. doi: 10.1155/2014/209619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sumartojo E. Structural factors in HIV prevention: concepts, examples, and implications for research. AIDS. 2000;14:S3–S10. doi: 10.1097/00002030-200006001-00002. [DOI] [PubMed] [Google Scholar]
- 4.Gupta GR, Parkhurst JO, Ogden JA, Aggleton P, Mahal A. Structural approaches to HIV prevention. Lancet. 2008;372:764–775. doi: 10.1016/S0140-6736(08)60887-9. [DOI] [PubMed] [Google Scholar]
- 5.Mammone A, Pezzotti P, Angeletti C, Orchi N, Carboni A, Navarra A, Sciarrone MR, Sias C, Puro V, Guasticchi G, et al. HIV incidence estimate combining HIV/AIDS surveillance, testing history information and HIV test to identify recent infections in Lazio, Italy. BMC Infect Dis. 2012;12:65–65. doi: 10.1186/1471-2334-12-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Goldberg DJ, Emslie JA, Smyth W, Reid D. A system for surveillance of voluntary HIV testing: results of the first 2 years, 1989-1990. AIDS. 1992;6:495–500. [PubMed] [Google Scholar]
- 7.Suligoi B, Rezza G. HIV infection: incidence estimate and surveillance systems. Epidemiol Prev. 2003;27:67–69. [PubMed] [Google Scholar]
- 8.Borghi V, Girardi E, Bellelli S, Angeletti C, Mussini C, Porter K, Roberto Esposito R. Late presenters in an HIV Surveillance System in Italy during the period 1992-2006. J Acquir Immune Defic Syndr. 2008;49:282–286. doi: 10.1097/QAI.0b013e318186eabc. [DOI] [PubMed] [Google Scholar]
- 9.Camoni L, Raimondo M, Regine V, Salfa MC, Suligoi B. Regional representatives of the HIV Surveillance System. Late presenters among persons with a new HIV diagnosis in Italy, 2010-2011. BMC Public Health. 2013;13:281–281. doi: 10.1186/1471-2458-13-281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Wechsberg WM, Golin C, El-Bassel N, Hopkins J, Zule W. Current interventions to reduce sexual risk behaviours and crack cocaine use among HIV-infected individuals. Curr HIV/AIDS Rep. 2012;9:385–393. doi: 10.1007/s11904-012-0131-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yin L, Wang N, Vermund SH, Shefherd BE, Ruan Y, Shao Y, Qian HZ. Sexual risk reduction for HIV-infected persons: a meta-analytic review of "positive prevention" randomized clinical trials. PLoS One. 2014;9:e107652–e107652. doi: 10.1371/journal.pone.0107652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bunnell R, Mermin J, Cock KM. HIV prevention for a threatened continent: implementing positive prevention in Africa. JAMA. 2006;296:855–858. doi: 10.1001/jama.296.7.855. [DOI] [PubMed] [Google Scholar]
- 13.Kennedy CE, Medley AM, Sweat MD, O'Reilly KR. Behavioral interventions for HIV positive prevention in developing countries: a systematic review and meta-analisys. Bull World Health Organ. 2010;88:615–623. doi: 10.2471/BLT.09.068213. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Camoni L, Regine V, Salfa MC, Nicoletti G, Canuzzi P, Magliocchetti N, Rezza G, Suligoi B SerT Study Group, author. Continued high prevalence of HIV, HBV and HCV among injecting and noninjecting drug users in Italy. Ann Ist Super Sanità. 2010;6:59–65. doi: 10.4415/ANN_10_01_08. [DOI] [PubMed] [Google Scholar]
- 15.Handford CD, Tynan AM, Rackal JM, Glazier RH. Setting and organization of care for persons living with HIV/AIDS. Cochrane Database Syst Rev. 2006;3:CD004348–CD004348. doi: 10.1002/14651858.CD004348.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ko NY, Liu HY, Lai YY, Pai YH, Ko WC. Case management interventions for HIV- infected individuals. Curr HIV/AIDS Rep. 2013;10:390–397. doi: 10.1007/s11904-013-0183-7. [DOI] [PubMed] [Google Scholar]
- 17. UNAIDS/WHO-Working Group on Global HIV/AIDS and STI Surveillance , author. Guidelines for second generation HIV surveillance. Geneva: UNAIDS/WHO; 2000. [Google Scholar]
- 18. UNAIDS/WHO Working Group on Global HIV/AIDS and STD Surveillance , author. The pre-surveillance assessment: guidelines for planning serosurveillance of HIV, prevalence of sexually transmitted infections and the behavioural components of second generation surveillance of HIV. Geneva: 2005. [Google Scholar]
- 19.Garnett G, Garcia-Calleja J, Rehle T, Gregson S. Behavioural data as an adjunct to HIV surveillance data. Sex Transm Infect. 2006;82:57–62. doi: 10.1136/sti.2005.016543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.McGarrigle CA, Fenton KA, Gill ON, Hughes G, Morgan D, Evans B. Behavioural surveillance: the value of national coordination. Sex Transm Infect. 2002;78:398–405. doi: 10.1136/sti.78.6.398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kelley CF, Kraft CS, Man TJ, Duphare C, Lee HW, Yang J, Easley KA, Tharp GK, Mulligan MJ, Sullivan PS, et al. The rectal mucosa and condomless receptive anal intercourse in HIV-negative MSM: implications for HIV transmission and prevention. Mucosal Immunol. 2016 doi: 10.1038/mi.2016.97. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Dorrucci M. Epidemiology of HIV. Update. Recenti Prog Med. 2010;101:12–15. [PubMed] [Google Scholar]
- 23.Camoni L, Federico B, Capelli G, Regine V, Salfa MC, Nicoletti G, Canuzzi P, Magliocchetti N, Rezza G, Suligoi B, et al. Few Italian drug users undergo HIV testing. AIDS Behav. 2011;15:711–717. doi: 10.1007/s10461-009-9616-0. [DOI] [PubMed] [Google Scholar]
- 24.Giuliani M, Vescio MF, Latini A, Palamara G, Pimpinelli F, Donà MG, Stivali F, Carduccelli F, Ensoli F, Carlo A, et al. Continous increase in HIV-1 incidence after the year 2000 among men who have sex with men in Rome: insights from a 25-years retrospective cohort study. Euro Surveill. 2014;19:20969–20969. doi: 10.2807/1560-7917.es2014.19.47.20969. [DOI] [PubMed] [Google Scholar]
- 25.Mills S, Saidel T, Magnani R, Brown T. Surveillance and modelling of HIV, STI, and risk behaviours in concentrated HIV epidemics. Sex Transm Infect. 2004;80:ii57–ii62. doi: 10.1136/sti.2004.011916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Suligoi B, Raimondo M, Fanales-Belasio E, Buttò S. The epidemic of HIV infection and AIDS, promotion of testing, and innovative strategies. Ann Ist Super Sanità. 2010;1:15–23. doi: 10.4415/ANN_10_01_03. [DOI] [PubMed] [Google Scholar]
- 27.Visalli G, Picerno I, Vita G, Spataro P, Bertuccio MP. Knowledge of sexually transmitted infections among younger subjects of the city of Messina (Sicily) J Prev Med Hyg. 2014;55:17–22. [PMC free article] [PubMed] [Google Scholar]
- 28.Kalichman SC, Rompa D, Cage M, DiFonzo K, Simpson D, Austin J, Luke W, Buckles J, Kyomugisha F, Benotsch E, et al. Effectiveness of an intervention to reduce HIV transmission risks in HIV-positive people. Am J Prev Med. 2001;21:84–92. doi: 10.1016/s0749-3797(01)00324-5. [DOI] [PubMed] [Google Scholar]
- 29.Wingood GM, DiClemente RJ, Mikhail I, Lang DL, McCree DH, Davies SL, Hardin JW, Hook EW, 3rd, Saag M. A randomized controlled trial to reduce HIV transmission risk behaviours and sexually transmitted diseases among women living with HIV: The WiLLOW Program. J Acquir Immune Defic Syndr. 2004;37:S58–S67. doi: 10.1097/01.qai.0000140603.57478.a9. [DOI] [PubMed] [Google Scholar]
- 30.Mulieri I, Santi F, Colucci A, Fanales-Belasio E, Gallo P, Luzzi AM. Sex workers clients in Italy: results of a phone survey on hiv risk behaviour and perception. Ann Ist Super Sanità. 2014;50:363–368. doi: 10.4415/ANN_14_04_12. [DOI] [PubMed] [Google Scholar]