Abstract
Background and Objective:
Central nervous system (CNS) relapse of diffuse large B cell lymphoma (DLBCL) is relatively uncommon and nearly fatal. Two years CNS relapse risk is 0.8% in low, 3.9% in intermediate and 12% in high risk patients. Our aim was to study, the baseline characteristics and outcome in term of median survival of DLBCL patients with CNS relapse.
Methods:
This is a retrospective analysis. All patients of DLBCL with CNS relapse from 2006 to 2014 were included. Data were collected from computerized Hospital Information System and analyzed for characteristics and median survival.
Results:
Out of twenty one patients included in the study, 14(66.3%) males and 7(33.7%) were females. On initial diagnosis of DLBCL, median age was 37.4 years (27-47). Ann Arbor stage of I-IV was in 3 (14.3%), 2(9.5%), 4(19%) and 12(57.1%) patients, respectively. Extra-nodal involvement was noted in 16(76.2%), high LDH in 18(85.7%), bone marrow involvement in 8(38.1%) and bulky disease in 5(23.8%) patients. International Prognostic Index (IPI) score was 1 in 4(19%), 2 in 9(42.9%), 3 in 8(38.1%) patients. Extra-nodal sites were gut in 2(9.1%) while 1(4.5%) patient of each of following organs involvement was seen: cervix, gluteal muscle, iliac bone, liver, ovaries, pancreas, parotid gland and testes. Chemotherapy CHOP was given to 16(76.2%) and RCHOP in 5(23.8%) patients. Prophylactic intrathecal methotrexate was given to 10(47.6%) patients. Complete response was in 10 (47.6%), partial response was in 3 (14.3%) and disease progression was in 8 (38.1%) patients. CNS relapse occurred in 17 (81%) patients within six months after completion of therapy. CNS relapse along with systemic disease was in 14(66.6%) patients. Isolated CNS relapse was noted in 7(33.3%) patients. Second line chemotherapy regimens were HDMTX 5(23.8%), HDMTX/TRIO IT 3(14.2%), HDMTX/HDAC 2(9.5%), HCVAD 3(14.2%), ICE 4(19.4%), DHAP 1(4.7%), ICE/HDMTX 1(4.7%), none 2(9.5%). Overall median survival of CNS relapsed patients was 54 days.
Conclusion:
Patients with DLBCL who had advanced stage, high LDH and extra-nodal involvement at initial presentation are at high risk for CNS relapse. About half of the patients had CNS relapse despite primary CNS prophylaxis. Once relapsed in CNS, these patients have very poor prognosis.
Keywords: CNS relapse, Chemotherapy, Survival, Prophylaxis
INTRODUCTION
Diffuse large B-cell lymphoma (DLBCL) is the most common lymphoid neoplasms in adults; accounting for approximately 32.5% of NHLs diagnosed annually.1 Secondary central nervous system (CNS) involvement in DLBCL includes an isolated CNS relapse or CNS involvement with systemic disease. This rare but fatal clinical problem is a therapeutic dilemma in the management of DLBCL.2 In DLBCL, the incidence of CNS relapse is 2.2% to 5% and 1.6% as isolated CNS relapse. Most relapses occur with a median duration of less than one year from the time of initial diagnosis.3-6 There is association of increased risk for developing CNS relapse in patients with elevated LDH, ≥2 extranodal sites and involvement of specific extranodal sites (testes, paranasal sinus, breast and bone marrow) on initial presentation.7-9 There is a validated prognostic model to predict the risk of CNS relapse utilizing five clinical factors (age > 60 years, LDH > normal, stage III or IV, ECOG PS >1, and involvement of the kidney or adrenal gland) thus recommending for CNS prophylaxis therapy.10,11 Risk of CNS relapse is higher in activated B-cell (ABC) than germinal center B-cell (GCB).12,13 Addition of rituximab to chemotherapy (CHOP) may improve the remission rate and overall survival of patients with DLBCL. However, question about risk reduction of CNS relapse with rituximab still remains unanswered with mixed results.14 There is no strong evidence that supports any single approach for CNS prophylaxis.15 Intrathecal methotrexate given at least once per systemic treatment cycle has been used for many years however, high-dose IV methotrexate-based prophylaxis may lower incidence of CNS relapses.16-19
Aim of this study was to reveal the baseline characteristics and risk factors associated with CNS relapse in patients with DLBCL. We also looked at the overall survival of these patients and impact of intrathecal chemotherapy.
METHODS
This is a retrospective analysis of total DLBCL twenty one patients treated at our institute. All patients of DLBCL with CNS relapse from 2006 to 2014 were included. Data were collected from Hospital Information System and analyzed for characteristics and median survival.
Statistical analysis
The data were analyzed using Statistical Package for Social Sciences (SPSS) version 19. Descriptive statistics were performed. Categorical data such as gender, LDH, extra nodal site involvement, bone marrow Involvement, bulky disease, IPI score, stage of disease, chemotherapy, response to chemotherapy were presented as frequency and percentage. Quantitative variables including age were mentioned as mean ± standard deviation. Base line characteristics were compared by using chi square test. Survival was measured by Kaplan-Meier curves. P-value less than 0.05 were considered significant.
RESULTS
Out of twenty one patients included in the study, 14(66.3%) males and 7(33.7%) were females. On initial diagnosis of DLBCL, median age was 37.4 years (27-47). Stage IV was in 12(57.1%) patients; whereas 4(19.0%), 2(9.5%) and 3 (14.3%) patients had stage III, II, I disease, respectively. Extra-nodal involvement was in 16(76.2%), high LDH in 18(85.7%), bone marrow involvement in 8(38.1%) and bulky disease in 5(23.8%) patients. International Prognostic Index (IPI) was 1 in 4(19%), 2 in 9(42.9%), 3 in 8(38.1%) patients (Table-I). Extra-nodal sites were gut in 2(9.1%) while one (4.5%) patient each had the following organs involvement; cervix, gluteal muscle, iliac bone, liver, ovaries, pancreas, parotid gland and testes. Chemotherapy CHOP was given to 16(76.2%), RCHOP 5(23.8%) patients. Prophylactic intrathecal methotrexate was given to 10(47.6%) patients.
Table-I.
Baseline characteristics of study participants.
| Baseline Characteristics (at time of diagnosis) | Mean ± SD or N (%) |
|---|---|
| Age (Years) | 37.41 ± 10.14 |
| Gender | |
| Male | 14 (66.7%) |
| Female | 07 (33.3%) |
| Stage of Disease | |
| I | 3 (14.3%) |
| II | 2 (9.5%) |
| III | 4 (19.0%) |
| IV | 12 (57.1%) |
| LDH | |
| High | 18 (85.7%) |
| Normal | 03 (14.3%) |
| Extra Nodal site involvement | |
| None | 5 (23.8%) |
| Yes | 16 (76.2%) |
| Bulky Disease | |
| Yes | 5 (23.8%) |
| No | 16 (76.2%) |
| Bone Marrow Involvement | |
| Yes | 8 (38.1%) |
| No | 13 (61.9%) |
| IPI | |
| 1 | 04 (19.0%) |
| 2 | 09 (42.9%) |
| 3 | 08 (38.1%) |
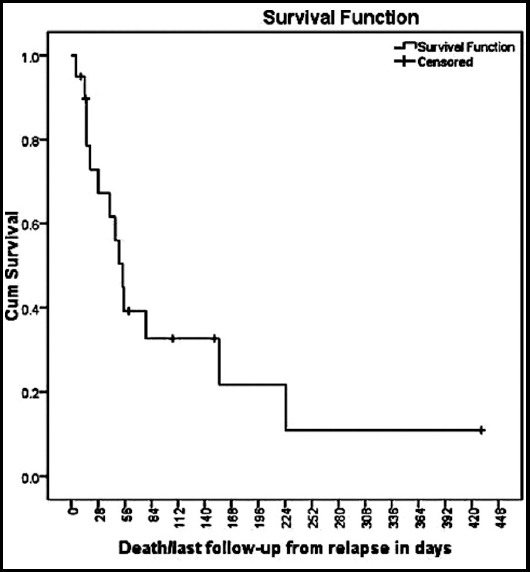
Complete response to chemotherapy was seen in 10 (47.6%), partial response in 3 (14.3%) and disease progression was seen in 8 (38.1%) patients. CNS relapse occurred in 17 (81%) patients within six months after completion of therapy. CNS relapse along with systemic disease was noted in 14(66.6%) patients. Isolated CNS relapse occurred in 7(33.3%) patients. Second line chemotherapy regimens were High Dose Methotrexate5 (23.8%), HDMTX/TRIO IT 3(14.2%), HDMTX/HDAC 2(9.5%), HCVAD 3(14.2%), ICE 4(19.4%), DHAP 1(4.7%), ICE/HDMTX 1(4.7%), none 2(9.5%) (Table-II). Overall median survival of patients with CNS relapse was 54 days (Fig.1). No characteristics were statistically significant when calculated with chi square test. At time of analysis only one patient was alive.
Table-II.
Subsequent second line chemotherapy.
| Second line Chemotherapy | n(%) |
|---|---|
| HDMTX | 5(23.8%) |
| High dose methotrexate | |
| HDMTX/TRIO IT | 3(14.2%) |
| High dose methotrexate/Methoreaxte, Cytrabine, Hydrocortisone | |
| HDMTX/HDAC | 2(9.5%) |
| High dose methotrexate/High dose Ara-C | |
| HCVAD Hyperfractionated cylcophospahmide, vincristine, doxorubicin, dexamethasone | 3(14.2%) |
| ICE | 4(19.4%) |
| Ifosphamide, carboplatin, etoposide | |
| DHAP | 1(4.7%) |
| Dexamethasone, High dose Ara-C, Cisplatin | |
| ICE/HDMTX | 1(4.7%) |
| Ifosphamide, carboplatin, etoposide/ High dose methotrexate | |
| None | 2(9.5%) |
| Total | 21 |
Fig.1.
DISCUSSION
In our study, most of the patients were young, advance staged and with high LDH. Only one patient had testicular involvement that is considered as high risk for CNS relapse. Patients who received rituximab along with conventional chemotherapy also developed CNS relapse. In a systematic review it is found that the use of rituximab has not influenced the incidence of CNS relapse compared with the use of CHOP.20 However, few reports have shown some benefit of adding rituximab to initial therapy.21 Most of the patients developed relapse within six months of the initial treatment that is consistent with published data.3-6 In this study, isolated CNS relapse (33%) which is higher than the available data.4,22 Identifying high risk population with aid of prognostic models like CNS-IPI10,11 and addition of different combinations of CNS directed therapy may help to improve survival in these patients. In our study, majority of patients with CNS relapse had advance stage disease (III/IV), extranodal disease, high LDH and bone marrow involvement, which are considered as high risk population.9 About half of patients who had CNS relapse, they had received CNS prophylaxis. This is consistent with established fact that intrathecal MTX may not reduce the risk in all high risk patients. High dose systemic methotrexate and cytarabine had been used as prophylaxis with mixed results.16 None of our patient received systemic high dose methotrexate, which has been advocated recently in many studies.17,18 As there is no current standard validated treatment of CNS relapse15, different salvage chemotherapeutic regimens were used according to patient tolerance status. Most of the patients died during second line treatment with very short median survival. Median survival in our study is short compared to available data, which could be due to poor tolerance to salvage chemotherapy in our population and late diagnosis, due to various reasons. If relapse in CNS occurs, then high dose therapy with autologous stem cell transplant can improve survival and this approach has shown better survival in isolated CNS relapse in comparison to CNS relapse with systemic disease.23 Our patients with CNS relapse were potential candidate for HDT/ACST but unfortunately, none of these patients could survive to reach that point except one who underwent autologous stem cell transplant on first relapse and allotransplant after second CNS relapse.
CONCLUSION
Patients with DLBCL who had advanced stage, high LDH and extra-anodal involvement at initial presentation are at high risk for CNS relapse. Once relapsed in CNS, these patients have very poor prognosis. High risk patients may have CNS relapse despite intrathecal chemotherapy prophylaxis.
ACKNOWLEDGMENT
We are grateful to Dr. Farhana Badar for assistance with statistical analysis, and Dr. Sheeraz Ali who reviewed this paper which improved the manuscript significantly.
Footnotes
Grant Support & Financial Disclosures: None.
Disclosures of conflict of interest: Authors do not have any conflict of interest in the publication of this article.
Authors’ Contribution
AN and AH: Conceived, designed and writing / editing of manuscript.
F: Data collection and Statistical analysis.
AH and NS: Review, editing and final approval of manuscript.
References
- 1.Al-Hamadani M, Habermann TM, Cerhan JR, Macon WR, Maurer MJ, Go RS. Non-Hodgkin lymphoma subtype distribution, geodemographic patterns, and survival in the US:A longitudinal analysis of the National Cancer Data Base from 1998 to 2011. Am J Hematol. 2015;90:790–795. doi: 10.1002/ajh.24086. doi:10.1002/ajh.24086. [DOI] [PubMed] [Google Scholar]
- 2.Kim SJ, Oh SY, Kim JS, Kim H, Lee GW, Won JH, et al. Secondary central nervous system (CNS) involvement in patients with diffuse large B-cell lymphoma:a therapeutic dilemma. Ann Hematol. 2011;90(5):539–546. doi: 10.1007/s00277-010-1104-0. doi:10.1007/s00277-010-1104-0. [DOI] [PubMed] [Google Scholar]
- 3.Boehme V, Zeynalova S, Kloess M, Loeffler M, Kaiser U, Pfreundschuh M, et al. Incidence and risk factors of central nervous system recurrence in aggressive lymphoma--a survey of 1693 patients treated in protocols of the German High-Grade Non-Hodgkin's Lymphoma Study Group (DSHNHL) Ann Oncol. 2007;18(1):149–157. doi: 10.1093/annonc/mdl327. doi:10.1093/annonc/mdl327. [DOI] [PubMed] [Google Scholar]
- 4.Haioun C, Besson C, Lepage E, Thieblemont C, Simon D, Rose C, et al. Incidence and risk factors of central nervous system relapse in histologically aggressive non-Hodgkin's lymphoma uniformly treated and receiving intrathecal central nervous system prophylaxis:a GELA study on 974 patients. Groupe d'Etudes des Lymphomes de l'Adulte. Ann Oncol. 2000;11(6):685–690. doi: 10.1023/a:1008394827806. doi:10.1023/A:1008394827806. [DOI] [PubMed] [Google Scholar]
- 5.Guirguis HR, Cheung MC, Mahrous M, Piliotis E, Berinstein N, Imrie KR, et al. Impact of central nervous system (CNS) prophylaxis on the incidence and risk factors for CNS relapse in patients with diffuse large B-cell lymphoma treated in the rituximab era:a single centre experience and review of the literature. Br J Haematol. 2012;159(1):39–49. doi: 10.1111/j.1365-2141.2012.09247.x. doi:10.1111/j.1365-2141.2012.09247.x. [DOI] [PubMed] [Google Scholar]
- 6.Rocha TMBDS, Costa FS, Pinto MSG, Silva ICD, Paes RP, Chiattone CS. Secondary infiltration of the central nervous system in patients with diffuse large B-cell lymphoma. Rev Bras Hematol Hemoter. 2013;35(4):256–262. doi: 10.5581/1516-8484.20130094. doi:10.5581/1516-8484.20130094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Zucca E, Conconi A, Mughal TI, Sarris AH, Seymour JF, Vitolo U, et al. Patterns of outcome and prognostic factors in primary large-cell lymphoma of the testis in a survey by the International Extranodal Lymphoma Study Group. J Clin Oncol. 2003;21:20–27. doi: 10.1200/JCO.2003.11.141. doi:10.1200/JCO.2003.11.141. [DOI] [PubMed] [Google Scholar]
- 8.Laskin JJ, Savage KJ, Voss N, Gascoyne RD, Connors JM. Primary paranasal sinus lymphoma:natural history and improved outcome with central nervous system chemoprophylaxis. Leuk Lymphoma. 2005;46:1721–1727. doi: 10.1080/17402520500182345. doi:10.1080/17402520500182345. [DOI] [PubMed] [Google Scholar]
- 9.Shimazu Y, Notohara K, Ueda Y. Diffuse large B-cell lymphoma with central nervous system relapse:prognosis and risk factors according to retrospective analysis from a single-center experience. Int J Hematol. 2009;89:577–583. doi: 10.1007/s12185-009-0289-2. doi:10.1007/s12185-009-0289-2. [DOI] [PubMed] [Google Scholar]
- 10.Schmitz N, Zeynalova S, Nickelsen M, et al. A new prognosticmodel to assess the risk of CNS disease in patients with aggressive B-cell lymphoma. Hematol Oncol. 2013;31(Suppl 1) Abstract 047. doi:10.1002/hon.2057. [Google Scholar]
- 11.Savage KJ, Zeynalova S, Kansara RR, Nickelsen M, Villa D, Sehn LH, et al. Validation of a prognostic model to assess the risk of CNS disease in patients with aggressive B-cell lymphoma. Blood. 2014;124:394. [Google Scholar]
- 12.Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016;127(20):2375–2390. doi: 10.1182/blood-2016-01-643569. doi:10.1182/blood-2016-01-643569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Savage KJ, Slack GW, Mottok A, Sehn LH, Villa D, Kansara R, et al. Impact of dual expression of MYC and BCL2 by immunohistochemistry on the risk of CNS relapse in DLBCL. Blood. 2016;127(18):2182–2188. doi: 10.1182/blood-2015-10-676700. doi:10.1182/blood-2015-10-676700. [DOI] [PubMed] [Google Scholar]
- 14.Law MF, Chan HN, Lai HK, Ha CY, Ng C, Yeung YM, et al. Effects of addition of rituximab to chemotherapy on central nervous system events in patients with diffuse large B-cell lymphoma. Mol Clin Oncol. 2015;3(4):747–752. doi: 10.3892/mco.2015.546. doi:10.3892/mco.2015.546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zahid MF, Khan N, Hashmi SK, Kizilbash SH, Barta SK. Central nervous system prophylaxis in diffuse large B-cell lymphoma. Eur J Haematol. 2016;97(2):108–120. doi: 10.1111/ejh.12763. doi:10.1111/ejh.12763. [DOI] [PubMed] [Google Scholar]
- 16.Abramson JS, Hellmann M, Barnes JA, Hammerman P, Toomey C, Takvorian T, et al. Intravenous methotrexate as central nervous system (CNS) prophylaxis is associated with a low risk of CNS recurrence in high-risk patients with diffuse large B-cell lymphoma. Cancer. 2010;116(18):4283–4290. doi: 10.1002/cncr.25278. doi:10.1002/cncr.25278. [DOI] [PubMed] [Google Scholar]
- 17.Holte H, Leppa S, Bjorkholm M, Fluge O, Jyrkkio S, Delabie J, et al. Dose-densified chemoimmunotherapy followed by systemic central nervous system prophylaxis for younger high-risk diffuse large B-cell/follicular grade 3 lymphoma patients:results of a phase II Nordic Lymphoma Group study. Ann Oncol. 2013;24(5):1385–1392. doi: 10.1093/annonc/mds621. doi:10.1093/annonc/mds621. [DOI] [PubMed] [Google Scholar]
- 18.Cheah CY, Herbert KE, O'Rourke K, Kennedy GA, George A, Fedele PL, et al. A multicentre retrospective comparison of central nervous system prophylaxis strategies among patients with high-risk diffuse large B-cell lymphoma. Br J Cancer. 2014;111(6):1072–1079. doi: 10.1038/bjc.2014.405. doi:10.1038/bjc.2014.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ferreri AJ, Bruno-Ventre M, Donadoni G, Ponzoni M, Citterio G, Foppoli M, et al. Risk-tailored CNS prophylaxis in a mono-institutional series of 200 patients with diffuse large B-cell lymphoma treated in the rituximab era. Br J Haematol. 2015;168(5):654–662. doi: 10.1111/bjh.13194. doi:10.1111/bjh.13194. [DOI] [PubMed] [Google Scholar]
- 20.Ghose A, Elias HK, Guha G, Yellu M, Kundu R, Latif T. Influence of Rituximab on Central Nervous System Relapse in Diffuse Large B-Cell Lymphoma and Role of Prophylaxis-A Systematic Review of Prospective Studies. Clin Lymphoma Myeloma Leuk. 2015;15(8):451–457. doi: 10.1016/j.clml.2015.02.026. doi:10.1016/j.clml.2015.02.026. [DOI] [PubMed] [Google Scholar]
- 21.Gregory G, Arumugaswamy A, Leung T, Chan KL, Abikhair M, Tam C, et al. Rituximab is associated with improved survival for aggressive B cell CNS lymphoma. Neuro Oncol. 2013;15(8):1068–1073. doi: 10.1093/neuonc/not032. doi:10.1093/neuonc/not032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gleeson M, Cunningham D, Hawkes EA, Qian W, Smith P, Chadwick N, et al. Risk of CNS Relapse with Diffuse Large B-Cell Lymphoma (DLBCL) in the Rituximab Era:Results from the UK NCRI R-CHOP 14 v 21 Trial. Blood. 2014;124:1723. [Google Scholar]
- 23.Lee MY, Kim HS, Lee JY, Lim SH, Kang ES, Ko YH. Efficacy and feasibility of autologous stem cell transplantation in patients with diffuse large B-cell lymphoma with secondary central nervous system involvement. Int J Hematol. 2015;102(6):678–688. doi: 10.1007/s12185-015-1874-1. doi:10.1007/s12185-015-1874-1. [DOI] [PubMed] [Google Scholar]


