Abstract
PURPOSE
Recent studies have revealed that the lack of continuity in preparing patients with spina bifida to transition into adult-centered care may have detrimental health consequences. We sought to describe current practices of transitional care services offered at spina bifida clinics in the US.
METHODS
Survey design followed the validated transitional care survey by the National Cystic Fibrosis center. Survey was amended for spina bifida. Face validity was completed. Survey was distributed to registered clinics via the Spina Bifida Association. Results were analyzed via descriptive means.
RESULTS
Total of 34 clinics responded. Over 90 characteristics were analyzed per clinic. The concept of transition is discussed with most patients. Most clinics discuss mobility, bowel and bladder management, weight, and education plans consistently. Most do not routinely evaluate their process or discuss insurance coverage changes with patients. Only 30% communicate with the adult providers. Sexuality, pregnancy and reproductive issues are not readily discussed in most clinics. Overall clinics self-rate themselves as a 5/10 in their ability to provide services for their patients during transition.
CONCLUSIONS
Characteristics of current transitional care services and formal transitional care programs at US clinics show wide variances in what is offered to patients and families.
Keywords: Spina bifida, transitional care, myelomeningocele
1. Introduction
Adults with congenital chronic conditions, their families and the pediatric healthcare community have long recognized the need for a system that would aid in facilitating health care from pediatric to adult-centered models. With an estimate of over 500,000 adolescents with various chronic health care needs reaching an age for transition into adult-centered care every year, a national recognition promoting transition planning is imperative [1]. Many congenital disorders, including spina bifida (SB) have seen increased survival rates over the last several decades [2]. With advances in medical and surgical management for those with SB, an increasing proportion of children are surviving into adulthood [3,4]. Although data regarding the prevalence of SB among adults has not been reported, it is estimated that 75% of children with SB will survive into adulthood [3]. Due to this, the management of SB related symptoms and conditions during different life stages, including the transition from youth to adulthood, has become of increased interest [5,6].
In addition to the anticipated medical complications that may occur in those with complex congenital conditions when compared to unaffected adolescents, 11 to 16 year olds with physical disabilities have reported more difficulty with decision making, making and communicating with friends, planning to attend college, and are more likely unable to express their future plans [7]. Challenges were also noted in achieving independent living, vocational independence, community mobility, and participation in social activities [7].
A report on the National Survey of Children with Special Health Care Needs revealed that only half of all families surveyed had conversations about their child’s changing health care needs as they reached adulthood [8]. This same survey revealed that only 1 in 5 physicians had discussed transition with the child [8]. Due in part to poor transitional care from pediatric to adult providers an increasingly large proportion of patients with SB are reportedly seeking medical attention at emergency departments rather than from primary and specialty care providers [9,10].
A plan for multidisciplinary care is important for adults to prevent adverse health outcomes. Recent studies have revealed that a lack of continuity and pre-paredness for adult-centered care may have detrimental health consequences [11,12].
In order to generate recommendations for what transitional care services should be provided for successful transition of care, we first must understand the services currently offered within the US. Little data currently exists on this topic. Therefore, in this descriptive study we sought to describe the transitional care services currently offered at SB clinics in the US through a survey provided to SB clinic directors and coordinators.
2. Methods
2.1. Survey design
The survey was modeled after the validated survey for the assessment of transition practices developed for cystic fibrosis (CF) [13]. With input from national experts in SB from the National Spina Bifida Patient Registry (NSBPR) and the Spina Bifida Association (SBA) the CF survey was revised to address specific needs of SB. We based these revisions on the Life-Course conceptual model for transition. This model was designed to address three functional domains of transition: health and condition self-management; social and personal relationships; and education/income support [5]. The evaluation of the survey was divided into four main categories: Current program status; Health and condition self-management; Social and personal relationships; Education Support.
The survey was constructed and administered via SurveyMonkey® (SurveyMonkey Inc., Palo Alto, CA, USA) with logic applied for ease of use. Face validation was carried out and suggested changes for clarity were completed until consensus was achieved. The final survey (122 questions) and administration plan was approved by the institutional review board at Duke Medical Center.
2.2. Distribution
Survey distribution was carried out through the SBA listserv for all registered SB clinics in the United States. Surveys were accompanied by an introduction stating the purpose. Surveys were not anonymous to ensure duplications were not included. Voluntary completion of the survey was requested by medical directors or clinic coordinators. No incentives were provided. Answers were collected from October 2015–January 2017.
2.3. Survey analysis
All surveys were completed online. Survey results were exported into Microsoft Excel 2010 (Microsoft Corp., Redmond, WA). A random selection of 5% of the survey responses were entered by hand into Excel to assess for accuracy of the data export. Centers that had more than one responder had their answers merged using the mean answer for each question; open-ended questions retained all responses from a single center in the final dataset. Descriptive statistics were carried out.
3. Results
3.1. Response characteristics
A total of 142 clinics are currently registered with the SBA; from these, 46 responses were received from 34 spina bifida programs from across the country (24% response rate). Nineteen of the twenty-one clinics enrolled in the NSBPR completed the survey. The incomplete surveys were removed from the data (n = 16) if less than 10% of the survey was completed. The large majority of the respondents were the nurse coordinators. Completed surveys were included from 2; 5; 4; 12 and 10 clinics in the Northeast, Mid-Atlantic, Southeast, Midwest, and Western states respectively. The majority of the responding clinics serve pediatric patients only. All results included had a response from each included clinic (n = 34) unless otherwise stated.
3.2. Current programs
Survey responses aimed to capture what services are provided to prepare for transition of care. We also aimed to capture the frequency with which these services were consistently (at least 75% of the time) carried out. More than half of the clinics stated that they have a formal transitional care program in place; and about 25% were established within the past year. Of clinics with a transition program, over 60% do not have a formal written protocol in place.
The responders self-described the strengths and weaknesses of their programs (Table 1). A minority (7%) have hired specific staff members to work on transitional care needs, but most report placing “very little” effort on improving transition processes. Overall, clinics (n = 28) rated their transition processes as average (5 on a 10-point scale) regarding their ability to fulfill patients’ needs.
Table 1.
Clinic reported strengths, weakness and obstacles. Responses from 26 clinics
| Clinic-reported strengths | Clinic-reported weaknesses | Clinic-reported obstacles to success |
|---|---|---|
| Initiating transition discussion | Patient satisfaction with process | Lack of adult providers |
| Fostering self-management skills | Communication between adult and pediatric providers | Time to dedicate to transition discussion |
| Involvement of families and patients in transition | Follow-up on successful transition completion Assisting with insurance coverage changes Ability to provide independence, education and vocation support |
The process of transition is discussed with patients over 75% of the time in the large majority clinics (over 70%). This initial discussion takes place at a mean age of 15 (range 10–25 years). Many clinics (19) will delay or expedite the timing of this conversation based upon the developmental/cognitive level of the patient, family request, changes in living situation or health stability, and which insurance a patient has and availability of adult providers for the patient. The mean age for actual transition to adult-centered care was 21 years (range 18–30 years). About 60% of clinics (n = 30) allow patients to opt out of transitioning to adult providers. The reported reasons for refusal are provider requests, insurance issues, or very complex ongoing medical care from the pediatric providers.
3.2.1. Preparedness/readiness/coordination of services
The assessment of patients’ readiness to transition is delegated to a social worker or nurse coordinator in more than half of the clinics (n = 33). Less than forty percent of clinics (n = 33) report having a written list of desirable self-management skills and/or knowledge that patients should have prior to transition, but when it exists a copy is usually given to patients. An explicit program within the clinic to foster the development of these desirable skills is rarely offered (n = 33). In the few clinics (20%) that do have explicit programs to foster these skills it is carried out by both adult and pediatric providers together 80% of the time.
An important prerequisite to accessing adult care is the availability of medical insurance, which often changes during transition. Assessment of a patient’s change in insurance benefits is designated to a specific team member at the majority of clinics (n = 31). Less than half of the clinics regularly discuss insurances changes during transition (n = 32). Some (20%) never discuss this topic (n = 30).
Many clinics report difficulty in coordination due to the limited overall availability of practitioners willing to take patients with spina bifida. Clinics also reported difficulty in transition to other practitioners due to those practitioners having limited education and experience for caring for those with spina bifida.
3.2.2. Information transfer
When discussing transitioning an individual, 8% of clinics report that an adult provider is present for this discussion consistently. When a transition-specific visit is carried out for a patient, 20% of clinics report having adult providers present consistently. Written and verbal communication between providers is only present in 30% of clinics (n = 32). Most clinics (over 70%, n = 29) report that they do not have a mechanism in place to confirm that an initial visit has occurred with the adult providers.
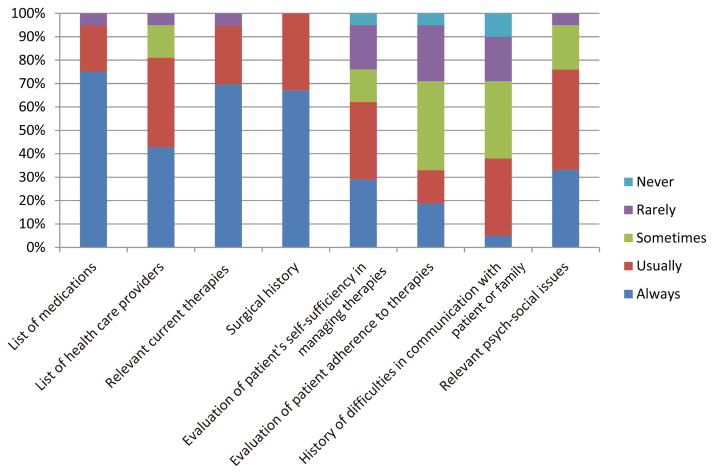
A written summary of the patient’s medical history is created before transition occurs nearly 50% of the time consistently (n = 32). About twenty percent of clinics do not create a medical summary at all. Information included in this summary, if provided, is listed in Fig. 1. Sixty-one percent of clinics (n = 26) do not allow the patient to contribute to the medical summary and the patient/family receives a copy of this medical summary at least 75% of the time at most of the clinics (n = 26). The content of the medical summary is standardized in the majority of the clinics (n = 26).
Fig. 1.
Frequency of items contained in a medical summary for adult providers, n = 29.
3.2.3. Primary care access
Only one clinic reported that the majority of their patients utilize the SB clinic for their primary pediatric care (n = 32). The SB clinic is usually able to identify the primary care provider (PCP) and has phone, written, and electronic contact (n = 32). The clinic communicates to the PCP about the status of transition most of the time (n = 32). The majority of clinics frequently assist in recommending adult PCPs for patients when needed (n = 32).
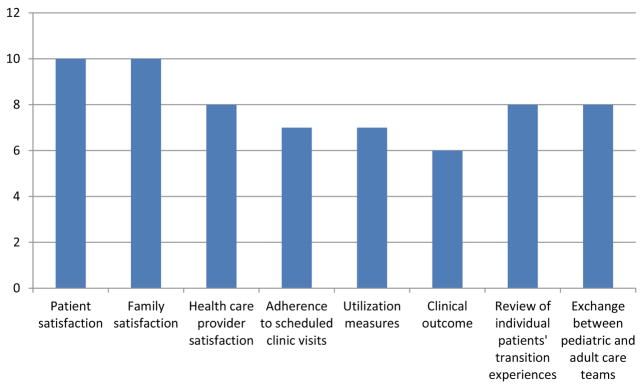
3.2.4. Program evaluation
Over 25% of clinics (n = 31) have never evaluated their transition process. Thirty percent of the clinics evaluate their transition process less than annually. Evaluations tend to encompass patient and family satisfaction, and communication processes between adult and pediatric providers. Clinical outcomes and health-care provider satisfaction are less commonly evaluated (Fig. 2).
Fig. 2.
Number of clinics performing each aspect as part of routine transitional care evaluation.
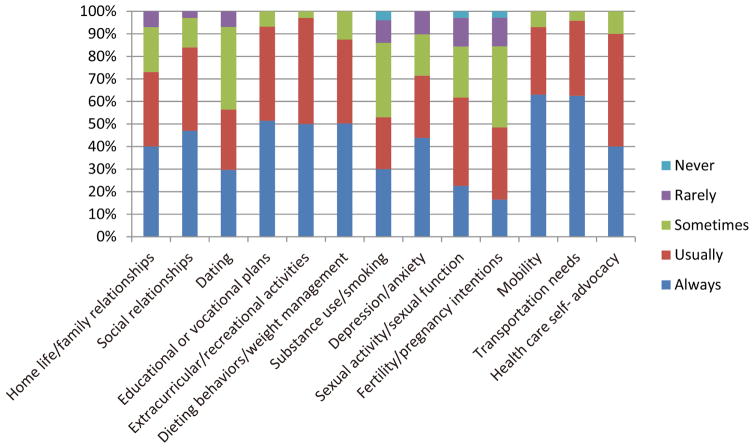
3.3. Health and condition self-management
Mobility, bowel and bladder management, transportation needs and coordination of one’s own transportation is assessed in nearly all clinics on a consistent basis. Weight management is discussed consistently in nearly 90% of clinics. Sexuality, pregnancy, and reproductive issues are infrequently a topic of discussion. The use of drugs, alcohol, and smoking are discussed consistently in 58% of clinics, but 13% rarely discuss these concerns. Forty-four percent of pediatric patients have the opportunity to meet with health providers in private at least 75% of the time. Figure 3 describes the frequency of health topics being assessed.
Fig. 3.
Frequency that each topic is part of health assessment or education for adolescents.
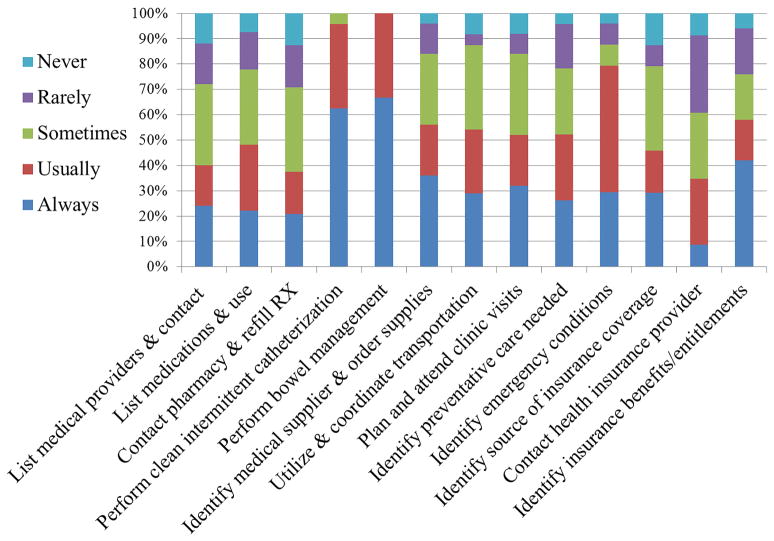
3.3.1. Condition self-management
A patient’s understanding of the transition process and his/her health goals are assessed more than half the time, as is the families’ understanding of the process. The frequency of assessment to determine a patient’s independent ability to complete health tasks is described in Fig. 4.
Fig. 4.
Frequency of assessment of patient’s ability to independently complete task n = 33.
3.4. Social and personal relationships
These areas of development are attended to consistently in nearly 90% of the responding clinics; family and romantic relationships less frequently than relationships with peers/friends.
3.5. Education support
Clinics focus on educational and vocational plans consistently. Most clinics discuss current employment or education. Maturity to function in the adult health care system is assessed more than half the time.
4. Discussion
Our national survey of registered SB programs elicited perspectives from the clinics regarding their delivery of transition-related services. A similar descriptive study has been carried out for sickle cell disease (SCD) transitional care utilizing an amended version of the validated CF survey [14]. They similarly found a wide variation in the specific transitional care practices that existed for SCD patients.
There is difficulty with adequate access to adult providers for our SB population. This was similarly noted as the largest obstacle to care for the SCD and CF populations [14]. Our survey further identified a lack of consistent communication between pediatric and adult providers in the majority of SB clinics. Communication is lacking verbally and in written form, with only 25% of clinics providing a medical and surgical summary to adult providers. Those with SB and hydrocephalus often suffer decreased IQs, and have impaired executive level functioning further increasing the need for attentive transition into adult centered care [18].
An apparent strength of all SB clinics is the ability to provide educational material to families regarding transition and to assess the patient and family’s understanding of the transition process. Although this education is carried out, a true readiness assessment of the patient to ensure that a patient has acquired self-management skills that will promote their health is rarely completed. This finding is similar to that of SCD clinics, where only 50% of clinics have a written list of self-management skills [14]. SB clinics do well in assessing specific adolescent and young adult needs such as educational plans, weight control, extracurricular activities, home and family relationships and dating behaviors.
Nearly half of clinics routinely evaluate their transition preparation activities at least once per year, similar to the SCD findings of 54% [14]. This evaluation is generally based on patient satisfaction rather than on clinical metrics or utilization measures. Survey results suggest that clinics are only fulfilling some of their patient’s needs, with an average self-ranking of 5 out of 10 regarding their ability to meet needs. The SCD survey also found an average self-ranking amongst clinics of 3.2 out of 5 [14]. A more objective measure for evaluation would be useful.
Other chronic congenital illnesses are also taking steps to create and standardize transitional care programs; of these, CF is perhaps the most formal. CF-specific transitional care programs were mandated in 2000. At that time, parallel increases in grant and financial support were put forth to aid administration of adult CF care. Through quality improvement programs, standardized guidelines were set that outlined the need for a formal transition plan to be created, annual meetings of the adult and pediatric teams, and goals of active transfer between 18–21 years of age with a target of 90% successfully transferred by 21 years of age [15]. These guidelines were established in 2008. Each center was then left to develop and implement their own guidelines to complete these goals. The three core areas needed for a successful transition program in CF have been identified as: 1) assessing for self-care readiness, 2) medical regimen adherence, and 3) mental health status [15]. When depression and mental health burdens go unaddressed in patients with chronic illness, patient self-management and self-care is often neglected; this leads to reduced health outcomes and increased associated hospital admission costs [16,17]. These obstacles to successful transition among CF programs are strikingly similar to those found in this survey of SB clinics and the SCD survey.
Our study has several limitations including the relatively low response rate by the registered clinics. This brings into question the generalizability of our results. However, it is noted that the findings from our study are largely in line with findings from the CF program as mentioned, and also sickle cell anemia transitional care surveys. The similarities in obstacles, findings, and needs does support that our results may be characteristic of all US clinics. Our survey did not ask clinics what tools they utilize to assess for things such as ability to function in the adult system. In the future determining the best tools for these types of assessments would be helpful in improving a clinic’s ability to assess for readiness to transition.
The results from our survey outline areas of strength and weakness across the country regarding current transitional care practices. We hope clinics will be able to utilize this information to see how others are practicing and that together we can conduct more research as to the direct effects of specific transitional care measures and health outcomes in our adult population.
5. Conclusion
SB clinics have a broad range of services currently being offered to assist with transition into adulthood. There seems to be little consistency in transitional care programs and evaluation techniques.
Footnotes
Conflict of interest
The authors have no conflicts of interest to report.
References
- 1.American Academy of Pediatrics AAoFP, American College of Physicians-American Society of Internal Medicine. A consensus statement on health care transitions for young adults with special health care needs. Pediatrics. 2002;110(6 Pt 2):1304–6. [PubMed] [Google Scholar]
- 2.Binks JA, Barden WS, Burke TA, et al. What do we really know about the transition to adult-centered health care? A focus on cerebral palsy and spina bifida. Arch Phys Med Rehabil. 2007;88:1064–73. doi: 10.1016/j.apmr.2007.04.018. [DOI] [PubMed] [Google Scholar]
- 3.Bowman RM, McLone DG, Grant JA, et al. Spina bifida outcome: a 25-year prospective. Pediatr Neurosurg. 2001;34(3):114–20. doi: 10.1159/000056005. [DOI] [PubMed] [Google Scholar]
- 4.Davis BE, Daley CM, Shurtleff DB, et al. Long-term survival of individuals with myelomeningocele. Pediatr Neuosurg. 2005;41(4):186–91. doi: 10.1159/000086559. [DOI] [PubMed] [Google Scholar]
- 5.Thibadeau JK, Alriksson-Schmidt AI, Zabel TA. The National Spina Bifida Program transition initiative: the people, the plan, and the process. Pediatr Clin N Am. 2010;57(4):903–10. doi: 10.1016/j.pcl.2010.07.010. [DOI] [PubMed] [Google Scholar]
- 6.Betz CL. Approaches to transition in other chronic illnesses and conditions. Pediatric Clinics of North America. 2010;57(4):983–96. doi: 10.1016/j.pcl.2010.07.017. [DOI] [PubMed] [Google Scholar]
- 7.Stevens SE, Steele CA, Jutai JW, et al. Adolescents with physical disabilities: some psychosocial aspects of health. J Adolesc Health. 1996;19(2):157–64. doi: 10.1016/1054-139X(96)00027-4. [DOI] [PubMed] [Google Scholar]
- 8.Lotstein D, McPherwson M, Strickland B, et al. Transition planning for youth with special health care needs: results from the National Survery of Children with Special Health Care Needs. Pediatrics. 2005;115:1562–8. doi: 10.1542/peds.2004-1262. [DOI] [PubMed] [Google Scholar]
- 9.McDonnell GV, McCann JP. Why do adults with spina bifida and hydrocephalus die? A clinic-based study. Eur J Pediatr Surg. 2000;10(suppl 1):31–2. doi: 10.1055/s-2008-1072411. [DOI] [PubMed] [Google Scholar]
- 10.Caterino JM, Scheatzle MD, D’Antonio JA. Descriptive analysis of 258 emergency department visits by spina bifida patients. J Emerg Med. 2006;31(1):17–22. doi: 10.1016/j.jemermed.2005.09.005. [DOI] [PubMed] [Google Scholar]
- 11.Summers SJ, Elliott S, McAdams S, Oottamasathien S, Brant WO, Presson AP, et al. Urologic problems in spina bifida patients transitioning to adult care. Urology. 2014;84(2):440–4. doi: 10.1016/j.urology.2014.03.041. [DOI] [PubMed] [Google Scholar]
- 12.Le JT, Mukherjee S. Transition to adult care for patients with spina bifida. Phys Med Rehabil Clin N Am. 2015;26(1):29–38. doi: 10.1016/j.pmr.2014.09.007. [DOI] [PubMed] [Google Scholar]
- 13.McLaughlin SE, Diener-West M, Indurkhya A, Rubin H, Heckmann R, Boyle MP. Improving transition from pediatric to adult cystic fibrosis care: lessons from a national survey of current practices. Pediatrics. 2008;121(5):e1160–6. doi: 10.1542/peds.2007-2217. [DOI] [PubMed] [Google Scholar]
- 14.Sobota A, Neufeld EJ, Sprinz P, Heeney MM. Transition from pediatric to adult care for sickle cell disease: results of a survey of pediatric providers. Am J Hematol. 2011 Jun;86(6):512–5. doi: 10.1002/ajh.22016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Okumura ML, Kleinhenz ME. Cystic fibrosis transitions of care: lessons learned and future directions for cystic fibrosis. Clin Chest Med. 2016;37(1):119–26. doi: 10.1016/j.ccm.2015.11.007. [DOI] [PubMed] [Google Scholar]
- 16.Logan D, Zelikovsky N, Labay L, et al. The illness management survey: identifying adolescents’ perceptions of barriers to adherence. J Pediatr Psychol. 2003;28(6):383–92. doi: 10.1093/jpepsy/jsg028. [DOI] [PubMed] [Google Scholar]
- 17.Hilliard ME, Eakin MN, Borrelli B, et al. Medication beliefs mediate between depressive symptoms and mediation adherence in cystic fibrosis. Health Psychol. 2015;34(5):496–504. doi: 10.1037/hea0000136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Roach JW, Short BF, Saltzman HM. Adult Consequences of Spina Bifida: A Cohort Study. Clin Orthop Relat Res. 2011;469(5):1246–52. doi: 10.1007/s11999-010-1594-z. [DOI] [PMC free article] [PubMed] [Google Scholar]