Abstract
The substance abuse, violence and HIV/AIDS (SAVA) syndemic represents a complex set of social determinants of health that impacts the lives of women. Specifically, there is growing evidence that intimate partner violence (IPV) places women at risk for both HIV acquisition and poorer HIV-related outcomes. This study assessed prevalence of IPV in an HIV clinic setting, as well as the associations between IPV, symptoms of depression and PTSD on three HIV-related outcomes—CD4 count, viral load, and missed clinic visits. In total, 239 adult women attending an HIV-specialty clinic were included. Fifty-one percent (95% CI: 45–58%) reported past year psychological, physical, or sexual intimate partner abuse. In unadjusted models, IPV was associated with having a CD4 count <200 (OR: 3.284, 95% CI: 1.251–8.619, p=0.016) and having a detectable viral load (OR: 1.842, 95% CI: 1.006–3.371, p=0.048). IPV was not associated with missing >33% of past year all type clinic visits (OR: 1.535, 95% CI: 0.920–2.560, p=0.101) or HIV specialty clinic visits (OR: 1.251, 95% CI: 0.732–2.140). In multivariable regression, controlling for substance use, mental health symptoms and demographic covariates, IPV remained associated with CD4 count <200 (OR: 3.536, 95% CI: 1.114–11.224, p=0.032), but not viral suppression. The association between IPV and lower CD4 counts, but not adherence markers such as viral suppression and missed visits, indicates a need to examine potential physiologic impacts of trauma that may alter the immune functioning of women living with HIV. Incorporating trauma-informed approaches into current HIV care settings is one opportunity that begins to address IPV in this patient population.
Background
Women continue to be disparately impacted by the co-occurring epidemics of HIV and intimate partner violence (IPV). Various factors have been identified as being linked to increased risk of HIV acquisition among women who have experienced IPV including, poorer mental health, substance abuse, ongoing sexual violence, increased frequency of sexually transmitted infections, and increased sexual risk behaviors (Campbell et al., 2008; Draughon, 2012; Jewkes, Dunkle, Nduna, & Shai, 2010). Relatively less attention has been given in the literature regarding ways in which current or past IPV may impact long-term HIV treatment adherence or outcomes, although similar pathways have been proposed (Campbell, Lucea, Stockman, & Draughon, 2013; Schafer et al., 2012).
In 2013, a White House issued report acknowledged the need to address the intersection of HIV and violence against women. This report highlighted the importance of gaining a more complete understanding of the impact of violence on the health of women and girls living with or at risk for HIV (Interagency Federal Working Group, 2013). Subsequently, a 2015 meta-analysis found that women who reported experiencing IPV were less likely to report current anti-retroviral therapy (ART) use, had poorer self-reported ART adherence, and were less likely to achieve viral suppression (Hatcher, Smout, Turan, Christofides, & Stockl, 2015).
Partner violence is not the only social determinant of health shown to impact HIV treatment adherence and outcomes among women. Syndemic theory, first introduced in 1994, has been used to frame studies examining a wide range of social and health-related factors that act together to impact HIV risk and treatment (Singer, 2009). Specifically, the substance abuse, violence and HIV/AIDS (SAVA) syndemic highlights the interconnected risks of these distinct risk factors (Singer, 1994, 1996, 2009). The purpose of this study was twofold: 1) to determine the prevalence of past year IPV among a sample of women attending an HIV specialty clinic, and 2) to examine the association between SAVA syndemic factors (past year IPV, substance use, mental health symptoms) and three HIV treatment and adherence related outcomes - CD4 count, viral load, and missed clinic visits.
Methods
Recruitment and Data Collection
A cross-sectional, tablet-administered survey with associated medical record review was completed with consenting adult women who were patients at an HIV specialty clinic. Participants were recruited between March 2014 and November 2015. Women were eligible to participate if they were at least 18 years of age, spoke English, were living with HIV, had been a patient at the study clinic for at least the past year, and reported being in an intimate relationship at any point during the past year. Interested women were screened for eligibility, and an oral consent script was reviewed with potential participants. A trained interviewer was available in the clinic to accommodate participants who reported vision or literacy concerns with completing the survey items. Study procedures were approved by the Johns Hopkins Medical Institution (JHMI) Institutional Review Board, and participants were compensated with a $10 gift card for their participation.
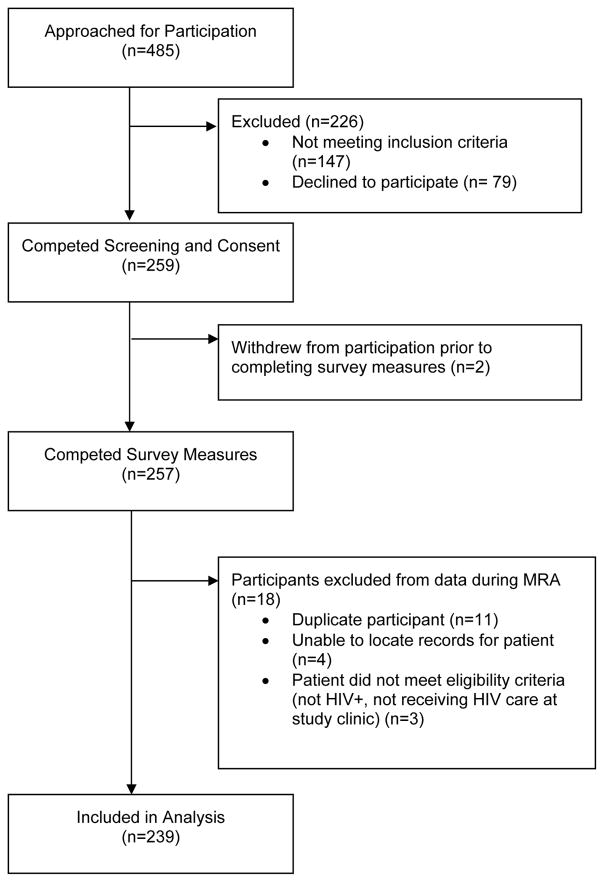
In total, 485 women approached the research team during the study’s recruitment period (see Figure 1). Of those, 53% (n=259) were eligible and consented to study participation; two participants declined to complete any study measures after consent. During review of medical records, 18 participants were excluded for reasons listed in Figure 1; this resulted in 239 women included in analysis.
Figure 1.
Study inclusion diagram.
Note: MRA: medical records abstraction
Measures
Intimate partner violence
Assessment of past year IPV included a four-question version of the Abuse Assessment Screen (AAS) which includes items for emotional, physical and sexual abuse as well as an item about feeling unsafe in a relationship, and the 46-item Severity of Violence Against Women Scales (SVAWS) which includes items specific to abusive behavior across nine domains of violence including: symbolic violence; threats of violence (mild, moderate, serious); physical violence (mild, minor, moderate, serious); and sexual violence (Marshall, 1992; McFarlane, Parker, Soeken, & Bullock, 1992). Women who answered “yes” to any item on the AAS, or to having experienced any item in the moderate or severe physical or the sexual violence categories on the SVAWS were classified as having experienced past year IPV.
Mental health and substance use
The Center for Epidemiologic Studies Depression Scale (CES-D) and PTSD Checklist Civilian Version (PCL-C) were used to assess past two weeks symptoms of depression, and past month symptoms of PTSD (Blanchard, Jones-Alexander, Buckley, & Forneris, 1996; Radloff, 1977). The Drug Abuse Screening Tool (DAST-10) and Alcohol Use Disorder Identification Test (AUDIT) were used to determine past year drug use, and past six month alcohol use (Babor, Higgins-Biddle, Saunders, & Monteiro, 2001; Bohn, Babor, & Kranzler, 1995; Skinner, 1982). Standard cut-off scores were used for the CES-D (≥16), AUDIT (≥8) and PCL-C (≥45) (Babor et al., 2001; Radloff, 1977; Ruggiero, Del Ben, Scotti, & Rabalais, 2003). One item from the DAST-10 (“In the past year, have you used drugs other than those required for medical reasons?”) was used in combination with lab or provider documentation of drug use in the medical record to create a composite variable of illicit drug use in the past year.
CD4 count, viral load and missed clinic visits
Data for the three outcomes were obtained by medical record review. Most recent CD4 count and viral load were obtained from recorded laboratory values taken on or before the day of survey completion. Values were dichotomized into clinically relevant groups (CD4 count ≥200 cells/mm3 or <200 cells/mm3; viral load detectable [>20 copies/ml] or not detectable [≤20 copies/ml]). The third outcome was the proportion of missed clinic visits in the past year calculated from the scheduled outpatient visits within the health system (both HIV specialty care and other system clinics) and the corresponding number of missed visits. The proportion of missed visits was dichotomized into two groups—missed ≤33% of scheduled visits compared to missed >33% of scheduled visits. Dichotomization of outcome variable was used to address concerns of non-normality within the data for these outcomes.
Data Analysis
Data were analyzed using SPSS Version 23 (IBM, 2014). Descriptive and bivariate analysis was completed with all outcome variables and covariates. Multivariable logistic regression models that included demographic covariates significantly associated with any of the three outcomes during bivariate testing were then built. In all models, SAVA covariates (IPV, mental health, and substance use variables) were included. For the CD4 count and viral load outcomes, analysis was limited to participants who were prescribed ART within the year prior to survey completion.
Results
The sample was primarily African-American (86.6%) and non-Hispanic (94.5%) women with a median age of 50 (IQR: 44–55). Over half of the women (58%) had completed high school or obtained a GED. While we did not include direct income measures, the overwhelming majority of participants utilized public insurance including Medicare, Medicaid or Ryan White funding (96.7%) and only 12.6% were employed outside the home. Additional demographic data is presented in Table 1.
Table 1.
Participant Demographics by Past Year IPV Status
| Overall b (n=239) | IPV + b (n=122) | IPV − b (n=117) | p valuea | |
|---|---|---|---|---|
| Age c (range 24–66) | 50 (44–55) | 50 (43–55) | 52 (44–56) | 0.175 |
| Race | 0.623 | |||
| Native American | 2 (0.8) | 2 (1.6) | 0 (0) | |
| Black/African American | 207 (86.6) | 106 (86.9) | 101 (86.3) | |
| White/Caucasian | 9 (3.8) | 5 (4.1) | 4 (3.4) | |
| Multiple races/mixed/other | 10 (4.2) | 4 (3.3) | 6 (5.1) | |
| Did not respond | 11 (4.6) | 5 (4.1) | 6 (5.1) | |
| Hispanic (n=229) | 3 (1.3) | 2 (1.7) | 1 (0.9) | 0.587 |
| Education (n=236) | 0.050 | |||
| 8th grade or less | 22 (9.2) | 18 (14.8) | 4 (3.4) | |
| Some high school | 77 (32.2) | 42 (34.4) | 35 (29.9) | |
| High school diploma/GED | 81 (33.9) | 35 (28.7) | 46 (39.3) | |
| Some college | 40 (16.7) | 21 (17.2) | 19 (16.2) | |
| Associate’s/vocational degree | 9 (3.8) | 3 (2.5) | 6 (5.1) | |
| Bachelor’s/4 year degree | 6 (2.5) | 2 (1.6) | 4 (3.4) | |
| Graduate work/degree | 1 (0.4) | 0 (0) | 1 (0.9) | |
| Insurance type | 0.436 | |||
| Public | 231 (96.7) | 119 (97.5) | 112 (95.7) | |
| Private | 8 (3.3) | 3 (2.5) | 5 (4.3) | |
| Children under 18 | 0.752 | |||
| Yes | 49 (20.5) | 26 (21.3) | 23 (19.7) | |
| No | 190 (79.5) | 96 (78.7) | 94 (80.3) | |
| Employed | 30 (12.6) | 9 (7.4) | 21 (17.9) | 0.014 |
| CES-D ≥16 (n=237) | 64 (27.0) | 48 (39.3) | 16 (13.9) | <0.001 |
| PCL ≥45 (n=237) | 56 (23.6) | 41 (33.6) | 15 (13.0) | <0.001 |
| Past year drug use | 120 (50.2) | 69 (56.6) | 51 (43.6) | 0.045 |
| AUDIT ≥8 (n=237) | 45 (19.0) | 32 (26.2) | 13 (11.3) | 0.003 |
Notes: Items in bold were statistically significant. IPV: intimate partner violence; CES-D: Center for Epidemiologic Centers Scales – Depression; PCL: post-traumatic checklist; AUDIT: Alcohol Use Disorders Identification Test.
p-values are for chi-square analysis examining differences between women reporting past year IPV and those not reporting past year IPV, except age in which differences were assessed and reported using Mann Whitney U-tests.
n (%)
median (IQR)
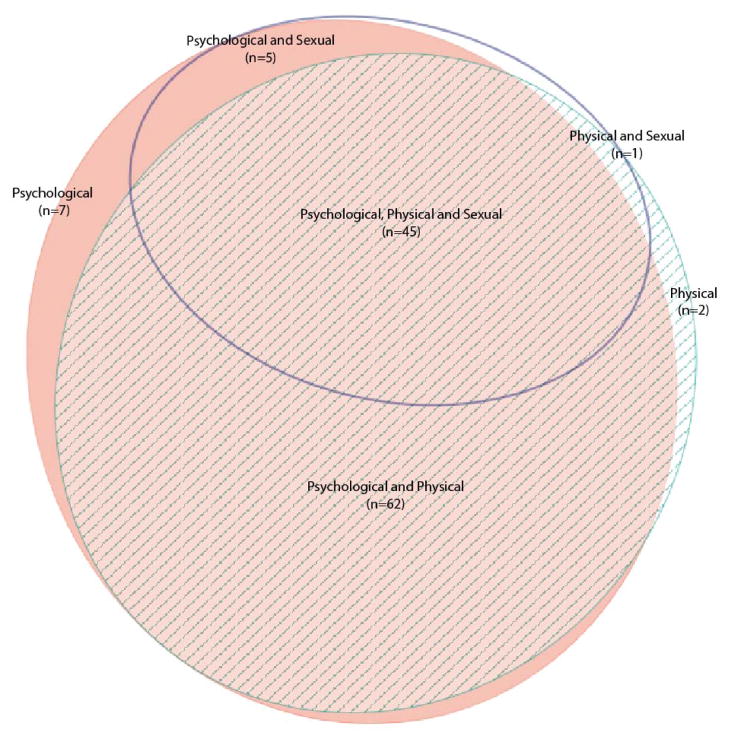
Prevalence of Intimate Partner Violence
Over half of the sample participants (n=122, 51%, 95% CI: 45–58%) reported past year physical, sexual or psychological IPV. Nearly all women reporting IPV (n=119, 97.5%, 95% CI: 95–100%) reported psychological abuse, with a similar proportion reporting physical violence (n=110, 90.1%, 95% CI: 85–96%). Fewer women (n=51, 41.8%, 95% CI: 33–51%) reported sexual violence (see Figure 2).
Figure 2.
Intimate partner violence types reported by participants (n=122).
Notes: Zero participants reported only sexual violence. Categories are mutually exclusive. Diagram created using eulerAPE (Micallef & Rodgers, 2014). Diagram proportions are approximate.
HIV Treatment Outcomes
From medical record reviews, the majority of women had well-controlled HIV disease with only 10% (n=25) having a most recent CD4 count <200 (95% CI: 4–14%). Almost one-third of women (n=71) had detectable viral loads (30%, 95% CI: 24–36%). Only fifteen women (6%) had both a detectable viral load and CD4 count <200. The number of scheduled clinic visits in the year prior to the survey had a wide range, (1–358 scheduled visits) primarily related to programs within the health system such as daily methadone maintenance treatment, which substantially increased the number of scheduled visits for some participants. The median number of annual scheduled visits was 26 (IQR: 16–41), and the median number of missed visits in the past year was seven (IQR: 3–13). Proportion of missed visits for participants ranged from zero to 84% with a median of 29.6% missed scheduled visits (IQR: 16.7–43.3%). The number of scheduled HIV specialty clinic visits ranged from 1 to 45 with a median of 8 visits (IQR: 5–10). Proportion of missed HIV specialty care visits ranged from zero to 100% with a median of 25% (IQR: 10.0–41.1%).
Associations with HIV treatment outcomes
In bivariate analysis, past year IPV was associated with having a CD4 count <200 (OR: 3.284, 95% CI: 1.251–8.619, p=0.016) (Table 2). This relationship maintained its significance in a multiple variable model controlling for demographic, mental health and substance use variables (OR: 3.536, 95% CI: 1.114–11.224, p=0.032), indicating that the odds of having a CD4 count <200 for women who reported past year IPV were three and a half times higher than their non-abused counterparts. IPV was also associated with having a detectable viral load but in bivariate analysis only (OR: 1.842, 95% CI: 1.006–3.371, p=0.048) (Table 3). Conversely, having graduated from high school decreased the odds of having a detectable viral load by 63% (OR: 0.367, 95% CI: 0.185–0.728, p=0.004), and women in the 45–55 and 56 and older age groups with progressively lower odds of having a detectable viral load. Neither the all type or HIV specialty missed clinic visit outcome was associated with past year IPV (Tables 4 and 5). Past year substance use was associated with both all type and HIV specialty missed clinic visits in bivariate and adjusted models. Alcohol abuse was associated with an increased odds of missing > 33% of HIV specialty clinic visits in bivariate models only (OR: 2.737, 95% CI: 1.408–5.322, p=0.003). Current employment was protective against missing >33% of all type clinic visits (OR: 0.374, 95% CI: 0.159–0.879, p=0.024) in bivariate analysis only.
Table 2.
Logistic Regression Models for CD4 Cell Count <200cell/mm3
| CD4<200 n (%)a n=24 |
CD4 ≥200 n (%)a n=199 |
ORb (95% CI) n=223 |
p-value | aORc (95% CI) n=219 |
p-value | |
|---|---|---|---|---|---|---|
| Past Year IPV | ||||||
| No | 6 (25) | 104 (52) | Ref | - | Ref | - |
| Yes | 18 (75) | 95 (48) | 3.284 (1.251–8.619) | 0.016 | 3.536 (1.114–11.224) | 0.032 |
| Age | ||||||
| 18–35 | 3 (12) | 12 (6) | Ref | - | Ref | - |
| 36–45 | 8 (33) | 40 (20) | 0.800 (0.183–3.498) | 0.767 | 0.958 (0.130–7.060) | 0.966 |
| 46–55 | 6 (25) | 99 (50) | 0.242 (0.054–1.097) | 0.066 | 0.363(0.054–2.441) | 0.297 |
| 56 and older | 7 (29) | 48 (24) | 0.583(0.131–2.596) | 0.479 | 1.206 (0.173–8.400) | 0.850 |
| Employment status | ||||||
| Unemployed | 20 (83) | 175 (88) | Ref | - | Ref | - |
| Employed | 4 (17) | 24 (12) | 1.458 (0.459–4.630) | 0.522 | 3.174 (0.690–14.599) | 0.138 |
| Level of education [n=221] | ||||||
| < HS graduation | 9 (38) | 85 (43) | Ref | - | Ref | - |
| HS graduation or beyond | 15 (63) | 112 (57) | 1.265 (0.528–3.029) | 0.598 | 2.415 (0.793–7.355) | 0.121 |
| Alcohol abuse [n=221] | ||||||
| AUDIT <8 | 17 (71) | 163 (83) | Ref | - | Ref | - |
| AUDIT ≥8 | 7 (29) | 34 (17) | 1.974 (0.760–5.128) | 0.163 | 1.187(0.352–4.002) | 0.782 |
| Past year drug use | ||||||
| No | 8 (33) | 106 (53) | Ref | Ref | - | |
| Yes | 16 (67) | 93 (47) | 2.280 (0.933–5.569) | 0.071 | 2.377(0.764–7.398) | 0.135 |
| PTSD [n=221] | ||||||
| PCL<45 | 17 (71) | 157 (80) | Ref | - | Ref | - |
| PCL ≥45 | 7 (29) | 40 (20) | 1.161 (0.627–4.163) | 0.320 | 1.261(0.357–4.462) | 0.719 |
| Depression [n=221] | ||||||
| CES-D<16 | 16 (67) | 148 (75) | Ref | - | Ref | - |
| CES-D ≥16 | 8 (33) | 49 (25) | 1.510 (0.609–3.745) | 0.374 | 1.055 (0.298–3.731) | 0.934 |
| Viral Suppression | ||||||
| Undetectable VL | 10 (42) | 153 (77) | Ref | - | Ref | - |
| Detectable VL | 14 (58) | 46 (23) | 4.657 (1.939–11.180) | 0.001 | 5.901 (2.066–16.849) | 0.001 |
Notes: Items in bold were statistically significant. IPV: intimate partner violence; CES-D: Center for Epidemiologic Centers Scales – Depression; PCL: post-traumatic checklist; AUDIT: Alcohol Use Disorders Identification Test; Ref=reference category; n=219 women prescribed anti-retroviral therapy and with complete survey data for all included covariates.
column %
bivariate associations
adjusted for displayed covariates
Table 3.
Logistic Regression Models for Detectable Viral Load (>20 copies/ml)
| VL detectable n (%)a n=60 |
VL not detectable n (%)a n=163 |
ORb (95% CI) n=223 |
p value | aORc (95% CI) n=219 |
p value | |
|---|---|---|---|---|---|---|
| Past Year IPV | ||||||
| No | 23 (38) | 87 (53) | Ref | - | Ref | - |
| Yes | 37 (62) | 76 (47) | 1.842 (1.006–3.371) | 0.048 | 1.699 (0.859–3.363) | 0.128 |
| Age | ||||||
| 18–35 | 6 (10) | 9 (6) | Ref | - | Ref | - |
| 36–45 | 19 (32) | 29 (18) | 0.983(0.301–3.211) | 0.977 | 0.293(0.069–1.250) | 0.097 |
| 46–55 | 26 (43) | 79 (49) | 0.494(0.160–1.519) | 0.218 | 0.168(0.042–0.664) | 0.011 |
| 56 and older | 9 (15) | 46 (28) | 0.293(0.084–1.030) | 0.056 | 0.118(0.027–0.524) | 0.005 |
| Employment status | ||||||
| Unemployed | 56 (93) | 139 (85) | Ref | - | Ref | - |
| Employed | 4 (7) | 24 (15) | 0.414(0.137–1.247) | 0.117 | 0.435 (0.121–1.567) | 0.203 |
| Level of education [n=221] | ||||||
| < HS graduation | 36 (60) | 58 (36) | Ref | - | Ref | - |
| HS graduation or beyond | 24 (40) | 103 (64) | 0.375(0.204–0.690) | 0.002 | 0.367(0.185–0.728) | 0.004 |
| Alcohol abuse [n=221] | ||||||
| AUDIT <8 | 45 (76) | 135 (83) | Ref | - | Ref | - |
| AUDIT ≥8 | 14 (24) | 27 (17) | 1.556(0.751–3.223) | 0.234 | 1.356(0.575–3.196) | 0.487 |
| Past year drug use | ||||||
| No | 24 (41) | 88 (54) | Ref | - | Ref | - |
| Yes | 35 (58) | 74 (45) | 1.684(0.925–3.064) | 0.088 | 1.587 (0.782–3.222) | 0.201 |
| PTSD [n=221] | ||||||
| PCL<45 | 47 (78) | 127 (78) | Ref | - | Ref | - |
| PCL ≥45 | 12 (20) | 35 (22) | 0.926(0.444–1.934) | 0.839 | 0.558(0.218–1.430) | 0.224 |
| Depression [n=221] | ||||||
| CES-D<16 | 44 (75) | 120 (74) | Ref | - | Ref | - |
| CES-D ≥16 | 15 (25) | 42 (26) | 0.974(0.492–1.929) | 0.940 | 0.642(0.268–1.537) | 0.320 |
Notes: Items in bold were statistically significant. IPV: intimate partner violence; CES-D: Center for Epidemiologic Centers Scales – Depression; PCL: post-traumatic checklist; AUDIT: Alcohol Use Disorders Identification Test; Ref=reference category; n=219 women prescribed antiretroviral therapy and with complete survey data for all included covariates
column %
bivariate associations
adjusted for displayed covariates
Table 4.
Logistic Regression Models for Past Year All Type Missed Visit Proportion >33%
| Missed >33% of visitsa n (%) n=109 |
Missed ≤33% of visits a n (%) n=128 |
ORb (95% CI) n=237 |
p value | aORc (95% CI) n=232 |
p value | |
|---|---|---|---|---|---|---|
| Past Year IPV | ||||||
| No | 48 (44) | 69 (54) | Ref | - | Ref | - |
| Yes | 61 (56) | 59 (46) | 1.535 (0.920–2.560) | 0.101 | 1.201 (0.648–2.226) | 0.562 |
| Age | ||||||
| 18–35 | 7 (6) | 11 (9) | Ref | - | Ref | - |
| 36–45 | 33 (30) | 19 (15) | 2.729 (0.906–8.224) | 0.074 | 1.246 (0.333–4.667) | 0.744 |
| 46–55 | 46 (42) | 64 (50) | 1.129 (0.407–3.134) | 0.815 | 0.805 (0.237–2.742) | 0.729 |
| 56 and older | 23 (21) | 34 (27) | 1.155 (0.393–3.400) | 0.793 | 0.689 (0.190–2.498) | 0.571 |
| Employment status | ||||||
| Unemployed | 101 (93) | 106 (83) | Ref | - | Ref | - |
| Employed | 8 (7) | 22 (17) | 0.374 (0.159–0.879) | 0.024 | 0.482 (0.178–1.303) | 0.150 |
| Level of education [n=234] | ||||||
| < HS graduation | 45 (42) | 52 (41) | Ref | - | Ref | - |
| HS graduation or beyond | 63 (58) | 74 (59) | 0.942 (0.561–1.581) | 0.821 | 1.436 (0.762–2.706) | 0.263 |
| Alcohol abuse [n=235] | ||||||
| AUDIT <8 | 84 (78) | 106 (84) | Ref | - | Ref | - |
| AUDIT ≥8 | 24 (22) | 21 (17) | 1.409 (0.735–2.701) | 0.302 | 0.743 (0.324–1.704) | 0.483 |
| Past year drug use | ||||||
| No | 35 (32) | 83 (65) | Ref | - | Ref | - |
| Yes | 74 (68) | 45 (35) | 3.843 (2.243–6.582) | <0.001 | 4.385 (2.326–8.264) | <0.001 |
| PTSD [n=235] | ||||||
| PCL<45 | 78 (72) | 101 (80) | Ref | - | Ref | - |
| PCL ≥45 | 30 (28) | 26 (21) | 1.457 (0.798–2.658) | 0.220 | 1.180 (0.503–2.765) | 0.704 |
| Depression [n=235] | ||||||
| CES-D<16 | 74 (69) | 98 (77) | Ref | - | Ref | - |
| CES-D ≥16 | 34 (32) | 29 (23) | 1.577 (0.886–2.807) | 0.122 | 1.234 (0.540–2.818) | 0.618 |
| Number of past year scheduled visits: | ||||||
| 1–6 | 2 (2) | 10 (8) | Ref | - | Ref | - |
| 7–12 | 15 (14) | 13 (10) | 5.769 (1.064–31.270) | 0.042 | 5.404 (0.852–34.256) | 0.073 |
| 13–26 | 48 (44) | 35 (27) | 7.000 (1.443–33.948) | 0.016 | 6.216 (1.129–34.231) | 0.036 |
| 27–52 | 33 (30) | 41 (32) | 4.146 (0.850–20.227) | 0.079 | 4.011 (0.719–22.367) | 0.113 |
| 53–104 | 9 (8) | 24 (19) | 1.875 (0.342–10.269) | 0.469 | 1.337 (0.213–8.392) | 0.757 |
| 105 or more | 2 (2) | 5 (4) | 2.000 (0.214–18.687) | 0.543 | 1.299 (0.112–15.068) | 0.835 |
Notes: Items in bold were statistically significant. IPV: intimate partner violence; CES-D: Center for Epidemiologic Centers Scales – Depression; PCL: post-traumatic checklist; AUDIT: Alcohol Use Disorders Identification Test; Ref=reference category; n=232 women with complete survey data for all included covariates.
column %
bivariate associations
adjusted for displayed covariates
Table 5.
Logistic Regression Models for Past Year Missed HIV Clinic Visits Proportion >33%
| Missed >33% of visitsa n (%) n=84 |
Missed ≤33% of visits a n (%) n=148 |
ORb (95% CI) n=232 |
p value | aORc (95% CI) n=227 |
p value | |
|---|---|---|---|---|---|---|
| Past Year IPV | ||||||
| No | 39 (46) | 77 (52) | Ref | - | Ref | - |
| Yes | 45 (54) | 71 (48) | 1.251 (0.732–2.140) | 0.413 | 0.931 (0.499–1.735) | 0.821 |
| Age | ||||||
| 18–35 | 7 (8) | 11 (7) | Ref | - | Ref | - |
| 36–45 | 26 (31) | 26 (18) | 1.571 (0.527–4.685) | 0.417 | 0.938 (0.269–3.267) | 0.920 |
| 46–55 | 33 (40) | 72 (49) | 0.720 (0.256–2.024) | 0.534 | 0.519 (0.161–1.677) | 0.273 |
| 56 and older | 18 (21) | 39 (26) | 0.725 (0.241–2.179) | 0.567 | 0.601 (0.176–2.059) | 0.418 |
| Employment status | ||||||
| Unemployed | 76 (91) | 127 (86) | Ref | - | Ref | - |
| Employed | 8 (10) | 21 (14) | 0.637 (0.269–1.508) | 0.305 | 0.943 (0.354–2.512) | 0.906 |
| Level of education [n=229] | ||||||
| < HS graduation | 37 (44) | 59 (41) | Ref | - | Ref | - |
| HS graduation or beyond | 47 (56) | 86 (59) | 0.871 (0.506–1.501) | 0.620 | 1.002 (0.540–1.860) | 0.995 |
| Alcohol abuse [n=230] | ||||||
| AUDIT <8 | 58 (70) | 127 (86) | Ref | - | Ref | - |
| AUDIT ≥8 | 25 (30) | 20 (14) | 2.737 (1.408–5.322) | 0.003 | 2.057 (0.956–4.422) | 0.065 |
| Past year drug use | ||||||
| No | 26 (31) | 90 (61) | Ref | - | Ref | - |
| Yes | 58 (69) | 58 (39) | 3.462 (1.961–6.110) | <0.001 | 3.175 (1.701–5.924) | <0.001 |
| PTSD [n=230] | ||||||
| PCL<45 | 56 (70) | 116 (79) | Ref | - | Ref | - |
| PCL ≥45 | 25 (30) | 31 (21) | 1.613 (0.873–2.980) | 0.127 | 1.102 (0.496–2.450) | 0.812 |
| Depression [n=230] | ||||||
| CES-D<16 | 56 (68) | 112 (76) | Ref | - | Ref | - |
| CES-D ≥16 | 27 (33) | 35 (24) | 1.543 (0.850–2.799) | 0.154 | 1.050 (0.477–2.308) | 0.904 |
Notes: Items in bold were statistically significant. IPV: intimate partner violence; CES-D: Center for Epidemiologic Centers Scales – Depression; PCL: post-traumatic checklist; AUDIT: Alcohol Use Disorders Identification Test; Ref=reference category; n=227 women with scheduled HIV clinic visits and complete survey data for all included covariates.
column %
bivariate associations
adjusted for displayed covariates
Discussion
Intimate partner violence is associated with a myriad of health issues among women living with HIV. The finding that past year IPV was an independent predictor of CD4 count when adjusting for mental health and substance abuse covariates without any attenuation of the odds ratios adds to the current body of knowledge regarding the impact of IPV on HIV disease progression and immunologic recovery after ART initiation. While much of the published literature focuses on the behavioral impact of IPV on adherence to care—through mental health symptoms, perpetrator interference, and increased risk-taking behaviors (Campbell et al., 2008; Draughon, 2012; Jewkes, Dunkle, Nduna, & Shai, 2010), our results suggest that additional physiologic mechanisms, such as immune and inflammatory processes related to stress, should be considered (Campbell et al., 2013; Siyahhan Julnes et al., 2016). Prior researchers examining biologic stress in women who have experienced IPV have shown alterations in the inflammatory and immune system markers (Garcia-Linares, Sanchez-Lorente, Coe, & Martinez, 2004; Out, Hall, Granger, Page, & Woods, 2012; Sanchez-Lorente, Blasco-Ros, Coe, & Martinez, 2010; Shafran et al., 1996).
Missed clinic visits have also been posited to impact adherence to HIV care among women who are experiencing IPV, and IPV has been linked to delated entry to care and avoidance of care seeking in multiple care settings (Duterte et al., 2008; Fugate, Landis, Riordan, Naureckas, & Engel, 2005; Hatcher et al., 2015; Illangasekare et al., 2012; Schafer et al., 2012). While we did not find a relationship between IPV and missed clinic visits in this sample, it is likely that the high overall no show rate among study participants and the strong relationship between substance use and missed visits contributed to this finding. This finding suggests that while interventions to encourage clinic attendance and retention in care are necessary, IPV may not be the direct driver of missed visits. Instead, comprehensively understanding and addressing the complex interactions between violence, substance use, and mental health is needed in such interventions.
Our results also highlighted the impact of IPV on both physical and mental health outcomes on women living with HIV. Higher rates of reported depressive and PTSD symptoms were reported by women who reported recent IPV. Yet contrary to previous work in which depression and PTSD have been associated with altered immune function and increased morbidity and mortality among patients living with HIV, in our sample these mental health symptoms were not associated with measured laboratory outcomes (Chander, Himelhoch, & Moore, 2006; Cruess et al., 2003; Leserman, 2003; Machtinger et al., 2012; Siyahhan Julnes et al., 2016). Multiple factors may have contributed to the lack of significance of this relationship in our results, primarily sample size and the use of CD4 count as the only measure of immune status. Assessment of additional biomarkers and a larger sample which allows for statistical assessment of the interactions between IPV, depression, PTSD and substance abuse may provide more insight into these relationships (Tsai & Venkataramani, 2016).
This study also found that past year IPV rates were higher in this sample than previously reported in the same HIV clinic setting—51% versus 26.5% (Illangasekare et al., 2012). This is likely related to differences in the chosen definition and measurement of IPV used in this study compared to the prior estimate. Specifically, women were allowed to self-identify their partner status and were not required to report being married or co-habitating in this study, but rather in a relationship (i.e., married, dating, living together, hooking up, etc.). This definition likely increased the number of women who reported being partnered in the past year. Similarly, we included multiple items and measures to capture psychological abuse and physical and sexual violence in order to holistically capture the spectrum of women’s experiences. This is in contrast to a previously reported study conducted in the clinic that included only one tool consisting of three items, the Partner Violence Screen (Feldhaus et al., 1997; Illangasekare et al., 2012). Women were also informed of this study’s focus on relationships and violence during the consent process, possibly raising their sensitivity to the issue.
Limitations
Cross-sectional data limits any inferences regarding causation. Particularly with regards to measuring both CD4 count and viral load at only one time point, it is not possible to determine whether the overall trajectory of a participants’ HIV disease was improving or deteriorating, and whether the rate of improvement or deterioration was consistent with what would be expected based on time since diagnosis, time on ART and time since achieving viral suppression. Further confounding of these outcomes is possible related to limitations in survey measures to capture trajectories of IPV, mental health symptoms and treatment, and substance use over time. Reliance on survey measures for these SAVA syndemic variables also introduces opportunities for recall and social desirability bias. Participant-entered electronic data collection and discussion of the separation of the research and clinical data during the consent process were utilized to minimize this bias and data entry error. Multiple other life stressors and traumas were outside the scope of this study, but have similar theoretical links to negative outcomes related to chronic stress response. Given the demographics of sample and study location, there is likely a great deal of unmeasured trauma history among this study’s participants, including childhood trauma, community violence and incarceration that could have confounded our results related to the relationship between SAVA variables and HIV treatment outcomes. The complex multidirectional relationships between trauma, mental health, substance use, and immune function need much additional examination. Future work needs to include opportunities in data collection and analysis to account for the cumulative impacts of lifetime trauma.
Clinical Implications
This study’s results add to the growing literature regarding HIV care outcomes for women experiencing violence. Previous work has shown IPV to be associated with a lower likelihood of being prescribed and adhering to ART (Hatcher et al., 2015), while our findings suggest that additional physiologic mechanisms may also be contributing to poorer HIV outcomes. Further, as the study clinic functions as a patient centered medical home with co-located mental health and substance abuse treatment services, it may be that our finding of higher viral suppression than other published studies is impacted by the clinical setting. Despite widespread support and recommendations from professional and regulatory organizations, universal assessment for IPV is not consistently implemented in HIV care settings. Too often, IPV assessment consists of only a single question and may be asked without eye contact or without privacy. Our findings suggest that a longer screening tool, even slightly longer such as the AAS, delivered via computer may increase disclosure substantially. Trauma-informed programs, which include raising awareness of the relationship between IPV and health, confidential and non-judgmental assessment of psychological abuse, physical and sexual violence, harm reduction, safety planning and referrals to community partners and advocates integrated in all levels of clinical services, are also essential in HIV clinic environments in which multiple medical and social factors are impacting patients’ health and well-being (Machtinger, Cuca, et al., 2015; Machtinger, Lavin, et al., 2015). This becomes particularly important given our results and those of similar work examining the impact of broader trauma experiences and PTSD on immune and inflammatory markers on patients living with HIV, as patients may be virally suppressed and still experiencing immune dysfunction as a result of trauma-related factors (Siyahhan Julnes et al., 2016).
Syndemic models demand that in order to intervene or promote change in one area of the syndemic, full attention must be paid to the other aspects. In particular, the viral load and missed visit outcomes can be viewed through a syndemic lens and in conjunction with previous work conducted regarding IPV, entry to care, and medication adherence. The missed visit outcome showed significant relationships with past year drug use, and recent work examining PTSD found links to immune and inflammatory biomarkers in a sample of virally suppressed patients living with HIV (Siyahhan Julnes et al., 2016). Each of these factors can have negative downstream impact on women’s health. In addition to implementing universal patient and provider education with a focus on the impact of violence and trauma on health in HIV care settings, addressing IPV and trauma history through community referrals is an avenue for intervention. The finding that women experiencing IPV in our sample were not more likely to have high clinic no show rates highlights the important role that clinical settings have in addressing the impact of violence on their patients’ health. While the high overall rate of missed visits leave opportunities for additional intervention to improve adherence to care broadly. Developing or strengthening partnerships with community resources and incorporating trauma-informed mental health, substance abuse and violence services into standard HIV care presents an opportunity to address these issues of utmost importance to patients’ health and well-being.
Conclusions
This study’s findings support both biologic and behavioral pathways through which IPV can impact women’s HIV care and outcomes. While the cumulative impact of IPV and other lifetime experiences of trauma on the immune system are not yet fully known, additional research is needed to further examine the multiple physiologic pathways that may contribute to increased risk of low CD4 count in these women. With a better understanding of the specific biologic changes and timelines in which their impacts are realized, we may begin to examine methods and opportunities for interrupting these changes and developing biobehavioral interventions to address IPV in the context of HIV and other SAVA syndemic factors such as substance use and mental health symptoms. The high prevalence of IPV and its impact on CD4 counts also demands close attention to identifying and addressing ongoing sources of violence in patients’ lives in order to comprehensively address the care of women living with HIV.
Acknowledgments
Funding Details: This work was supported by the National Institute of Mental Health under grant F31MH100995; the National Institute of Allergy and Infectious Diseases under grant 1P30AI094189; and the National Institute of Child Health and Development under grant T32HD087162.
Footnotes
Disclosure statement: The authors have no conflicts of interest to disclose.
Contributor Information
Jocelyn C. Anderson, Johns Hopkins University School of Nursing, 525 N. Wolfe St., Baltimore, MD 21205.
Jacquelyn C. Campbell, Johns Hopkins University School of Nursing, 525 N. Wolfe St., Baltimore, MD 21205, 410 955-2778.
Nancy E. Glass, Johns Hopkins University School of Nursing, 525 N. Wolfe St., Baltimore, MD 21205.
Michele R. Decker, Johns Hopkins Bloomberg School of Public Health, Department of Population, Family and Reproductive Health, 615 N. Wolfe Street, E4142, Baltimore, MD 21205, Ph. 410.502.2747.
Nancy Perrin, Johns Hopkins University School of Nursing, 525 N. Wolfe St., Baltimore, MD 21205.
Jason Farley, Johns Hopkins University School of Nursing, Johns Hopkins University School of Medicine, 525 N. Wolfe Street, SON House Room 204; Baltimore, MD 21205, 410-502-7563.
References
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. The alcohol use disorders identification test guidelines for use in primary care. Geneva: World Health Organization; 2001. [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD checklist (PCL) Behaviour Research and Therapy. 1996;34(8):669–673. doi: 10.1016/0005-7967(96)00033-2. 0005-7967(96)00033-2 [pii] [DOI] [PubMed] [Google Scholar]
- Bohn MJ, Babor TF, Kranzler HR. The alcohol use disorders identification test (AUDIT): Validation of a screening instrument for use in medical settings. Journal of Studies on Alcohol. 1995;56(4):423–432. doi: 10.15288/jsa.1995.56.423. [DOI] [PubMed] [Google Scholar]
- Campbell JC, Baty ML, Ghandour RM, Stockman JK, Francisco L, Wagman J. The intersection of intimate partner violence against women and HIV/AIDS: A review. International Journal of Injury Control and Safety Promotion. 2008;15(4):221–231. doi: 10.1080/17457300802423224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campbell JC, Lucea MB, Stockman JK, Draughon JE. Forced sex and HIV risk in violent relationships. American Journal of Reproductive Immunology. 2013;69(Suppl 1):41–44. doi: 10.1111/aji.12026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chander G, Himelhoch S, Moore RD. Substance abuse and psychiatric disorders in HIV-positive patients: Epidemiology and impact on antiretroviral therapy. Drugs. 2006;66(6):769–789. doi: 10.2165/00003495-200666060-00004. [DOI] [PubMed] [Google Scholar]
- Cruess DG, Petitto JM, Leserman J, Douglas SD, Gettes DR, Ten Have TR, Evans DL. Depression and HIV infection: Impact on immune function and disease progression. CNS Spectrum. 2003;8(1):52–58. doi: 10.1017/s1092852900023452. [DOI] [PubMed] [Google Scholar]
- Draughon JE. Sexual assault injuries and increased risk of HIV transmission. Advanced Emergency Nursing Journal. 2012;34(1):82–87. doi: 10.1097/TME.0b013e3182439e1a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duterte EE, Bonomi AE, Kernic MA, Schiff MA, Thompson RS, Rivara FP. Correlates of medical and legal help seeking among women reporting intimate partner violence. J Womens Health (Larchmt) 2008;17(1):85–95. doi: 10.1089/jwh.2007.0460. [DOI] [PubMed] [Google Scholar]
- Feldhaus KM, Koziol-McLain J, Amsbury HL, Norton IM, Lowenstein SR, Abbott JT. Accuracy of 3 brief screening questions for detecting partner violence in the emergency department. Journal of the American Medical Association. 1997;277(17):1357–1361. [PubMed] [Google Scholar]
- Fugate M, Landis L, Riordan K, Naureckas S, Engel B. Barriers to domestic violence help seeking: implications for intervention. Violence Against Women. 2005;11(3):290–310. doi: 10.1177/1077801204271959. [DOI] [PubMed] [Google Scholar]
- Garcia-Linares MI, Sanchez-Lorente S, Coe CL, Martinez M. Intimate male partner violence impairs immune control over herpes simplex virus type 1 in physically and psychologically abused women. Psychosomatic Medicine. 2004;66(6):965–972. doi: 10.1097/01.psy.0000145820.90041.c0. [DOI] [PubMed] [Google Scholar]
- Hatcher AM, Smout EM, Turan JM, Christofides N, Stockl H. Intimate partner violence and engagement in HIV care and treatment among women: A systematic review and meta-analysis. AIDS. 2015;29(16):2183–2194. doi: 10.1097/QAD.0000000000000842. [DOI] [PubMed] [Google Scholar]
- IBM. IBM SPSS Statistics for Windows (Version 23.0) Armonk, NY: IBM Corporation; 2014. [Google Scholar]
- Illangasekare S, Tello M, Hutton H, Moore R, Anderson J, Baron J, Chander G. Clinical and mental health correlates and risk factors for intimate partner violence among HIV-positive women in an inner-city HIV clinic. Women’s Health Issues. 2012;22(6):e563–569. doi: 10.1016/j.whi.2012.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Interagency Federal Working Group. Addressing the Intersection of HIV/AIDS Violence Against Women and Girls and Gender-Related Health Disparities. Washington, DC: The White House; 2013. [Google Scholar]
- Jewkes RK, Dunkle K, Nduna M, Shai N. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: A cohort study. Lancet. 2010;376(9734):41–48. doi: 10.1016/S0140-6736(10)60548-X. S0140-6736(10)60548-X [pii] [DOI] [PubMed] [Google Scholar]
- Leserman J. HIV disease progression: Depression, stress, and possible mechanisms. Biological Psychiatry. 2003;54(3):295–306. doi: 10.1016/s0006-3223(03)00323-8. S0006322303003238. [DOI] [PubMed] [Google Scholar]
- Machtinger EL, Cuca YP, Khanna N, Rose CD, Kimberg LS. From treatment to healing: The promise of trauma-informed primary care. Women’s Health Issues. 2015;25(3):193–197. doi: 10.1016/j.whi.2015.03.008. [DOI] [PubMed] [Google Scholar]
- Machtinger EL, Haberer JE, Wilson TC, Weiss DS. Recent trauma is associated with antiretroviral failure and HIV transmission risk behavior among HIV-positive women and female-identified transgenders. AIDS and Behavior. 2012;16(8):2160–2170. doi: 10.1007/s10461-012-0158-5. [DOI] [PubMed] [Google Scholar]
- Machtinger EL, Lavin SM, Hilliard S, Jones R, Haberer JE, Capito K, Dawson-Rose C. An expressive therapy group disclosure intervention for women living with HIV improves social support, self-efficacy, and the safety and quality of relationships: A qualitative analysis. Journal of the Association of Nurses in AIDS Care. 2015;26(2):187–198. doi: 10.1016/j.jana.2014.05.001. [DOI] [PubMed] [Google Scholar]
- Marshall LL. Development of the severity of violence against women scales. Journal of Family Violence. 1992;7(2):103–121. [Google Scholar]
- McFarlane J, Parker B, Soeken K, Bullock L. Assessing for abuse during pregnancy. Severity and frequency of injuries and associated entry into prenatal care. Journal of the American Medical Association. 1992;267(23):3176–3178. doi: 10.1001/jama.267.23.3176. [DOI] [PubMed] [Google Scholar]
- Micallef L, Rodgers P. eulerAPE: drawing area-proportional 3-Venn diagrams using ellipses. PLoS One. 2014;9(7):e101717. doi: 10.1371/journal.pone.0101717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Out D, Hall RJ, Granger DA, Page GG, Woods SJ. Assessing salivary C-reactive protein: Longitudinal associations with systemic inflammation and cardiovascular disease risk in women exposed to intimate partner violence. Brain Behavior and Immunity. 2012;26(4):543–551. doi: 10.1016/j.bbi.2012.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977 doi: 10.1177/014662167700100306. [DOI] [Google Scholar]
- Ruggiero KJ, Del Ben K, Scotti JR, Rabalais AE. Psychometric properties of the PTSD checklist-civilian version. Journal of Trauma and Stress. 2003;16(5):495–502. doi: 10.1023/A:1025714729117. [DOI] [PubMed] [Google Scholar]
- Sanchez-Lorente S, Blasco-Ros C, Coe CL, Martinez M. Recovery of immune control over herpes simplex virus type 1 in female victims of intimate partner violence. Psychosomatic Medicine. 2010;72(1):97–106. doi: 10.1097/PSY.0b013e3181c5080a. [DOI] [PubMed] [Google Scholar]
- Schafer KR, Brant J, Gupta S, Thorpe J, Winstead-Derlega C, Pinkerton R, … Dillingham R. Intimate partner violence: A predictor of worse HIV outcomes and engagement in care. AIDS Patient Care and STDS. 2012;26(6):356–365. doi: 10.1089/apc.2011.0409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shafran SD, Singer J, Zarowny DP, Phillips P, Salit I, Walmsley SL, … Tsoukas CM. A comparison of two regimens for the treatment of mycobacterium avium complex bacteremia in AIDS: rifabutin, ethambutol, and clarithromycin versus rifampin, ethambutol, clofazimine, and ciprofloxacin. Canadian HIV Trials Network Protocol 010 Study Group. New England Journal of Medicine. 1996;335(6):377–383. doi: 10.1056/NEJM199608083350602. [DOI] [PubMed] [Google Scholar]
- Singer M. AIDS and the health crisis of the U.S. urban poor: The perspective of critical medical anthropology. Social Science & Medicine. 1994;39(7):931–948. doi: 10.1016/0277-9536(94)90205-4. [DOI] [PubMed] [Google Scholar]
- Singer M. A dose of drugs, a touch of violence, a case of AIDS: Conceptualizing the SAVA syndemic. Free Inquiry in Creative Sociology. 1996;24(2):99–110. [Google Scholar]
- Singer M. Introduction to syndemics: A systems approach to public and community health. San Francisco, CA: Jossey-Bass; 2009. [Google Scholar]
- Siyahhan Julnes P, Auh S, Krakora R, Withers K, Nora D, Matthews L, … Kapetanovic S. The association between post-traumatic stress disorder and markers of inflammation and immune activation in HIV-infected individuals with controlled viremia. Psychosomatics. 2016 doi: 10.1016/j.psym.2016.02.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skinner HA. The drug abuse screening test. Addictive Behaviors. 1982;7(4):363–371. doi: 10.1016/0306-4603(82)90005-3. [DOI] [PubMed] [Google Scholar]
- Tsai AC, Venkataramani AS. Syndemics and health disparities: A methodological note. AIDS and Behavior. 2016;20(2):423–430. doi: 10.1007/s10461-015-1260-2. [DOI] [PMC free article] [PubMed] [Google Scholar]