Abstract
Objective:
The aim of this study is to investigate if a handheld ultrasound device (BladderScan® BVI 6100) can accurately measure bladder volumes in prostate radiotherapy (RT) patients.
Methods:
A comparison was made of contoured bladder volumes based on treatment planning CT (TPCT) and BladderScan® BVI 6100 ultrasound device in a large prostate RT population. Three bladder volume (BV) measurements were taken using the bladder volume instrument (BVI) device on prostate RT patients immediately prior to TPCT (n = 190). The CT delineation bladder volumes were also recorded. The mean of the three BVI readings (BVImean) and the maximum (BVImax) of the readings were considered for a comparative analysis.
Results:
There was a strong positive correlation between the BVI and CT delineated bladder volumes (BVImean r = 0.825; BVImax r = 0.830). The mean difference [± standard deviation (SD)] was an underestimation of BV for both BVImean and BVImax (44.8 ± 88.2 ml and 32.9 ± 87.5 ml, respectively).
Conclusion:
This is the largest study to date (n = 190), assessing the accuracy of the BladderScan® BVI 6100 in the prostate RT population. The BVI 6100 provides an acceptable indication of BV for use in prostate RT patients for the purposes of monitoring BV.
Advances in knowledge:
The BladderScan® BVI 6100 provides a convenient and non-irradiating method of indicating BV for use in prostate RT patients.
Introduction
Bladder-filling inconsistencies during a course of prostate radiotherapy (RT) can have dosimetric consequences which impact on gastrointestinal and genitourinary toxicity.1 If these bladder-filling inconsistencies can be identified and corrected prior to treatment then the planned treatment may be replicated with greater accuracy. Many departments use in-room image verification to assess bladder volumes, this has some disadvantages. Acquiring and reviewing the images takes several minutes; most verification systems use additional radiation doses and if a significant BV inconsistency is found, the patient is taken off the treatment couch, creating inefficiencies in service delivery. A quick and convenient device to measure BV, which does not require any radiation dose and can be used outside the treatment room would be advantageous both prior to treatment planning CT (TPCT) and RT treatment. This could assess the effectiveness of bladder-filling interventions, monitor patient compliance with bladder-filling interventions and improve workflow by identifying patients presenting with BV incompatible with treatment, prior to entering the treatment room.
Ultrasound equipment have proven to be convenient, non-invasive and accurate at measuring bladder volume (BV) in various settings.2, 3 The ultrasound device investigated in this study is the BladderScan® BVI 6100 (Verathon Inc, Bothell, WA) (Figure 1). There is conflicting evidence regarding the accuracy of the various BladderScan devices (BVI) 2500; 3000; 6100; 6200 and 6400) with some studies reporting the bladder volume instrument (BVI) as a validated method of measuring BV3–8 and others disproving this.9, 10
Figure 1.
BladderScan® BVI 6100 (Verathon Inc, Bothell, WA). BVI, bladder volume instrument.
The objective of this technical note is to compare BV assessed using the TPCT delineated volume and the BladderScan® BVI 6100, in a radiation therapy setting using a large sample of prostate RT patients. This comparison will inform radiation therapy department if the BladderScan® BVI 6100 can be used for prostate patients to access BV reproducibility and identify BV inconsistencies, prior to treatment.
Methods and Materials
Patient population
A total of 244 prostate RT patients were enrolled in a phase III Randomised Control Trial (All Ireland Co-operative Oncology Research Group, Study 05–04). The trial compared BV variation in patients following a 1080 ml (six plastic cups) water-drinking bladder-filling protocol with patients following a 540 ml (three plastic cups) water-drinking bladder-filling protocol.11 The previous publication11 reported on the patients that were enrolled on the trial post the cessation of a pre-CT hydration protocol (n = 110), this current research reports on unplanned secondary analysis of all eligible trial patients (both pre and post the cessation of the CT hydration protocol) (n = 190, supplementary data: appendix A). The design, objectives, treatment methods, statistical considerations and main trial outcomes have been reported previously.11 Inclusion criteria included a Karnofsky Performance Status of ≥60 radical prostate external beam RT in the supine position, no history of urinary incontinence, catheterisation or previous surgery for urinary conditions except transurethral resection of the prostate and provision of written informed consent. The only exclusion criterion was evidence of any significant clinical disorder that made it undesirable for the patient to participate or if it is felt that the patient could not comply with the protocol. All patients underwent a supine 5 mm slice thickness TPCT scan with a full/partial full bladder, from L5 to 2 cm below the ischial tuberosity.
Bladder-filling protocol
A full/partial-full bladder was achieved by following a strict bladder-filling protocol: 1-void bladder; 2-consume a specific volume of water (1080 ml or 540 ml) in 10 min; and 3-wait 30–40 mins prior to the TPCT.
Bladder volume assessment
As per institutional protocol, the entire BV (wall and lumen) was delineated by the treating physician. The TPCT BV value was generated from the automatic calculations from the treatment planning systems in cubic centimetres (cc).The BVI 6100 was used to measure BV immediately prior to the TPCT, with the patient positioned for treatment on the CT couch. On each occasion, three BV measurements were taken at the supra pubic region for each patient, in accordance with the device specifications. The BVI measures ultrasonic reflections on multiple planes and displays the volume in millilitres (ml) on an LCD screen (range:0–999 ml). The examination was completed by a radiation therapist trained and experienced in the use of the BVI device and measurements took 1–2 min to complete. The mean of the three readings (BVImean) and the maximum reading (BVImax) were considered for comparative analysis. The BVImean was selected based on published BVI research3, 6,8 and BVImax was chosen as it was anticipated that this may best represent the BV at the time of the TPCT, which took place immediately following the bladder imaging. The BVI was calibrated in line with the manufacturer’s recommendations for the duration of the study.
Statistical analysis
Pearson’s correlation was used to assess correlation between the BVI measurements (BVImean and BVImax) and the corresponding TPCT based on the individual patient readings. A Bland-Altman analysis12 was used to describe agreement between the methods. The correlation coefficient measures the strength of a relation between two variables, not the agreement between them. Bland-Altman plots were used to plot the difference against mean and limits of agreement, this is a more appropriate measure of the clinical significance of differences between the measurement methods. Statistical analyses were carried out using IBM® SPSS® statistical software v. 20.0. p < 0.05 was considered statistically significant.
Results
Data for 190 patients were analysed (Supplementary material 1). A summary of the BV at the time of TPCT is shown in Table 1. Figure 2 shows the scatterplots of the BV measured using the BVI [BVImean (Figure 2a) and BVImax (Figure 2b)] and CT delineated volumes. There was a strong correlation between the TPCT BV and the BVImean and BVImax (r = 0.825, p < 0.0005 and r = 0.830, p < 0.0005 respectively).
Table 1.
BV and variation
| CT delineated BV (cc) | BVImean (ml) | BVImax (ml) | |
| Mean (SD) | 282.6 (149.7) | 237.7 (148.1) | 249.7 (150.6) |
| 95% confidence interval | 261.2–303.9 | 216.6–258.9 | 228.2–271.2 |
| Median | 247.0 | 214.7 | 225.0 |
| Minimum | 70.0 | 27.0 | 30.0 |
| Maximum | 1015.0 | 828.0 | 863.0 |
BV, bladder volume; BVI, bladder volume instrument BladderScan® BVI 6100; BVImean, mean of three BVI measurements; BVImax, maximum BVI measurement; cc, cubic centimetres; ml, millilitres; SD, standard deviation.
Figure 2.
Scatter plots of BV measured by the BladderScan Device (BVI) and the delineated BV from the TPCT. (a) Graph of raw data comparing the BV by the mean of the three BVI measurements (BVImean) and the delineated BV on the TPCT. (b) Graph of raw data comparing the BV by the maximum measurement recorded by the BVI (BVImax) and the delineated BV on the TPCT. BV, bladder volume; BVI, bladder volume instrument BladderScan® BVI 6100; TPCT, treatment planning CT.
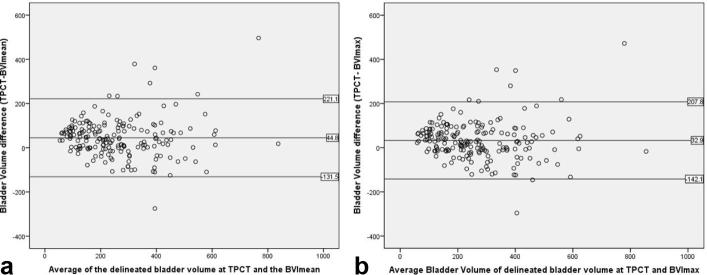
Figure 3 displays the Bland Altman scatterplots of the differences in BV delineated from TPCT and BVImean (Figure 3a) and BVImax (Figure 3b) plotted against the averages of the TPCT and BVI measurements. The Bland Altman plot represents the relationship between the measurement error and the true value. These scatterplots suggest that the magnitude of the difference between TPCT delineated BV and BVImean and BVImax are not related to the magnitude of BV. As the true BV is not known, the mean of the two measurements was used as the best estimate. The mean difference/bias, 95% limits of arguments and standard error mean of the BVI measurements are summarised in Table 2.
Figure 3.
Bland-Altman plots of the differences, between the BV measured with the BladderScan device (BVI) and the delineated BV from the TPCT, against the means. (a) A Bland-Altman plot showing the differences (Delineated TPCT minus BVImean) against the averages of the two methods. Horizontal lines are drawn at the mean difference and at the mean difference plus and minus two SDs. (b) A Bland-Altman plot showing the differences (Delineated TPCT minus BVImax) against the averages of the two methods. Horizontal lines are drawn at the mean difference and at the mean difference plus and minus two SDs. BV, bladder volume; BVI, bladder volume instrument BladderScan® BVI 6100; SDs, standard deviations; TPCT, treatment planning CT.
Table 2.
Summary of the Bland-Altman plot statistics and the standard error in calculation of the difference in the BV delineated at the TPCT and that calculated using BVImean and BVImax>
| Device | Bias/mean difference ± SD (ml) | 95% Limits of agreement (ml) |
SE difference
(ml) |
| BVImean | +44.8 ± 88.2 | −131 to +221 | 6.4 |
| BVImax | +32.9± 87.5 | −142 to +208 | 6.3 |
BV, bladder volume; BVI, bladder volume instrument BladderScan® BVI 6100; BVImean, mean of three BVI measurements; BVImax, maximum BVI measurement; ml, millilitres; SD, standard deviation; SE, standard error; TPCT, treatment planning CT.
Discussion
This study compares BV delineated on TPCT to the BVI 6100 on 190 prostate RT patients, the largest of its kind, to date, in the RT setting. The results suggest that BVI may be used to provide an acceptable indication of BV prior to CT and treatment for the purpose of monitoring bladder volumes. A strong correlation was reported between BV measured by the BVI and the delineated BV from the TPCT scan (BVImean r = 0.82 and BVImax r = 0.83). Several studies in the RT setting have reported similar strong correlations (ranging from r = 0.88 to 0.97) for the degree of association between various BVI devices (BVI 3000; 6100; 6400) and CT volumes.4,6–8,13 The large number of patients in this study compared with previous publications, may account for the slightly lower correlations than previously reported. Both BVI measurement methods proved to have an equally strong correlation coefficient with the delineated volumes.
The mean CT delineated BV was marginally greater than the mean BVImean (difference: 44.8 ± 88.2 ml) and closer to the mean BVImax (difference: 32.9 ± 87.5 ml) (Table 2). In this study the delineated bladder volumes included the entire bladder, wall and urine. In the case of our institution, delineating the inner wall of the bladder was found to be inaccurate. Therefore, it is reasonable to expect larger TPCT delineated volumes than the BVI volumes because of this contouring method. The bias falls outside the 10% difference of the measurements, at 16 and 12% respectively but is clinically acceptable given the BV involved. Other authors investigating the BVI in prostate patients reported smaller mean difference between the BVImean and the CT volumes. O’Shea et al3 found −9.7 ± 64.6 ml (n = 50) and Hynds et al7 reported 9.0 ml (n = 30). Ahmad et al8 recorded a mean difference of −16 ± 67 ml in a group of cervical cancer patients (n = 24).
The SD of the difference between CT and BVI (BVImean: 88.2 ml and BVImax: 87.5 ml) can be considered a measure of the accuracy of the BVI. In previous studies, reported accuracy levels were 64.6 ml in the prostate population3 and 67 ml in the cervical population.8 The clinical interpretation of these accuracy levels suggest that the BVI exhibits a degree of inaccuracy when compared to delineated volumes, but the clinical significance of this could be argued given the volumes of fluid that patients are routinely requested to consume prior to RT (e.g. 1080 ml/540 ml11). The measurements falling outside the limits of agreement (two SDs) represent seven patients whose delineated volumes (range: 348–1050 cc) were greater than the BVI volumes (range: 113–519 ml), and one patient whose CT volume (257 cc) was less than the BVI volumes (532 ml). BV of 150 ml has been reported as an optimal volume for prostate RT,1 so maintaining volumes at this level should ensure consistency with CT within the limits of agreement.
It could be argued that the CT delineated volume is not the “gold standard” for quantifying BV. Previous studies investigating the BVI in the diagnostic imaging setting used methods such as urethral catheterisation, voiding and cystometry.7, 10 The ability to measure the reproducibility of BV during treatment is important. Inconsistency in BV can reduce target position accuracy14 and increase toxicity. The BVI provides a non-ionizing, quick and convenient method to identify patients with BV that are incompatible with treatment/planning and prior to commencement of daily RT, which has the potential to improve workflow efficiency. The BVI can also be used to assess the effectiveness of bladder-filling interventions and check patient compliance with same.
Conclusion
The comparison of the BVI device and the TPCT delineated BV showed a strong correlation between both measurement methods. The BVI marginally underestimated the volume recorded by delineating the bladder. The accuracy of the BVI is acceptable based on the large volumes of water patients consume during patient preparation for RT. The BladderScan®BVI 6100 provides an acceptable indication of BV for use in prostate RT patients for the purposes of monitoring bladder filling.
Contributor Information
Laura Mullaney, Email: laura.mullaney@tcd.ie.
Evelyn O’Shea, Email: Evelyn.o'shea@slh.ie.
Mary T Dunne, Email: mary.dunne@slh.ie.
Pierre G Thirion, Email: pierreagnes@eircom.net.
John G Armstrong, Email: armstrongtravelling@gmail.com.
REFERENCES
- 1. Moore A, Forde E, O’Shea E, Armstrong J, O’Hara T, O’Neill L. A dosimetric evaluation of threshold bladder volumes for prostate cancer radiotherapy. J Med Imaging Radiat Sci 2017; 48: 270–5. doi: 10.1016/j.jmir.2017.03.003 [DOI] [PubMed] [Google Scholar]
- 2. Marks LS, Dorey FJ, Macairan ML, Park C, deKernion JB. Three- dimensional ultrasound device for rapid determination of bladder volume. Urology 1997; 50: 341–8. doi: 10.1016/S0090-4295(97)00293-8 [DOI] [PubMed] [Google Scholar]
- 3. O’Shea E, Armstrong J, O’Hara T, O’Neill L, Thirion P. Validation of an external ultrasound device for bladder volume measurements in prostate conformal radiotherapy. Radiography 2008; 14: 178–83. doi: 10.1016/j.radi.2007.06.001 [DOI] [Google Scholar]
- 4. O’Doherty UM, McNair HA, Norman AR, Miles E, Hooper S, Davies M, et al. Variability of bladder filling in patients receiving radical radiotherapy to the prostate. Radiother Oncol 2006. 2006; 79: 335–40. doi: 10.1016/j.radonc.2006.05.007 [DOI] [PubMed] [Google Scholar]
- 5. D’Amico AV, Manola J, Loffredo M, Lopes L, Nissen K, O’Farrell DA, et al. A practical method to achieve prostate gland immobilization and target verification for daily treatment. Int J Radiat Oncol Biol Phys 2001; 51: 1431–6. doi: 10.1016/S0360-3016(01)02663-3 [DOI] [PubMed] [Google Scholar]
- 6. Gawthrop J, Oates R. Measured bladder volume for radiotherapy of the prostate using the hand-held BladderScan® BVI 3000. Radiographer 2012; 59: 8–12. doi: 10.1002/j.2051-3909.2012.tb00167.x [DOI] [Google Scholar]
- 7. Hynds S, McGarry CK, Mitchell DM, Early S, Shum L, Stewart DP, et al. Assessing the daily consistency of bladder filling using an ultrasonic Bladderscan device in men receiving radical conformal radiotherapy for prostate cancer. Br J Radiol 2011; 84: 813–8. doi: 10.1259/bjr/50048151 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Ahmad R, Hoogeman MS, Quint S, Mens JW, de Pree I, Heijmen BJ. Inter-fraction bladder filling variations and time trends for cervical cancer patients assessed with a portable 3-dimensional ultrasound bladder scanner. Radiother Oncol 2008; 89: 172–9. doi: 10.1016/j.radonc.2008.07.005 [DOI] [PubMed] [Google Scholar]
- 9. Beckers GM, van der Horst HJ, Frantzen J, Heymans MW. The BladderScan BVI 6200® is not accurate enough for use in a bladder retraining program. J Pediatr Urol 2013; 9: 904–9. doi: 10.1016/j.jpurol.2012.12.013 [DOI] [PubMed] [Google Scholar]
- 10. Dudley NJ, Kirkland M, Lovett J, Watson AR. Clinical agreement between automated and calculated ultrasound measurements of bladder volume. Br J Radiol 2003; 76: 832–4. doi: 10.1259/bjr/31249864 [DOI] [PubMed] [Google Scholar]
- 11. Mullaney LM, O'Shea E, Dunne MT, Finn MA, Thirion PG, Cleary LA, et al. A randomized trial comparing bladder volume consistency during fractionated prostate radiation therapy. Pract Radiat Oncol 2014; 4: e203–e212. doi: 10.1016/j.prro.2013.11.006 [DOI] [PubMed] [Google Scholar]
- 12. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Int J Nurs Stud 2010; 47: 931–6. doi: 10.1016/j.ijnurstu.2009.10.001 [DOI] [PubMed] [Google Scholar]
- 13. Stam MR, van Lin EN, van der Vight LP, Kaanders JH, Visser AG. Bladder filling variation during radiation treatment of prostate cancer: can the use of a bladder ultrasound scanner and biofeedback optimize bladder filling? Int J Radiat Oncol Biol Phys 2006; 65: 371–7. doi: 10.1016/j.ijrobp.2005.12.039 [DOI] [PubMed] [Google Scholar]
- 14. Cambria R, Jereczek-Fossa BA, Zerini D, Cattani F, Serafini F, Luraschi R, et al. Physical and clinical implications of radiotherapy treatment of prostate cancer using a full bladder protocol. Strahlenther Onkol 2011; 187: 799–805. doi: 10.1007/s00066-011-2259-x [DOI] [PubMed] [Google Scholar]