Abstract
Though the incidence of concomitant ipsilateral intracapsular and extracapsular fracture neck of femur is still a rare presentation in day to day fracture hip admissions. Cases of simultaneous ipsilateral intra- and extra-capsular neck of femur fractures are forestalled with problems relating to diagnosing this injury as well as debate regarding optimal methods of fixation versus arthroplasty. We did a literature review to assess frequency of such fracture incidence, highlight methods of treatment applied, current practice for management as well as case report presentation.
Keywords: Concomitant/simultaneous intracapsular/extracapsular fractures, Fracture fixation, Hip fractures/complications, Hip fractures/radiography, Ipsilateral hip fractures/surgery, Hip joint/surgery, Hip fracture neck of femur fracture segmental fracture hemiarthroplasty dynamic hip fixation
Introduction
In the field of orthopaedics, hip fractures are a common occurrence, be they are a result of an elderly falling in her home or a substantially younger individual crawling away from the scene of a bad road traffic accident. Hip fractures have, for a long time, been classified broadly into intracapsular and extracapsular subtypes, so it is a rarity when a patient is admitted to hospital presenting with a simultaneous intra and extracapsular type of hip fracture. We are presenting a challenging case with literature review of similar cases and their management.
There are only limited case reports of a simultaneous intra- and extra-capsular fracture of the hip throughout the literature. Most of cases reported were due either misplacement of DHS or 2ry subcapital fracture.
Most cases have occurred following low energy falls in elderly osteoporotic patients with the exception of a few cases following road traffic accidents [5], [6].
Methods of fixation vary between cases. DHS fixation is the most common means of fixation adopted in multiple cases (seven cases), four of which used supplementary anti-rotation devices. One patient underwent fixation with a long stem hemiarthroplasty and Parham bands [6]. In our case total hip replacement with constrained cup was chosen by the treating surgeon.
Case presentation
History
The patient in question was an 88-year-old lady of unpleasantly confused disposition (due to cognitive impairment) found on the floor of her nursing home after having tripped over a mat and thenceforth being unable to mobilize and complaining of pain in her right hip (Fig. 1).
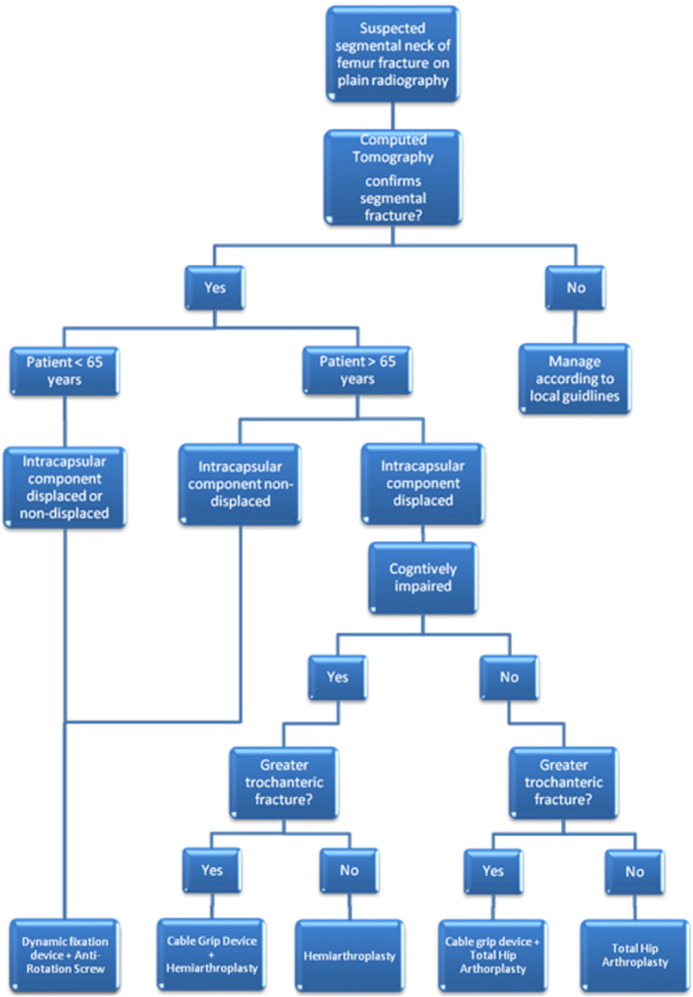
Fig. 1.
Algorithm for the management of segmental neck of femur fractures.
Clinical examination
On clinical examination she had a tender right hip with a shortened and externally rotated leg.
Investigations
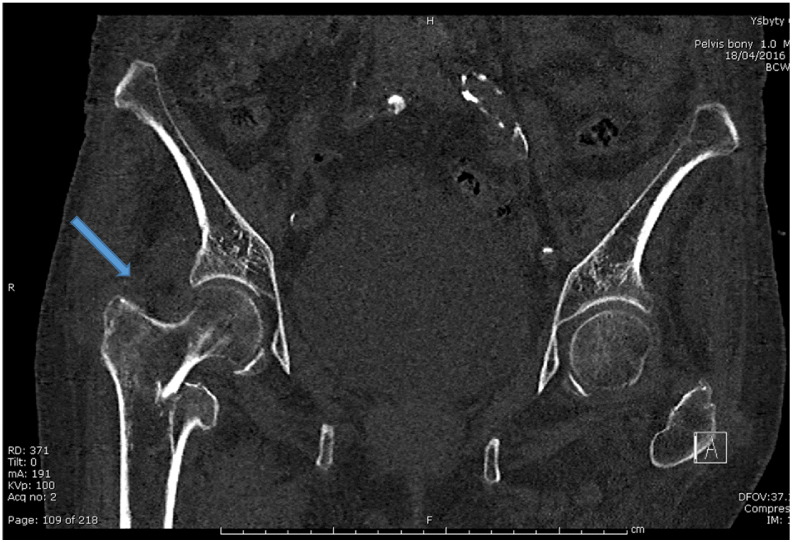
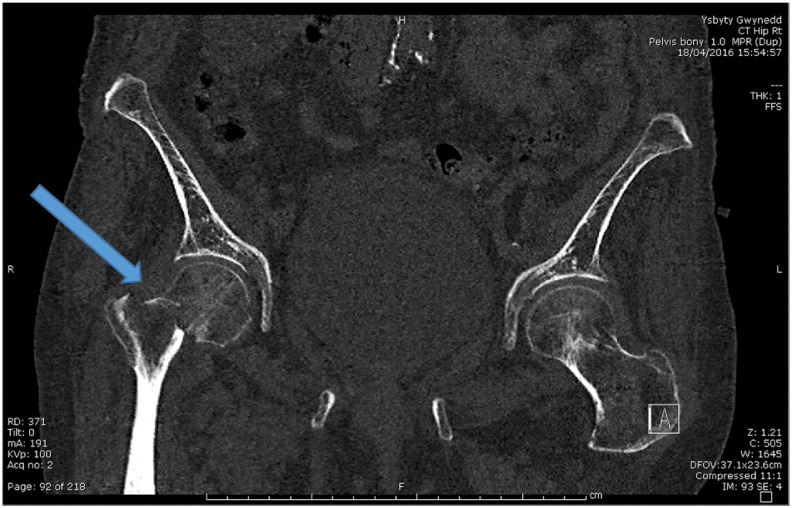
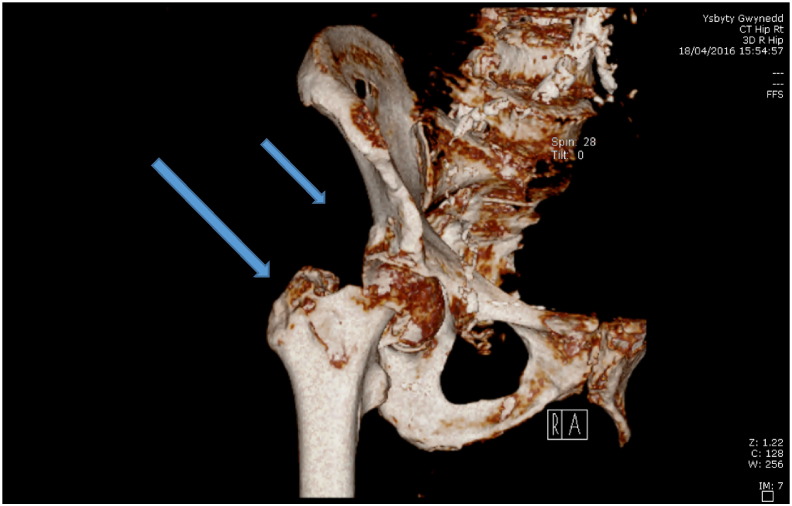
The initial X-rays of her affected hip (Fig. 2, Fig. 3) could not confirm a definitive fracture so a CT was requested which reported “an impacted fracture of the right neck of femur extending from the subcapital region anteriorly to the intertrochanteric region posteriorly”, raising the question of whether or not one segment of the fracture (possibly the intracapsular part) had actually preexisted, escaping prior diagnosis (Fig. 4, Fig. 5, Fig. 6, Fig. 7, Fig. 8).
Fig. 2.
Initial AP X-ray on admission.
Fig. 3.
Initial lateral view.
Fig. 4.
CT scan images showing intracapsular and extracapsular fracture neck of femur.
Fig. 5.
CT scan images showing intracapsular and extracapsular fracture neck of femur.
Fig. 6.
3-D CT scan images showing intracapsular and extracapsular fracture neck of femur.
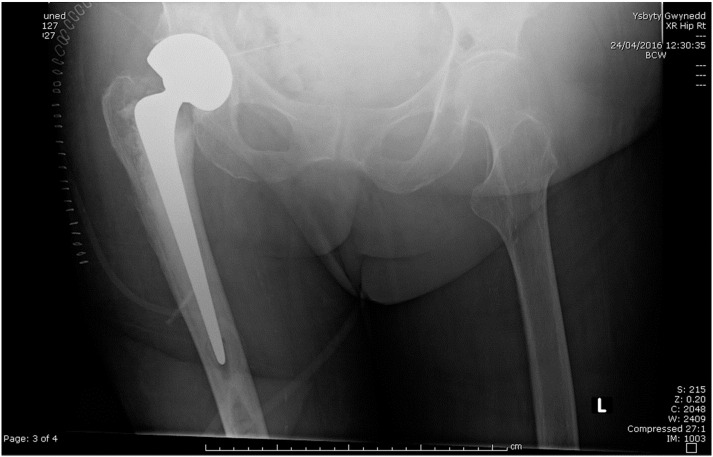
Fig. 7.
postoperative X-ray following THR.
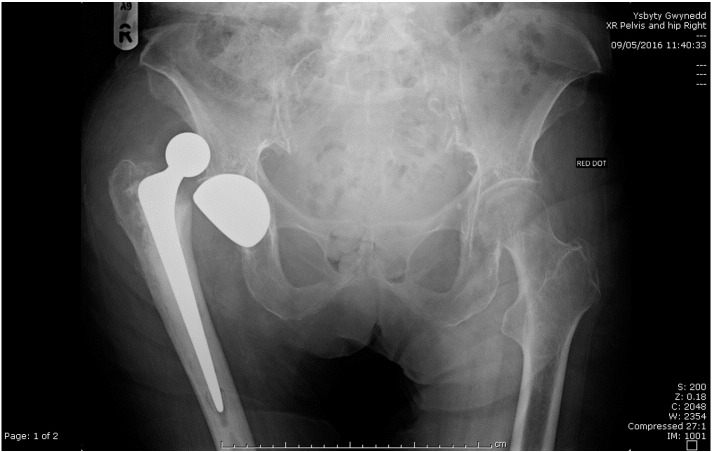
Fig. 8.
X-ray showing dislocation of the THR.
Management plan
The operative management for this patient was a choice between a hemiarthroplasty and a total hip replacement. Due to the uncommon nature of the fracture with the intertrochanteric element making the risk of dislocation higher, it was decided to treat this case with a cemented collarless total hip replacement (Table 1, Table 2).
Table 1.
The results of our search are summarized in the table below showing limited cases of similar incidence in last quarter of a century.
| Author/year | Age | Sex | Mechanism | Fracture type | Pre-op imaging | Implant used | Follow-up (months) | Outcome |
|---|---|---|---|---|---|---|---|---|
| Cooke, R F 1989 [1] | 73 | F | Fall | Subcapital + basicervical | X-ray | DHS | 30 | Good |
| An 1989 | NA | NA | Fall | Intertrochanteric + neck | X-ray | Hemiarthroplasty with Parham bands | NA | Good |
| Lawrence 1993 [2] | Elderly | NA | Fall | Intertrochanteric + subcapital | X-ray | Pinning | 2 | Death-unrelated |
| Cohen 1999 [3] | 79 | F | Fall | Peritrochanteric + subcapital | X-ray | DHS | 24 | Good |
| Yuzo 2001 [4] | 89 | F | Fall | Neck + trochanter | X-ray, CT, MRI | Bipolar hemiarthroplasty | NA | Good |
| Poul 2001 [5] | 83 | F | Fall | Intertrochanteric + subcapital | X-ray | DHS + TSP + ARS | 12 | AVN |
| Lakshmanan 2005 [6] | 91 | F | Fall | Subcapital with extracapsular extension | X-ray | Hemiarthroplasty | 6 | Good |
| Sayegh 2005 [7] | 54 | M | Crush injury (olive press) | Intertrochanteric + subcapital | X-ray | DHS and cerclage | 58 | Good |
| Poulter 2007 [8] | 76 | F | Fall | Intertrochanteric + subcapital | X-ray | PCCP | 4 | Good |
| Butt 2007 [9] | 30 | M | RTA | Neck + reverse oblique | X-ray | DHS + ARS | 12 | Good |
| Perry 2008 [10] | 86 | F | Fall | Intertrochanteric + neck | X-ray | DHS | 3 | AVN |
| Dhar 2008 [10] | 30 | M | RTA | T shape NOF | X-ray | DCP + lag screws | 12 | Good |
| Loupasis 2010 [11] | 36 | M | RTA | Intertrochanteric + subcapital | X-ray | DHS + ARS | 24 | Good |
| Raviraj 2011 [12] | 38 | M | RTA | Neck and peritrochanteric | X-ray, CT | DCS + ARS | 28 | Good |
| Muzaffar 2011 [13] | Mid-age | F | RTA | Transcervical, trochanter + shaft | X-ray | NA | NA | Death–polytrauma |
| Tahir 2014 [14] | 87 | F | Fall | Ipsilateral subcapital, greater trochanteric and intertrochanteric fracture | X-ray, CT | Bipolar hemiarthroplasty and proximal femur plate fixation | 3 | Good |
Concomitant intra and extracapsular neck of femur fractures reported in the literature (THR: total hip replacement; Hemi: hemiarthroplasty; PCCP: Percutaneous Compression Plating; DHS: dynamic hip screw; ARS: anti-rotation screw; DCP: Dynamic Compression Plate; TSP: Trochanter Stabilizing Plate; DCS: Dynamic Condylar Screw NA: not available; NR: not recorded).
Table 2.
Statistical analysis of data in Table 1.
| Statistics | |||
|---|---|---|---|
| Gender | Age | ||
| N | Valid | 14 | 13 |
| Missing | 2 | 3 | |
| Age | ||
|---|---|---|
| Mean | N | Std. Deviation |
| 62.8462 | 13 | 28.97944 |
| Age | |||
|---|---|---|---|
| Gender | Mean | N | Std. Deviation |
| Male | 63.8000 | 5 | 28.70888 |
| Female | 70.7143 | 7 | 21.45316 |
| Total | 67.8333 | 12 | 23.73656 |
| Gender | |||||
|---|---|---|---|---|---|
| Frequency | Percent | Valid percent | Cumulative percent | ||
| Valid | m | 5 | 31.3 | 35.7 | 35.7 |
| f | 9 | 56.3 | 64.3 | 100.0 | |
| Total | 14 | 87.5 | 100.0 | ||
| Missing | System | 2 | 12.5 | ||
| Total | 16 | 100.0 | |||
Post operatively, she was initially unstable, scoring a NEWS ranging 8–9 that was mainly a side effect of her cognitive impairment and agitation, which had her desaturating on air enough to require oxygen, only to pull off the oxygen mask as soon as the nursing staff managed to put one on.
Even though physiotherapy wasn't entirely feasible in light of her mental status, she recovered reasonably well, all things considered, and after a few weeks was eagerly attempting to get out of bed in her quest for a restroom.
Unfortunately, she was readmitted shortly after being discharged to her nursing home, a few days following a fall, only to contract a dislocation of her THR. Her hip was successfully relocated under anaesthesia and she went back to her nursing home the day after.
We searched the literature for similar cases and methods of fixation or implant used, mechanism of injury, follow up and outcome if available.
Methods
We conducted the following database search AMED (Allied and Complementary Medicine) 1985 to May 2016, Database Field Guide Embase 1974 to 2016 May 26, Database Field Guide HMIC Health Management Information Consortium 1979 to March 2016, Database Field Guide PsycINFO 1806 to May Week 4 2016, Database Field Guide Books@Ovid May 23, 2016, Database Field Guide Ovid Journals Database, Database Field Guide NHS Wales Full Text Journals, Database Field Guide Epub Ahead of Print, In-Process & Other Non-Indexed Citations, Ovid MEDLINE(R) Daily and Ovid MEDLINE(R) 1946 to present.
The following keywords were used in the searches: intracapsular neck of femur fracture or extracapsular neck of femur fracture or these terms were connected by the Boolean operators “AND” and “OR”. Additionally, the reference lists of included articles and relevant reviews were also examined for potential studies. No language restriction was applied.
Results
We identified in our search 16 cases of similar incidence over the past 27 years. The incidence of such fracture is more common in females (9 females) 56% with average age around 62 years in our literature review.
Concomitant intra and extracapsular fractures of neck of femur occurred in a bimodal age distribution and this is directly related to the injury mechanism. Incidence peaks in the mid-30s in high energy trauma, and mid-60s in low energy trauma.
Dynamic hip screw was used in 6 cases (43%) as a mean of fixation versus 25% for hemiarthroplasty. Antirotation screws were used in 4 cases whilst trochanteric stabilizing plate was applied in one case
The advantages of internal fixation compared with arthroplasty are: it allows the patient to retain his or her own femoral head with less surgical trauma compared with arthroplasty. Mortality and morbidity may be marginally reduced in very frail patients with reduced risk of sepsis and complications of wound healing.
Randomised trials and review articles have reported a lower rate of re-operation and tendency to better functional outcomes in elderly patients undergoing arthroplasty compared with internal fixation [13], [14], [15]. No difference in mortality has been shown between the two procedures [16]).
X-rays are usually the initial investigation needed but resorting to CT scans may reveal concomitant subtle fractures that may not appear obviously on x ray as in our case and this might change the management plan as well as the team embarking on the plan according to experience especially if THR is planned in the course of management. Tahir et al. in 2014 [17] proposed an Algorithm for the management of segmental neck fractures.
Conclusions
Our results would recommend tailoring surgical plan according to the patient age, functional mobility, expectations and displacement of intracapsular component. When approaching concomitant intra and extracapsular fractures of neck of femur, the objectives are to provide a stable construct whilst preserving the femoral head where possible. Typically, in intracapsular fractures of the femoral head, younger patients undergo dynamic hip screw (DHS) fixation to preserve the femoral head, whereas elderly patients undergo hemiarthroplasty or THR due to the risk of AVN in what for many patients will be definitive surgery. The choice between hemiarthroplasty and total hip replacement is still a matter of debate taking in the consideration the fracture pattern, level of mobility, cognitive impairment as well as surgeon experience when approaching such age group.
References
- 1.Cooke R.F., Limbird R., Jackson W.T. Simultaneous ipsilateral intertrochanteric and subcapital fracture of the hip. A case report. Orthopedics. 1989;12(5):721–723. doi: 10.3928/0147-7447-19890501-11. [DOI] [PubMed] [Google Scholar]
- 2.Isaacs C., Lawrence B. Concomitant ipsilateral intertrochanteric and subcapital fracture of the hip. J. Orthop. Trauma. 1993;7(2):146–148. doi: 10.1097/00005131-199304000-00008. (Available from: http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L23880248/nhttp://findit.library.jhu.edu/resolve?sid=EMBASE&issn=08905339&id=doi:&atitle=Concomitant+ipsilateral+intertrochanteric+and+subcapital+fracture+of+the+hip.&stitle=J+Orthop [Internet]) [DOI] [PubMed] [Google Scholar]
- 3.Cohen I., Rzetelny V. Simultaneous ipsilateral pertrochanteric and subcapital fractures. Orthopedics. 1999;22(5):535–536. [PubMed] [Google Scholar]
- 4.Oda Y., Yamanaka M., Tada H., Isaka N. A case of femoral neck and trochanteric fracture in ipsilateral femur. Orthop. Traumatol. 2001;50(4):1072–1075. [Google Scholar]
- 5.Poul J., Vejrostova M. Rotational acetabular osteotomy in the treatment of Legg-Calve-Perthes disease. Acta Chir. Orthop. Traumatol. Cechoslov. 2001;68(6):357–362. [PubMed] [Google Scholar]
- 6.Lakshmanan P., Peehal J.P. Management of an unusual intra- and extra-capsular subcapital femoral neck fracture. Acta Orthop. Belg. 2005;71(5):622–625. [PubMed] [Google Scholar]
- 7.Sayegh F.E., Karataglis D., Trapotsis S.J., Christoforides J.E., Pournaras J.D. Concomitant ipsilateral pertrochanteric and subcapital fracture of the proximal femur. Eur. J. Trauma. 2005;31(1):64–67. [Google Scholar]
- 8.Poulter R.J., Ashworth M.J. Concomitant ipsilateral subcapital and intertrochanteric fractures of the femur. Inj. Extra. 2007;38(3):88–89. [Google Scholar]
- 9.Femoral neck fracture with ipsilateral trochanteric fracture: is there room for osteosynthesis?J. Orthop. Surg. 2007;5(1) (Internet) [Google Scholar]
- 10.Perry D.C., Scott S.J. Concomitant ipsilateral intracapsular and extracapsular femoral neck fracture: a case report. J. Med. Case Rep. 2008;2:68. doi: 10.1186/1752-1947-2-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Loupasis G., Ntagiopoulos P.G., Asimakopoulos A. Concomitant ipsilateral subcapital and intertrochanteric fractures of the femur: a case report. J. Med. Case Rep. 2010;4:363. doi: 10.1186/1752-1947-4-363. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Raviraj A., Anand A. Ipsilateral femoral neck and trochanter fracture. Indian J. Orthop. 2011;45(3):284. doi: 10.4103/0019-5413.80052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lakkol S., Naique S. Int. J. Surg. Case Rep. [Internet] 5(5) Elsevier; Jun 26, 2016. Segmental neck of femur fractures: a unique case report of an ipsilateral subcapital, greater trochanteric and intertrochanteric fracture and proposed management algorithm; pp. 277–281.10.1016/j.ijscr.2014.03.012 Available from: [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang H., Chen J., Chen F., Que W. The effect of tranexamic acid on blood loss and use of blood products in total knee arthroplasty: a meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2012;20(9):1742–1752. doi: 10.1007/s00167-011-1754-z. [DOI] [PubMed] [Google Scholar]
- 16.Sebestyen A., Boncz I., Toth F., Pentek M., Nyarady J., Sandor J. Correlation between risk factors and mortality in elderly patients with femoral neck fracture with 5-year follow-up. Orv. Hetil. 2008;149(11):493–503. doi: 10.1556/OH.2008.28228. [DOI] [PubMed] [Google Scholar]
- 17.Tahir M., Lakkol S., Naique S. Segmental neck of femur fractures: a unique case report of an ipsilateral subcapital, greater trochanteric and intertrochanteric fracture and proposed management algorithm. Int. J. Surg. Case Rep. 2014;5(5):277–281. doi: 10.1016/j.ijscr.2014.03.012. [DOI] [PMC free article] [PubMed] [Google Scholar]