ABSTRACT
In Italy, the National Plan for the Elimination of Measles and Congenital Rubella 2010–15 suggests offering Measles, Mumps and Rubella (MMR) vaccination to susceptible women who underwent voluntary termination of pregnancy (VTP) In Rome, S. Eugenio Hospital is one of the structures where VTP is practised in an Operative Unit called “Family Planning” The primary goal of this study was to estimate the prevalence of susceptibility to rubella, using IgG and IgM immunoassays, among women accessing VTP and to offering MMR vaccination to susceptible women. Secondarily, this study evaluated acceptance of the vaccination offer From 2013 to 2015, data were collected from 1513 voluntary termination of pregnancy (VTP) cases The results show a significant increase of 5 percent in susceptibility prevalence in the target group from 13.6% in 2013 and 2014 to 18.4% in 2015 The association between rubella susceptibility and age was statistically significant (p<0.01) Throughout the entire period, acceptance of the vaccine proposal was 19% (45/232) among susceptible women; 58% (135/232) refused the vaccine and 23% (52/232) took time to think about it This study shows an increase of 5 percent in the prevalence of rubella susceptibility over two years. This result is worrying, even considering the short span of the data collection The rate of acceptance of vaccination is unsatisfactory considering the possibility of future pregnancies This issue deserves continued action, which, going forward, might transform a “project” into a shared strategy as part of a wider network with the goal of aligning Italy with international recommendations.
KEYWORDS: Active offering, immunization programs, MMR vaccine, rubella, voluntary interruption of pregnancy
Introduction
The international community has aimed to eliminate measles and rubella in five World Health Organization (WHO) Regions by 2020.1,2 According to the European Regional Verification Commission for Measles and Rubella Elimination (RVC) data, in 2015 measles was endemic in 18 of 53 (34%) countries in Europe. For rubella, the situation was similar, and both infections were endemic in 16 countries, Italy included.3
From 2005 to 2013, Italian surveillance data reported a total of 75 congenital rubella infections (7 probable and 68 confirmed cases, according to the 2012 EU congenital rubella case definition).4 The national annual mean incidence in these years was 1.5 per 100,000 live births (mean annual number of live births in Italy: 553,389); two incidence peaks of congenital rubella infections occurred in 2008 and 2012, with an incidence of 5.0 and 3.6 per 100,000 newborns, respectively.
Overall, 160 rubella infections in pregnancy were reported, among which 147 were classified as confirmed, nine as probable and four as possible cases.5
In Italy, underreporting of congenital rubella has been demonstrated to be a problem. Underreporting of congenital rubella in Italy was 53% in 2010–2014. The main sources of data are the hospital discharge registries, which have been shown to be inappropriate for detecting congenital rubella cases. Therefore, further efforts are required to improve congenital rubella surveillance so that it is more sensitive and specific.6
In Italy, the National Plan for the Elimination of Measles and Congenital Rubella (PNEMoRc) 2010–15 included the objective of reducing prevalence of susceptibility to rubella among young women to under 5% and to improve Measles, Mumps and Rubella (MMR) vaccination coverage between adults and children.7
Among the actions, the plan suggested finding every opportunity to protect women of childbearing age and to offer MMR vaccination to susceptible women who underwent voluntary termination of pregnancy (VTP).
In Italy, regional and local data about vaccination coverage for MMR in childbearing-age women are not available. Seroprevalence studies have been conducted,8 and surveillance data have been obtained through the Italian Behavioral Risk Factor Surveillance System (“PASSI”, which stands for “health progress made at local health unit level in Italy”), which describes the local situation.9
Experiences with offering MMR vaccination in adolescent and adult women are scarce at the international level10,11; no data are available for describing MMR offer after VTP.
For this reason, we decided to analyse a local experience conducted in Rome in S. Eugenio Hospital, one of the public structures on Roman territory where VTP is practised in the “Family Planning” operative unit. The procedure is performed in the Day Surgery unit preceded by a day of pre-hospitalization.
In Rome, from 2013 to 2015, 23355 VTP were notified. According to these data, S. Eugenio Hospital is responsible for 11% of those interventions.12,13,14
Women may access this service directly or through territorial Family Counselling Center.
Aim
The primary goal of this study was to estimate the prevalence of susceptibility to rubella among women accessing VTP and of offer of MMR vaccination to susceptible women; secondarily, this study evaluates acceptance of this offer.
Results
Data from 2013 to 2015 were collected from 1513 voluntary termination of pregnancy (VTP) cases: 1243 surgical procedures and, from 2015, 270 RU486 administrations.15
Stratifying data by age, there were no significant differences in carrying out surgical or medical abortion and in different behaviours towards the vaccine proposal. Therefore, 2015 data will be discussed in aggregate, without distinguishing surgical and pharmacological procedures.
In 98% (1484/1513) of cases, susceptibility was evaluated through Rubella IgG and IgM immunoassays.
Table 1 summarizes the results of the evaluation of susceptibility to rubella and acceptance of the vaccine among women accessing the Family Planning Unit of S. Eugenio Hospital.
Table 1.
Susceptible women offered vaccination to rubella and adhesion to vaccinal proposal by year- Data from Family Planning Unit, S. Eugenio Hospital (2013–15).
| VTPa (N) | Rubella test (N (%)) | Susceptible (N (%)) | Adhesion to vaccinal proposal (N (%)) | |
|---|---|---|---|---|
| 20131 | 316 | 294 (93%) | 40 (13,6%) | 16 (40%) |
| 2014 | 573 | 566 (99%) | 77 (13.6%) | 19 (25%) |
| 2015 | 6242 | 624 (100%) | 115 (18.4%)* | 10 (8%) |
| Tot. | 1513 | 1484 (98%) | 232 (15.6%) | 45 (19%) |
VTP: voluntary termination of pregnancy
data referred to 2nd semester of 2013
of these, from 2015, 270 administrations of RU486 (“pharmacological” abortion);
p<0,05
These results show a significant increase of 5 percentage points in susceptibility prevalence in the target group from 13.6% in 2013 and 2014 to 18.4% in 2015 (OR 0.69; 95% CI 0.50 – 0.95). The mean age in 2014 and 2015 groups was similar.
The prevalence of susceptibility to rubella was not influenced by nationality. It was higher in Italian women than in foreign women (16.8% vs 14%) (Table 2), but this difference was not statistically significant (OR 0.81; CI 0.59 – 1.12).
Table 2.
Susceptible women by geographical origin- Data from Family Planning Unit, S. Eugenio Hospital (2013–15).
| Nationality | Rubella test (N) | Susceptible (N (%)) |
|---|---|---|
| Italian | 850 | 143 (16.8%) |
| Foreign | 634 | 89 (14.0%) |
| Tot. | 1484 | 232 (15.6%) |
Figure 1 shows the results of the age-stratified rubella test in 2014 and 2015, when data about age were collected. These data coincide with other Italian data collected, where VTP rates were higher in women between 25–34 years old from 2014 to 2015.16,17
Figure 1.

Women who performed a Rubella test by age and proportion of susceptible; data from Family Planning Unit, S. Eugenio Hospital (2014–15, n. 1190).
In the two-year period of 2014–15, 16% (192/1190) of women were susceptible to the disease. The prevalence fell from 22% in 18–24-year-old women to 11% in women over 35. The trend was statistically significant (p<0.01).
Throughout the entire period, acceptance of the vaccine was 19% (45/232) among susceptible women (see Table 1); 58% (135/232) refused the proposal and 23% (52/232) took time to think about it.
In the two-year period of 2014–15, 15% (29/188) of women accepted the vaccine. Figure 2 shows the results stratified by age.
Figure 2.
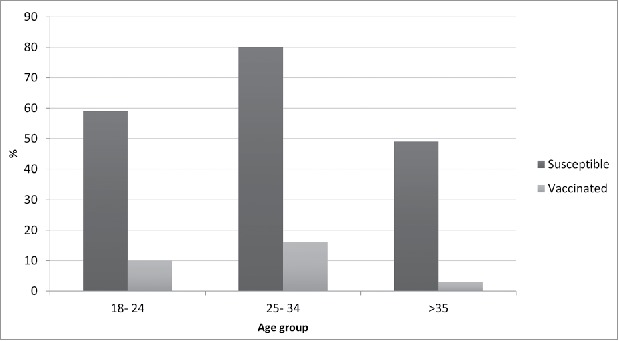
Women who accepted to be vaccinated by age; data from Family Planning Unit, S. Eugenio Hospital (2014–15).
These data were influenced by age: in the 18–24 age group, 17% (10/59) of women accepted the vaccination. Women between 25 and 34 years old showed the highest percentage of acceptance of the vaccine (20%, 16/80), and only 6% of women over 35 years (3/49) accepted the vaccine. However, this difference was not statistically significant.
There were no statistically significant differences in nationality: 15% of Italian women and 16% of foreigners accepted the vaccination (OR = 0.87 IC 95% 0.38–1.99).
Over the years, the results showed a reduction in the prevalence of vaccination acceptance from 40% (16/40) in 2013 to 25% (19/77) in 2014 to 9% (10/115) in 2015. However, the differences were not statistically significant.
Finally, data on the two types of voluntary interruption of pregnancy (surgical vs pharmacological intervention) were compared in order to assess whether they influenced acceptance of the vaccination. The results for 2015 showed greater acceptance of the vaccine among the 270 women undergoing the pharmacological procedure (13%) compared to the 354 who had a surgical procedure (6%), but the difference was not statistically significant (OR 2.58; 95% CI 0.67–9.55).
Discussion
Data from the PASSI surveillance system from 2012–13 estimated that the Italian Local Healthcare Unit had a 57% prevalence of immune women aged 18–49 years old; these women underwent vaccination (33%) or achieved immunization from past infection detected by a positive Rubella test (24%). In the same target group, 3% were susceptible and 40% were not aware of their immune status against rubella.18 Therefore, to reach elimination, interventions are needed for women of childbearing age.
This study showed an increase of 5 percentage points in the prevalence of rubella susceptibility over two years. This result is worrying, even taking into account the short span of the data collection.
Rubella susceptibility in the sample was 15.6%, far from the 5% required for women of childbearing age by objective 4 of the National Elimination Plan. This work provides a confirmation at the local level of what is already known at the national and regional levels.
Age influences rubella susceptibility: as the women grow older, the proportion of protection increases because women over 35 years had a greater chance of being exposed to the virus. Younger women, though not vaccinated, did not contract the infection because viral circulation was hampered by vaccine campaigns. As expected, in this study, a significant decrease of susceptibility with increasing age was noted. However, this is not the reason for the increasing susceptibility in 2015.
Over that period, 19% of non-immunized women accepted vaccination. This percentage is not satisfactory considering the possibility of future pregnancies. We may need to consider that the emotional context is stressful and leaves no space for preventative considerations. However, the better findings among women undergoing pharmacological abortion (with the limitation of the reduced size of the sample) are important.
In this regard, some Italian experiences on vaccination during the postpartum period show more encouraging results.19,20 Additionally, the role of the recent and popular phenomenon of “vaccine hesitancy” has to be considered.21
In this study, from 2013 to 2015, the prevalence of acceptance of vaccination has worsened, falling by 31 percentage points. It is necessary to ask how vaccination can be sustained over time and overcome the inevitable reduction of motivation among health workers.
This study brings to different conclusion, at different levels.
Rubella susceptibility is still an important problem in pregnancy and this study shows the results of a first experience of active offering of rubella vaccine after VTP, outlining the difficulties in having the prophylaxis accepted in this specific situation. A better adherence was found among women from 25 to 34 years. Even if we did not ask the women if they considered having a child in the future, this may be due to the awareness of the possibility of future pregnancies and the desire to avoid risk for the unborn. This observation must lead to implement the offer in the services involved in supporting women and maternity, to take advantage of all the contact opportunities with the National Health Service (vaccination against Human Papilloma Virus, cytological screening, contraception).
Future studies should deeply investigate the reasons for accepting or refusing vaccine after VTP and evaluate differences in accepting the vaccination proposal between surgical and pharmacological abortion. The results could induce modification in the way of offering vaccine and motivating women and healthcare workers. In order to implement this intervention, continuous action must be taken forward, transforming a “project” into a shared strategy, part of a wider network, trying to align Italy to the recommendation at international level.1,2,3
In any case, the priority to keep coverage high in early childhood must be reaffirmed, because studies like this demonstrate that promoting and accepting vaccination practice in adulthood is a complex task for public healthcare providers.
Materials and methods
Starting from July 2013, in the S. Eugenio Hospital, a protocol for controlling rubella serology among all women undergoing VTP and actively offering the MMR vaccination was used. From January 2015, the evaluation and the offer were extended to women accessing a medical abortion through administration of Mifepristone (RU486) within the first seven weeks of pregnancy.
Rubella IgG and IgM immunoassays were conducted for all women among the blood tests carried out before surgery. The test was not performed in women who presented a recent result of these immunoassays or underwent an emergency protocol (which does not provide the test). These situations were the only exclusion criteria. The test was performed with a Liaison XL tool (“DiaSorin” Company) through Chemiluminescent Immunoassays (CLIA).
Reference values were as follows: IgG was negative if <5 UI/mL, uncertain between 5 and 10 UI/mL, and positive if >10 UI/mL; IgM was negative if <20 UI/mL, uncertain between 20 and 25 UI/mL, and positive if >25 UI/mL. Women with negative or uncertain results were considered susceptible.
Susceptible women received short counselling and an information booklet for MMR vaccination. The vaccine was administered, if accepted, before hospital discharge and after obtaining informed consent.
From July to December 2013, data were collected in aggregate mode using monthly reports drawn up by the operative unit.
In 2014 and 2015, we collected individual data, including date of birth and date of sample collection, through an efficient information flow with the Laboratory of S. Eugenio Hospital. Therefore, these data were considered only for the 2014–2015 sample.
Each access to the structure was considered an incident case of IVG in this population because anonymization of data did not allow us to exclude women undergoing multiple procedures.
This study was not submitted to the Ethics Committee's approval because it was carried out within the local transposition of what PNEMoRc advised. In addition, the data collection method guaranteed the anonymity of the participants
Data were analysed using SPSS software.
Disclosure of potential conflicts of interest
The authors report no conflicts of interest.
References
- 1.“The Global Vaccine Action Plan 2011–2020 ”, WHO 2012. http://www.who.int/immunization/global_vaccine_action_plan/GVAP_doc_2011_2020/en/ [Google Scholar]
- 2.“European Vaccine Action Plan 2015–2020 ”, WHO, 2014. http://www.euro.who.int/en/health-topics/communicablediseases/hepatitis/publications/2014/european-vaccine-action-plan-20152020-2014. [Google Scholar]
- 3.“4th Meeting of the European Regional Verification Commission for Measles and Rubella Elimination (Rvc) ”, WHO 2015. http://www.euro.who.int/en/health-topics/communicable-diseases/measles-and-rubella/publications/2016/4th-meeting-of-the-european-regional-verification-commission-for-measles-and-rubella-elimination-rvc. [Google Scholar]
- 4.European Commission Commission Implementing Decision of 8 August 2012 (2012/506/EU) amending Decision 2002/253/EC laying down case definitions for reporting communicable diseases to the Community network under Decision No 2119/98/EC of the European Parliament and of the Council. Official J Eur Union. Luxembourg: Publications Office Eur Union. 27.9.2012;L 262 http://eur-lex.europa.eu/legal-content/EN/TXT/?uri=CELEX%3A32012D0506. [Google Scholar]
- 5.Giambi C, Bella A, Filia A, Del Manso M, Nacca G, Declich S, Rota MC; Regional contact points for rubella. Underreporting of congenital rubella in Italy, 2010–2014. Eur J Pediatr. 2017;176(7):955–962. doi: 10.1007/s00431-017-2935-7. PMID:28551878. [DOI] [PubMed] [Google Scholar]
- 6.Giambi C, Bella A, Filia A, Del Manso M, Nacca G, Declich S, Rota MC; Regional contact points for rubella. Underreporting of congenital rubella in Italy, 2010–2014. Eur J Pediatr. 2017;176(7):955–962. doi: 10.1007/s00431-017-2935-7. PMID:28551878. [DOI] [PubMed] [Google Scholar]
- 7.Presidency of the Council of Ministers Rep.n. 66/ State–Regions Conference of 23 March 2011; Italian national plan for the elimination of measles and congenital rubella (PNEMoRc) 2010–2015. [Google Scholar]
- 8.Rota MC, Bella A, Gabutti G, Giambi C, Filia A, Guido M, De Donno A, Crovari P, Ciofi Degli Atti ML; Serological Study Group . Rubella seroprofile of the Italian population: an 8-year comparison. Epidemiol Infect. 2007;135(4):555–62. doi: 10.1017/S0950268806007400. PMID:17076939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Baldissera S, Campostrini S, Binkin N, Minardi V, Minelli G, Ferrante G, Salmaso S; PASSI Coordinating Group . Features and initial assessment of the Italian Behavioral Risk Factor Surveillance System (PASSI), 2007–2008. Prev Chronic Dis. 2011;8(1):A24. PMID:21159236. [PMC free article] [PubMed] [Google Scholar]
- 10.Plans P, de Ory F, Campins M, Álvarez E, Payà T, Guisasola E, Compte C, Vellbé K, Sánchez C, Lozano MJ, Aran I, Bonmatí A, Carreras R, Jané M, Cabero L. Prevalence of anti-rubella, anti-measles and anti-mumps IgG antibodies in neonates and pregnant women in Catalonia (Spain) in 2013: susceptibility to measles increased from 2003 to 2013. Eur J Clin Microbiol Infect Dis. 2015;34(6):1161–71. doi: 10.1007/s10096-015-2339-4. PMID:25666082. [DOI] [PubMed] [Google Scholar]
- 11.Lo Giudice D, Capua A, La Fauci V, Squeri R, Grillo OC, Calimeri S. Congenital rubella syndrome and immunity status of immigrant women living in southern Italy: a cross-sectional, seroepidemiological investigation. Travel Med Infect Dis. 2014;12(3):253–7. doi: 10.1016/j.tmaid.2014.01.003. PMID:24502919. [DOI] [PubMed] [Google Scholar]
- 12.Lazio Region, Health and Socio-Sanitary Integration Direction Voluntary Termination of Pregnancy in 2013. http://www.regione.lazio.it/binary/rl_sistemi_informativi_sanitari/tbl_documenti/SIS_RPT_IVG_09_2013.pdf.
- 13.Lazio Region, Health and Socio-Sanitary Integration Direction Voluntary Termination of Pregnancy in 2014. http://www.regione.lazio.it/binary/rl_sanita/tbl_contenuti/rapporto_ivg_2014.pdf.
- 14.Lazio Region, Health and Socio-Sanitary Integration Direction Voluntary Termination of Pregnancy in 2015. https://www.regione.lazio.it/binary/rl_sanita/tbl_contenuti/rapporto_IVG2015_nov2016.pdf.
- 15.Raymond EG, Shannon C, Weaver MA, Winikoff B. First-trimester medical abortion with mifepristone 200 mg and misoprostol: a systematic review. Contraception. 2013;87(1):26–37. doi: 10.1016/j.contraception.2012.06.011. PMID:22898359. [DOI] [PubMed] [Google Scholar]
- 16.Italian Health Department Report on law 194/78, protection of motherhood and VTP. Data 2014–2015. http://www.salute.gov.it/mgs/C_17_pubblicazioni_2552_allegato.pdf.
- 17.Italian Health Department Report on law 194/78, protection of motherhood and VTP. Preliminar data 2014 and final data 2013. http://www.salute.gov.it/imgs/C_17_pubblicazioni_2428_allegato.pdf.
- 18.Lancia A, Vazzoler C, Arrivi F, Pettinicchio V, Marzani S, Trinito MO. The evaluation of susceptibility to rubella in women of childbearing age; the experience of the Asl Roma C. Ig Sanita Pubbl. 2014;70(2):247–54. [PubMed] [Google Scholar]
- 19.Ferraroni E, Volta A, Capuano C, et al.. Prevenzione della rosolia congenita: vaccinazione nel post-partum in un punto nascita di I. livello. Medico e Bambino Pagine Elettroniche. 2007;26(4). https://www.medicoebambino.com/_donne_rosolia_vaccinazione_sieronegative_gravidanza. [Google Scholar]
- 20.Leonardi G, Campra D, Silano V, et al.. Recupero vaccinale anti-rosolia nel post-partum. Medico e Bambino Pagine Elettroniche. 2008;27(7). https://www.medicoebambino.com/?id=RI0807_10.html [Google Scholar]
- 21.MacDonald NE, Vaccine hesitancy: Definition, scope and determinants. Vaccine. 2015;33(34):4161–4. (14 August 2015) doi: 10.1016/j.vaccine.2015.04.036. [DOI] [PubMed] [Google Scholar]


