A 4-year-old Indian boy presented because of recurrent biliary colic and jaundice for the previous 2 weeks. There was no history of fever. Laboratory investigations revealed alanine aminotransferase, 156 U/L (normal, 0-30 U/L); aspartate aminotransferase, 204 U/L (normal, 0-30 U/L); serum alkaline phosphatase, 920 U/L (normal, 30-120 U/L); and serum bilirubin, 8.4 mg/dL (normal, 0.2-1.2 mg/dL).
Abdominal US revealed a normal gallbladder, dilation of the intrahepatic biliary radicles, and a dilated common bile duct (CBD) of 14 mm, with an ill-defined rounded echogenic shadow inside the lower end of the CBD. The possible differential diagnoses of CBD polyp, choledochal cyst with sludge, CBD stone, and a dead coiled worm were considered. EUS was performed with a linear echoendoscope (Pentax EG 3830 UT; Pentax, Tokyo, Japan) by use of a Hitachi Avius processor (Hitachi, Tokyo, Japan) before ERCP to determine the cause of the dilated CBD and further characterize the echogenic shadow seen on US.
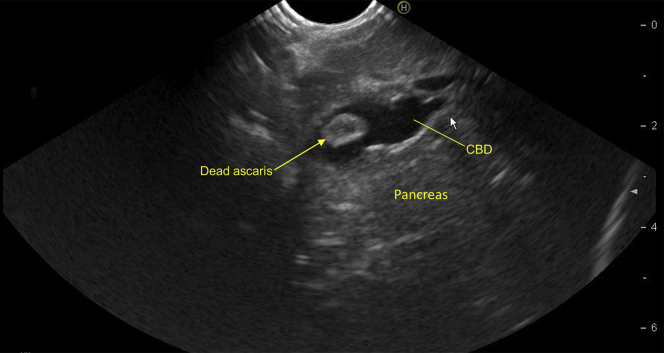
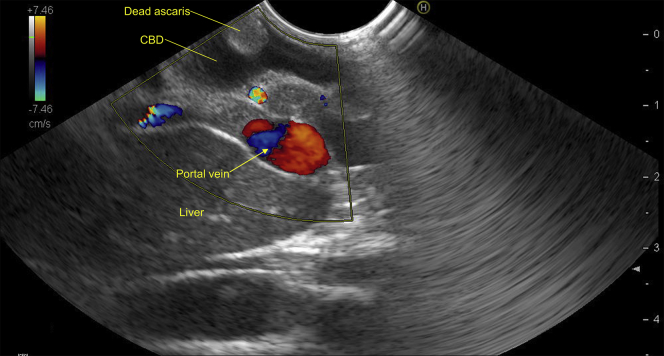
Linear EUS from the stomach revealed dilatation of the CBD to 14 mm, with a rounded hyperechoic structure without acoustic shadowing in the lower CBD (Figs. 1 and 2; Video 1, available online at www.VideoGIE.org). Linear EUS from the duodenal bulb with color Doppler imaging showed a hyperechoic avascular structure with a central anechoic area inside the CBD (Figs. 3 and 4; Video 1). This structure was without acoustic shadow, and it appeared to be attached to the wall of the CBD from one discrete attachment point, whereas the remaining structure was noted to move with the pulsatile flow of biliary secretions (Fig. 5). The central part of this structure was anechoic (Fig. 6).
Figure 1.
Linear EUS view from the stomach showing dilated CBD with rounded hyperechoic structure without acoustic shadowing in the lower CBD. CBD, common bile duct.
Figure 2.
Linear EUS view showing rounded hyperechoic structure in dilated common bile duct. CBD, common bile duct.
Figure 3.
Linear EUS view from duodenal bulb with color Doppler image showing hyperechoic avascular structure with a central anechoic area inside the common bile duct. CBD, common bile duct.
Figure 4.
Dual-color Doppler image showing avascular hyperechoic structure with vascular portal vein. CBD, common bile duct.
Figure 5.
Zoom image showing dead Ascaris attached to the wall of the CBD from 1 discrete attachment point, whereas the remaining structure was noted to move with the pulsatile flow of biliary secretions. CBD, common bile duct.
Figure 6.
The central part of the hyperechoic structure was anechoic. CBD, common bile duct.
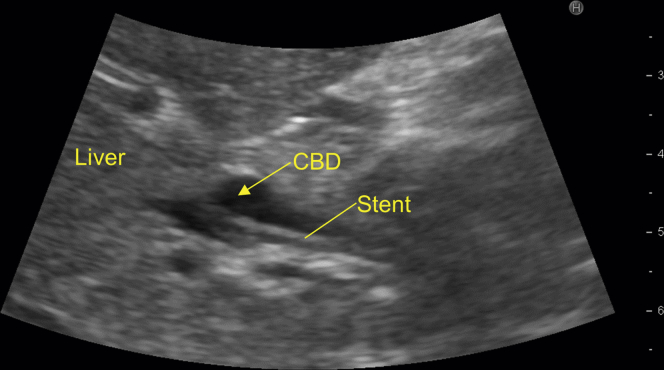
After biliary sphincterotomy and multiple balloon sweeps on ERCP, yellow fragments were removed, which were suggestive of recently fragmented Ascaris (Fig. 7; Video 1). Stool examination revealed eggs of Ascaris lumbricoides. Microscopic examination of the removed fragments showed features of Ascaris lumbricoides. The follow-up investigations revealed normalization of the diameter of the CBD with a stent in situ on US (Fig. 8) and normalization of liver test results.
Figure 7.
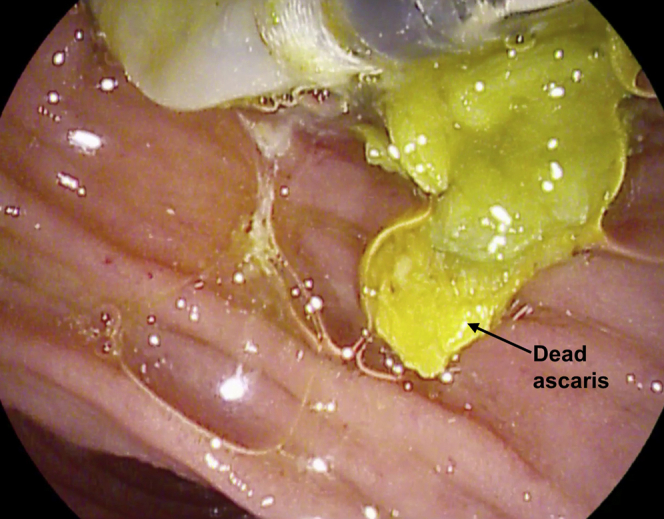
After biliary sphincterotomy and multiple balloon sweeps on ERCP, yellow fragments were removed, suggestive of recently fragmented Ascaris.
Figure 8.
US view of the abdomen showing CBD with stent inside. CBD, common bile duct.
The patient’s clinical condition improved significantly after ERCP. The patient underwent deworming with albendazole and passed multiple roundworms in his stool, further confirming the diagnosis of obstructive jaundice due to ascariasis.
Ascariasis is a common problem in tropical regions. The worm usually continues to survive in the bile duct or pancreatic duct, causing biliary colic, obstructive jaundice, cholangitis, or acute pancreatitis. Live Ascaris worms are usually identified on US or EUS and show the characteristic features of a linear mobile echogenic structure with a central anechoic lumen. However, in the present case, the anechoic lumen was not seen because the lumen disappears once the worm dies, and coiling can occur as the worm shrivels up and becomes smaller.
The diameter of the coiled structure in the present case was 8 mm, whereas a live worm is generally 8 to 10 cm long. Ascaris worms can die inside the bile duct and create a foreign body, which can act as a nidus for stone or sludge formation. Obstructive jaundice due to dead Ascaris is a rare but important disorder in the developing world. Because the worm shrivels up after death, accurate identification requires a high index of suspicion. The characteristic features of the dead worm on EUS include a hyperechoic structure without any acoustic shadow. A coiled dead Ascaris worm on EUS shows the appearance of a hyperechoic avascular structure with a central hypoechoic area inside the CBD. EUS is the most sensitive investigation for evaluation of a dilated CBD and can improve the sensitivity of diagnosis of pancreaticobiliary ascariasis.
Pancreaticobiliary ascariasis is usually treated by endoscopic intervention, which is performed by gently holding the live worm lying outside the ampulla with a basket or forceps. In this case, endoscopic removal of dead fragments was performed by a balloon. Treatment with antihelminthetics is recommended to prevent re-entry of any other roundworm residing in the small bowel.
In conclusion, we describe an unusual appearance of a dead Ascaris worm on EUS. Biliary ascariasis should be considered in any child presenting with obstructive jaundice in endemic regions.
Disclosure
All authors disclosed no financial relationships relevant to this publication.
Footnotes
Written transcript of the video audio is available online at www.VideoGIE.org.
Supplementary data
Linear EUS from the stomach revealed dilatated common bile duct (CBD) with rounded hyperechoic structure without acoustic shadowing in the lower CBD. Linear EUS from duodenal bulb with color Doppler imaging showed hyperechoic avascular structure with a central anechoic area inside the CBD. This structure was without acoustic shadow, and it appeared to be attached to the wall of the CBD from 1 discrete attachment point, whereas the remaining structure was noted to move with the pulsatile flow of biliary secretions. The central part of this structure was anechoic. After biliary sphincterotomy and multiple balloon sweeps on ERCP, yellow fragments were removed, which were suggestive of recently fragmented Ascaris.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Linear EUS from the stomach revealed dilatated common bile duct (CBD) with rounded hyperechoic structure without acoustic shadowing in the lower CBD. Linear EUS from duodenal bulb with color Doppler imaging showed hyperechoic avascular structure with a central anechoic area inside the CBD. This structure was without acoustic shadow, and it appeared to be attached to the wall of the CBD from 1 discrete attachment point, whereas the remaining structure was noted to move with the pulsatile flow of biliary secretions. The central part of this structure was anechoic. After biliary sphincterotomy and multiple balloon sweeps on ERCP, yellow fragments were removed, which were suggestive of recently fragmented Ascaris.