Abstract
Aim
Purpose of this case report is to highlight the precision and accuracy obtained with patient specific implants for orbital reconstruction designed on the basis of volumetric analysis of orbital computed tomographic scan (CT) scans using virtual planning, computerised designing and manufacturing and stereolithographic models to correct late post-traumatic orbital deformities such as enophthalmos and diplopia.
Material and methods
This case report describes a patient who visited our outpatient clinic for correction of enophthalmos and persistent diplopia in upward gaze, seven months post trauma. Three dimensional (3D) virtual treatment planning was carried out by using the 3D CT data. The unaffected orbit of the contralateral side was superimposed on the deformed orbit to highlight the defect and a customized implant was designed in the desired size and shape on the virtual model using computer aided designing and manufacturing (CAD-CAM) and milled in titanium mesh for precise anatomic orbital reconstruction.
Results
There was a marked improvement in both the diplopia in upward gaze and enophthalmos post surgery when the customized patient specific orbital implant was used.
Conclusion
The concept of using customized implant with the help of 3D virtual treatment planning, 3D stereolithographic models and CAD-CAM greatly improves the correction of extremely difficult late post-traumatic orbital deformities.
Keywords: Enophthalmos, Diplopia, Customized implant, Orbital volume
1. Introduction
Orbital and naso-orbital ethmoid fractures can result in changes in bony orbital dimensions that may alter the function of intraorbital contents and lead to serious complications. Orbital wall fractures can result in increased orbital volume, tissue herniation into maxillary sinus, fat atrophy, loss of ligament support, scar contracture, subsequently leading to enophthalmos and diplopia. Such deformities are extremely difficult to manage due to the complex and highly variable anatomy.1 It is generally accepted that the presence of clinical symptoms like diplopia, enophthalmos, motility disturbances of the globe, and fractures resulting in orbital floor or wall defects larger than 10 mm in diameter, indicate the need for surgical treatment ie open reduction, internal rigid fixation and orbital reconstruction.
The unique anatomy of the orbit and the resulting surgical approaches make the process of fitting and aligning implants difficult, time consuming and operator dependent.1, 2 During the past decades, autogenous bone grafts were considered ideal for the treatment of orbital floor fractures. However, it is important to consider the following factors: the quantity of bone required at the recipient site, the biologic qualities of the donor bone, the unpredictable resorption of the bone graft, and the considerable donor site morbidity.1 These listed shortcomings associated with autogenous bone graft have led to the development of four basic types of implant materials for orbital wall reconstruction: allogeneic grafts, xenografts, nonresorbable synthetic alloplastic materials, and resorbable synthetic alloplastic materials.2, 15 Titanium mesh and high-density porous polyethylene implants are presently the most commonly used nonresorbable synthetic allopastic materials for orbital floor reconstructions. Most commercially available implants are supplied in generic sizes and shapes, which are designed on the basis of the “average” patient, not the “average” defect.1
Use of newer technologies from computer-guided surgical planning and additive manufacturing, produce passive fitting implants customized for patient-specific needs, and have allowed reconstruction of late orbital deformities. When this is used for late deformities, there is sufficient time to assess, plan, and custom manufacture the highly precise implants. Planning and simulation involves creation of a virtual model of the desired surgical outcome using special planning software. The accuracy of implant fit can be virtually verified before surgery. 3D models and virtual reconstructions can be used for manufacturing patient-specific implants. During the surgical procedure, planning is transferred to the surgical site as accurately as possible. The aim of reconstruction is to restore the orbit in 3 dimensions.2, 15
Purpose of this case report is to highlight the precision and accuracy obtained with patient specific implants for orbital reconstruction designed on the basis of volumetric analysis of orbital computed tomographic scan (CT) scans using virtual planning, computerised designing and manufacturing and stereolithographic models to correct late post-traumatic orbital deformities such as enophthalmos and diplopia.
2. Case report
A 29-year-old male patient presented to our outpatient clinic in May 2017, reporting with diplopia during upward gaze and severe enophthalmos. He had a history of trauma due to motor vehicle accident seven months back when he was rushed to a nearby hospital and managed conservatively for bleeding. He later visited some other centre, and was operated for his associated maxillary fractures and was left un-noticed for his left orbital wall fractures.
Clinical examination revealed restriction of eye movements of the left eye in upward gaze, leading to diplopia during upward gaze and severe enophthalmos. CT scan revealed fractures of orbital floor, medial wall, nasal bone (left side), infraorbital and supraorbital rims and also showed few plates and screws fixed at lefort I level as patient was operated previously (Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6, Fig. 7).
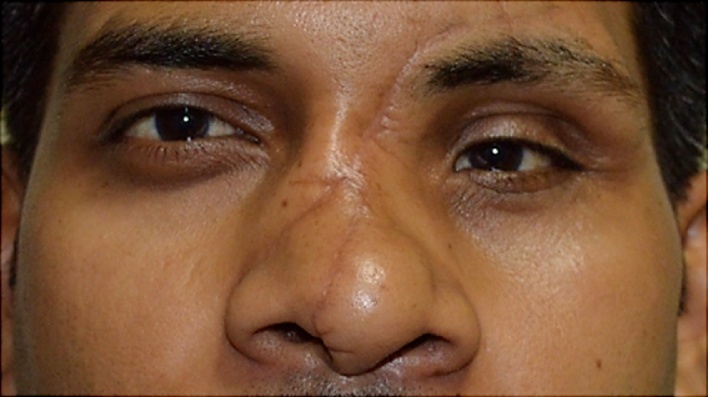
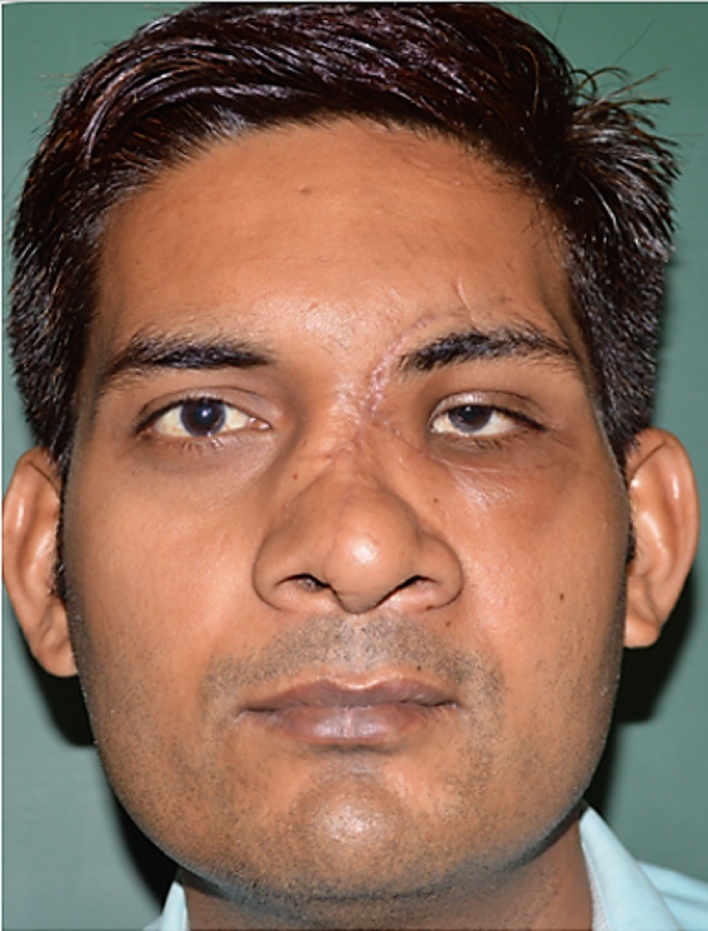
Fig. 1.
Preoperative frontal view of a patient having 3 mm hypoglobus and facial asymmetry.
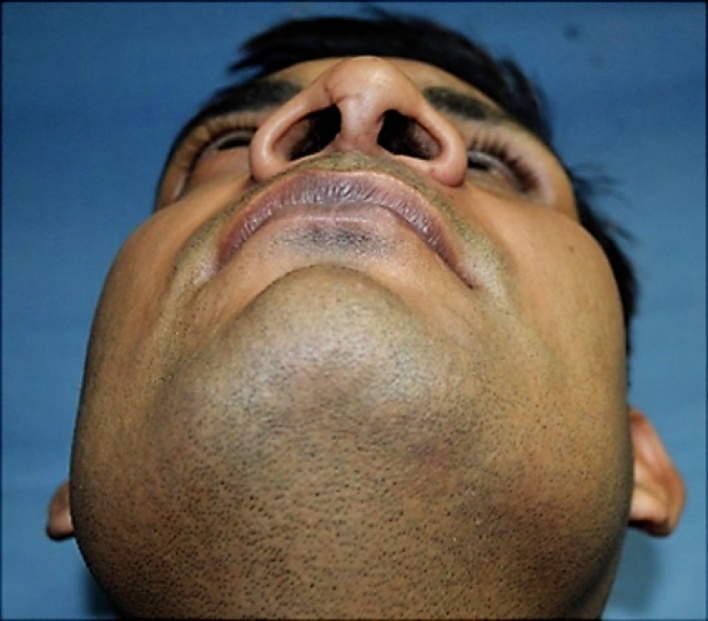
Fig. 2.
Preoperative picture showing marked hypoglobus and scar mark present over his nose.
Fig. 3.
Preoperative picture showing restriction of left eye movement in upward gaze.
Fig. 4.
Preoperative picture showing depressed left malar and infraorbital region and also marked enophthalmos (5 mm) in his left eye.
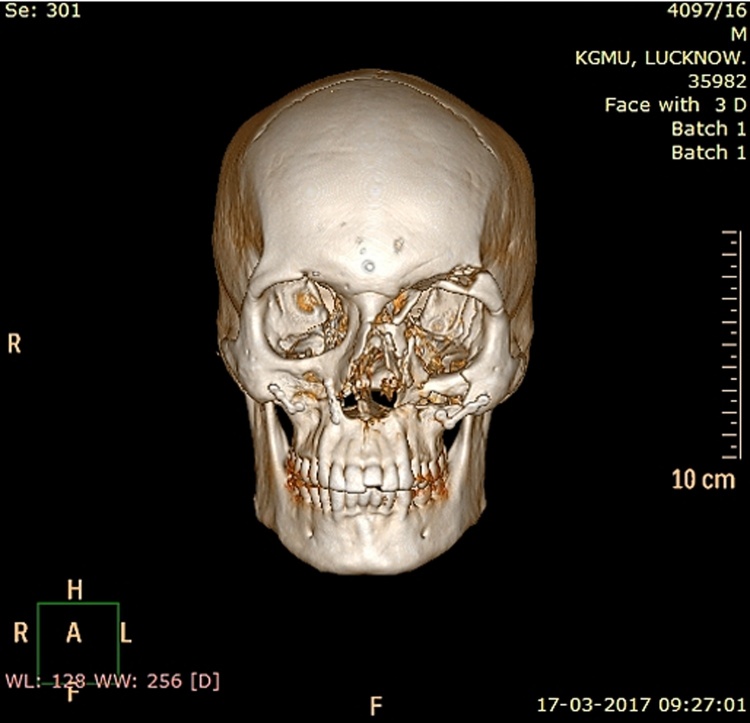
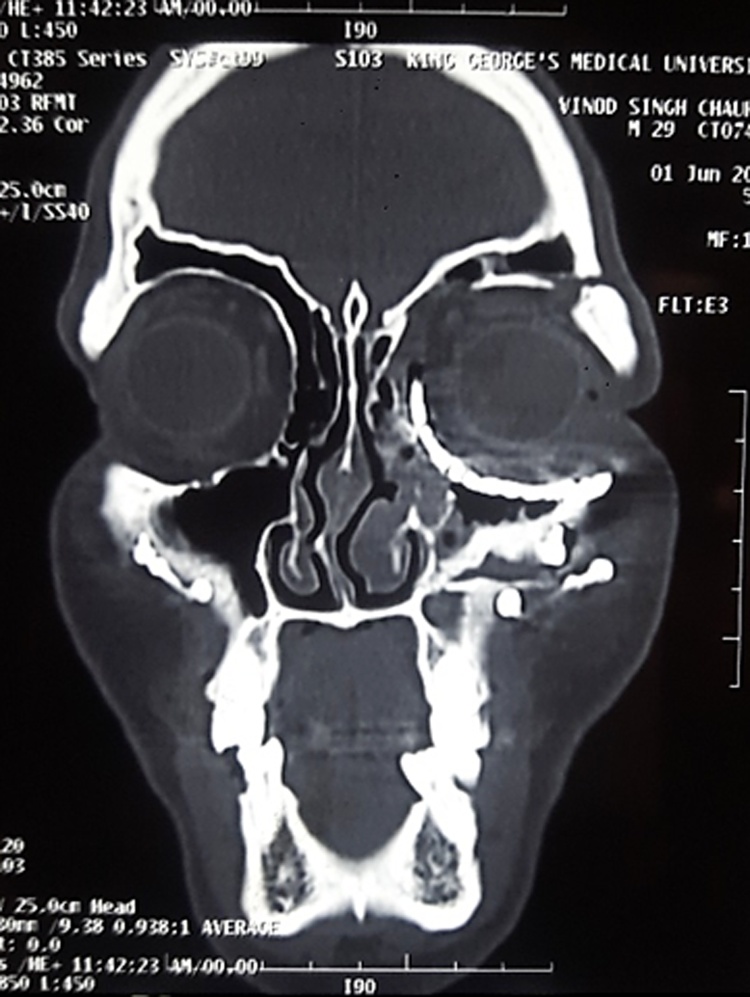
Fig. 5.
Preoperative CT face 3D reconstruction frontal view, section showing fracture of orbital floor left side, medial orbital, superior orbital wall, and inferior, medial and superior orbital rim.
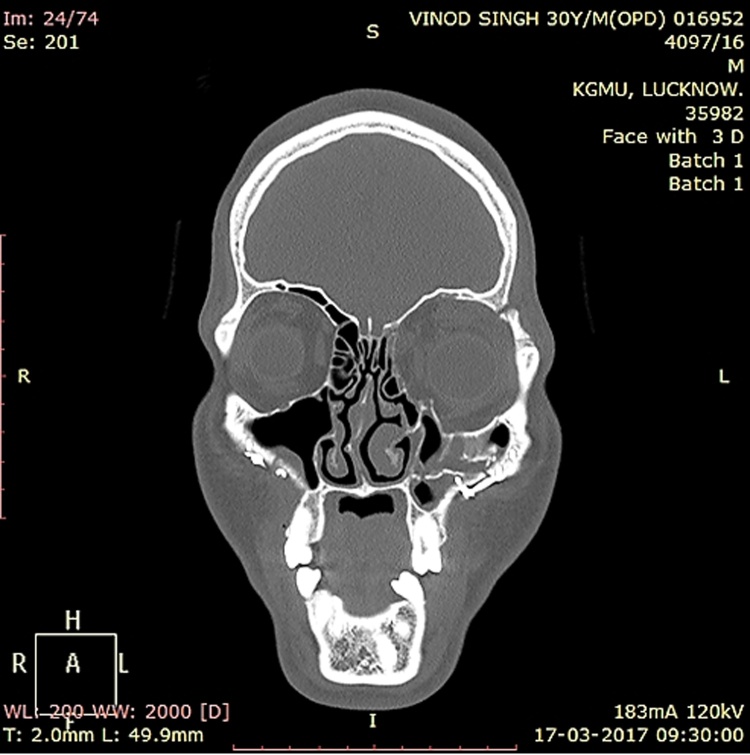
Fig. 6.
Preoperative CT coronal section, showing marked increase in orbital volume in left eye, fracture orbital floor, medial wall, superior wall and fronto zygomatic suture region.
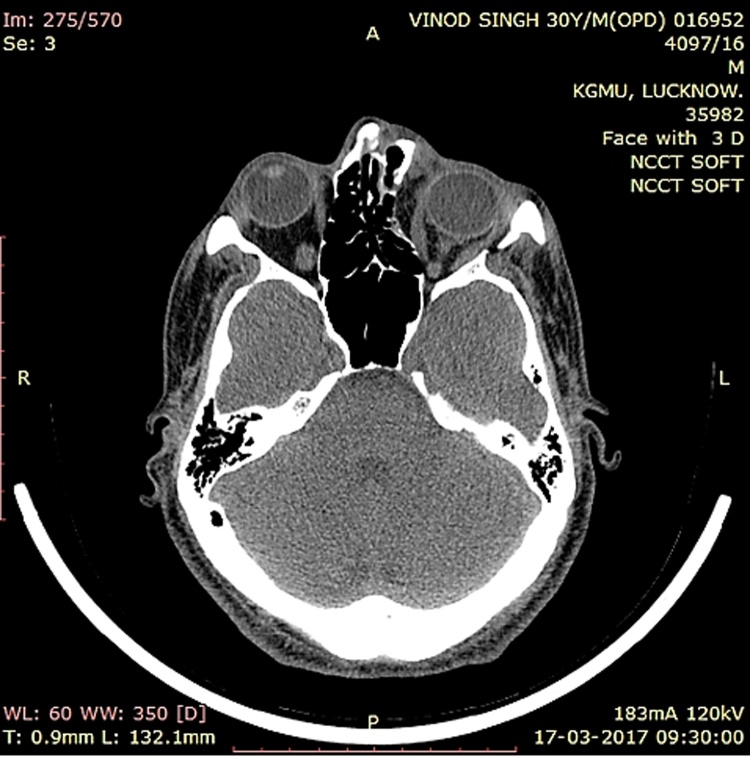
Fig. 7.
Preoperative CT axial section fracture at zygomatico-sphenoid suture region, and posterior positioning of left eye globe as compared with right eye.
3. Clinical management, imaging, and patient specific implant fabrication workflow
Patient management required a thorough ophthalmic and clinical evaluation combined with an adequate imaging procedure. Preoperatively, a thin-cut (2 mm) computed tomographic scan (CT 64-slice scanner) was obtained. The data were recorded in a generic Digital Imaging and Communications in Medicine (DICOM) format and transferred to a Windows-based computer workstation with computer-assisted design and computer-assisted manufacturing software. The software converted the data for 3-dimensional reconstruction in the axial, coronal, and sagittal views. The scan was adjusted by anatomic landmarks for symmetry. Planning was performed by mirroring the unaffected side to the side where reconstruction was necessary. The data of the reconstructed orbit with the determination of the planned patient specific implant were sent to the manufacturer. The surgeon and the software designer planned the patient specific implant in titanium mesh to create its optimal shape and size. Flanges were added to the design to ensure perfect sagittal positioning and screw holes were also designed for fixation along the orbital rims.
This implant could be easily stabilized, and had the unique ability to compensate for volume without resorbption thus maintaining the orbital shape and volume (Fig. 8, Fig. 9, Fig. 10, Fig. 11).
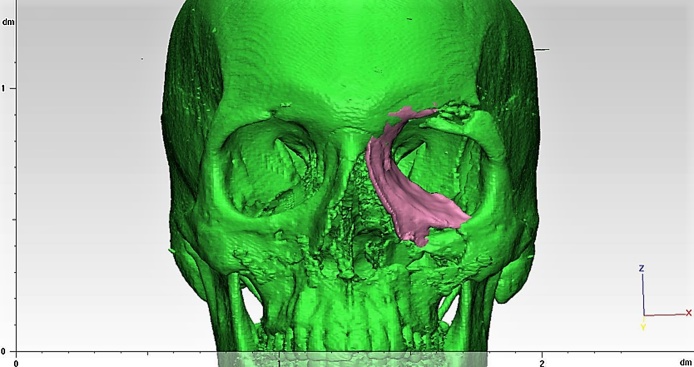
Fig. 8.
Computer Assisted Designing of implant for 3D reconstruction of fracture medial wall, orbital floor and superior orbital wall.
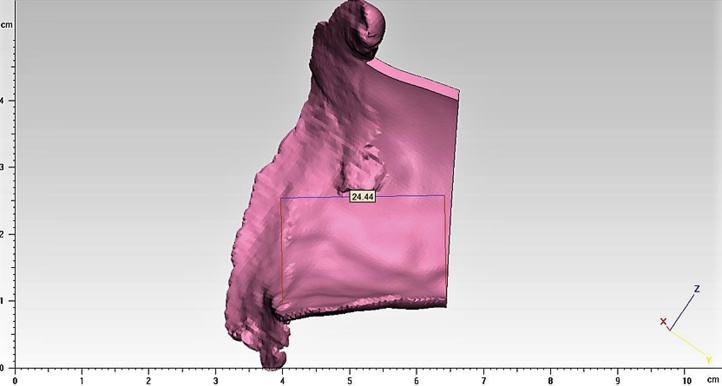
Fig. 9.
3D computerized designing of implant with its antero-posterior dimension.
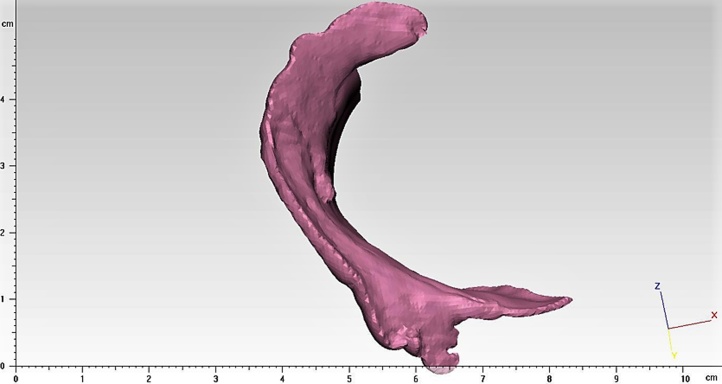
Fig. 10.
Computerized designed complete implant extension.
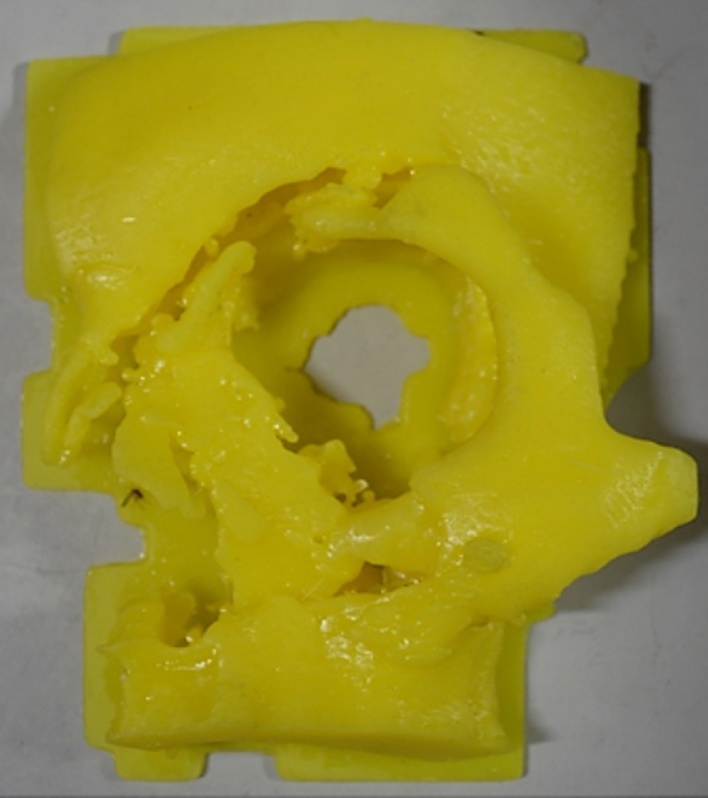
Fig. 11.
Stereolithographic model showing fracture of orbital floor, medial wall and superior walls for treatment planning.
4. Surgical technique
After part preparation, tarsorrhaphy suture was placed for protection of the eye globe. Local anesthesia with vasoconstrictor was injected before making the subciliary incision, extended medially up to the scar on the nose and forehead. Incision was made through skin, and preorbital orbicularis oculi muscle was dissected down to the preorbita. The entrapped orbital muscles and periorbital fat was released. Medial canthotomy was done for proper placement of implant to reconstruct medial wall of orbit, orbital floor and part of the superior orbital rim. Implant was placed and eye movements were checked before its fixation over the orbital rim (Fig. 12).
Fig. 12.
Intraoperative picture showing placement of 3D reconstructed customized implant.
5. Results
Patient showed marked correction of his upward gaze diplopia and enophthalmos when a customized patient specific implant was used. He was very pleased and quite satisfied with the result (Table 1, Fig. 13, Fig. 14, Fig. 15).
Table 1.
Postoperative results as compared to preoperative findings.
| Preoperative findings | Postoperative findings |
|---|---|
| Diplopia in upward gaze | Diplopia absent in all gaze |
| Enophthalmos, 5 mm present in left eye | No enophthalmos |
| Hypoglobus, 3 mm left eye | No hypoglobus |
| Infraorbital nerve paresthesia absent | Infraorbital nerve paresthesia absent |
| Restricted ocular movement in all directions | No restriction of ocular movement in any direction |
| Orbital volume of left eye more as compared to right eye | Orbital volume of left eye less as compared to right eye (over correction) |
Fig. 13.
Postoperative frontal profile of the patient showing marked correction of hypoglobus and enophthalmos in his left eye and improvement in facial symmetry of the patient.
Fig. 14.
Postoperative coronal section showing symmetrical orbital volume in both the orbit after reconstruction with customized implant.
Fig. 15.
Postoperative 3D CT face section showing proper reconstruction of medial orbital wall, orbital floor, and superior orbital wall in left eye.
6. Discussion
Both prospective and retrospective studies of patients who have sustained midfacial fractures indicate that as many as 40% may sustain serious ocular injury that warrant ophthalmologic referral.10, 11 A recent study demonstrated that up to 91% of patients with orbital fractures, who had an ophthalmic evaluation within 1 week of their injury, sustained some form of ocular injury. Many of these were classified as mild but 45% were moderate or severe injuries.
Understanding the injury is the first step towards reconstruction of the late orbital deformities as orbital trauma may result in serious changes to the orbital dimensions, thereby altering both the position and function of intraorbital contents, leading to serious complications such as diploplia, enophthalmos or visual acuity disturbances. Although diplopia and enophthalmos are symptoms of an acute orbital injury, they are the most common late sequelae of orbital blow-out fractures; and represent the greatest reason for patients to seek late reconstruction of their orbital deformities.
The correction of enophthalmos and diplopia has been discussed widely in the literature. Industry preformed meshes are popular for the reconstruction of orbital fractures.3 However, in cases where there is scant remaining bone tissue or reduction of fractured fragments is not possible, customized implants have been described as a viable option to restore the orbital contours and the orbital volume. Such orbital reconstruction is a simple, swift surgery with less morbidity when compared with osteotomies and mobilization. Customized implants offer the advantage of no resorbption, unlike bone grafts, and larger volumes can be used, unlike mesh, when a drastic volume reduction is necessary.
With advances in diagnostic imaging and surgical approaches, availability of different biomaterials including lyophilized dura, polyethylene or polydioxanone sheets, hydroxyapatite blocks, titanium mesh, ceramic inlays and autogenous bone grafts, individual, inexpensive customized implants have become possible for orbital reconstruction. The ideal material for orbital reconstruction still remains controversial. The more elastic is the material, the less capable it is to withstand the dynamic stresses of the large bony orbital defects. Resorbable implants tend to produce foreign body reactions, implant exposure or completely resorb leaving only remnants of fibrous connective tissue. Autologous bone grafts offer minimal contourability and may result in donor site defects. PEEK (polyetheretherketone)15 is extensively used for craniofacial reconstruction worldwide offering advantages like excellent biocompatibility, good mechanical strength and radiographic translucency, ability to be manufactured as thin parts and can be drilled for rigid plate fixation to the maxillofacial skeleton. However, it is still not available commercially in developing countries due to its high cost. Titanium has a long track record in the reconstruction of large orbital defects and correction of globe. It is radio-opaque and produces very specific postoperative radiographic image and can be affixed using standard osteosynthesis screws.1, 2 Most commercially available implants are supplied in generic sizes and shapes, which are designed on the basis of the “average” patient, not the “average” defect.16
Correction of diplopia not only requires adequate reconstruction of the orbital content and releasing tissues, but also correction of orbital volume. In 2002, Gellrich et al. used computer-assisted planning for orbital reconstruction using mirror image of the healthy contralateral orbit to design implant for affected orbit. This virtual design regained the lost symmety between the two orbits. Surgical navigation allowed intraoperative control of the new contours, with an average difference of 0.43 cm3 between the healthy and operated orbit. Overcorrecting the globe has been suggested to avoid any relapse in globe projection.9 Even with a good orbital reconstruction, inadequate reestablishment of orbital volume can result in enophthalmos, diplopia, and reduced visual acuity.
An et al reported a direct relationship between an increased orbital volume and moderate enophthalmos based on his study on the changes in orbital volume and delayed enophthalmos, assisted by CT scan Images.8 For every 1 ml of volume increase there is approximately 0.9 mm of enophthalmos.1 Post-traumatic enophthalmos is more related to a failure to restore the orbital volume and reconstruction of the height of retrobulbar portion of orbit, than changes in the contents of soft tissue. It may also result from atrophied orbital adipose tissue, dislocation of trochlea, scar contraction in retrobulbar tissues, unrepaired fractures in the orbital walls, and displaced orbital tissue.2
Our patient showed full improvement in his upward gaze diplopia and enophthalmos, due to the precise fit of the pre-shaped orbital floor implant thereby leading to accurate ‘true-to original’ shape. Although, numerous techniques to quantify the position of the ocular globe have been developed, there is evidence that such evaluation is not yet a precise science. For this reason, a clinical subjective evaluation of enophthalmos and diplopia was used in the present study.
Consensus is to correct enophthalmos and delayed diplopia by precise restoration of the orbital contours and volume, the role of overcorrection of orbital volume in treating late enophthalmos is an interesting topic and requires further investigation in greater detail in future studies.
7. Conclusion
The patient specific implant appear to be very useful for precise pretraumatic reconstruction of extensive orbital wall damage thereby correcting enophthalmos, hypoglobus and diplopia. This technology, offers the possibility of physically replicating the morphology of damaged anatomic structures, and may be used to explain, plan, and perform an operation in extremely difficult cases. This approach makes the use of a limited surgical access, and the precise fit greatly decreases the operation time. The concept of customized patient specific orbital implants greatly improves the correction of very difficult late post-traumatic orbital deformities.
Conflict of interest
None.
References
- 1.Pedemonte C., Sáez F., Vargas I., González L.E., Canales M., Salazar K. Can customized implants correct enophthalmos and delayed diplopia in posttraumatic orbital deformities? A volumetric analysis. Int J Oral Maxillofac Surg. 2016;45:1086–1094. doi: 10.1016/j.ijom.2016.04.007. [DOI] [PubMed] [Google Scholar]
- 2.Wolff J., Sándor G.K., Pyysalo M., Miettinen A., Koivumäki A.V., Kainulainen V.T. Late reconstruction of orbital and naso-orbital deformities. Oral Maxillofacial Surg Clin N Am. 2013;25:683–695. doi: 10.1016/j.coms.2013.07.008. [DOI] [PubMed] [Google Scholar]
- 3.Baumann A., Sinko K., Dorner G. Late reconstruction of the orbit with patient-specific implants using computer-aided planning and navigation. J Oral Maxillofac Surg. 2015;73:S101–S106. doi: 10.1016/j.joms.2015.06.149. [DOI] [PubMed] [Google Scholar]
- 8.An J.G., Zhang Y., Zhang Z.Y. Computer-assisted fabricated individual titanium mesh for reconstruction of orbital wall. Beijing Da Xue Xue Bao. 2008;40(1):88–91. [PubMed] [Google Scholar]
- 9.Metzger M.C., Schön R., Weyer N. Anatomical 3-dimensional pre-bent titanium implant for orbital floor fractures. Ophthalmology. 2006;113(10):1863–1868. doi: 10.1016/j.ophtha.2006.03.062. [DOI] [PubMed] [Google Scholar]
- 10.Schön R., Metzger M.C., Zizelmann C., Weyer N., Schmelzeisen R. Individually preformed titanium mesh implants for a true-to-original repair of orbital fractures. Int J Oral Maxillofac Surg. 2006;35:990–999. doi: 10.1016/j.ijom.2006.06.018. [DOI] [PubMed] [Google Scholar]
- 11.Metzger M.C., Schön R., Schulze D. Individual preformed titanium meshes for orbital fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2006;102:442–447. doi: 10.1016/j.tripleo.2006.02.031. [DOI] [PubMed] [Google Scholar]
- 15.Jalbert F., Boetto S., Nadon F., Lauwers F., Schmidt E., Lopez R. One-step primary reconstruction for complex craniofacial resection with PEEK custom-made implants. J Craniomaxillofac Surg. 2014;42(2):141–148. doi: 10.1016/j.jcms.2013.04.001. [DOI] [PubMed] [Google Scholar]
- 16.Mustafa S.F., Evans P.L., Bocca A., Patton D.W., Sugar A.W., Baxter P.W. Customized titanium reconstruction of post-traumatic orbital wall defects: a review of 22 cases. Int J Oral Maxillofac Surg. 2011;40:1357–1362. doi: 10.1016/j.ijom.2011.04.020. [DOI] [PubMed] [Google Scholar]
Further reading
Park SW, Choi JW, Koh KS, Oh TS. Mirror-imaged rapid prototype skull model and pre-molded synthetic scaffold to achieve optimal orbital cavity reconstruction. J Oral Maxillofac Surg. 2015; 73: 1540-1553.
Mommaerts MY, Büttner M, Vercruysse H, Wauters L, Beerens M. Orbital wall reconstruction with two-piece puzzle 3D printed implants: technical note Craniomaxillofac. Trauma Reconstr. 2016; 9: (1) 55-61.
Kozakiewicz M, Elgalal M, Loba P, et al. Clinical application of 3D pre-bent titanium implants for orbital floor fractures. J CranioMaxillofac Surg. 2009; 37: 229-234.
Wilde F, Schramm A. Computer-aided reconstruction of the facial skeleton: planning and implementation in clinical routine. HNO. 2016; 64: (9) 641-649.
Fan X, Zhou H, Lin M, Fu Y, Li J. Late reconstruction of the complex orbital fractures with computer-aided design and computer-aided manufacturing Technique. J Craniofac Surg. 2007; 18: (3) 665-673.
Jaquiéry C, Aeppli C, Cornelius P, Palmowsky A, Kunz C, Hammer B. Reconstruction of orbital wall defects: critical review of 72 patients. Int J Oral Maxillofac Surg. 2007; 36: 193-199.
Tang W, Guo L, Long J, Wang H, Lin Y, Liu L, Tian W. Individual design and rapid prototyping in reconstruction of orbital wall defects. J Oral Maxillofac Surg. 2010; 68: 562-570.