Abstract
Introduction:
Posterior fossa extradural hematoma (PFEDH) is rare among the traumatic brain injury and represent about 4–7% cases of all EDHs. This rare condition is rapidly fatal unless identified and intervened timely. Because of limited space in posterior fossa, comparatively small volume can cause clinical deterioration. Early diagnosis by cranial computed tomography and emergent evacuation is vital for a good outcome.
Materials and Methods:
This study was conducted at Level I trauma center at All India Institute of Medical Sciences, New Delhi, India. Hospital medical records were reviewed from September 2007 to June 2015. There were 856 cases of acute EDHs and of these 69 cases had PFEDHs. Records of patients with PFEDHs were reviewed for the mode of injury, Glasgow Coma Scale (GCS) at admission, imaging, type of intervention, outcome, and follow-up. GCS was assessed at 6 months and 12 months follow-up. Pertinent literature is reviewed.
Results:
Of these 69 patients, 51 were males and 18 females. The mean age of patients was 28.6 years (range 4–43 years). Forty-three patients had GCS 15 at admission, and only 4 of them had admission GCS <8. Mean EDH volume was 29.2 ml. Sixty-six patients were operated, three managed conservatively. Sixty-seven patients were discharged, of which, 56 (81.1%) had GCS 15. Two patients died. Most common associated injuries were long bone fractures (18, 26.1%) followed by blunt injury thorax (11, 15.9%). Mean follow-up duration was 69.2 months (range 6–94 months). At 6 months follow-up, 61 (88.4%) patients had good recovery (Glasgow Outcome Score [GOS] 5) and at 12 months, 62 (89.8%) had GOS 5.
Conclusion:
PFEDH are rare. They are usually associated with occipital bone fractures and may also have a supratentorial hematoma. It may be rapidly fatal due to the expansion of hematoma and compromise of the posterior cranial fossa space leading to brainstem compression, tonsillar herniation, and/or obstructive hydrocephalus. Early diagnosis and emergent evacuation lead to good outcome.
Keywords: Extradural hematoma, posterior fossa, surgery, trauma
Introduction
In posterior fossa, traumatic conditions are less frequent, and extradural hematoma is the most frequently encountered traumatic pathology. Traumatic posterior fossa extradural hematomas (PFEDHs) represent a rare clinical entity. It has been reported that PFEDH constitutes only 4–7% (1.2–15% in various studies for all age groups) of all extradural hematomas.[1,2] This rare condition can present with rapid clinical deterioration by quickly increasing in size and causing brain stem compression. Therefore, timely diagnosis of PFEDH is very important for good outcomes.[3] Obtaining cranial computed tomography (CT) for detecting PFEDH that has not caused any clinical findings yet, is especially of vital importance.
Materials and Methods
In this study, we reviewed the data over a period of 94 months extending from September 2007 to June 2015 at Jai Prakash Narayan Apex Trauma Center, a tertiary level trauma center attached to the All India Institute of Medical Sciences, New Delhi, India. We found a total of 856 cases of EDHs, of which only 69 (8.1%) were located in the posterior fossa. The records were retrospectively analyzed for clinical presentation, admission Glasgow Coma Scale (GCS), mode of injury, radiological findings, any other associated intracranial traumatic lesion, type of intervention and postoperative outcome. Postoperative scans, within 2–4 h of surgery were acquired in all cases. Outcomes were assessed on the basis of Glasgow Outcome Score (GOS) at the time of discharge and at 6 months of follow-up. Search was made on pubmed.org with key words “traumatic posterior fossa extradural hematoma” for published literature on PFEDHs and the results were compared.
Results
A total of 856 cases of EDHs were found during 94 months from September 2007 to June 2015. Of these, 69 (8.1%) were PFEDHs.
The mean age of patients was 28.6 years (4–43 years). Twenty-eight (40.6%) of them were below 18 years. Eighteen (26.1%) of them were females. Most common mode of injury was road traffic accident (n = 48, 69.6%), rest were either fall from height (n = 18, 26.1%) or assault (n = 3, 4.3%). Post-resuscitation admission GCS varied from GCS 15 in 43 (62.3%) cases, GCS 13–14 in 12 (17.4%), GCS 9–12 in 10 (14.5%), and GCS 3–8 in 4 (5.8%) cases. Three patients had GCS 3 and 1 had GCS 4 [Table 1].
Table 1.
Clinicoradiological features

The most common clinical presentation was with headache that was present in all conscious patients (43, 62.3%) and was primarily localized to the site of the primary impact that was an occipital or suboccipital region in most cases. Vomiting was seen in 36 (52.2%) cases and altered sensorium in 26 (37.7%) were the other common presentations.
All patients underwent noncontrast CT (NCCT) brain with 5 mm axial cuts of the posterior fossa, and PFEDH was present in all cases. In the majority of cases, it was unilateral (n = 65, 94.2%) and in 4 (5.8%) cases, it was on either side of the midline. The mean volume of EDH was 29.2 ml in operated patients and 10.8 ml in nonoperated patients. Mean EDH volume in adults (n = 41) was 36.8 ml and in pediatric group (n = 28), it was 20.6 ml. Among the associated CT findings, occipital bone fracture was the most frequent, present in 53 (76.8%) cases followed by frontal contusions in 7 (10.1%) and acute subdural hematoma (SDH) in 9 (13.0%) cases. Supratentorial acute SDH over frontoparietal convexity was seen in 6 (8.7%) cases, whereas infratentorial acute SDH over the cerebellar convexity were seen in 3 (4.3%) cases. In 21 (30.4%) cases, the EDH was extenting to the supratentorial compartment [Figure 1]. Hydrocephalus due to compression or obliteration of the fourth ventricle was seen in 12 (17.4%) cases that resolved after the evacuation of EDH in all cases in the postoperative period [Figure 2]. However, in two cases, the hydrocephalus reappeared on the postoperative day 7 and day 11, in both these cases, there was an associated intraventricular hemorrhage in the admission CT. Both cases were subjected to cerebrospinal fluid diversion with ventriculoperitoneal shunt.
Figure 1.
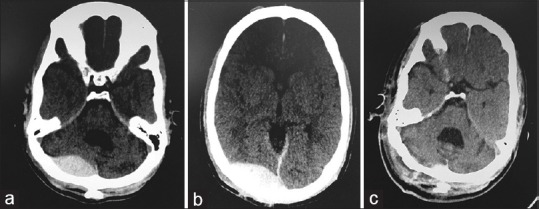
(a) Another patient with posterior fossa extradural hematoma straddling the transverse sinus showing the infratentorial part, (b) supratentorial part of extradural hematoma in the same patient as in Figure 2a, (c) postoperative scan of patient in Figure 2a showing complete evacuation
Figure 2.

(a) Preoperative computed tomography showing posterior fossa extradural hematoma with compression of the fourth ventricle and dilated temporal horns, (b) preoperative scan of patient in Figure 1a showing upstream hydrocephalus, (c) bone window showing occipital bone fracture, (d) postoperative scan showing complete evacuation of extradural hematoma
Of these 69 cases, 63 were operated, and 6 were initially planned for nonsurgical management. However, three out of these six patients failed the nonsurgical management and had to be operated between day 2 and day 4 of trauma. Incision and craniotomy were made as per the site and size of EDH. Fifty-nine cases (85.5%) underwent paramedian suboccipital craniotomy as all of these had unilateral EDHs. Midline suboccipital craniotomy was done in 7 (10.1%) cases. Of these seven who underwent midline suboccipital craniotomy, three cases had associated cerebellar convexity acute SDH that is why they also underwent evacuation of acute SDH and lax duraplasty resulting in formal posterior fossa decompression. In addition, two patients underwent decompressive hemicraniectomy with the removal of acute SDH over frontoparietal convexity and lax duraplasty with pericranium; one patient underwent bifrontal decompressive craniectomy [Figure 3], and one patient was operated for the right frontal contusion with pericontusional edema and subfalcine herniation. All patients were subjected to early NCCT brain in the postoperative period. Postoperative scans were acceptable in all 66 cases who underwent surgery.
Figure 3.

(a) Another patient's scan showing posterior fossa extradural hematoma and left sided frontotemporal acute subdural hematoma and bilateral frontal contusions and subarachnoid hemorrhage, (b) postoperative scan of patient in a showing evacuation of posterior fossa extradural hematoma and left-sided acute subdural hematoma and bilateral frontotemporal decompressive craniectomy
Sixty-seven patients were discharged, of which, to discharge, 56 (81.1%) had GCS 15, 5 (7.2%) had GCS 13–14, 2 (2.9%) had GCS 9–12, and 4 (5.8%) patients had GCS <8. Two patients died. Mean follow-up duration was 69.2 months. At 6 months follow-up, 61 (88.4%) patients had a good recovery (GOS 5) and at 12 months follow-up, 62 (89.8%) patients had GOS 5 [Table 2]. In addition, patients with isolated PFEDH (n = 58) had a much better outcome. Fifty-six out of 58 were discharged with GCS 15, 1 had GCS 14, and another one had GCS 13. At 6 months and 12 months follow-up, all 58 had good recovery (GOS 5), [Table 3]. In sharp contrast, patients with associated intracranial CT findings in addition to PFEDHs (n = 11) had poor outcomes. No one was discharged with GCS 15. Only three had GOS 5 at 6 months, and four had GOS 5 at 12 months.
Table 2.
Outcomes based on Glasgow outcome score

Table 3.
Outcome based on computed tomography findings

Most common associated injuries were long bone fractures (18, 26.1%) followed by blunt injury thorax (11, 15.9%), blunt injury abdomen (8, 11.6%), spine fractures (5, 7.2%), and maxillofacial injuries (2, 2.9%). These injuries were managed as indicated.
Discussion
Extradural hematoma is seen in 1% of patients who present with head trauma. PFEDHs are reported to constitute 0.1–0.3% of all cranial traumatic conditions. Most of these cases are associated with skull fractures. However, an extradural hematoma can develop without a fracture. Owing to the increased plasticity of the bones, the rate of developing extradural hematoma without a fracture is higher in children. Extradural hematoma generally develops by separation of the periosteal duramater from the calvarium and rupture of the interposed vessels after trauma. The rupture of the vessel causes a rapid increase in the size of the hematoma. However, if the venous structures are involved, late and chronic clinical pictures may develop. Unlike supratentorial EDHs where the source of bleeding is usually the middle meningeal artery in temporoparietal EDHs and the anterior ethmoidal artery in frontal EDHs,[4] PFEDHs have a venous origin in 85% of the cases and develop as a result of injury to the transverse or sigmoid sinuses secondary to occipital bone fracture.[5] The classical history of an extradural hematoma as described in the context of temporal EDHs is a short interval of posttraumatic unconsciousness followed by a “lucid interval” that may last for hours, which in turn, is followed by altered sensorium and development of potentially fatal neurological condition secondary to compression of the brainstem. Diagnosing extradural hematoma in the lucid interval is extremely important for good outcomes. However, in cases of PFEDHs, this classical description does not apply. The treatment of epidural hematoma is surgical except for very small hematomas that are followed-up.[6] Since most of the PFEDHs are of venous origin and expand slowly, it takes longer for the clinical picture to develop in PFEDH and it is of vital importance to use imaging methods for early diagnosis. Currently, NCCT scan is the imaging of choice in brain trauma. An acute extradural hematoma is seen as a biconvex hyperdense mass located between the duramater and the bone on NCCT. If the blood continues to accumulate rapidly, one can see hypodense areas within the lesion “Swirl sign” and suggests the high probability of finding an actively bleeding vessel.
On magnetic resonance (MR) imaging, the acute extradural hematoma is seen as a localized extra-axial collection between the dura and the inner table of skull bone. Imaging of the dura as a line with very low signal between the hematoma and the brain parenchyma is pathognomonic for extradural hematoma. While it is not always possible to differentiate small extradural hematomas that have not formed a biconvex shape yet due to small volume, demonstration of dura between the parenchyma, and the hematoma is diagnostic on MR imaging. In addition, MR imaging is more sensitive in the detection of associated parenchymal conditions or dural venous sinus thrombosis possibly associated with PFEDH.[4,7] Since obtaining an MR imaging study is difficult in unstable trauma patients, the initial imaging of choice and the most commonly used method is still NCCT. In our study, of the 69 patients with a traumatic PFEDHs, 53 (76.8%) patients had an occipital bone fracture. Other conditions included subarachnoid hemorrhage, occipital and temporal fracture, supratentorial SDH, cerebral edema, cerebellar parenchymal pathology, and supratentorial parenchymal hematoma. When the patients with only occipital fractures are excluded, in concordance with the literature, the most commonly encountered posterior fossa traumatic pathology was extradural hematoma. In the literature, it has been reported that PFEDHs are most commonly encountered in the first decade.[8,9] In our study, 28 (40.6%) cases were pediatric, and 19 (27.5%) were in their first decade.
Cranial CT examination has earned a place as an effective imaging method by having a short acquisition time, allowing demonstration of occipital fractures that are associated with great majority of PFEDHs, defining the size and mass effects of the hematoma and providing visualization of possible supratentorial conditions that are reported to be associated with half of the cases in the literature.[10,11] Early cranial CT examination should be performed routinely in patients who do not have any neurological findings as well. Furthermore, considering small occipital fractures can be overlooked during physical examination and plain film studies, patients with cranial trauma involving the posterior fossa should definitely be examined with cranial CT. By effectively demonstrating early PFEDHs without clinical findings and the associated pathologies, and allowing early treatment, CT is an indispensable entity.
As per the search results on pubmed.org with key words “traumatic posterior fossa extradural hematoma” we found many case series [Table 4]. Bozbuga et al.[8] reported 73 cases in 1999, the largest series on PFEDH till now. Out of 73, they operated 53 cases. Eighty-nine percent of operated patients had a good recovery, and 5.4% died. Malik et al. published another series of 61 patients in 2007. Of these 48 were managed surgically, 36 (59%) had a good recovery and 15% died. Roka et al.[17] reported 43 patients in 2008, of these 33 were operated and were followed up for 79 months with 81.8% good recovery in the operated patients and 3% overall mortality. Jang et al.,[13] in 2011, published the review of 34 patients with 96 months follow-up. Nineteen patients underwent surgical evacuation with 73.7% having a good recovery and 5.3% mortality. Three series comprised pediatric cases only. Sencer et al.,[12] in 2012, Prasad et al.,[11] in 2012, and Gupta et al.,[16] in 2002, published pediatric series with 40, 18, and 18 cases, respectively. Sencer reported good recovery in all cases. Prasad's series had 94.4% patients with good recovery. Both these series showed better outcomes in pediatric age group.
Table 4.
Comparison of case series of posterior fossa extradural hematoma

In this study, we report 69 patients with PFEDHs, the second largest case series as per PubMed-indexed literature. Sixty-six of them were operated. Sixty-seven patients were discharged, of which, at discharge, 56 (81.1%) had GCS 15, 5 (7.2%) had GCS 13–14, 2 (2.9%) had GCS 9–12, and 4 (5.8%) patients had GCS <8. Two patients died (2.9%). At 6 months follow-up, 61 (88.4%) patients had good recovery (GOS 5) and at 12 months follow-up, 62 (89.8%) patients had GOS 5. Hence, it can be concluded that PFEDHs are rare events and may be rapidly fatal if neglected, however with timely interventions can result in excellent outcomes, particularly in patients with isolated PFEDHs. Admission GCS is the single most important factor that determined the immediate and long-term outcomes. Patients with additional intracranial findings had relatively poor GCS at admission and categorically much poor outcomes. Nonsurgical management is a viable option in select patients with low EDH volumes, but with intensive monitoring, and low threshold should be kept for surgical evacuation in such patients.
Conclusion
PFEDH are rare. They may be rapidly fatal due to the expansion of hematoma and compromise of the posterior cranial fossa space leading to brainstem compression, tonsillar herniation, and/or obstructive hydrocephalus. Early diagnosis and emergent evacuation lead to good outcome. They are usually associated with occipital bone fractures and may also have associated injuries in form of supratentorial or infratentorial subdural hematoma, intraparenchymal hematoma or intraventricular hemorrhage. Associated intracranial injuries should also be managed emergently as per the clinical situation. However despite best possible management these associated injuries lead to worse outcomes depending upon the severity of associated injury.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Asanin B. Traumatic epidural hematomas in posterior cranial fossa. Acta Clin Croat. 2009;48:27–30. [PubMed] [Google Scholar]
- 2.Ammirati M, Tomita T. Posterior fossa epidural hematoma during childhood. Neurosurgery. 1984;14:541–4. doi: 10.1227/00006123-198405000-00002. [DOI] [PubMed] [Google Scholar]
- 3.Berker M, Cataltepe O, Ozcan OE. Traumatic epidural haematoma of the posterior fossa in childhood: 16 new cases and a review of the literature. Br J Neurosurg. 2003;17:226–9. doi: 10.1080/0268869031000153071. [DOI] [PubMed] [Google Scholar]
- 4.Samudrala S, Cooper PR. Traumatic intracranial hematomas. In: Wilkins RH, Rengachary SS, editors. Neurosurgery. 2nd ed. New York: McGraw-Hill; 1996. pp. 2797–807. [Google Scholar]
- 5.Garza-Mercado R. Extradural hematoma of the posterior cranial fossa. Report of seven cases with survival. J Neurosurg. 1983;59:664–72. doi: 10.3171/jns.1983.59.4.0664. [DOI] [PubMed] [Google Scholar]
- 6.Rivas JJ, Lobato RD, Sarabia R, Cordobés F, Cabrera A, Gomez P. Extradural hematoma: Analysis of factors influencing the courses of 161 patients. Neurosurgery. 1988;23:44–51. doi: 10.1227/00006123-198807000-00010. [DOI] [PubMed] [Google Scholar]
- 7.Osborn AG. Craniocerebral Trauma, Diagnostic Neuroradiology. St. Louis: Mosby; 1994. pp. 204–5. [Google Scholar]
- 8.Bozbuga M, Izgi N, Polat G, Gürel I. Posterior fossa epidural hematomas: Observations on a series of 73 cases. Neurosurg Rev. 1999;22:34–40. doi: 10.1007/s101430050006. [DOI] [PubMed] [Google Scholar]
- 9.Peter JC, Domingo Z. Subacute traumatic extradural haematomas of the posterior fossa: A clinicopathological entity of the 5- to 10-year-old child. Childs Nerv Syst. 1990;6:135–8. doi: 10.1007/BF00308489. [DOI] [PubMed] [Google Scholar]
- 10.Pozzati E, Tognetti F, Cavallo M, Acciarri N. Extradural hematomas of the posterior cranial fossa. Observations on a series of 32 consecutive cases treated after the introduction of computed tomography scanning. Surg Neurol. 1989;32:300–3. doi: 10.1016/0090-3019(89)90234-6. [DOI] [PubMed] [Google Scholar]
- 11.Prasad GL, Gupta DK, Sharma BS, Mahapatra AK. Traumatic pediatric posterior fossa extradural hematomas: A tertiary-care trauma center experience from India. Pediatr Neurosurg. 2015;50:250–6. doi: 10.1159/000438488. [DOI] [PubMed] [Google Scholar]
- 12.Sencer A, Aras Y, Akcakaya MO, Goker B, Kiris T, Canbolat AT. Posterior fossa epidural hematomas in children: Clinical experience with 40 cases. J Neurosurg Pediatr. 2012;9:139–43. doi: 10.3171/2011.11.PEDS11177. [DOI] [PubMed] [Google Scholar]
- 13.Jang JW, Lee JK, Seo BR, Kim SH. Traumatic epidural haematoma of the posterior cranial fossa. Br J Neurosurg. 2011;25:55–61. doi: 10.3109/02688697.2010.520759. [DOI] [PubMed] [Google Scholar]
- 14.Balik V, Lehto H, Hoza D, Sulla I, Hernesniemi J. Posterior fossa extradural haematomas. Cent Eur Neurosurg. 2010;71:167–72. doi: 10.1055/s-0030-1249046. [DOI] [PubMed] [Google Scholar]
- 15.Malik NK, Makhdoomi R, Indira B, Shankar S, Sastry K. Posterior fossa extradural hematoma: Our experience and review of the literature. Surg Neurol. 2007;68:155–8. doi: 10.1016/j.surneu.2006.10.051. [DOI] [PubMed] [Google Scholar]
- 16.Gupta PK, Mahapatra AK, Lad SD. Posterior fossa extradural hematoma. Indian J Pediatr. 2002;69:489–94. doi: 10.1007/BF02722650. [DOI] [PubMed] [Google Scholar]
- 17.Roka YB, Kumar P, Bista P, Sharma GR, Adhikari P. Traumatic posterior fossa extradural haematoma. JNMA J Nepal Med Assoc. 2008;47:174–8. [PubMed] [Google Scholar]
- 18.Kabre A, Alliez JR, Kaya JM, Bou Harb G, Reynier Y, Alliez B. Extradural hematoma of the posterior fossa. Neurochirurgie. 2001;47(2-3 Pt 1):105–10. [PubMed] [Google Scholar]


