Abstract
Aim
In Japan, the do not attempt resuscitation (DNAR) order is practised routinely even though no related laws or guidelines exist. This study aimed to clarify the current status of DNAR, reveal existing DNAR‐related issues, and improve the application of DNAR.
Methods
A questionnaire survey of medical institutions in Kanagawa Prefecture (total population, 9,120,000) about the current status of DNAR was carried out.
Results
The results showed that DNAR has been practised at approximately 90% of the hospitals surveyed, but only about 30% have developed in‐hospital DNAR guidelines. Approximately 80% of the hospitals do not involve patients in the decision on their own DNAR orders. Because the DNAR order has not been legislated, it is often unclear whether to resuscitate patients when a request for an ambulance is made for a cardiac arrest at home.
Conclusion
It is necessary for prefectures, municipalities, and local medical control authorities to take the initiative in establishing an ordinance on DNAR orders and developing guidelines.
Keywords: Ambulances, cardiopulmonary arrest, clinical decision‐making, prehospital care, terminal care
Introduction
In Japan, end‐of‐life (EOL) care has been discussed from various perspectives along with medical technological advances, population ageing, and the trend towards nuclear families. In 2007, the Japanese Ministry of Health, Labour and Welfare issued the Guidelines for Decision‐Making on End‐of‐Life Care.1 In 2014, guidelines for EOL care were also published by the Japanese Circulation Society, the Japanese Association for Acute Medicine, and the Japanese Society for Intensive Care Medicine.2 These guidelines (published in Japanese) define “end of life” as a terminal phase of disease when it appears unlikely that the life of the patient will be saved even with appropriate treatment. In addition, the guidelines recommend the medical team to speak with patients nearing the end of life if they are capable of decision‐making, or with family members, and to clearly record whether life‐prolonging treatment is desired or when treatment should be reduced or terminated. However, the guidelines simply provide a general idea about the process, not a clear description of the necessary steps, such as what professionals to involve in the decision‐making process on do not attempt resuscitation (DNAR) orders and what forms to use.
A key issue in EOL care is the DNAR order for withholding resuscitation of a patient having a cardiac arrest. In the USA and Europe, the movement towards the legalization of the DNAR order started to expand in the 1980s, and today, DNAR orders are regulated, for example, by state law. In contrast, the DNAR order is not legislated in Japan. Furthermore, the background to the current situation and the decision‐making process are unclear, suggesting that each hospital issues DNAR orders independently in various clinical settings. In addition, when a patient with a DNAR order has a cardiac arrest at home or at an elderly nursing care facility, the responding paramedics are often confused by the DNAR order but provide cardiopulmonary resuscitation (CPR) anyway because no law or regulations state otherwise.
In this study, to reveal how DNAR orders are managed at hospitals, we carried out a questionnaire survey of all hospitals in Kanagawa Prefecture (Japan) to reveal the current situation surrounding the in‐hospital use of DNAR orders.
Kanagawa Prefecture borders Tokyo Metropolis and has a population of 9,127,323 (as of April 2016), making it the second most populous of Japan's 47 prefectures after Tokyo Metropolis. Kanagawa also ranks sixth amongst Japan's prefectures in terms of the number of hospitals.
Method
A questionnaire survey was mailed to the directors of all 292 hospitals registered by the Kanagawa Prefecture Hospital Association to ask the physicians the following questions concerning DNAR orders. Responses to the questionnaire were received between 15 August and 30 September in 2014. Respondents were given the option of remaining anonymous but were asked to provide their name and position where possible.
-
Please tell us about your hospital. Which of the following best describes your facility?
(a) General hospital (b) Hospital with long‐term care beds
-
Do you implement DNAR orders?
(a) Yes, being practised (b) No, not being practised
-
Do you have the in‐hospital guidelines for the management of DNAR orders?
(a) Yes (b) No
-
Who issues DNAR orders?
(a) Physician in charge (b) Team of physicians led by the physician in charge (c) Physicians and nurses (d) Physicians, nurses, and other professionals (e) A special committee
-
What proportion of patients with a DNAR order was involved in the decision process of their DNAR order?
(a) 0–25% (b) 26–50% (c) 51–75% (d) ≥76%
-
What leading diseases/conditions do patients with DNAR orders have?
Open‐ended response
-
What do you think are the advantages of DNAR orders?
Open‐ended response
-
What do you think are the disadvantages of DNAR orders?
Open‐ended response
-
What actions do you take for DNAR patients undergoing a cardiac arrest at home?
Open‐ended response
-
What instructions do you give to an EMS team who responded to a request to treat a patient undergoing cardiac arrest at home but who had previously issued a DNAR order?
Open‐ended response
Results
After excluding hospitals specialized in obstetrics, pediatrics, and psychiatry, a secondary questionnaire survey of 270 of the 292 hospitals was undertaken, and 136 (general hospitals, 58%; hospitals with long‐term care beds, 42%) responded to the survey (response rate, 50.3%).
We compared the hospitals that did or did not respond using Pearson's χ2‐test, based on cross‐tabulation by which of the prefecture's tertiary emergency medical care zones the hospital was located in, the number of hospital beds, and whether the beds were for general or long‐term care. Comparison based on the prefecture's four tertiary emergency medical care zones did not reveal any significant differences (P = 0.008). Comparison of hospitals by the number of beds (i.e., ≤100, 101–200, 201–500, >500) also did not reveal any significant differences (P = 0.44). Lastly, there were no significant differences between the hospitals in terms of whether they provided long‐term medical care (P = 0.10). There were 77 respondents (56.2%) who provided their name, all of whom were physicians. By position and department, 44 of these respondents were hospital directors, 12 were from the intensive care department, 8 were from the internal medicine department, 4 were from the surgery department, 3 were from the palliative care department, and 6 were from other departments.
DNAR orders were considered necessary by 96% of the hospitals and unnecessary by 4%.
Implementation of the DNAR order was “being practised” by 88% of the hospitals and “not being practised” by the remaining 12%.
With regard to in‐hospital guidelines, 27% responded with “yes”, 71% with “no”, and 2% with “currently being created”.
- When asked who issues DNAR orders, the most frequent response was the “physician in charge” (52% of respondents). Some answered that “physicians, nurses, and other professionals” were responsible for issuing DNAR orders, and “other professionals” included medical social workers, nurses acting as discharge coordinator, care workers, and persons in charge of rehabilitation (Fig. 1).
Figure 1.
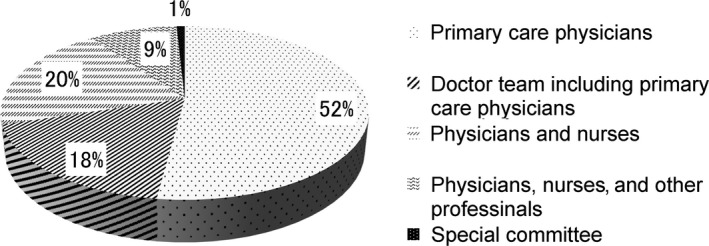 Decision‐makers of do not attempt resuscitation orders in 136 surveyed medical institutions in Kanagawa Prefecture, Japan.
Decision‐makers of do not attempt resuscitation orders in 136 surveyed medical institutions in Kanagawa Prefecture, Japan. - The proportion of patients with a DNAR order who had been involved in the decision process of their DNAR order was ≤25% at 81% of the hospitals, 25–50% at 12%, 50–75% at 1%, and ≥75% at 6% (Fig. 2).
Figure 2.
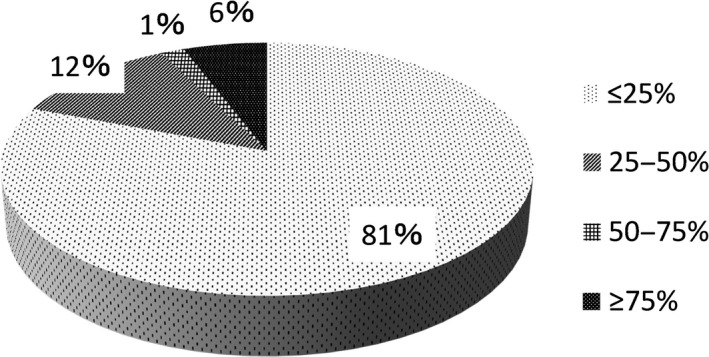 Involvement of patients in the decision‐making process for their own do not attempt resuscitation order, reported by 136 surveyed medical institutions in Kanagawa Prefecture, Japan.
Involvement of patients in the decision‐making process for their own do not attempt resuscitation order, reported by 136 surveyed medical institutions in Kanagawa Prefecture, Japan. - The leading diseases/conditions of patients with DNAR orders were malignant tumors, followed by pneumonia and old age/senility (Fig. 3).
Figure 3.
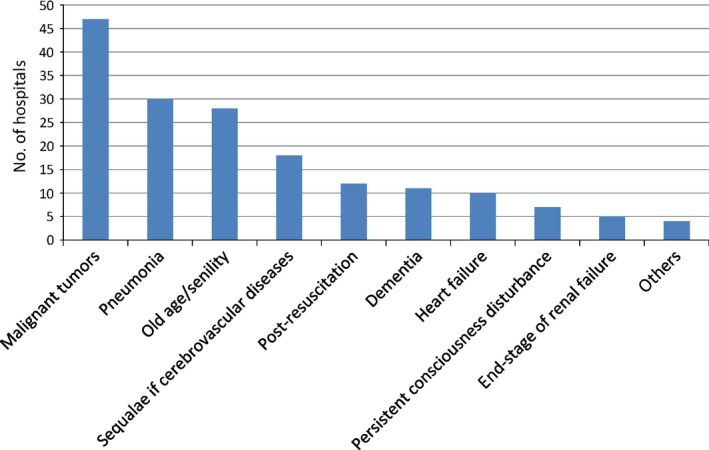 Diseases of patients with a do not attempt resuscitation order, as reported by 136 surveyed medical institutions in Kanagawa Prefecture, Japan.
Diseases of patients with a do not attempt resuscitation order, as reported by 136 surveyed medical institutions in Kanagawa Prefecture, Japan. DNAR order‐related advantages (responses were received from 84 hospitals, including multiple responses from the same hospital) included ease of response in the absence of the primary care physician (24 responses), no need for unnecessary life‐prolonging treatment (26), possibility of providing medical services requested by the patients and families (21), alleviation of mental stress among staff members (9), unified intention between medical care staff and family members (6), avoidance of problems at the time of acute deterioration (5).
Respondents identified the following issues with DNAR orders (responses were received from 94 hospitals, including multiple responses from the same hospital). Issues involving the patient's family members were as follows: the DNAR order was not agreed on by all family members (18 responses), the DNAR order was not fully understood by the family (14), and the intention of family members changed with time (5). For health‐care providers, DNAR order‐related problems were the following: instructions were unclear about what should or should not be done (12), dispute about whether to administer CPR when transporting patients to another hospital or by an emergency medical service (EMS) team (4), using the DNAR order as the reason for inaction when an event occurred that was unrelated to the underlying disease (2), unable to verify DNAR orders given verbally (2), unable to provide thorough care (1), uncertainty about the valid period of DNAR orders (1), and junior physicians who did not apply the DNAR order appropriately (1).
- Actions taken for DNAR patients undergoing a cardiac arrest at home were categorized by hospital hours. During clinic hours, the leading response was request for an ambulance (58%), followed by home visit by the primary care physician to confirm death (27%), requesting the family to bring the patient to the hospital by car (13%), and dispatching a transport vehicle to bring the patient to the hospital (2%). After clinic hours, the top hospital response was requesting an ambulance (60%), followed by home visit by the primary care physician to confirm death (28%), and requesting the family to bring the patient to hospital by car (12%) (Fig. 4).
Figure 4.
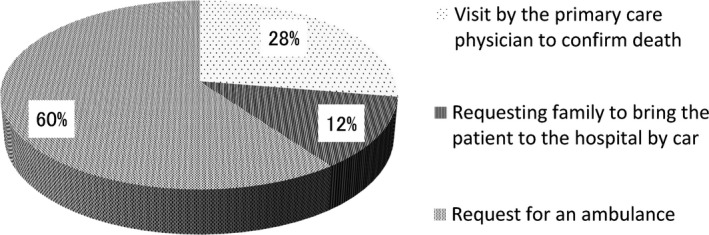 Management of patients with a do not attempt resuscitation order who had an acute deterioration at home, as reported by 136 surveyed medical institutions in Kanagawa Prefecture, Japan.
Management of patients with a do not attempt resuscitation order who had an acute deterioration at home, as reported by 136 surveyed medical institutions in Kanagawa Prefecture, Japan. - When asked about the instructions given to the EMS team who might respond to a request to treat a patient undergoing cardiac arrest at home who had a previously issued a DNAR order, 15% of institutions instructed them not to carry out CPR. Conversely, 18% of institutions instructed the EMS team to carry out CPR (basic life support only, 17%; advanced life support, 1%). The most frequent response given by approximately 70% of physicians was that no specific instructions were issued, with the decision on whether to perform CPR being left to the discretion of the EMS team (Fig. 5).
Figure 5.
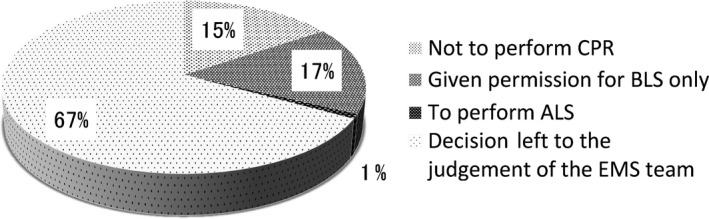 Do not attempt resuscitation order‐related instructions to emergency medical service (EMS) teams, as provided by 136 surveyed medical institutions in Kanagawa Prefecture, Japan. ALS, advanced life support; BLS, basic life support.
Do not attempt resuscitation order‐related instructions to emergency medical service (EMS) teams, as provided by 136 surveyed medical institutions in Kanagawa Prefecture, Japan. ALS, advanced life support; BLS, basic life support.
Discussion
The questionnaire began by asking about the need for DNAR orders in hospitals (Question 1), with 96% of responses indicating that they are necessary. The next question on whether the hospitals implemented DNAR orders in routine medical practice (Question 2) also yielded a high affirmative response rate of 88%. These responses indicate that there is a considerable need for DNAR orders in health‐care settings, and that they are in fact already extensively practiced in routine medical care. However, more respondents stated that their hospital did not have any internal guidelines in place for implementing the DNAR orders (71%) than those who stated their hospital did (27%) (Question 3).
When it comes to decision‐making on EOL care and DNAR orders, the various guidelines in Japan1, 2 and the USA and Europe3, 4, 5 emphasize respect for the patient's wishes based on proper medical advice, and recommend that health‐care providers engage in therapeutic decision‐making as part of a medical team consisting of various specialists, rather than simply entrusting decisions to a single physician. Within this context of a high implementation rate of DNAR orders and a lack of established guidelines at most hospitals, the next question concerned the individual or team who was responsible for issuing the DNAR orders (Question 4). Although 30% of respondents attributed this decision either to a multidisciplinary team consisting of physicians, nurses, and other specialists, or to a special committee, most respondents stated that physicians alone issued the order, with 52% indicating the primary care physician only and 18% indicating a medical team that included the primary care physician.
On the paramount issue of patient involvement in the decision‐making process on DNAR orders (Question 5), only 6% of respondents claimed that the patients themselves were involved in at least 75% of all DNAR orders, and 1% claimed that patients were involved in at least 50% of DNAR orders. Conversely, the majority of respondents indicated that the patients were largely uninvolved in the decision‐making process, with 81% stating that patient involvement accounted for less than 25% of all DNA orders.
In the question addressing patient diseases and background factors (Question 6), malignant tumors, pneumonia, old age/senility, sequelae of cerebrovascular disease, and dementia were the most common responses. While patient prognosis and quality of life have been identified as factors that influence decision‐making on DNAR orders,6, 7, 8, 9 it is not always feasible to expect a favorable outcome for patients with malignant tumors or pneumonia, or in patients who are elderly or senile, and this poor prognosis can lead to a DNAR order. However, even if a patient has a poor prognosis, it does not always mean that he/she does not wish to be resuscitated or receive aggressive treatment. As the final decision on DNAR orders will differ according to the attitude of the individual patient,10, 11, 12, 13 it is essential to confirm each and every patient's intentions wherever possible. Apart from these diseases and background factors, patients with sequelae of cerebrovascular disease or dementia or patients in a persistent vegetative state may lack decision‐making capability. Although a lack of decision‐making capability or the presence of a communicative disorder are typically identified as reasons why patients do not (or cannot) participate in the decision‐making process for DNAR orders,14 the existence of background factors such as cerebrovascular disease, dementia, or persistent vegetative state is likely to influence the lack of patient involvement in this process. However, the proportion of cerebrovascular disease, dementia, and persistent vegetative state in patients described in this questionnaire was extremely small compared to the rate of patients who were not involved in decision‐making on DNAR orders, suggesting that lack of decision‐making capability is not the only reason for the lack of patient involvement. In fact, the questionnaire was not able to demonstrate the direct reasons for the lack of patient involvement in decision‐making on DNAR orders.
While many of the physicians who responded to the questionnaire recognized the need for DNAR orders (Question 1) and actually implemented them (Question 2), when asked about the advantages of DNAR orders (Question 7), the most common responses were that they enabled the hospital to provide the type of care that patients and their family members wanted (25%; 21/84 hospitals, with multiple responses from the same hospital), that they eliminated unnecessary treatment (31.0%, 26/84 hospitals), and that they facilitated treatment by other medical personnel apart from the primary care physician (28.6%; 24/84 hospitals). Other less‐common responses were that DNAR orders helped to reduce the psychological stress of medical staff, enabled the medical staff to avoid potential crises when there was a sudden change in the patient's condition, and enabled peaceful EOL care in the manner desired by the patients and their family members when patients were close to death.
Conversely, when asked about the disadvantages of DNAR orders (Question 8), the most common response related to problems in dealing with family members. When the patient cannot participate in the decision‐making process for DNAR orders, the opinion of family members in their capacity as legally authorized representatives becomes crucial. However, the most commonly identified disadvantage of DNAR orders was that family members are often unable to agree on the DNAR order (19.1%; 18/94 hospitals); within this category, one of the issues raised most frequently was that family members who had travelled a long way to the hospital were opposed to the treatment plan. Other disadvantages included inadequate understanding of DNAR orders among family members (14.9%, 14/94 hospitals), and changes in the opinions of family members (5.3%, 5/94 hospitals), leading to confusion within the hospital. These findings suggest the importance of establishing guidelines on how to appoint a suitable legally authorized representative. The findings also highlight the need for proper understanding among family members by taking time to explain the situation, and by confirming their understanding a set period of time later. Furthermore, medical staff must have the requisite level of skill to explain the situation to family members in a manner that they can relate to.15, 16
Other disadvantages described in the responses concerned the medical staff. For example, in patients for whom DNAR orders had been issued, there was a lack of understanding among medical staff in determining the specific treatments to be provided and treatments to be withheld, and in failing to provide treatment for acute diseases separate from the patient's underlying disease. Furthermore, there were different attitudes among medical staff, such as young physicians and nurses, leading to confusion within the hospital (17.0%, 16/94 hospitals). In all aspects of EOL care, there are frequent reports of differing opinions among medical personnel on the extent of treatment that should be provided to patients,6, 17, 18 as well as the need for EOL care education and training.19, 20 To prevent this type of confusion, the Physician Orders for Life‐Sustaining Treatment paradigm established in the USA clearly specifies the patient's wishes and prescribes the extent of treatment to be provided, and has proven effective in eliminating this confusion in health‐care settings.21, 22 Another disadvantage of DNAR issues identified in the responses was that health‐care providers outside the hospital (such as paramedics or ambulance staff) were performing CPR on patients who had gone into cardiac arrest while at home (4%; 4/94 hospitals). This response highlighted the issue that DNAR orders are at present only shared by hospitals, rather than by the entire medical care sphere or community. As Japan's ageing population grows and the number of elderly people at home increases, we anticipate that this problem will become more pronounced.
Questions 9 and 10 addressed the response of health‐care providers when a patient with a DNAR order suffers a cardiac arrest in a setting outside the hospital, thus highlighting the fourth and fifth issues surrounding DNAR orders.
When a patient goes into cardiac arrest in the hospital, the hospital staff are the only responders so they can act in accordance with the DNAR order. However, if the patient were to suffer a cardiac arrest outside the hospital (e.g., at home), approximately 60% of physicians who were asked what to do by family members would respond by telling the family to call an ambulance. As a general rule, the EMS team provides CPR when encountering patients in cardiac arrest. Even in patients with a DNAR order, in Japan this order currently represents nothing more than an agreement between the hospital's medical professionals and the patient's family. Even if the family verbally instructs the EMS team not to perform CPR or shows them the relevant documentation issued by the hospital, there are no legal grounds to support their claims. The result is that the EMS team decides that it must perform CPR regardless of the family's wishes (even if there are sufficient grounds for the family to act as proxy in conveying the patient's wishes). The fourth issue is that DNAR orders have no legal recognition in Japan.
The EMS team must receive the physician's instructions before transporting a patient to the hospital without performing CPR. However, when asked in the capacity of physician in charge how to respond, only 15% of physicians said that they would instruct the EMS team to withhold CPR, while approximately 70% said that they would leave the decision to the EMS team. The fifth issue is that, even when a DNAR order is in place, the response of physicians varies, thus causing confusion in emergency settings.
Resolving this issue requires the adoption of legislation on DNAR orders such as that in the USA. Establishing DNAR orders in accordance with legal procedures, recording these decisions in a specified document, and having the patient carry this document on his/her person would finally allow EMS teams and other third‐party medical professionals outside the hospital to share the DNAR order.
Although this questionnaire was undertaken at hospitals in Kanagawa Prefecture, the results showed that many of the responding physicians recognized the need for DNAR orders, and many of the hospitals had a system in place for DNAR orders. It is unclear whether the very small extent of patient involvement in the decision‐making process on DNAR orders can be attributed to Japanese culture or beliefs but it does appear that there are limited opportunities in routine clinical practice in Japan for health‐care providers and patients to hold direct discussions while the patient is still lucid on how to respond if the patient were to suffer a cardiac arrest. As Japan confronts the reality of an ageing society, this is an issue that affects not only Kanagawa Prefecture but the entire nation. In the context of EOL care, future guidelines and the like should clarify the decision‐making process on DNAR orders, including when to confirm the patient's intention. In the absence of legislation such as that in the USA and Europe, it is preferable to establish prefectural ordinances or similar legislation to make DNAR orders legally effective so that they can be shared by the EMS team.
In Japan, the demand for a DNAR order is increasing, and the orders are frequently issued in clinical settings, often resulting in various problems because of the lack of appropriate legislation or guidelines. There is an urgent need for prefectures or municipalities to establish relevant laws and for local medical control authorities to develop guidelines.
Limitations
Caution must be paid when interpreting the DNAR order‐related problems noted here, because the survey was limited to a small number of institutions within Kanagawa Prefecture. However, there are almost no previous studies that have revealed the current status of DNAR orders in Japan. Because raising and resolving problems associated with DNAR order is an urgent issue in the field of EOL care, we believe that, even though this survey was carried out only within Kanagawa Prefecture, it provides the first step toward confronting problems associated with DNAR orders. In the future, a nation‐wide survey of institutions and patients may be a necessary step towards realizing better EOL care from multilateral perspectives.
Conflicts of Interest
None declared.
Funding Information
No funding information provided.
References
- 1. Japanese Ministry of Health, Labour and Welfare . Guidelines for Decision‐Making on End‐of‐Life Care. [cited May 2007]. Available from: http://www.mhlw.go.jp/shingi/2007/05/dl/s0521-11a.pdf [in Japanese]. [Accessed 2 March 2017]
- 2. Japanese Association for Acute Medicine, Japanese Society of Intensive Care Medicine, and Japanese Circulation Society . Guidelines for end‐of‐life care in emergency and intensive care treatment. [cited 4 November 2014]. Available from: http://www.jaam.jp/html/info/2014/pdf/info-20141104_02_01_02.pdf. [in Japanese].
- 3. Holms S, Jorgensen EO. Ethical issues in cardiopulmonary resuscitation. Resuscitation 2001; 50: 135–9. [DOI] [PubMed] [Google Scholar]
- 4. Bossaert LL, Perkins GD, Askitopoulou H et al European resuscitation council guidelines for resuscitation 2015 section 11. The ethics of resuscitation and end‐of‐life decisions. Resuscitation 2015; 95: 302–11. [DOI] [PubMed] [Google Scholar]
- 5. American Heart Association . American Heart Association Guidelines for CPR & ECC. Part 3. Ethical issues. 2015. [Accessed 3 March 2017]. Available from: https://eccguidelines.heart.org/index.php/circulation/cpr-ecc-guidelines-2/part-3-ethical-issues.
- 6. Bacerra M, Hurst SA, Junod Perron N, Cochet S, Elger BS. ‘Do not attempt resuscitation’ and ‘cardiopulmonary resuscitation’ in an inpatient setting: factors influencing physicians’ decisions in Switzerland. Gerontology 2011;57:414–21. [DOI] [PubMed] [Google Scholar]
- 7. Fujimoto K, Minami S, Yamamoto S et al Comparison of timing and decision‐makers of do‐not‐resuscitate orders between thoracic cancer and non‐cancer respiratory disease patients dying in a Japanese acute care hospital. Support. Care Cancer 2014; 22: 1485–92. [DOI] [PubMed] [Google Scholar]
- 8. Zingmond DS, Wenger NS. Regional and institutional variation in the initiation of early do‐not‐resuscitate organs. Arch. Intern. Med. 2005; 165: 1705–12. [DOI] [PubMed] [Google Scholar]
- 9. Naess M. “Do‐not‐attempt‐resuscitation”‐orders in ICCUs: a survey of attitudes and experiences of nurses in Norway. Intensive Crit. Care Nurs. 2009; 25: 140–6. [DOI] [PubMed] [Google Scholar]
- 10. Asai N, Ohkuni Y, Ashworth L, Kaneko N. Implementation of do not attempt resuscitate orders in a Japanese nursing home. Am. J. Hosp. Palliat. Care. 2014; 31: 27–32. [DOI] [PubMed] [Google Scholar]
- 11. Jesus JE, Allen MB, Michael GE et al Preferences for resuscitation and intubation among patients with do‐not‐resuscitate/do‐not‐intubate orders. Mayo Clin. Proc. 2013; 88: 658–65. [DOI] [PubMed] [Google Scholar]
- 12. Cherniack EP. Increasing use of DNR orders in the elderly worldwide: whose choice is it? J. Med. Ethics 2002; 28: 303–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Gorton AJ, Jayanthi NV, Lepping P, Scriven MW. Patients’ attitude towards “do not attempt resuscitation” status. J. Med. Ethics 2008; 34: 624–6. [DOI] [PubMed] [Google Scholar]
- 14. Hurst SA, Beccera M, Perrier NJ, Perron NJ, Cochet S, Elger B. Including patients in resuscitation decisions in Switzerland: from doing more to do better. J. Med. Ethics 2013; 39: 158–65. [DOI] [PubMed] [Google Scholar]
- 15. Deep KS, Griffith CH, Wilson JF. Discussing preferences for cardiopulmonary resuscitation: what do resident physicians and their hospitalised patients think was decided? Patient Educ. Couns. 2008; 72: 20–5. [DOI] [PubMed] [Google Scholar]
- 16. Robinson F, Cupples M, Corrigan M. Implementing a resuscitation policy for patients at the end of life in an acute hospital setting: qualitative study. Palliat. Med. 2007; 21: 305–12. [DOI] [PubMed] [Google Scholar]
- 17. Uhlmann RF, Cassel CK, McDonald WJ. Some treatment‐withholding implications of no‐code orders in an academic hospital. Crit. Care Med. 1984; 12: 879–91. [DOI] [PubMed] [Google Scholar]
- 18. Fritz Z, Fuld J, Haydock S, Palmer C. Interpretation and intent: a study of the (mis)understanding of DNAR orders in a teaching hospital. Resuscitation 2010; 81: 1138–41. [DOI] [PubMed] [Google Scholar]
- 19. Forte DN, Vincent JL. Velasco IT Association between education in EOL care and variability in EOL practice: a survey of ICU physicians. Intensive Care Med. 2012; 38: 404–12. [DOI] [PubMed] [Google Scholar]
- 20. Elo G, Dioszeghy C, Dobos M, Andorka M. Ethical considerations behind the limitation of cardiopulmonary resuscitation in Hungary—the role of education and training. Resuscitation 2005; 64: 71–7. [DOI] [PubMed] [Google Scholar]
- 21. Richardson DK, Fromme E, Zive D, Fu R, Newgard CD. Concordance of out‐of hospital and emergency department cardiac arrest resuscitation with documented end‐of‐life choices in Oregon. Ann. Emerg. Med. 2014; 63: 375–83. [DOI] [PubMed] [Google Scholar]
- 22. Jesus JE, Geideman JM, Venkat A et al Physician orders for life‐sustaining treatment and emergency medicine: ethical considerations, legal issues, and emerging trends. Ann. Emerg. Med. 2014; 64: 140–4. [DOI] [PubMed] [Google Scholar]


