Abstract
Case
A 64‐year‐old man with complaints of dyspnea and orthopnea secondary to a hepatic hydrothorax refractory to diuretic medication underwent the transjugular intrahepatic portosystemic shunt (TIPS) procedure to decrease the portal vein pressure. The TIPS procedure failed due to severe liver stiffness. Direct intrahepatic portocaval shunt (DIPS), a modified TIPS procedure that directly inserts a stent from the inferior vena cava to the portal vein, was successfully carried out.
Outcome
The DIPS procedure significantly decreased the patient's pleural effusion and respiratory symptoms.
Conclusion
No other medical treatment is available to control refractory pleural effusion caused by portal hypertension; however, the TIPS (or DIPS) procedure can be successfully carried out in patients <60 years old with a Model of End‐Stage Liver Disease score <15.
Keywords: Ascites; hypertension, portal; liver cirrhosis; pleural effusion; portosystemic shunt, transjugular intrahepatic
Introduction
Patients with liver cirrhosis frequently have various serious complications of portal hypertension, including ascites, hydrothorax, and hemorrhage from the varicose vein. Hepatic hydrothorax is defined as a significant pleural effusion that develops in patients with liver cirrhosis without any other underlying pulmonary or cardiac diseases. Hepatic hydrothorax is relatively uncommon, with an estimated prevalence of 5% to 12% in cirrhotic patients.1 However, compared to ascites, the symptoms of hepatic hydrothorax are more severe as the refractory pleural effusion directly decreases the lung volume, causing intolerable respiratory disorders, including dyspnea and chest pain.1 Decreasing portal vein pressure is the primary treatment goal in these patients. However, in patients with decompensated liver cirrhosis, conservative medical management of refractory hydrothorax is difficult, so concurrent thoracic drainage may be necessary.
The transjugular intrahepatic portosystemic shunt (TIPS), a useful interventional radiological procedure that aims to decrease the portal vein pressure, was originally reported in 1969.2 During the TIPS procedure, an intrahepatic shunt is created by placing a stent between the right branch of the portal vein and the right hepatic vein, and this diverts the blood stream from the portal vein into the systemic circulation (Fig. 1A). The efficacy of TIPS for treating refractory hepatic hydrothorax has been reported in several studies.1, 2, 3, 4, 5 In patients with difficult presentations or contraindications to the TIPS procedure, a direct intrahepatic portocaval shunt (DIPS), a modified TIPS procedure, can be used. During the DIPS procedure, a metallic stent is placed from the inferior vena cava (IVC) into the portal vein through the caudate lobe under intravascular ultrasound (IVUS) guidance (Fig. 1B).3 We describe a patient with refractory hydrothorax due to liver cirrhosis who was successfully treated with the DIPS procedure. This is the first case report in Japan about using the DIPS procedure with IVUS guidance.
Figure 1.

Schemes of a transjugular intrahepatic portosystemic shunt (TIPS) (A) and a direct intrahepatic portosystemic shunt (DIPS) (B). A, TIPS (original procedure) is created by stenting between the right (Rt.) branch of the portal vein (PV) and the Rt. hepatic vein (HV). B, DIPS is a modified TIPS procedure in which direct stent insertion is carried out from the inferior vena cava (IVC) into the PV through the caudate lobe under intravascular ultrasound (IVUS) guidance.
Case
A 64‐YEAR‐OLD MAN was admitted to our emergency department with complaints of severe dyspnea and orthopnea. He had been repeatedly hospitalized for the same reasons over the last 3 years. He had a history of liver cirrhosis, an esophageal varicose vein, and chronic obstructive pulmonary disease. On arrival, his vital signs were as follows: Glasgow Coma Scale score, 15 (eyes, 4; verbal, 5; motor, 6); blood pressure, 167/89 mmHg; heart rate, 167/min; respiratory rate, 28/min; and saturation of peripheral oxygen (SpO2), 95% with 10 L/min oxygen through a mask. On physical examination, labored breathing, abdominal swelling, and peripheral pitting edema were identified. Electrocardiogram and ultrasound echocardiogram showed no cardiac dysfunction (ejection fraction >60%) on admission (day 1). Blood test results indicated hypoalbuminemia (albumin, 2.0 g/dL), hyperbilirubinemia (total bilirubin, 2.2 mg/dL), and coagulopathy (prothrombin time – international normalized ratio, 1.56). These results confirmed the clinical diagnosis of liver cirrhosis with an esophageal varicose vein, which was estimated to be a class C according to the Child–Pugh classification.
Chest radiographs (Fig. 2A) and computed tomography scans showed a large amount of pleural effusion in the right thoracic cavity. Thoracic drainage was carried out (Fig. 1B), while at the same time administering 20% albumin and diuretics (furosemide and spironolactone) daily for 3 days. As the mean volume of pleural fluid did not decrease to less than 1000 mL/day, the TIPS procedure was selected as the next treatment on post‐admission day 9 (Fig. 2D). A vascular anomaly due to parenchymal fibrosis was observed in the hepatic veins. Furthermore, the liver stiffness was too severe to penetrate the portal vein with a needle. Therefore, the DIPS procedure was undertaken on post‐admission day 15 under IVUS guidance (Fig. 1b, and Fig. 3). An intrahepatic shunt was successfully created between the portal vein and IVC through the caudal lobe using a metalic stent (E‐Luminexx R, Bard Peripheral Vascular, Tempe, AZ, USA: diameter, 10 mm; length, 60 mm). Following successful placement of the DIPS, the mean portal vein pressure changed from hypertensive (30 mmHg) to normotensive (18 mmHg). The daily volume of right pleural effusion was significantly decreased, and the chest tube was removed on post‐admission day 19. The patient was free from dyspnea; thus, he was transferred to another hospital for rehabilitation.
Figure 2.
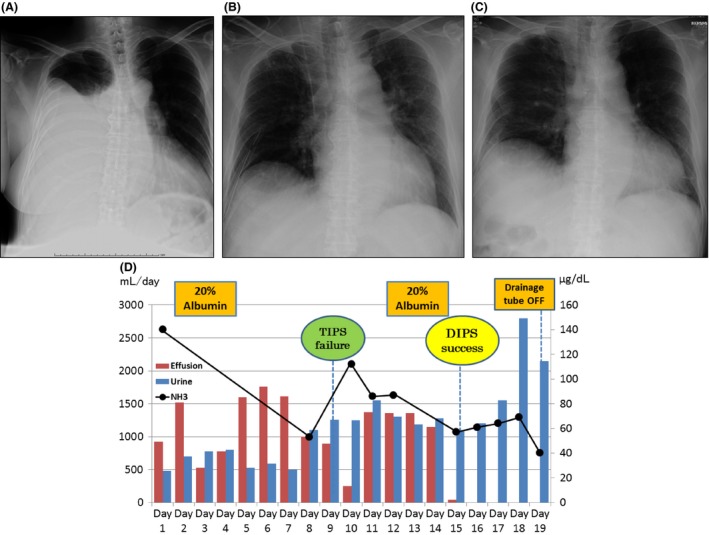
A, Chest radiographs of a 64‐year‐old man showing severe pleural effusion in the right thoracic cavity on arrival at hospital. B, On day 2, a massive pleural effusion (1520 mL) was drained again, and we continued to i.v. administer two types of diuretics (furosemide, 40 mg; spironolactone, 25 mg/day). C, No pleural effusion was observed on chest radiographs after the direct intrahepatic portosystemic shunt (DIPS) procedure was carried out. D, The patient's clinical course is shown graphically. TIPS, transjugular intrahepatic portosystemic shunt.
Figure 3.

Fluoroscopy and angiography in a 64‐year‐old man with refractory pleural effusion caused by portal hypertension. Imaging was carried out during the direct intrahepatic portosystemic shunt procedure. Fluoroscopy image during angiogram showing a guide wire (GW) and 4‐Fr catheter penetrating from the inferior vena cava (IVC) to the portal vein (PV) through the caudal lobe of the liver. This was a direct portosystemic shunt to the IVC that corresponded to the segment between the two arrowheads. A, Digital subtraction angiogram showing portosystemic shunt flow circulating from the PV (white arrow) to the IVC (black arrow), which corresponds to a segment between the two arrowheads. B, A high‐magnification view of the fluoroscopic image showing the replacement of a nitinol stent (E‐LuminexxR, Bard Peripheral Vascular, Tempe, AZ, USA; diameter, 10 mm; length, 60 mm) between the PV and IVC. An intravascular ultrasound (IVUS) probe was inserted from the right femoral vein to the IVC for real‐time needle guidance. The white and black arrows indicate the PV and IVC, respectively. C, Vertical sector image created by the IVUS probe showing detailed, real‐time visualization, which facilitates needle puncture from the IVC to the PV. CBD, common biliary duct; GB, gall bladder; HA, hepatic artery; SV, splenic vein.
Discussion
We propose the following possible treatments for hepatic hydrothorax: (i) pleural drainage, (ii) treatment with diuretics, (iii) treatment with albumin, (iv) pleurodesis, if possible, (v) the TIPS or DIPS procedure, (vi) surgery.1, 2, 4
The clinical indications for the TIPS procedure are as follows: (i) uncontrollable variceal bleeding, (ii) the presence of refractory ascites or hydrothorax, (iii) miscellaneous abnormal symptoms, including acute gastropathy, hepatorenal syndrome, Budd–Chiari syndrome, and hepatopulmonary syndrome. Similarly, clear contraindications for the TIPS procedure have also been established: (i) right heart failure with pulmonary hypertension, (ii) severe polycystic liver disease, (iii) liver abscess or severe sepsis, (iv) unrelieved biliary obstruction, (v) portal hypertension induced by an arterioportal fistula. Additional contraindications of the TIPS procedure include: (vi) hepatic vein thrombosis, (vii) coagulopathy, (viii) hepatocellular carcinoma, (ix) severe liver failure.2, 3, 4 Direct intrahepatic portocaval shunt should be considered for patients who have a vascular anomaly, portal vein thrombosis, calcification, or an unsuitable parenchymal tract due to hepatocellular carcinoma, and a secondary approach should be considered for occluded TIPS revision.4
Several studies have reported on the remarkable success of TIPS to improve portal hypertension. Indeed, a TIPS can significantly reduce the portosystemic pressure gradient in more than 90% of cases, with the portosystemic pressure gradient maintained within 12 mmHg after the TIPS procedure.5 Transjugular intrahepatic portosystemic shunt improved untreatable refractory hydrothorax in more than 80% of these cases and facilitated the complete removal of pleural effusion in 60–70% of patients. In addition, the TIPS procedure provided symptomatic relief in 70–80% of patients with refractory hydrothorax.3, 6 However, there have been several reports of worsening hepatic encephalopathy (HE) after the TIPS procedure in 30–46% of cases and intrahepatic shunt insufficiency in 15–25%.2, 3, 4, 5, 6 The deterioration of hepatic function, hepatorenal syndrome, intraperitoneal hemorrhage, or hemobilia may also occur in rare cases.2, 3, 4, 5, 6 The approximate survival rates of patients who underwent the TIPS procedure were as follows: 3 months, 80%; 6 months, 75%; 1 year, 40–60%; 3 years, 25%; and 5 years, 15%.2, 6, 7
Regarding the prognosis after the TIPS procedure, three indexes are generally used as cut‐off values to determine the benefit of TIPS for patients with severe liver disease. Namely, the Child–Pugh score (>12), Model of End‐stage Liver Disease (MELD) score (>22), and serum bilirubin level (>3 mg/dL) have been proposed as predictors of a bad prognosis.3, 4, 5 When patients are younger than 60 years old and their pre‐TIPS MELD score is <15 points, symptomatic recovery is estimated to be better.3, 6, 7 Our patient was 64 years old (>60 years), his Child–Pugh score was 13 (>12), and his MELD score was 21 (>15). Although age and the severity of liver dysfunction may be used to determine the patient's benefits, we could not rule out TIPS (or DIPS) as a treatment procedure, because his laboratory data were within the cut‐off values, the MELD score was 21 (<22), and total bilirubin level was 2.1 (<3.0 mg/dL). Furthermore, the absence of heart failure and HE (NH3 57 μg/dL) were also good prognostic factors for beneficial TIPS.2, 4 This may explain why we achieved a better outcome after the DIPS procedure. The patient's symptoms recovered quickly after DIPS without worsening HE. Our results provided us with significant insights on the TIPS procedure in terms of managing emergency cases of portal hypertension, particularly in patients whose hydrothorax or ascites are difficult to control.
Conclusions
Our patient with refractory hepatic hydrothorax due to cirrhosis was managed using a modified TIPS procedure, a DIPS, which resulted in a significant decrease in pleural effusion and symptoms. In cases of persistent hepatic hydrothorax refractory to any conservative medical management, the TIPS (or DIPS) procedure can be a promising option for treating severe portal hypertension.
Conflict of Interest
None declared.
Acknowledgements
We thank Ms. Rika Ono for her technical assistance with submitting the manuscript. We also acknowledge Editage for their English editing.
Funding Information
No funding information provided.
References
- 1. Siddappa PK, Kar P. Hepatic hydrothorax. Trop. Gastroenterol. 2009; 30: 135–41. [PubMed] [Google Scholar]
- 2. Rössle M. TIPS: 25 years later. J. Hepatol. 2013; 59: 1081–93. [DOI] [PubMed] [Google Scholar]
- 3. Fidelman N, Kwan SW, LaBerge JM, Gordon RL, Ring EJ, Kerlan RK Jr. The transjugular intrahepatic portosystemic shunt: an update. Am. J. Roentogenol. 2012; 199: 746–55. [DOI] [PubMed] [Google Scholar]
- 4. Kirby JM, Cho KJ, Midia M. Image‐guided intervention in management of complications of portal hypertension: more than TIPS for success. Radiographics 2013; 33: 1473–96. [DOI] [PubMed] [Google Scholar]
- 5. Boyer TD, Haskal ZJ. American Association for the Study of Liver Diseases Practice Guidelines: the role of transjugular intrahepatic portosystemic shunt creation in the management of portal hypertension. J. Vasc. Interv. Radiol. 2005; 16: 615–29. [DOI] [PubMed] [Google Scholar]
- 6. Siegerstetter V, Deibert P, Ochs A, Olschewski M, Blum HE, Rössle M. Treatment of refractory hepatic hydrothorax with transjugular intrahepatic portosystemic shunt: long‐term results in 40 patients. Eur. J. Gastroenterol. Hepatol. 2001; 13: 529–34. [DOI] [PubMed] [Google Scholar]
- 7. Dhanasekaran R, West JK, Gonzales PC et al Transjugular intrahepatic portosystemic shunt for symptomatic refractory hepatic hydrothorax in patients with cirrhosis. Am. J. Gastroenterol. 2010; 105: 635–41. [DOI] [PubMed] [Google Scholar]


