Abstract
This paper applies constructs from the Self-Medication Hypothesis and Social Cognitive Theory to explain the development of substance use and psychological distress after a disaster. A conceptual model is proposed, which employs a sequential mediation model, identifying perceived coping self-efficacy, psychological distress, and self-medication as pathways to substance use after a disaster. Disaster exposure decreases perceived coping self-efficacy, which in turn increases psychological distress and subsequently increases perceptions of self-medication in vulnerable individuals. These mechanisms lead to an increase in postdisaster substance use. Last, recommendations are offered to encourage disaster researchers to test more complex models in studies on postdisaster psychological distress and substance use.
Keywords: Disasters, Psychological Distress, Substance use, Self-medication, Social Cognitive Theory, Self-efficacy
Disasters are unexpected events that terrify, horrify or engender substantial losses for many people simultaneously (Norris et al. 2002). As such, disasters are commonly referred to as, “big events,” “community-wide events,” or “collective trauma.” Disasters are further defined by their type, which include, but are not limited to, natural and technological disasters and mass violence. Natural disasters occur from weather or geophysical forces (e.g. hurricanes, earthquakes, and volcanoes). Technological disasters happen because of human negligence or error (e.g. building or bridge collapses, dam or levee failures, nuclear reactor accidents), and mass violence transpires because individuals or groups intend to cause harm to many people (e.g. terrorist attack or mass shooting; Fullerton, Ursano, Norwood, & Holloway, 2003). Disasters, regardless of type, are prospectively linked to numerous behavioral health outcomes, including increased use of tobacco, marijuana, and alcohol (Forman-Hoffman, Riley, and Pici 2005; Flory et al. 2009; North et al. 2011; Parslow and Jorm 2006; Vlahov, Galea, Ahern, Resnick, Boscarino, et al. 2004), and many anxiety and mood disorders, including depression and posttraumatic stress disorder (PTSD; Boscarino, Kirchner, Hoffman, Sartorius, & Adams, 2011; Breslau, Davis, & Schultz, 2003; Fullerton et al., 2013; Nandi, Galea, Ahern, & Vlahov, 2005; Rohrbach, Grana, Vernberg, Sussman, & Sun, 2009; Vetter, Rossegger, Rossler, Bisson, & Endrass, 2008; Walsh et al., 2014).
These postdisaster behavioral and mental health outcomes also affect each other. Evidence suggests that individuals with postdisaster mental disorders smoke more cigarettes and marijuana and drink more alcohol than those without mental health problems (Forman-Hoffman, Riley, and Pici 2005; Flory et al. 2009; North et al. 2011; Parslow and Jorm 2006; Vlahov, Galea, Ahern, Resnick, Boscarino, et al. 2004). Conversely, individuals who engage in postdisaster smoking or drinking, but are without a mental disorder, are more likely to develop mental illness, compared to individuals who do not engage in postdisaster substance use (Van der Velden et al. 2007; Van der Velden, Kleber, and Koenen 2008; Koenen et al. 2005).
Two theories, Self-Medication Hypothesis (SMH) and Social Cognitive Theory (SCT) (Bandura 1989; Khantzian 1985), are frequently discussed to explain postdisaster substance use and mental health problems, but rarely are their assumptions rigorously tested a priori. This paper will highlight and describe the assumptions and primary constructs from the SMH and SCT that can be plausibly tested in disaster studies, while also noting the limitations of these theories for explaining postdisaster substance use and mental health problems. Also, a testable conceptual model, which incorporates constructs from the SMH and Social Cognitive Theory, will be proposed to illustrate the pathways and conditions for postdisaster substance use. Last, recommendations and strategies are offered about how to test complex models for postdisaster substance use and mental health problems.
SELF-MEDICATION HYPOTHESIS (SMH)
The SMH was first introduced by Khantzian, Mack, and Schatzberg in 1974. In their seminal paper, Khantzian et al. (1974) reviewed five case-studies that involved patients addicted to heroin. The authors concluded from their observations and interviews that their clinical patients did not develop methods for dealing with psychological distress, and proposed that chronic heroin use developed to compensate for the lack of “common adaptive mechanisms” (Khantzian et al., 1974, pg. 3). This strategy helped patients cope with challenges of the human condition, such as anxiety, loss, anguish, and sexual frustration. SMH was later expanded to cocaine use, then alcohol, and more recently, has encompassed all forms of drug addiction (Khantzian, 2003).
The SMH has two primary assumptions: (1) psychoactive drugs relieve psychological suffering, and (2) personal preference for a particular substance depends on the psychopharmacological properties of the substance (Khantzian 1997). The second assumption hypothesizes that the choice of drug depends on how well the drug ameliorates affective states the user finds painful or problematic. For example, individuals who experience intense anxiety or fear may use depressants, such as alcohol and marijuana, because of their calming and sedative effects. Conversely, stimulants, such as nicotine and cocaine, because of their energizing properties—improved mood, increased energy, self-esteem, and self-confidence—may appeal to individuals who are avoidant, depressed, or have low self-esteem (Khantzian 2003; Khantzian 1997). This paper focuses only on the first assumption because it offers an explanation for the link between substance use and psychological distress. Readers interested in the second assumption can refer to Khantzian and others (Khantzian 1985; Khantzian 2003; Khantzian 1997; Suh et al. 2008; McKernan et al. 2015).
SMH was established based on case studies using clinical samples, where patients have both severe substance use problems and mental disorders, which limits causal conclusions and generalizability. Outside of clinical settings, however, SMH has gained a significant amount of empirical support. Chilcoat and Breslau (1998) randomly selected 1,200 (ages 21–30) individuals from a 400,000-member health maintenance organization in southeast Michigan to prospectively investigate the causal pathway of PTSD and substance use disorders. At baseline, there were 110 people with a history of drug abuse or dependence and 855 individuals without a history. Among individuals without a history of drug abuse or dependence, having a history of PTSD increased the risk of being diagnosed with a substance abuse or dependence disorder at follow-up (OR=4.4 [95% CI=1.6, 12.0]). Conversely, after adjusting for race, age, sex, and education, there was no significant difference in the incidence of PTSD among individuals with and without a history of substance abuse or dependence. Another study by Taylor et al. (2012) followed a cohort of 627 adolescents for four years and found that baseline unipolar and anxiety disorders predicted the development of substance use disorders at follow-up, but substance use disorders at baseline were not associated with mental disorders at follow-up. Last, Jacobson et al. (2008) analyzed data from the Millennium Cohort Study and found the risk of new-onset heavy weekly drinking (OR=1.63 [CI=1.36, 1.96]), binge drinking (OR=1.46 [CI=1.24, 1.171]), and alcohol-related problems (OR=1.63 [ CI=1.33, 2.01]) were higher among military personnel who deployed and reported combat exposures compared to non-deployed personnel. Other studies also provide evidence for SMH (Crum et al. 2013; Nordløkken, Pape, and Heir 2016; Parslow and Jorm 2006; Boscarino, Adams, and Galea 2006).
Psychological distress seems to precede substance use problems, but the question remains, however, whether these individuals are using drugs to relieve psychological distress (i.e., self-medication). Data from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC), a nationally representative survey of mental illness in community-dwelling adults, suggested that 24.1% of individuals with mood disorders reported using alcohol or drugs to relieve symptoms; 10% of individuals with an anxiety disorder (excluding PTSD) reported self-medicating with alcohol; 3.1% of individuals with an anxiety disorder reported self-medicating with alcohol and drugs; and 21.4% of individuals with PTSD reported using alcohol and other drugs to relieve their psychological symptoms (Leeies et al. 2010; Robinson et al. 2009).
Only data from experimental approaches can discern whether there is a causal relationship between psychological distress and self-medication. Disasters, especially natural disasters and terrorist attacks, can be considered an acute stressful condition, and how participants react in experimental settings could correspond with how individuals respond to disasters. These experiments typically involve exposing participants to acute stressful conditions and offering either a placebo or drug immediately after the exposure. For example, Thomas et al. (2011) randomly assigned participants, who were non-treatment-seeking alcoholics ages 21 thru 65, to a Trier Social Stress Test (TSST)—a standardized procedure for creating moderate psychosocial stress in laboratory settings (Kirschbaum, Pirke, and Hellhammer 1993)—or stress-free condition. Immediately after the task, participants in both groups were primed with an initial dose of their preferred alcoholic beverage. The participants were then asked to participate in a mock taste of two glasses of alcohol, and the primary dependent variables were whether the participant drank all the alcohol available and the total amount of alcohol consumed. Results showed that stressed participants had twice the probability than non-stressed participants (60% vs. 30%) of drinking all the alcohol available. Another study had 17 male and female daily smokers complete a TSST and stress-free task (Childs and de Wit 2010). After each task, participants had repeated opportunities to either smoke or earn money. Results showed that being in the stress condition, compared to the stress-free condition, significantly increased cravings for cigarettes. However, the stress condition did not increase the total number of cigarettes smoked compared to the stress-free condition (Childs and de Wit 2010). Last, de Wit, Soderpalm, Nikolayev, and Young (2003) randomly assigned 37 non-problem social drinkers, ages 21–35, to a placebo or ethanol condition. Each group participated in two tasks; the stress task involved completing a modified version of the TSST, and the stress-free task involved conversing with a technician for 10 minutes. Immediately after each condition, participants provided a saliva sample to measure cortisol levels and were asked how distressed they felt using questions from the Visual Analogue Scale. Participants were then given a beverage containing either ethanol or the placebo, and over the next 30 minutes, participants were offered up to six additional drinks. At the end of the session participants again provided a saliva sample to measure cortisol levels, and were asked how distressed they felt. Contrary to their hypothesis (i.e., social stress would increase consumption of ethanol but not placebo beverage) results showed that participants in both groups consumed more drinks after the stressful condition than the stress-free condition. Also, among participants in the ethanol group, stressful conditions increased anxiety, uneasiness, and weakened some of the acute subjective effects of ethanol (i.e., self-reported feelings of cheerfulness, focus, outgoingness, and drowsiness), however, these changes in subjective states did not correspond with a change in alcohol consumption.
Findings from experimental studies are mixed; stressful conditions increase the desire and craving to drink or smoke and subjective states of being (McRae-Clark et al. 2011; Childs and de Wit 2010), but these subjective feelings do not consistently predict increased substance consumption. Therefore, exposure to stressful conditions may not predispose individuals to more substance use but instead may place the body or mind in a heightened state of arousal, and the individual may select from an assortment of behavior, including substance use, or other strategies, to restore homeostasis. Healthier individuals may not respond to stressful situations by using drugs, whereas those with a history of substance use and or mental health disorders, may react to stressful conditions by administering more drugs (Abrams et al. 2002; Gordh, Brkic, and Söderpalm 2011). For individuals with a history of substance use or mental health problems, drug use may be an established or salient response to stressful conditions (i.e., self-medication). This may explain why healthy individuals, those without prior substance use and mental health problems and or postdisaster mental health problems, report few or no substance use problems after disasters, while those with substance use and mental health histories report the most problems (Breslau, Davis, and Schultz 2003; North et al. 2011; Cerda et al. 2008; Nordløkken, Pape, and Heir 2016; Parslow and Jorm 2006).
Postdisaster substance use can be interpreted as a self-medication strategy in which drugs are used to cope with psychological distress caused by disaster exposure. However, given that the stress-inducing effects of disasters cannot be measured in experimental settings, it is important that perceptions of self-medication be measured in disaster studies to determine if changes in perceptions of self-medication are also associated with changes in postdisaster substance use. The act of self-medicating may itself be influenced by a lack of perceived coping self-efficacy (Cinciripini et al. 2003; Engels et al. 2005; Skutle 1999)—beliefs that one can deal with physical, cognitive and emotional demands of stressors (Sandler et al. 2000), which would embed SMH within the broader context of Bandura’s Social Cognitive Theory.
SOCIAL COGNITIVE THEORY (SCT)
Unlike SMH, which is focused primarily on individual-level determinants, SCT acknowledges that environmental factors influence individuals and groups, and conversely, individuals and groups influence environmental factors (i.e. reciprocal determinism; Bandura, 1978, 1989). SCT places behavior within the social context; behaviors are learned and maintained by observing others perform the behavior and observing the consequences of that behavior (Bandura 2004; Bandura 1978; Bandura 1989). These experiences are stored in memory and reenacted. Bandura theorized that these cognitive-related tasks of observing, encoding, and re-enacting behavior were central to human learning and motivation. Self-efficacy, reflecting personal beliefs about the ability to perform behaviors that bring about desired outcomes, was identified as the central cognitive mechanism that influenced whether the behavior was initiated and maintained (Bandura 1977; Bandura 1982). Collective efficacy, reflecting beliefs about the ability of a group to perform concerted actions that bring desired outcomes, was added to address how people work together in communities, organizations, and political institutions to create safe and orderly spaces (Bandura 2000).
Individuals exposed to a disaster have to manage their functioning and the environmental burdens caused by it, and the ability to do this has been broadly referred to as perceived coping self-efficacy (henceforth self-efficacy; Benight & Bandura, 2004). Though disasters are considered traumatic events, it is the individual who appraises the magnitude of threat inherent in the event, and beliefs about self-efficacy affect how disasters are interpreted. However, this appraisal process occurs alongside the body’s natural physiological response to traumatic events. Sudden sweating, heart palpitations, and aches and pains, which are common physiological responses to traumatic events, can be interpreted by individuals as not coping well with the traumatic event thus decreasing self-efficacy. Further, disasters frequently directly or indirectly result in the death of close family members and friends or destroy property and communities, and the loss of loved ones and resources can be additional sources of stress as well as diminish the capacity of individuals to function and manage themselves after being exposed to disasters (Benight et al. 1999; Hobfoll 1989).
Low self-efficacy may produce more psychological distress because individuals feel they are unable to control themselves or their surroundings (Benight and Bandura 2004). Indeed, research has shown that self-efficacy is negatively associated with psychological distress after a disaster. A systematic review of 27 cross-sectional and prospective studies of adult and adolescent survivors of collective trauma (i.e. disasters) addressing the relationship between self-efficacy and psychological outcomes found medium to large effects of self-efficacy on general distress (weighted average correlation [r] = −.50) and severity and frequency of PTSD (r = −.36 and r = −.77, respectively). Reviewing only the prospective studies produced a larger effect size for PTSD symptom severity (r= −.62) and general distress (r = −.55; Luszczynska, Benight, & Cieslak, 2009).
Self-efficacy could also buffer or protect against psychological distress. Prati, Pietrantoni, and Cicognani (2010) recruited 451 rescue workers (firefighters, paramedics, and medical technicians), and asked how stressful was their last most difficult emergency call (i.e., stress appraisal). Rescue workers answered questions about how well they emotionally responded to emergency calls, which addressed job burnout, compassion satisfaction (i.e., positive feelings a person derives from helping others), and compassion fatigue (i.e., indifference to suffering), and rated their perceived self-efficacy. Results showed that stress appraisal was positively associated with compassion fatigue, compassion satisfaction, and burnout. Also, self-efficacy was positively related to compassion satisfaction, and negatively related to compassion fatigue and burnout. However, there were significant interactions between stress appraisal and self-efficacy for compassion satisfaction, compassion fatigue, and burnout. These interactions were decomposed, and the authors found that stress appraisal was associated with compassion satisfaction, burnout, and compassion fatigue for rescue workers with low self-efficacy but not in rescue workers with high self-efficacy. These results suggested that the rescue workers with high self-efficacy were less affected by high-stress conditions in comparison with rescue workers with low self-efficacy. Therefore, self-efficacy could function as a determinant, mechanism, and moderator of psychological distress.
Disasters affect the well-being of not only individuals, but organizations, neighborhoods, and communities. Proper mobilization and allocation of scarce resources after disasters require that communities, not individuals, are sufficiently prepared to handle the environmental demands of disasters. Communities with collective efficacy perceive they can respond to disasters by strategically mobilizing and allocating resources, and repairing damaged infrastructure (Norris et al. 2008). Two studies by Ursano et al. (2014) and Fullerton et al. (2015) examined the effect of perceived collective efficacy and community collective efficacy—measured using zip codes to define community units—on PTSD and depression outcomes using a cross-sectional random sample of 2249 public health workers exposed to the 2004 Florida Hurricane sample. After controlling for sociodemographics, community socioeconomic characteristics, personal injury/damage, and community storm damage perceived collective self-efficacy and community collective efficacy were negatively associated with PTSD symptom severity. The authors also examined the odds of having probable PTSD, and found that each point increase in individual-level collective efficacy decreased the odds of PTSD by 6% (CI=0.92, 0.97), and each point increase in community-level collective efficacy decreased the odds of PTSD by 7% (CI=0.88, 0.98). Similar findings emerged for depression; community-level and individual-level collective efficacy were negatively associated with depressive symptom severity (β= −0.09 [CI=−0.13, −0.04] and β= −0.09 [CI=−0.12, −0.06], respectively), even after controlling for the same variables mentioned previously. More studies have documented the importance of collective efficacy as a correlate of postdisaster psychological distress (Benight 2004; Lowe et al. 2015), and similar to self-efficacy, this construct also may function as a determinant, mechanism, and moderator of psychological distress.
Although self-efficacy and collective efficacy have demonstrable effects on postdisaster psychological distress, little information is available for postdisaster substance use. Self-efficacy and collective efficacy are likely associated with post-disaster substance use because these constructs are related to psychological distress, and psychological distress is related to postdisaster substance use. Self-efficacy and collective efficacy could be common causes of postdisaster psychological distress and substance use or could act as mediators and moderators of the psychological distress and substance use relationship. The importance of producing evidence of an association cannot be understated, given that self-efficacy is one of the most used constructs for promoting behavior change (Strecher et al. 1986). If self-efficacy and collective efficacy are shown to affect psychological distress and substance use, then pre-and postdisaster interventions can be developed to reduce postdisaster psychological distress and substance use either through improved self-efficacy or collective efficacy. Therefore, going forward, disaster researchers should include measures for collective efficacy and self-efficacy, alongside the commonly used measures for mental disorders to better understand the mechanisms behind postdisaster substance use.
UNIFYING THE SELF-MEDICATION HYPOTHESIS AND SOCIAL COGNITIVE THEORY
SMH does not address the origins of psychological distress, and although SCT can explain the origins of psychological distress and substance use, few studies have applied constructs from SCT to postdisaster substance use. Therefore, these theories can be integrated to help explain the strong relation between postdisaster substance use and psychological distress.
Self-medication, the act of using substances to relieve symptoms of psychological distress (Khantzian 1997), can occur after exposure to stressful conditions. If self-medication develops in the absence of more adaptive methods of coping and responding to stressful demands, then self-efficacy and collective efficacy may play pivotal roles in determining whether self-medication behavior is initiated and or maintained after exposure to a disaster. Therefore, the conceptual model presented in Figure 1 describes the relations between these variables. This conceptual model illustrates a complex sequential mediation pathway (X→M1→M2→M3→Y). Specifically, the effect of disaster exposure on substance use is hypothesized to be mediated through self-efficacy, psychological distress, and perceptions of self-medication in that sequential order. Disaster exposure decreases self-efficacy, which in turn increases psychological distress, which subsequently increases perceptions of self-medication, which increases postdisaster substance use. This complex mediation model can be decomposed into simpler sequential mediation models (X→M1→M2→Y, X→M1→M3→Y, or X→M2→M3→Y), and even simple mediation models that examine self-efficacy (X→M1→Y), psychological distress (X→M2→Y), and self-medication (X→M3→Y) separately as pathways to substance use after disaster exposure. This model can be further simplified to direct effects only (X→Y). For example, many studies report that disaster exposure increases the risk for postdisaster substance (Fullerton et al. 2013; Parslow and Jorm 2006; Rohrbach et al. 2009; Vlahov et al. 2002; Vlahov, Galea, Ahern, Resnick, Boscarino, et al. 2004; Vlahov, Galea, Ahern, Resnick, and Kilpatrick 2004), but these simpler paths may be less beneficial if the goal is to have a greater understanding of the mechanisms of postdisaster increase in substance use. However, given the amount of data required to test the full model, it may be prudent to test the less complex pathways first to see if there is evidence of mediation before testing the entire model.
Figure 1.
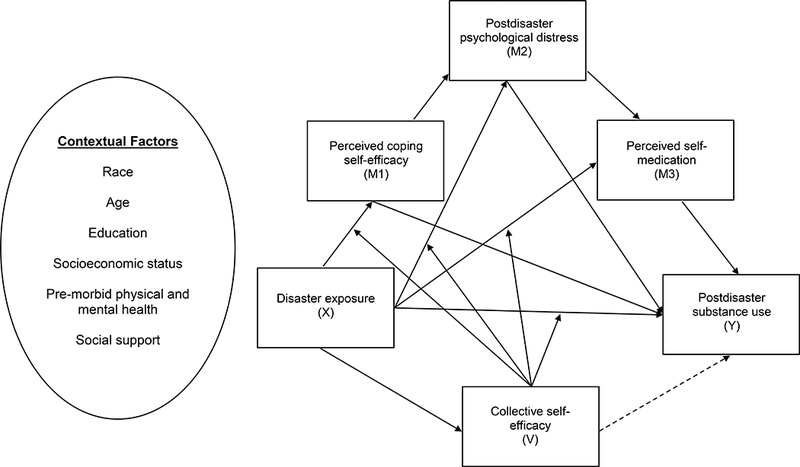
A conceptual diagram of a conditional process model illustrating the conditional effects of disaster exposure on substance use (e.g. cigarettes, alcohol, and marijuana). The focus of this model is complex sequential mediation pathway (X→M1→M2→M3→Y). The effect of disaster exposure on substance use is mediated through perceived-coping self-efficacy, psychological distress, and self-medication in that sequential order. Collective efficacy acts as a buffer against the deleterious effects of disaster exposure. Specifically, collective efficacy protects against the harmful effects disaster exposure has on self-efficacy, psychological distress, self-medication, and substance use. If collective efficacy is measured after the disaster, it could also serve as another pathway to substance use (as denoted by the dotted line). Contextual factors, such as social support and socioeconomic status, can be used to identify differences in perceived coping self-efficacy among sub-groups and vulnerable populations who are at an increased risk for postdisaster psychological distress, feelings of self-medication, and postdisaster substance use. Further contextual factors can be included as confounders to improve the estimation of causal direct and indirect pathways.
Collective efficacy protects against the deleterious effects disaster exposure has on self-efficacy, psychological distress, perceived self-medication, and substance use. If collective efficacy is measured during the disaster, it could also serve as another pathway to substance use. Last, contextual factors, such as social support and socioeconomic status, can be used to identify differences in perceived coping self-efficacy among sub-groups and vulnerable populations who are at an increased risk for postdisaster psychological distress and substance use. Further contextual factors could be included as confounders to improve the estimation of causal direct and indirect pathways. Preferably contextual factors should be independent of or at least measured before disaster exposure to ensure that these factors themselves are not influenced by disaster exposure.
This proposed conceptual model represents only some of the many possible pathways that could lead to postdisaster substance use. There are many other conceptual models that complement or run counter to the one proposed. For example, Hobfoll’s Conservation of Resources model proposes that stress results from the loss or the threat of loss of resources, or the lack of resource gain after the investment of resources (Hobfoll 1989). Hobfoll’s model complements the model proposed here because resource loss may be the primary “catalyst” (Benight et al. 1999, pg. 2447) that decreases perceived coping self-efficacy. However, our model proposes that postdisaster substance use is used to alleviate psychological distress and not necessarily resource loss, though research does support the association of resource loss with substance use (Cerdá, Tracy, and Galea 2011; Kishore et al. 2008). Emotional regulation, which is the process of monitoring, evaluating, and modifying emotional reactions (Thompson 1991), is also another important factor to consider. Individuals with adaptive emotional regulation strategies, such as positive refocusing and reappraisal, may maintain high levels of coping self-efficacy after disaster exposure compared to individuals with less adaptive emotional regulation strategies, such as rumination and catastrophizing (Thompson 1991; Garnefski, Kraaij, and Spinhoven 2001). However, like resource loss, postdisaster substance use is not used to cope with poor emotional regulation strategies. Instead, postdisaster substance use is a behavioral strategy to treat symptoms of psychological distress (i.e. self-medication). Researchers are encouraged to compare these models empirically to determine which model best predicts postdisaster substance use.
This proposed model is not hypothesizing a complete mediation of the effect disaster exposure has on postdisaster substance use. On the contrary, after quantifying the proposed indirect pathways, a direct effect of disaster exposure on postdisaster substance use may remain, especially if the magnitude of disaster exposure (i.e. disaster severity) is measured. Certain statistical analyses, such as structural equation modeling (SEM), allow researchers to test competing models to determine which model best fits or explains the data (Tomarken and Waller 2005). If hypotheses and variable relations are defined a priori, then disaster researchers will have the information available to build these complex models and test them against the data to see which model best explains postdisaster substance use.
RECOMMENDATIONS AND CONCLUSION
Disaster researchers have identified several key determinants for postdisaster substance use and psychological distress, yet rarely are these factors explored more deeply to uncover the mechanisms of action. Take for example disaster severity: the evidence is nearly consistent that the magnitude of disaster exposure is associated with psychological distress and substance use (Fullerton et al. 2013; Parslow and Jorm 2006; Rohrbach et al. 2009; Vlahov et al. 2002; Vlahov, Galea, Ahern, Resnick, Boscarino, et al. 2004; Vlahov, Galea, Ahern, Resnick, and Kilpatrick 2004), yet there is almost no evidence illustrating the mechanisms of action. This paper represents a step forward because it presents a case for multiple pathways leading to postdisaster psychological distress and substance, and if shown to be efficacious, could lead to a better understanding of increased postdisaster substance consumption. However, research in this area may benefit from additional steps, and three recommendations are offered.
1. Incorporate constructs from psychosocial theories into research on postdisaster substance use.
There needs to be a greater effort for including constructs from psychosocial theories when investigating postdisaster substance use. For example, though self-medication is mentioned as a plausible explanation for finding an increase in substance use after a disaster, rarely is there a measure for self-medication included in the study; researchers should include questions that measure perceptions of self-medication. Many national surveys on drug and alcohol abuse include a question that measures self-medication (Leeies et al. 2010; Bolton, Robinson, and Sareen 2009; Crum et al. 2013). This question could be modified to match the circumstances of the disaster under study. Including constructs from psychosocial theories will improve our understanding of postdisaster substance use, and will also provide opportunities to develop theoretically informed interventions.
2. Think about moderators and mediators during the planning phase of the study.
Researchers should consider potential mediators and moderators during the planning phase of disaster research, especially if proposed outcomes are psychological distress or substance use. To test mediation and moderation rigorously, researchers should also use prospective designs and collect at least three waves of data. Multiple waves of data would allow researchers to evaluate how changes in the specified mediator corresponded with changes in the chosen outcome variable. This method for testing mediation is preferable over cross-sectional or prospective designs with only two waves of data collection (Maxwell and Cole 2007). Also, potential moderators and mediators should be theoretically relevant but should also adhere to the rules of moderation and mediation (Baron and Kenny 1986). Regarding moderation, a moderator cannot be causally associated with the exposure variable. This assumption can be met by defining moderators as variables that can be ascertained before the disaster, such as socioeconomic status or neighborhood characteristics. Including variables that are plausibly affected by disaster exposure as interactions may still be theoretically beneficial. For example, a person’s self-efficacy may be altered by disaster exposure, but this variable could be considered a moderator because self-efficacy can be measured outside of the disaster context. In this manner, post-disaster self-efficacy is regarded as a proxy measure for pre-disaster self-efficacy, but the findings should be interpreted in light of these methodological limitations. Regarding mediation, disaster exposure should causally affect the potential mediator, and the mediator should causally affect the outcome. Potential mediators could be the ones outlined in this study or could be other postdisaster determinants of health, such as social support or access to health services.
3. Adopt more complex analytical strategies for assessing postdisaster substance use.
The Baron-Kenny approach to mediation (Baron and Kenny 1986) has been heavily criticized for not quantifying nor testing indirect effects (Hayes 2009), among many other concerns (Zhao, Lynch, and Chen 2010). Also, including multiplicative interactions terms, especially interactions that involve two continuous variables, in regression models without decomposing the interactions will be of little interpretive value. Researchers should use the PROCESS (Hayes 2013) macro or SEM packages (Muthen and Muthen 2010) to address questions of mediation and moderation. These packages offer useful tools for quantifying and testing indirect effects and testing and decomposing interactions. SEM also provides many tools for testing alternative models for the data which is useful for researchers attempting to develop better explanatory and predictive models for postdisaster psychological distress and substance use.
Self-medication, self-efficacy, and collective efficacy may be important determinants, mediators, and moderators for postdisaster psychological distress and substance use. By following the suggestions and recommendations in this paper, researchers can begin to test theories apriori and uncover new explanations for postdisaster substance use. This new knowledge will help improve our understanding of the etiology of postdisaster substance consumption, which would benefit the world economically and socially because health care professionals are ever more frequently responding to the behavioral health consequences of disasters worldwide.
ACKNOWLEDGEMENTS
None
FUNDING
The study was supported by a National Institute on Drug Abuse grant (1 R21 DA021782–01, K. Ward, PI).
REFERENCES
- Abrams Kenneth, Kushner Matt G., Medina Krista Lisdahl, and Voight Amanda. 2002. “Self-Administration of Alcohol before and after a Public Speaking Challenge by Individuals with Social Phobia.” Psychology of Addictive Behaviors 16 (2): 121–28. doi: 10.1037//0893-164X.16.2.121. [DOI] [PubMed] [Google Scholar]
- Bandura Albert. 1977. “Self-Efficacy: Toward a Unifying Theory of Behavioral Change.” Psychological Review 84 (2): 191–215. doi: 10.1037/0033-295X.84.2.191. [DOI] [PubMed] [Google Scholar]
- Bandura A 1978. “The Self System in Reciprocal Determinism.” American Psychologist 33 (4): 344–58. doi: 10.1037/0003-066X.33.4.344. [DOI] [Google Scholar]
- Bandura A 1982. “Self-Efficacy Mechanism in Human Agency.” American Psychologist 37 (2): 122–47. doi: 10.1037/0003-066X.37.2.122. [DOI] [Google Scholar]
- Bandura A 1989. “Human Agency in Social Cognitive Theory.” The American Psychologist 44 (9): 1175–84. doi: 10.1037/0003-066x.44.9.1175. [DOI] [PubMed] [Google Scholar]
- Bandura A 2000. “Exercise of Human Agency Through Collective Efficacy.” Current Directions in Psychological Science 9 (3): 75–78. doi: 10.1111/1467-8721.00064. [DOI] [Google Scholar]
- Bandura A 2004. “Health Promotion by Social Cognitive Means.” Health Education & Behavior 31 (2): 143–64. doi: 10.1177/1090198104263660. [DOI] [PubMed] [Google Scholar]
- Baron R, and Kenny D. 1986. “The Moderator-Mediator Variable Distinction in Social Psychological Research: Conceptual, Strategic, and Statistical Considerations.” Journal of Personality and Social Psychology 51 (6): 1173–82. doi: 10.1037/0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Benight Charles C. 2004. “Collective Efficacy Following a Series of Natural Disasters.” Anxiety, Stress & Coping 17 (4): 401–20. doi: 10.1080/10615800512331328768. [DOI] [Google Scholar]
- Benight Charles C., and Bandura Albert. 2004. “Social Cognitive Theory of Posttraumatic Recovery: The Role of Perceived Self-Efficacy.” Behaviour Research and Therapy 42 (10): 1129–48. doi: 10.1016/j.brat.2003.08.008. [DOI] [PubMed] [Google Scholar]
- Benight Charles C., Swift Erika, Sanger Jean, Smith Anne, and Zeppelin Dan. 1999. “Coping Self-Efficacy as a Mediator of Distress Following a Natural Disaster.” Journal of Applied Social Psychology 29 (12): 2443–64. doi: 10.1111/j.1559-1816.1999.tb00120.x. [DOI] [Google Scholar]
- Bolton James M., Robinson Jennifer, and Sareen Jitender. 2009. “Self-Medication of Mood Disorders with Alcohol and Drugs in the National Epidemiologic Survey on Alcohol and Related Conditions.” Journal of Affective Disorders 115 (3). Elsevier B.V.: 367–75. doi: 10.1016/j.jad.2008.10.003. [DOI] [PubMed] [Google Scholar]
- Boscarino Joseph A., Adams Richard E., and Galea Sandro. 2006. “Alcohol Use in New York after the Terrorist Attacks: A Study of the Effects of Psychological Trauma on Drinking Behavior.” Addictive Behaviors 31 (4): 606–21. doi: 10.1016/j.addbeh.2005.05.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boscarino Joseph A., Kirchner H. Lester, Hoffman Stuart N., Sartorius Jennifer, and Adams Richard E.. 2011. “PTSD and Alcohol Use after the World Trade Center Attacks: A Longitudinal Study.” Journal of Traumatic Stress 24 (5): 515–25. doi: 10.1002/jts.20673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breslau Naomi, Davis Glenn C, and Schultz Lonni R. 2003. “Posttraumatic Stress Disorder and the Incidence of Nicotine, Alcohol, and Other Drug Disorders in Persons Who Have Experienced Trauma.” Archives of General Psychiatry 60 (3): 289–94. http://www.ncbi.nlm.nih.gov/pubmed/12622662. [DOI] [PubMed] [Google Scholar]
- Cerdá Magdalena, Tracy Melissa, and Galea Sandro. 2011. “A Prospective Population Based Study of Changes in Alcohol Use and Binge Drinking after a Mass Traumatic Event.” Drug and Alcohol Dependence 115 (1–2): 1–8. doi: 10.1016/j.drugalcdep.2010.09.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerda Magdalena, Vlahov David, Tracy Melissa, and Galea Sandro. 2008. “Alcohol Use Trajectories among Adults in an Urban Area after a Disaster: Evidence from a Population-Based Cohort Study.” Addiction 103 (8): 1296–1307. doi: 10.1111/j.1360-0443.2008.02247.x. [DOI] [PubMed] [Google Scholar]
- Chilcoat Howard D., and Breslau Naomi. 1998. “Investigations of Causal Pathways between PTSD and Drug Use Disorders.” Addictive Behaviors 23 (6): 827–40. doi: 10.1016/S0306-4603(98)00069-0. [DOI] [PubMed] [Google Scholar]
- Childs E, and de Wit H. 2010. “Effects of Acute Psychosocial Stress on Cigarette Craving and Smoking.” Nicotine & Tobacco Research 12 (4): 449–53. doi: 10.1093/ntr/ntp214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cinciripini Paul M., Wetter David W., Fouladi Rachel T., Blalock Janice A., Carter Brian L., Cinciripini Lynn G., and Baile Walter F.. 2003. “The Effects of Depressed Mood on Smoking Cessation: Mediation by Postcessation Self-Efficacy.” Journal of Consulting and Clinical Psychology 71 (2): 292–301. doi: 10.1037/0022-006X.71.2.292. [DOI] [PubMed] [Google Scholar]
- Crum Rosa M, Mojtabai Ramin, Lazareck Samuel, Bolton James M, Robinson Jennifer, Sareen Jitender, Green Kerry M, et al. 2013. “A Prospective Assessment of Reports of Drinking to Self-Medicate Mood Symptoms with the Incidence and Persistence of Alcohol Dependence.” JAMA Psychiatry 70 (7): 718–26. doi: 10.1001/jamapsychiatry.2013.1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Wit Harriet, Soderpalm Anna H. V., Nikolayev Lilia, and Young Elizabeth. 2003. “Effects of Acute Social Stress on Alcohol Consumption in Healthy Subjects.” Alcoholism: Clinical & Experimental Research 27 (8): 1270–77. doi: 10.1097/01.ALC.0000081617.37539.D6. [DOI] [PubMed] [Google Scholar]
- Engels Rutger C. M. E., Hale William W., Noom Marc, and de Vries Hein. 2005. “Self-Efficacy and Emotional Adjustment as Precursors of Smoking in Early Adolescence.” Substance Use & Misuse 40 (12): 1883–93. doi: 10.1080/10826080500259612. [DOI] [PubMed] [Google Scholar]
- Flory Kate, Hankin Benjamin L., Kloos Bret, Cheely Catherine, and Turecki Gustavo. 2009. “Alcohol and Cigarette Use and Misuse Among Hurricane Katrina Survivors: Psychosocial Risk and Protective Factors.” Substance Use & Misuse 44 (12): 1711–24. doi: 10.3109/10826080902962128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Forman-Hoffman Valerie, Riley William, and Pici Melissa. 2005. “Acute Impact of the September 11 Tragedy on Smoking and Early Relapse Rates among Smokers Attempting to Quit.” Psychology of Addictive Behaviors 19 (3): 277–83. doi: 10.1037/0893-164X.19.3.277. [DOI] [PubMed] [Google Scholar]
- Fullerton Carol S., McKibben Jodi B.A., Reissman Dori B., Scharf Ted, Kowalski-Trakofler Kathleen M., Shultz James M., and Ursano Robert J.. 2013. “Posttraumatic Stress Disorder, Depression, and Alcohol and Tobacco Use in Public Health Workers After the 2004 Florida Hurricanes.” Disaster Medicine and Public Health Preparedness 7 (1): 89–95. doi: 10.1017/dmp.2013.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fullerton Carol S., Ursano Robert J., Liu Xian, McKibben Jodi B. A., Wang Leming, and Reissman Dori B.. 2015. “Depressive Symptom Severity and Community Collective Efficacy Following the 2004 Florida Hurricanes.” PLOS ONE 10 (6): e0130863. doi: 10.1371/journal.pone.0130863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fullerton Carol S, Ursano Robert J, Norwood Ann E, and Holloway Harry H. 2003. “Trauma, Terrorism, and Disaster” In Terrorism and Disaster: Individual and Community Mental Health Interventions, edited by Ursano Robert J., Fullerton Carol S., and Norwood Ann E, 1–23. New York, New York: Cambridge University Press. [Google Scholar]
- Garnefski N, Kraaij V, and Spinhoven P. 2001. “Negative Life Events, Cognitive Emotion Regulation and Emotional Problems.” Personality & Individual Differences 30 (8): 1311–27. [Google Scholar]
- Gordh Anna H.V. Söderpalm, Brkic Sejla, and Söderpalm Bo. 2011. “Stress and Consumption of Alcohol in Humans with a Type 1 Family History of Alcoholism in an Experimental Laboratory Setting.” Pharmacology Biochemistry and Behavior 99 (4): 696–703. doi: 10.1016/j.pbb.2011.05.028. [DOI] [PubMed] [Google Scholar]
- Hayes Andrew F. 2009. “Beyond Baron and Kenny: Statistical Mediation Analysis in the New Millennium.” Communication Monographs 76 (4): 408–20. doi: 10.1080/03637750903310360. [DOI] [Google Scholar]
- Hayes Andrew F. 2013. Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach. First. New York: Guilford Press. [Google Scholar]
- Hobfoll SE 1989. “Conservation of Resources. A New Attempt at Conceptualizing Stress.” The American Psychologist 44 (3): 513–24. http://www.ncbi.nlm.nih.gov/pubmed/2648906. [DOI] [PubMed] [Google Scholar]
- Jacobson Isabel G, Ryan Margaret A K, Hooper Tomoko I, Smith Tyler C, Amoroso Paul J, Boyko Edward J, Gackstetter Gary D, Wells Timothy S, and Bell Nicole S. 2008. “Alcohol Use and Alcohol-Related Problems before and after Military Combat Deployment.” JAMA 300 (6): 663–75. doi: 10.1001/jama.300.6.663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khantzian EJ 1985. “The Self-Medication Hypothesis of Addictive Disorders: Focus on Heroin and Cocaine Dependence.” The American Journal of P 142 (11): 1259–64. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ 1997. “The Self-Medication Hypothesis of Substance Use Disorders: A Reconsideration and Recent Applications.” Harvard Review of Psychiatry 4 (5): 231–44. doi: 10.3109/10673229709030550. [DOI] [PubMed] [Google Scholar]
- Khantzian EJ 2003. “Understanding Addictive Vulnerability: An Evolving Psychodynamic Perspective.” Neuro-Psychoanalysis 5 (1): 5–21. doi: 10.1080/15294145.2003.10773403. [DOI] [Google Scholar]
- Khantzian EJ, Mack JF, and Schatzberg AF. 1974. “Heroin Use as an Attempt To Cope: Clinical Observations.” American Journal of Psychiatry 131 (2): 160–64. doi: 10.1176/ajp.131.2.160. [DOI] [PubMed] [Google Scholar]
- Kirschbaum Clemens, Pirke Karl-Martin, and Hellhammer Dirk H.. 1993. “The ‘Trier Social Stress Test’ – A Tool for Investigating Psychobiological Stress Responses in a Laboratory Setting.” Neuropsychobiology 28 (1–2): 76–81. doi: 10.1159/000119004. [DOI] [PubMed] [Google Scholar]
- Kishore Vimal, Katherine P Theall William Robinson, Pichon Jamilia, Scribner Richard, Roberson Emily, and Johnson Sandy. 2008. “Resource Loss, Coping, Alcohol Use, and Posttraumatic Stress Symptoms among Survivors of Hurricane Katrina: A Cross-Sectional Study.” American Journal of Disaster Medicine 3 (6): 345–57. http://www.ncbi.nlm.nih.gov/pubmed/19202888. [PubMed] [Google Scholar]
- Koenen KC, Hitsman B, Lyons MJ, Niaura R, McCaffery J, Goldberg J, Eisen SA, True W, and Tsuang M. 2005. “A Twin Registry Study of the Relationship between Posttraumatic Stress Disorder and Nicotine Dependence in Men.” Arch Gen Psychiatry 62 (11): 1258–65. doi: 10.1001/archpsyc.62.11.1258. [DOI] [PubMed] [Google Scholar]
- Leeies Murdoch, Pagura Jina, Sareen Jitender, and Bolton James M.. 2010. “The Use of Alcohol and Drugs to Self-Medicate Symptoms of Posttraumatic Stress Disorder.” Depression and Anxiety 27 (8): 731–36. doi: 10.1002/da.20677. [DOI] [PubMed] [Google Scholar]
- Lowe Sarah R., Sampson Laura, Gruebner Oliver, and Galea Sandro. 2015. “Psychological Resilience after Hurricane Sandy: The Influence of Individual- and Community-Level Factors on Mental Health after a Large-Scale Natural Disaster.” Edited by Chao Linda. PLOS ONE 10 (5): e0125761. doi: 10.1371/journal.pone.0125761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Luszczynska Aleksandra, Benight Charles C., and Cieslak Roman. 2009. “Self-Efficacy and Health-Related Outcomes of Collective Trauma.” European Psychologist 14 (1): 51–62. doi: 10.1027/1016-9040.14.1.51. [DOI] [Google Scholar]
- Maxwell Scott E., and Cole David A.. 2007. “Bias in Cross-Sectional Analyses of Longitudinal Mediation.” Psychological Methods 12 (1): 23–44. doi: 10.1037/1082-989X.12.1.23. [DOI] [PubMed] [Google Scholar]
- McKernan Lindsey Colman, Nash Michael R., Gottdiener William H., Anderson Scott E., Lambert Warren E., and Carr Erika R.. 2015. “Further Evidence of Self-Medication: Personality Factors Influencing Drug Choice in Substance Use Disorders.” Psychodynamic Psychiatry 43 (2): 243–75. doi: 10.1521/pdps.2015.43.2.243. [DOI] [PubMed] [Google Scholar]
- McRae-Clark Aimee L., Carter Rickey E., Price Kimber L., Baker Nathaniel L., Thomas Suzanne, Saladin Michael E., Giarla Kathleen, Nicholas Katherine, and Brady Kathleen T.. 2011. “Stress- and Cue-Elicited Craving and Reactivity in Marijuana-Dependent Individuals.” Psychopharmacology 218 (1): 49–58. doi: 10.1007/s00213-011-2376-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthen LK, and Muthen BO. 2010. Mplus User’s Guide. Sixth Los Angeles, CA: Muthén & Muthén. [Google Scholar]
- Nandi A, Galea S, Ahern J, and Vlahov D. 2005. “Probable Cigarette Dependence, PTSD, and Depression after an Urban Disaster: Results from a Population Survey of New York City Residents 4 Months after September 11, 2001.” Psychiatry 68 (4): 299–310. doi: 10.1521/psyc.2005.68.4.299. [DOI] [PubMed] [Google Scholar]
- Nordløkken A, Pape H, and Heir T. 2016. “Alcohol Consumption in the Aftermath of a Natural Disaster: A Longitudinal Study” Public Health 132 Elsevier Ltd: 33–39. doi: 10.1016/j.puhe.2015.11.007. [DOI] [PubMed] [Google Scholar]
- Norris Fran H., Stevens Susan P., Pfefferbaum Betty, Wyche Karen F., and Pfefferbaum Rose L.. 2008. “Community Resilience as a Metaphor, Theory, Set of Capacities, and Strategy for Disaster Readiness.” American Journal of Community Psychology 41 (1–2): 127–50. doi: 10.1007/s10464-007-9156-6. [DOI] [PubMed] [Google Scholar]
- Norris Fran H, Friedman Matthew J, Watson Patricia J, Byrne Christopher M, Diaz Eolia, and Kaniasty Krzysztof. 2002. “60,000 Disaster Victims Speak: Part I. An Empirical Review of the Empirical Literature, 1981–2001.” Psychiatry 65 (3): 207–39. [DOI] [PubMed] [Google Scholar]
- North Carol S, Ringwalt Christopher L, Downs Dana, Derzon Jim, and Galvin Deborah. 2011. “Postdisaster Course of Alcohol Use Disorders in Systematically Studied Survivors of 10 Disasters.” Archives of General Psychiatry 68 (2): 173–80. doi: 10.1001/archgenpsychiatry.2010.131. [DOI] [PubMed] [Google Scholar]
- Parslow Ruth A., and Jorm Anthony F.. 2006. “Tobacco Use after Experiencing a Major Natural Disaster: Analysis of a Longitudinal Study of 2063 Young Adults.” Addiction 101 (7): 1044–50. doi: 10.1111/j.1360-0443.2006.01481.x. [DOI] [PubMed] [Google Scholar]
- Prati Gabriele, Pietrantoni Luca, and Cicognani Elvira. 2010. “Self-Efficacy Moderates the Relationship between Stress Appraisal and Quality of Life among Rescue Workers.” Anxiety, Stress & Coping 23 (4): 463–70. doi: 10.1080/10615800903431699. [DOI] [PubMed] [Google Scholar]
- Robinson Jennifer, Sareen Jitender, Cox Brian J., and Bolton James. 2009. “Self-Medication of Anxiety Disorders with Alcohol and Drugs: Results from a Nationally Representative Sample.” Journal of Anxiety Disorders 23 (1): 38–45. doi: 10.1016/j.janxdis.2008.03.013. [DOI] [PubMed] [Google Scholar]
- Rohrbach Louise A., Grana Rachel, Vernberg Eric, Sussman Steve, and Sun Ping. 2009. “Impact of Hurricane Rita on Adolescent Substance Use.” Psychiatry: Interpersonal and Biological Processes 72 (3): 222–37. doi: 10.1521/psyc.2009.72.3.222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandler Irwin N., Tein Jenn-Yun, Mehta Paras, Wolchik Sharlene, and Ayers Tim. 2000. “Coping Efficacy and Psychological Problems of Children of Divorce.” Child Development 71 (4): 1099–1118. doi: 10.1111/1467-8624.00212. [DOI] [PubMed] [Google Scholar]
- Skutle Arvid. 1999. “The Relationship among Self-Efficacy Expectancies, Severity of Alcohol Abuse, and Psychological Benefits from Drinking.” Addictive Behaviors 24 (1): 87–98. doi: 10.1016/S0306-4603(98)00007-0. [DOI] [PubMed] [Google Scholar]
- Strecher VJ, DeVellis B. McEvoy, Becker MH, and Rosenstock IM. 1986. “The Role of Self-Efficacy in Achieving Health Behavior Change.” Health Education & Behavior 13 (1): 73–92. doi: 10.1177/109019818601300108. [DOI] [PubMed] [Google Scholar]
- Suh Jesse J., Ruffins Stephen, Robins C. Edward, Albanese Mark J., and Khantzian Edward J.. 2008. “Self-Medication Hypothesis: Connecting Affective Experience and Drug Choice.” Psychoanalytic Psychology 25 (3): 518–32. doi: 10.1037/0736-9735.25.3.518. [DOI] [Google Scholar]
- Thomas Suzanne E., Bacon Amy K., Randall Patrick K., Brady Kathleen T., and See Ronald E.. 2011. “An Acute Psychosocial Stressor Increases Drinking in Non-Treatment-Seeking Alcoholics.” Psychopharmacology 218 (1): 19–28. doi: 10.1007/s00213-010-2163-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thompson Ross A. 1991. “Emotional Regulation and Emotional Development.” Educational Psychology Review 3 (4): 269–307. doi: 10.1007/BF01319934. [DOI] [Google Scholar]
- Tomarken Andrew J., and Waller Niels G.. 2005. “Structural Equation Modeling: Strengths, Limitations, and Misconceptions.” Annual Review of Clinical Psychology 1 (1): 31–65. doi: 10.1146/annurev.clinpsy.1.102803.144239. [DOI] [PubMed] [Google Scholar]
- Ursano Robert J., McKibben Jodi B. A., Reissman Dori B., Liu Xian, Wang Leming, Sampson Robert J., and Fullerton Carol S.. 2014. “Posttraumatic Stress Disorder and Community Collective Efficacy Following the 2004 Florida Hurricanes.” Edited by Dekel Sharon. PLoS ONE 9 (2): e88467. doi: 10.1371/journal.pone.0088467. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Velden Peter G., Kleber Rolf J., and Koenen Karestan C.. 2008. “Smoking Predicts Posttraumatic Stress Symptoms among Rescue Workers: A Prospective Study of Ambulance Personnel Involved in the Enschede Fireworks Disaster.” Drug and Alcohol Dependence 94 (1–3): 267–71. doi: 10.1016/j.drugalcdep.2007.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van der Velden Peter G, Grievink Linda, Olff Miranda, Gersons Berthold P R, and Kleber Rolf J. 2007. “Smoking as a Risk Factor for Mental Health Disturbances after a Disaster: A Prospective Comparative Study.” The Journal of Clinical Psychiatry 68 (1): 87–92. http://www.ncbi.nlm.nih.gov/pubmed/17284135. [DOI] [PubMed] [Google Scholar]
- Vetter Stefan, Rossegger Astrid, Rossler Wulf, Bisson Jonathan I, and Endrass Jerome. 2008. “Exposure to the Tsunami Disaster, PTSD Symptoms and Increased Substance Use - an Internet Based Survey of Male and Female Residents of Switzerland.” BMC Public Health 8: 92. doi: 10.1186/1471-2458-8-92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vlahov D, Galea S, Ahern J, Resnick H, Boscarino JA, Gold J, Bucuvalas M, and Kilpatrick D. 2004. “Consumption of Cigarettes, Alcohol, and Marijuana among New York City Residents Six Months after the September 11 Terrorist Attacks.” American Journal of Drug & Alcohol Abuse 30 (2): 385–407. doi: 10.1081/ADA-120037384. [DOI] [PubMed] [Google Scholar]
- Vlahov D, Galea Sandro, Ahern Jennifer, Resnick Heidi, and Kilpatrick Dean. 2004. “Sustained Increased Consumption of Cigarettes, Alcohol, and Marijuana among Manhattan Residents after September 11, 2001.” American Journal of Public Health 94 (2): 253–54. doi: 10.2105/AJPH.94.2.253. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vlahov D, Galea S, Resnick H, Ahern J, Boscarino J a, Bucuvalas M, Gold J, and Kilpatrick D. 2002. “Increased Consumption of Cigarettes, Alcohol, and Marijuana among Manhattan Residents after the September 11th Terrorist Attacks.” American Journal of Epidemiology 555 (11): 988–96. [DOI] [PubMed] [Google Scholar]
- Walsh Kate, Elliott Jennifer C., Shmulewitz Dvora, Aharonovich Efrat, Strous Rael, Frisch Amos, Weizman Abraham, Spivak Baruch, Grant Bridget F., and Hasin Deborah. 2014. “Trauma Exposure, Posttraumatic Stress Disorder and Risk for Alcohol, Nicotine, and Marijuana Dependence in Israel.” Comprehensive Psychiatry 55 (3): 621–30. doi: 10.1016/j.comppsych.2013.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolitzky-Taylor Kate, Bobova Lyuba, Zinbarg Richard E., Mineka Susan, and Craske Michelle G.. 2012. “Longitudinal Investigation of the Impact of Anxiety and Mood Disorders in Adolescence on Subsequent Substance Use Disorder Onset and Vice Versa.” Addictive Behaviors 37 (8): 982–85. doi: 10.1016/j.addbeh.2012.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhao Xinshu, Lynch John G., and Chen Qimei. 2010. “Reconsidering Baron and Kenny: Myths and Truths about Mediation Analysis.” Journal of Consumer Research 37 (2): 197–206. doi: 10.1086/651257. [DOI] [Google Scholar]


