Abstract
Background
Multiple operative treatments are available for the fixation of intertrochanteric femoral fractures. This analysis was conducted to provide guidance on the appropriate clinical choice to accommodate individual patients.
Methods
A systematic review was performed to identify relevant articles in databases. Randomized controlled trials (RCTs) of adults with intertrochanteric femoral fractures were eligible if they compared 2 or more of the following interventions: proximal femoral nail anti-rotation (PFNA), percutaneous compression plate (PCCP) use, dynamic hip screw (DHS) fixation, gamma nail (GN) fixation, and artificial femoral head replacement (FHR). Bayesian network meta-analysis was performed to simultaneously compare all treatment methods.
Results
In total, 24 active-comparator studies involving 3097 participants were identified. Across all populations, greater reductions in blood loss and operation time were observed for PFNA than for other treatments. In terms of bleeding, more blood loss was observed for DHS use than for the PFNA (SMD, 1.96; 95% CI, 1.01–1.96), PCCP (SMD, 1.26; 95% CI, 0.31–2.20), and GN (SMD, 0.26; 95% CI, − 0.35–0.87) techniques. However, a more beneficial effect was observed for DHS use than for FHR (SMD, − 0.23; 95% CI, − 1.26–0.81). DHS use resulted in a significantly longer duration of operation time than the PFNA (SMD, 0.75; 95% CI, − 0.02–0.75), PCCP (SMD, 0.61; 95% CI, − 0.20–1.44), and GN (SMD, 0.25; 95% CI, − 0.26–0.77) techniques. Similarly, greater reductions in operation time were observed for DHS use than for FHR (SMD, − 0.12; 95% CI, − 1.15–0.91).
Conclusions
The findings provide supporting evidence demonstrating the superiority of PFNA over other treatments for intertrochanteric femoral fracture. PFNA treatment results in the lowest amount of blood loss and the shortest operation time. These findings add to the existing knowledge of intertrochanteric femoral fracture treatment options.
Keywords: Intertrochanteric hip fracture, Surgical intervention, Meta-analysis
Background
The incidence of intertrochanteric hip fracture, which accounts for 31–51% of proximal femoral fractures [1], has increased during the last decade. Accompanied by physical deterioration, this type of fracture is prevalent among geriatric patients. Furthermore, most patients with this type of fracture experience medical comorbidities, which can worsen complications if left untreated. Consequently, early surgery is considered the best option for these patients by the majority of clinicians worldwide. The advantages of surgery include the restoration of anatomical alignment and early rehabilitation [2]. Moreover, early surgery can reduce the risk of complications.
Fixation with dynamic hip screws (DHS) is generally considered the standard management option for treating these fractures and has gained extensive acceptance [3, 4]. However, various types of implants are available, including extramedullary and intramedullary devices. Consequently, the preferred treatment option remains controversial due to the lack of randomized controlled trials (RCTs) comparing these therapies. Accordingly, an analysis that integrates evidence of current on treatment options for intertrochanteric hip fracture is needed.
A traditional pairwise meta-analysis cannot simultaneously include various types of prevalent therapies. To identify the optimal treatment method, we compared all candidate therapies in the same analysis by performing a network of treatments meta-analysis involving a direct analysis and a combined analysis. We aimed to comprehensively integrate the current evidence regarding blood loss and operation time outcomes from operative interventions in patients with intertrochanteric fractures.
Materials and methods
Search strategy
EMBASE, MEDLINE, CNKI, and the Cochrane Library were searched. All searches were limited to RTCs involving humans. Searches were not limited by language, publication date, or publication status. We also reviewed the reference lists of all selected studies to identify any additional relevant articles. The searches incorporated the following keywords: “intertrochanteric fractures,” “proximal femoral nail anti-rotation,” “dynamic hip screw,” “gamma nail,” “percutaneous compression plate,” and “artificial femoral head replacement.”
Study selection
Studies that satisfied the following inclusion criteria were eligible for the analysis: (1) RCTs involving human participants treated for intertrochanteric hip fractures; (2) evaluations including either surgical time or blood loss, with complete data; (3) patients aged over 18 years; (4) the highest-quality study or the most recent publication in cases where data were duplicated; (5) comparison of at least two of the five treatments studied (DHS, PFNA, GN, PCCP, FHR).
Data extraction and quality assessment
The data were reviewed independently by two extractors. Extractors resolved any disagreements by consensus. The following details were extracted from each study: name of the first author, country of origin, sample size, year of publication, treatments compared, design, population characteristics, outcome measures, and fracture classification. The outcome measures of interest were surgical time and blood loss, as measured by change from baseline. The reviewers evaluated the methodological quality of all individual studies using the JADAD scale [5]. Particularly, the reviewers assessed the procedures of randomization sequence generation, appropriate blinding, allocation concealment, and reporting of withdrawal.
Statistical analysis
Eligible trials comprising direct and indirect comparisons were summarized qualitatively. In addition, essential clinical outcomes and methodological variables were recorded. We performed a traditional “head-to-head” meta-analysis to calculate the pooled estimates of the standard mean difference (SMD) and 95% confidence intervals (CIs). We conducted the statistical analysis using Stata version 11.0 (Stata Corporation, College Station, TX, USA) and developed a DerSimonian-Laird random effects model for comparisons between two strategies [6]. The Cochrane Q test and the I2 statistic were assessed to determine the effect of between-study heterogeneity [7, 8]. Begg’s test was also conducted to investigate publication bias [9].
We also performed a random effects Bayesian network meta-analysis to enhance the head-to-head meta-analysis. Using this method, all five treatments could be simultaneously considered. In addition, this method increases statistical power by merging both direct and indirect comparison evidence across all five interventions. Therefore, conclusions could be educed on the relative effectiveness of interventions, such as GN fixation and PCCP use, which have never before been directly compared.
The network meta-analyses were undertaken using Bayesian Markov chain Monte Carlo (MCMC) simulation methods with minimally informative prior distributions. Thousands of simulated iterations were run based on the data and description of the proposed distributions of relevant parameters in WinBUGS software (version 1.4.3. MRC Biostatistics Unite, Cambridge, UK) [10]. The first 10,000 iterations (burn-in) were discarded, and 40,000 further iterations were run. Pooled effect sizes are reported as posterior medians of SMDs, and the corresponding 95% credible intervals (CrIs) were applied using the 2.5th and 97.5th percentiles of the posterior distribution, which can be interpreted similar to conventional 95% CIs [11]. We also calculated the percentage contribution of each effect size in the evidence base, i.e., the probability that each treatment was the most effective therapy or the second most effective therapy, etc. The distribution of ranking probabilities is presented graphically.
Meta-regression analyses were conducted to evaluate whether the publication year and type of fractures could explain the latent heterogeneity. The inconsistency between direct and indirect comparisons was evaluated using the loop-specific method [12]. This approach evaluates the difference (inconsistency factor) and 95% CI, between direct and indirect estimations for a specific comparison. Inconsistency was defined as disagreement between direct and indirect evidence with a 95% CI excluding 0.
Results
Eligible studies and characteristics
After reviewing all selected studies, 24 trials involving five treatments met the selection criteria [13–36]. A total of 3097 individuals with sufficient data were included in the quantitative synthesis (meta-analysis). The study selection process, including reasons for exclusion, is presented by a flowchart (Fig. 1). The characteristics of all involved studies are summarized in Table 1. Figure 2 shows all comparisons analyzed within the network. The study sample size varied from 60 to 426 participants, with a median sample size of 129. The mean age of patients varied from 62.2 to 83.6 years. According to the Evans or AO/OTA classification, all fractures were categorized as stable (Evans type I/II and AO/ATO type 31-A1) or unstable (Evans type III–V and AO/ATO type 31-A2/A3). In 7 trials, all selected patients had unstable fractures; in 15 trials, all selected patients had compound fractures, either stable or unstable. We conducted a quality assessment of all included studies (Table 2) and found that the studies had a broad range of overall reporting quality. The proportions of studies with definite descriptions of randomization, allocation concealment, blinding, dropout, and intention-to-treat analysis were 83.33% (20/24), 70.83% (17/24), 62.5% (15/24), 87.5% (21/24), and 91.67% (22/24), respectively. According to meta-regression analyses, blood loss and operation time were not affected by differences across trials in terms of the publication year or type of fractures (Table 3). No evidence of inconsistency between the direct and indirect estimates was observed in this meta-analysis (Table 4). No publication bias was observed among the included studies (Table 5).
Fig. 1.
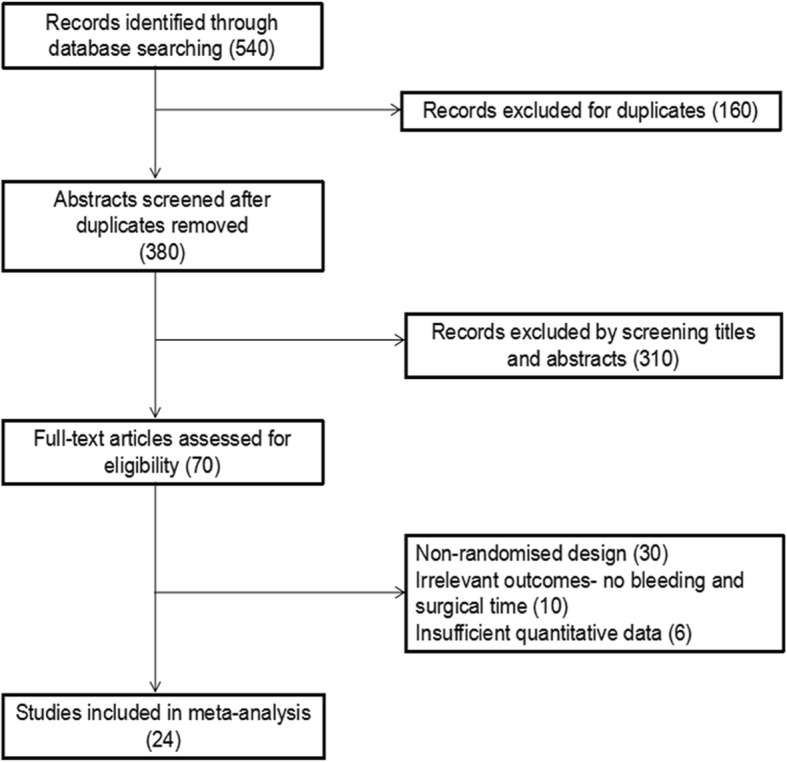
Flowchart of the study selection process
Table 1.
Baseline characteristics of included studies
| Author (year) | Country | Intervention | Mean age (years) | Patients (number) | Type of fractures (unstable/stable) |
|---|---|---|---|---|---|
| Tang 2009 | China | DHS, FHR | 80.7 | 109 | 109/0 |
| Verettas 2010 | Greece | DHS, GN | 80.1 | 118 | 118/0 |
| Zou 2009 | China | DHS, PFNA | 65 | 121 | 94/27 |
| Xu 2010 | China | DHS, PFNA | 78.2 | 106 | 106/0 |
| Wang 2010 | China | DHS, FHR | 83.5 | 60 | 60/0 |
| Peyser 2007 | Israel | DHS, PCCP | 80.8 | 103 | 60/22 |
| Ahrengart 2002 | Sweden | DHS, GN | 80 | 426 | 222/204 |
| Xu 2010 | China | PFNA, GN | 76.7 | 107 | 40/67 |
| Butt 1995 | UK | DHS, GN | 78.5 | 95 | 30/30 |
| Leung 1992 | China | DHS, GN | 79.6 | 186 | 50/136 |
| Kosygan 2002 | England | DHS, PCCP | 82.8 | 108 | 49/59 |
| Peter 1995 | Canada | DHS, GN | 80.1 | 102 | 58/44 |
| Kukla 1997 | Austria | DHS, GN | 83.5 | 120 | 54/66 |
| Yang 2011 | America | DHS, PCCP | 76.5 | 66 | NA |
| Hoffman 1996 | New Zealand | DHS, GN | 80.9 | 67 | 22/45 |
| Garg 2011 | India | DHS, PFNA | 62.2 | 81 | 81/0 |
| Guo 2013 | China | PFNA, PCCP | 72.9 | 90 | 49/41 |
| Brandt 2002 | Netherlands | DHS, PCCP | 80.9 | 71 | 41/30 |
| Aktselis 2014 | Greece | DHS, GN | 83 | 71 | 71/0 |
| Vaquero 2012 | Spain | PFNA, GN | 83.6 | 61 | 61/0 |
| Utrilla 2005 | Spain | DHS, GN | 80.2 | 210 | 54/156 |
| Goldhagen 1994 | America | DHS, GN | 78 | 63 | NA |
| Christopher 2001 | England | DHS, GN | 81 | 400 | 193/207 |
| Huang 2006 | China | DHS, FHR | 72.8 | 156 | 43/113 |
Fig. 2.
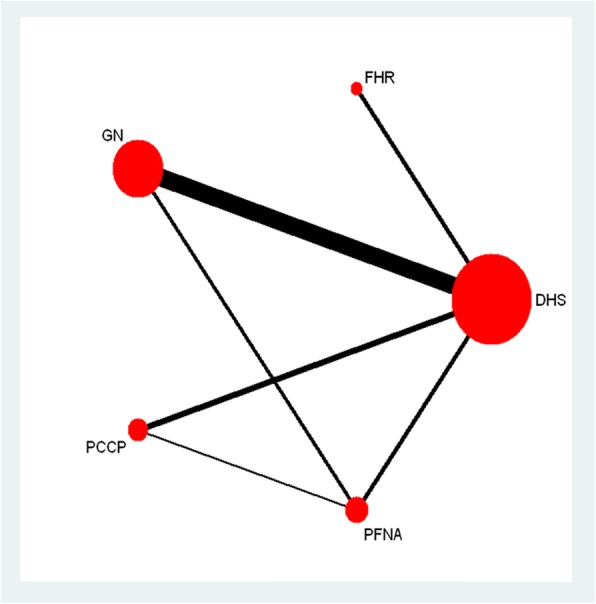
The eligible clinical trials included in the network meta-analysis. The width of the connecting lines is proportional to the number of available head-to-head (direct) comparisons. The size of each node is proportional to the number of randomly assigned participants (sample size)
Table 2.
Methodological quality assessment by adjusted Jadad scale
| Author | Random sequence generation | Allocation concealment | Blinding of participants | Dropout Addressed | ITT |
|---|---|---|---|---|---|
| Tang 2009 | Unclear | Unclear | Unclear | Adequate | Y |
| Verettas 2010 | Adequate | Unclear | Unclear | Adequate | Y |
| Zou 2009 | Inadequate | Unclear | Unclear | Unclear | Y |
| Xu 2010 | Adequate | Adequate | Adequate | Adequate | Y |
| Wang 2010 | Inadequate | Unclear | Unclear | Unclear | N |
| Peyser 2007 | Adequate | Adequate | Adequate | Adequate | Y |
| Ahrengart 2002 | Adequate | Adequate | Adequate | Adequate | Y |
| Xu 2010 | Adequate | Adequate | Adequate | Adequate | Y |
| Butt 1995 | Adequate | Adequate | Adequate | Unclear | Y |
| Leung 1992 | Adequate | Adequate | Inadequate | Adequate | Y |
| Kosygan 2002 | Adequate | Adequate | Adequate | Adequate | Y |
| Peter 1995 | Adequate | Adequate | Adequate | Adequate | Y |
| Kukla 1997 | Adequate | Adequate | Adequate | Adequate | Y |
| Yang 2011 | Adequate | Adequate | Adequate | Adequate | Y |
| Hoffman 1996 | Adequate | Adequate | Adequate | Adequate | Y |
| Garg 2011 | Adequate | Unclear | Unclear | Adequate | N |
| Guo 2013 | Adequate | Adequate | Unclear | Adequate | Y |
| Brandt 2002 | Adequate | Adequate | Adequate | Adequate | Y |
| Aktselis 2014 | Inadequate | Unclear | Unclear | Adequate | Y |
| Vaquero2012 | Adequate | Adequate | Adequate | Adequate | Y |
| Utrilla 2005 | Adequate | Adequate | Adequate | Adequate | Y |
| Goldhagen 1994 | Adequate | Unclear | Unclear | Unclear | Y |
| Christopher | Adequate | Adequate | Adequate | Adequate | Y |
| Huang 2006 | Adequate | Adequate | Adequate | Adequate | Y |
ITT intention-to-treat analysis
Table 3.
Results of the meta-regression
| Outcome | Regression coefficient(95%CI) | |
|---|---|---|
| Publication year | Type of fractures | |
| Blood loss | − 0.02 (− 0.11, 0.08) | − 0.70 (− 2.04, 0.64) |
| Operation time | − 0.32 (− 0.10, 0.04) | − 0.22 (− 1.28, 0.83) |
Table 4.
Assessment of inconsistency between direct and indirect evidence
| Loop | Blood loss | Operation time |
|---|---|---|
| Inconsistency 95% CI | Inconsistency 95% CI | |
| DHS,PCCP, PFNA | 3.59 (0.00, 7.33) | 1.82 (0.00, 5.77) |
| DHS, GN, PFNA | 2.66 (0.00, 4.77) | 0.71 (0.00, 2.71) |
Table 5.
Assessment of heterogeneity and publication bias for trials included indirect meta-analyses
| Comparisons | Number | Q-test heterogeneity(P/I2) | Begg’s test (p) |
|---|---|---|---|
| Blood loss | |||
| DHS vs PFNA | 2 | 0.00/98.3% | 1.00 |
| DHS vs GN | 7 | 0.01/66% | 0.76 |
| DHS vs PCCP | 3 | 0.00/82.9% | 1.00 |
| DHS vs FHR | 3 | 0.04/69.4% | 0.30 |
| PFNA vs GN | 1 | NA | NA |
| PFNA vs PCCP | 1 | NA | NA |
| Operation time | |||
| DHS vs PFNA | 3 | 0.00/98.8% | 0.30 |
| DHS vs GN | 11 | 0.00/91.5% | 1.00 |
| DHS vs PCCP | 4 | 0.00/92.9% | 0.73 |
| DHS vs FHR | 3 | 0.00/91.4% | 1.00 |
| PFNA vs GN | 2 | 0.63/0% | 1.00 |
| PFNA vs PCCP | 1 | NA | NA |
P < 0.05 indicates significant heterogeneity in Cochrane Q-test, publication bias in Begg’s test. NA not applicable
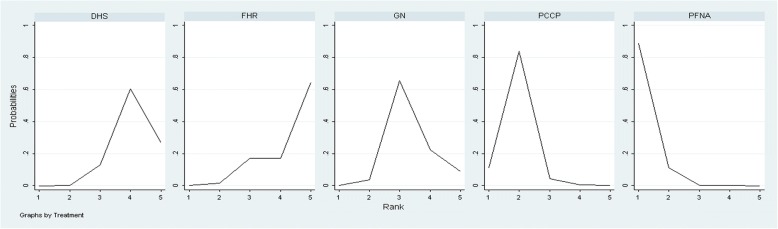
Blood loss
The results of our network meta-analysis comparing the five treatments regarding the outcome of blood loss are reported in Table 6. The outcome of five treatments ranked by the blood loss is also presented. Except for FHR, all interventions had greater effects on blood loss than DHS treatment. A relatively greater increase in blood loss was seen in DHS treatment than for PFNA (SMD 1.96; 95% CI, 1.014–1.963) or PCCP (SMD 1.26; 95% CI, 0.31–2.20) interventions (Table 6). This finding indicated that the PFNA intervention leads to the least blood loss among the five treatments studied. PFNA intervention consistently showed the highest probability of having the superior ranking position among all approaches, and PCCP use showed the second highest probability (Fig. 3).
Table 6.
Results of the direct and indirect meta-analyses
| a | ||||
| DHS | 3.41(0.13, 6.70) | 0.17(− 0.04, 0.38) | 0.71(0.11, 1.31) | − 0.19(− 0.61, 0.22) |
| 1.96(1.014, 1.963) | PFNA | − 0.43(− 0.81, − 0.04) | 0.93(0.50, 1.37) | NA |
| 0.26(− 0.35, 0.87) | − 1.70(− 2.74, − 0.66) | GN | NA | NA |
| 1.26(0.31, 2.20) | − 0.70(− 1.87, 0.46) | 1.00(− 0.10, 2.09) | PCCP | NA |
| − 0.23(− 1.26, 0.81) | − 2.19(− 3.60, − 0.77) | − 0.49(− 1.69, 0.71) | − 1.49(− 2.90, − 0.08) | FHR |
| b | ||||
| DHS | 1.24(− 1.36, 3.84) | 0.21(− 0.12, 0.54) | 0.34(− 0.49, 1.16) | − 0.12(− 0.92, 0.67) |
| 0.75(− 0.02, 0.75) | PFNA | − 0.30(− 0.60, 0.01) | 0.94(0.50, 1.37) | NA |
| 0.25(− 0.26, 0.77) | − 0.49(− 1.3, 0.33) | GN | NA | NA |
| 0.61(− 0.20, 1.44) | − 0.14(− 1.16, 0.88) | 0.35(− 0.59, 1.32) | PCCP | NA |
| − 0.12(− 1.15, 0.91) | − 0.86(− 2.15, 0.42) | − 0.37(− 1.52, 0.78) | − 0.72(− 2.03, 0.59) | FHR |
a Comparison of blood loss between 5 treatments. b Comparison of operation time between 5 treatments. Results of direct comparisons are listed in the upper triangle, and the estimation was calculated as the row-defining treatment compared with the column-defining treatment. Results of network meta-analysis are listed in the lower triangle, and the estimation was calculated as the column-defining treatment compared with the row-defining treatment
Fig. 3.
Ranking probability curves for blood loss during the operation. The graph displays the distribution of probabilities for each treatment. The X-axis represents the rank, and the Y-axis represents probabilities. The ranking indicates the probability that a particular treatment is the “best,” “second best,” etc
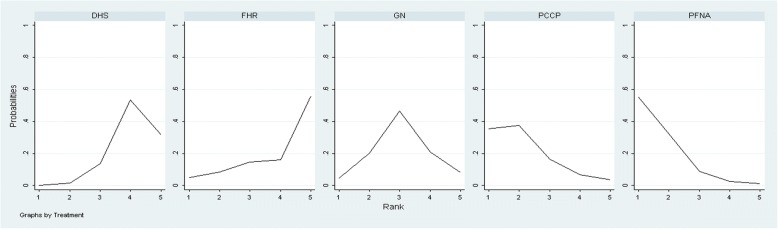
Operation time
Table 6 shows the results of the network meta-analysis on the outcome of operation time. Except for FHR, all interventions had greater effects on operation time than DHS treatment. A relatively longer operation time was observed for DHS than for PFNA (SMD 0.75; 95% CI, − 0.02–0.75) or PCCP (SMD 0.61; 95% CI, − 0.20–1.44) interventions. A significantly shorter duration was observed for the PFNA approach than for GN (SMD − 0.49; 95% CI, − 1.3–0.33), or FHR use (SMD − 0.86; 95% CI, − 2.15–0.42). Therefore, PFNA, PCCP, and GN interventions resulted in significantly greater decreases in operation time. Figure 4 shows that among the five treatments, PFNA treatment exhibited the highest probability of reducing the operation time, and PCCP treatment had the second highest probability.
Fig. 4.
Ranking probability curves for operation time. The graph displays the distribution of probabilities for each treatment. The X-axis represents the rank, and the Y-axis represents probabilities. The ranking indicates the probability that a particular treatment is the “best,” “second best,” etc
Discussion
This network meta-analysis reviewed existing evidence for the treatment of intertrochanteric hip fractures, with the aim to synthesize the evidence and to confirm decision-making in the absence of direct comparisons. Almost all previous RCTs or meta-analysis studies were evaluations of direct comparisons among DHS, GN, PFNA, and PCCP approaches. Few studies compared FHR with these treatments. Our findings integrate these previous comparisons.
With the rapid increase in the aging population, intertrochanteric hip fractures have shown an increasing trend. This type of fracture is a worldwide health problem, leading to serious medical consequences that interfere with quality of life and mortality [37]. During the past decades, this type of fracture has resulted in increased economic burden and has led to increased consumption of health care resources [38]. Nevertheless, considerable debate and controversy still exist regarding the optimal method and device for fixation of intertrochanteric fractures.
The DHS, which is an extramedullary fixation device, has previously been considered the gold standard treatment for intertrochanteric fractures [39]. However, this intervention, although technically simpler, requires a considerable amount of exposure and ambient soft tissue stripping, which can lead to heavy bleeding [40]. The disadvantages of traditional internal fixation, such as increased blood loss, postoperative pain, and slow function recovery, led to the emergence of a minimally invasive surgical option as an alternative treatment technique [41]. PCCP is a new type of minimally invasive surgical device. It consists of a biaxial, two parallel femoral neck screws, and three cortical screws. We can insert the screws through two 2-cm incisions percutaneously. Compared with DHS implants, it can reduce the damage of the lateral cortex and lateral femoral muscles. GN is an intramedullary implant with a short lever arm and a small bending moment. Compared with DHS implants, this implant has two advantages: The relatively semi-closed operation through a small incision does not require exposure of the fracture site; in addition, sliding screws can generate pressure on the proximal medial cortex to increase the stability of internal plants and fracture site. Therefore, inserting GN nails helps to reduce blood loss and shorten the operation time. PFNA intervention involves an innovative implant developed by the AO/ASIF group that is based on a proximal femoral nail (PFN) with a special helical blade. We found that PFNA treatment leads to the lowest amount of blood loss and the shortest operation time among the five treatments.
After PFNA, the amount of blood loss for each method ranked in the following increasing order: PCCP, GN, FHR, and DHS. Less blood loss during an operation leads to fewer incidences of allogenic blood and reduces potential risks of transfusion reactions, disease transmission and immunomodulation [42–44]. The risk of a serious or fatal transfusion-transmitted disease is approximately 3 in 10,000, while the chance of a minor allogenic reaction is 1 in 100 [42]. Regarding the reduction in operation time, PFNA treatment was also ranked as the top intervention. A shorter surgical time reduces the risk of minor or major anesthesia problems and blood loss, which helps to prevent the occurrence of anemia and hypoalbuminemia and improves patient recovery. Additionally, from a mechanical point of view, adequate evidence has demonstrated the superiority of the helical blade over a sliding hip screw for head stabilization and fragment sliding. The distinctive design consists of a large surface and an incremental core diameter, assuring maximum compaction and optimal hold in the bone. Because the PFNA blade can induce compaction of cortical bone, the increased rotational and angular stability can resist rotation and varus collapse of the head, as shown in cadaveric studies [45]. Therefore, PFNA, one type of modified minimally invasive implant technique used for internal fixation in elderly patients, is generally accepted in modern treatment of orthopedic trauma [46, 47].
The advantages of our analysis are that we simultaneously compared more than two treatments in the same analysis and provided relative effect estimates for all treatment comparisons, even for those that have not been directly compared before; thus, for each treatment, we estimated the probability that the given treatment is optimal. However, there are several limitations of our network meta-analyses that need to be acknowledged. First, we only analyzed total blood loss and surgical time because these were the most frequently reported outcomes in all included studies. However, many other outcomes should be considered, such as postoperative functional status, radiation time, complication rate, and fixation failure. Additional clinical trials and longitudinal studies with these outcomes may be reported in the future, enabling similar analyses. Second, statistical heterogeneity was moderate; however, most comparisons had wide 95% CIs and included values that indicated very high or no heterogeneity. Existing uncertainties regarding the potential heterogeneity of these studies should be explored.
Conclusion
In conclusion, PFNA is biomechanically and biologically superior to other implant techniques for treating intertrochanteric hip fractures. It provides stable intramedullary fixation to resist varus collapse, leading to the lowest amount of blood loss and the shortest operation time.
Acknowledgments
Funding
Each author certifies that he, or a member of his immediate family, has no funding or commercial associations (e.g., consultancies, stock ownership, equity interest, patent/licensing arrangements) that might pose a conflict of interest in connection with the submitted article.
All ICMJE Conflict of Interest Forms for authors and Journal of Orthopaedic Surgery and Research®editors and board members are on file with the publication and can be viewed on request.
Abbreviations
- CI
Confidence interval
- CNKI
Chinese National Knowledge Infrastructure
- DHS
Dynamic Hip Screw
- FHR
Artificial Femoral Head Replacement
- GN
Gamma Nail
- NA
Not applicable
- PCCP
Percutaneous Compression Plate
- PFNA
Proximal Femoral Nail Anti-rotation
- RCT
Randomized Controlled Trial
- SMD
Standard mean difference
Authors’ contributions
Both ZAH and XFW contribute equally to this paper. This paper is approved by all authors for publication. All authors contribute to the data analysis and in drafting and critically revising the paper and agree to be accountable for all aspects of the work. All authors read and approved the final manuscript.
Ethics approval and consent to participate
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published map and institutional affiliations.
Footnotes
This work was performed at Yuhang Branch of the Second Affiliated Hospital of Zhejiang University, Hangzhou, China.
Contributor Information
Zhengan Hao, Email: zheanhao@163.com.
Xifeng Wang, Email: wangxifeng816@163.com.
Xingqun Zhang, Email: sunshine46816@163.com.
References
- 1.Adams CI, Robinson CM, Court-Brown CM, Mcqueen MM. Prospective randomized controlled trial of an intramedullary nail versus dynamic screw and plate for intertrochanteric fractures of the femur. J Orthop Trauma. 2001;15:394–400. doi: 10.1097/00005131-200108000-00003. [DOI] [PubMed] [Google Scholar]
- 2.Ahrengart L, Törnkvist H, Fornander P, Thorngren KG, Pasanen L, Wahlström P, et al. A randomized study of the compression hip screw and Gamma nail in 426 fractures. Clin Orthop Relat Res. 2002;401:209–222. doi: 10.1097/00003086-200208000-00024. [DOI] [PubMed] [Google Scholar]
- 3.Aktselis I, Kokoroghiannis C, Fragkomichalos E, Koundis G, Deligeorgis A, Daskalakis E, et al. Prospective randomised controlled trial of an intrame-dullary nail versus a sliding hip screw for intertrochanteric fractures of the femur. Int Orthop. 2014;38:155–161. doi: 10.1007/s00264-013-2196-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Anothaisintawee T, Attia J, Nickel JC, Thammakraisorn S, Numthavaj P, McEvoy M, et al. Management of chronic prostatitis/chronic pelvic pain syndrome:a systematic reviewand network meta-analysis. JAMA. 2011;305:78–86. doi: 10.1001/jama.2010.1913. [DOI] [PubMed] [Google Scholar]
- 5.Butt MS, Krikler SJ, Nafie S, Ali MS. Comparison of dynamic hip screwand gammanail: a prospective, randomized, controlled trial. Injury. 1995;26:615–618. doi: 10.1016/0020-1383(95)00126-T. [DOI] [PubMed] [Google Scholar]
- 6.Caldwell DM, Ades AE, Higgins JPT. Simultaneous comparison of multiple treatments: combining direct and indirect evidence. BMJ. 2005;33:897–900. doi: 10.1136/bmj.331.7521.897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chaimani A, Higgins JPT, Mavridis D, Spyridonos P, Salanti G. Graphical tools for network meta-analysis in STATA. PLoS One. 2013;8:e76654. doi: 10.1371/journal.pone.0076654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cheng T, Zhang G, Zhang X. Review: minimally invasive versus conventional dynamic hip screw fixation in elderly patients with intertrochanteric fractures: a systematic review and meta-analysis. Surg Innov. 2011;18:99–105. doi: 10.1177/1553350611409062. [DOI] [PubMed] [Google Scholar]
- 9.Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0.The Cochrane Collaboration, 2011; Available at: http://handbook-5-1.cochrane.org/. Accessed 29 Mar 2011.
- 10.DerSimonian R, Laird N. Meta-analysis in clinical trials. Controlled Clin Trials. 1986;7:177–188. doi: 10.1016/0197-2456(86)90046-2. [DOI] [PubMed] [Google Scholar]
- 11.Dodd RY. The risk of transfusion-transmitted infection. N Engl J Med. 1992;327:419–421. doi: 10.1056/NEJM199208063270610. [DOI] [PubMed] [Google Scholar]
- 12.Doppelt SH. The sliding compression screw—today’s best answer for stabilization of intertrochanteric hip fractures. Orthop Clin North Am. 1980;11:507–523. [PubMed] [Google Scholar]
- 13.Eastwood EA, Magaziner J, Wang J, Silberzweig SB, Hannan EL, Strauss E, et al. Patients with hip fracture: subgroups and their outcomes. J Am Geriatr Soc. 2002;50:1240–1249. doi: 10.1046/j.1532-5415.2002.50311.x. [DOI] [PubMed] [Google Scholar]
- 14.Garg B, Marimuthu K, Kumar V, Malhotra R, Kotwal PP. Outcome of short proximalfemoral nail antirotation and dynamic hip screw for fixation of unstable trochanteric fractures. A randomised prospective comparative trial. Hip Int. 2011;21:531–536. doi: 10.5301/HIP.2011.8657. [DOI] [PubMed] [Google Scholar]
- 15.Goldhagen PR, O'Connor DR, Schwarze D, Schwartz E. A prospective comparative s-tudy of the compression hip screw and the gamma nail. J Orthop Trauma. 1994;8:367–372. doi: 10.1097/00005131-199410000-00001. [DOI] [PubMed] [Google Scholar]
- 16.Guo Q, Shen Y, Zong Z, Zhao Y, Liu H, Hua X, et al. Percutaneous compressionplate versus proximal femoral nail anti-rotation in treating elderly patients with intertrochanteric fractures: a prospective randomized study. J Orthop Sci. 2013;18:977–986. doi: 10.1007/s00776-013-0468-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Haidukewych GJ, Israel TA, Berry DJ. Reverse obliquity fractures of the intertrochanteric region of the femur. J Bone Joint Surg Am. 2001;83-A:643–650. doi: 10.2106/00004623-200105000-00001. [DOI] [PubMed] [Google Scholar]
- 18.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21:1539–1558. doi: 10.1002/sim.1186. [DOI] [PubMed] [Google Scholar]
- 19.Higgins JP, Whitehead A. Borrowing strength from external trials in a meta-analysis. Stat Med. 1996;15:2733–2749. doi: 10.1002/(SICI)1097-0258(19961230)15:24<2733::AID-SIM562>3.0.CO;2-0. [DOI] [PubMed] [Google Scholar]
- 20.Hoffman CW, Lynskey TG. Intertrochanteric fractures of the femur: a randomized pr-ospective comparison of the Gamma nail and the Ambi hip screw. ANZ J Surg. 1996;66:151–155. doi: 10.1111/j.1445-2197.1996.tb01144.x. [DOI] [PubMed] [Google Scholar]
- 21.Huang XQ, Liao YH, Wang XD, Wang XM, Gon SH. Recovery of lower limb func-tion in elder patients with intertrochanteric fractures treated with hip joint replacement versus dynamic hip screw. Chin J Clil Reha. 2006;4:36–38. [Google Scholar]
- 22.Jadad AR, Moore RA, Carroll D, Jenkinson C, Reynolds DJ, Gavaghan DJ, et al. Assessing the quality of reports of randomized clinical trials: is blinding necessary? Control Clin Trials. 1996;17:1–12. doi: 10.1016/0197-2456(95)00134-4. [DOI] [PubMed] [Google Scholar]
- 23.Kosygan KP, Mohan RNewman RJ. The Gotfried percutaneous compression plate co-mpared with the conventional classic hip screw for the fixation of intertrochanteric f-ractures of the hip. J Bone Joint Surg Br. 2002;84:19–22. doi: 10.1302/0301-620x.84b1.11919. [DOI] [PubMed] [Google Scholar]
- 24.Kukla C, Heinz T, Berger G, Kwasny O, Rosenberger A, Vécsei V. Gamma nail vs. dynamic hip screw in 120 patients over 60 years—a randomized trial. Eur Surg. 1997;29:290–293. doi: 10.1007/BF02621324. [DOI] [Google Scholar]
- 25.Leslie WD, Metge CJ, Mahmoud A, Lix LM, Finlayson GS, Morin SN, et al. Direct costs of fractures in Canada and trends 1996-2006: a population-based cost-of-illness analysis. J Bone Miner Res. 2011;26:2419–2429. doi: 10.1002/jbmr.457. [DOI] [PubMed] [Google Scholar]
- 26.Leung KS, So WS, Shen WY, Hui PW. Gamma nails and dynamic hip screws for p-eritrochanteric fractures. A randomised prospective study in elderly patients. J Bone Joint Surg Br. 1992;74:345–351. doi: 10.1302/0301-620X.74B3.1587874. [DOI] [PubMed] [Google Scholar]
- 27.Linden JV, Kaplan HS. Transfusion errors: causes and effects. Transfus Med Rev. 1994;8:169–183. doi: 10.1016/S0887-7963(94)70109-7. [DOI] [PubMed] [Google Scholar]
- 28.Lorich DG, Geller DS, Nielson JH. Osteoporotic pertrochanteric hip fractures: management and current controversies. Instr Course Lect. 2004;53:441–454. [PubMed] [Google Scholar]
- 29.O'Brien PJ, Meek RN, Blachut PA, Broekhuyse HM, Sabharwal S. Fixation of intertrochanteric hip fractures: gamma nail versus dynamic hip screw. A randomized, prospective study. Can J Surg. 1995;38:516–520. [PubMed] [Google Scholar]
- 30.Parker MJ, Gurusamy K Modern methods of treating hip fractures. Disabil Rehabil 2005; 27:1045–1051. [DOI] [PubMed]
- 31.Parker MJ, Handoll HH. Gamma and other cephalocondylic intramedullarynails versus extramedullary implants for extracapsular hip fractures in adults. Cochrane Database Syst Rev. 2008;16:CD000093. doi: 10.1002/14651858.CD000093.pub4. [DOI] [PubMed] [Google Scholar]
- 32.Perkins HA. Transfusion-induced immunologic unresponsiveness. Transfus Med Rev. 1988;2:196–203. doi: 10.1016/S0887-7963(88)70045-0. [DOI] [PubMed] [Google Scholar]
- 33.Peyser A, Weil YA, Brocke L, Sela Y, Mosheiff R, Mattan Y, et al. A prospective, randomised study comparing the percutaneous compression plate and the compression hip screw for the treatment of intertrochanteric fractures of the hip. J Bone Joint Surg Br. 2007;89:1210–1217. doi: 10.1302/0301-620X.89B9.18824. [DOI] [PubMed] [Google Scholar]
- 34.Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for p-resenting results from multiple treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;64:163–171. doi: 10.1016/j.jclinepi.2010.03.016. [DOI] [PubMed] [Google Scholar]
- 35.Spiegelhalter D, Thomas A, Best N, Lunn D. WinBugs version 1.4 user manual. Cambridge: MRC Biostatistics Unit; 2003. [Google Scholar]
- 36.Strauss E, Frank J, Lee J, Kummer FJ, Tejwani N. Helical blade versus sliding hip screw for treatment of unstable intertrochanteric hip fractures: a biomechanical evaluation. Injury. 2006;37:984–989. doi: 10.1016/j.injury.2006.06.008. [DOI] [PubMed] [Google Scholar]
- 37.Tang C, Xiang Z, Shen X. Prospective study of artificial femoral head replacement and DHS internal fixation for comminuted femoral intertrochanteric fractures in elderly patients. Chin J Bone Joint Injury. 2009;9:778–780. [Google Scholar]
- 38.Utrilla AL, Reig JS, Muñoz FM, Tufanisco CB. Trochanteric gamma nail and compression hip screw for trochanteric fractures: a randomized, prospective, comparative study in 210 elderly patients with a new design of the gamma nail. J Orthop Trauma. 2005;19:229–233. doi: 10.1097/01.bot.0000151819.95075.ad. [DOI] [PubMed] [Google Scholar]
- 39.Verettas DA, Ifantidis PC. Systematic effects of surgical treatment of hip fractures: gl-iding screw-plating vs intramedullary nailing. Injury. 2010;41:279–284. doi: 10.1016/j.injury.2009.09.012. [DOI] [PubMed] [Google Scholar]
- 40.Wandel S, Jüni P, Tendal B, Nüesch E, Villiger PM, Welton NJ, et al. Effects of glucosamine, chondroitin, or placebo in patients with osteoarthritis of hip or knee: network meta-analysis. BMJ. 2010;341:c4675. doi: 10.1136/bmj.c4675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang Y, He P, Wei L. A randomly controlled study of instable intertrochanteric fractures of the femur in elderly patients treated by artificial femoral head replace-ment and DHS internal fixation. Chin J Bone Joint Injury. 2010;10:869–872. [Google Scholar]
- 42.White JJ, Khan WS, Smitham PJ. Perioperative implications of surgery in elderly patients with hip fractures: an evidence-based review. J Perioper Pract. 2011;21:192–197. doi: 10.1177/175045891102100601. [DOI] [PubMed] [Google Scholar]
- 43.Xu YZ, Geng DC, Mao HQ, Zhu XS, Yang HL. A comparison of the proximal fem-oral nail antirotation device and dynamic hip screw in the treatment of unstable pertrochanteric fracture. J Int Med Res. 2010;38:1266–1275. doi: 10.1177/147323001003800408. [DOI] [PubMed] [Google Scholar]
- 44.Xu YZ, Geng DC, Yang H, Zhu GM, Wang XB. Comparative study of trochanteric fracture treated with the proximal femoral nail anti-rotation and the third generation of gamma nail. Injury. 2010;41:1234–1238. doi: 10.1016/j.injury.2010.03.005. [DOI] [PubMed] [Google Scholar]
- 45.Zou J, Xu Y, Yang H. A comparison of proximal femoral nail antirotation and dynamic hip screw devices in trochanteric fractures. J Int Med Res. 2009;37:1057–1064. doi: 10.1177/147323000903700410. [DOI] [PubMed] [Google Scholar]
- 46.Yang E, Qureshi S, Trokhan S, Joseph D. Gotfried percutaneous compression plating compared with sliding hip screw fixation of intertrochanteric hip fractures: a prospect-ive randomized study. J Bone Joint Surg Am. 2011;93:942–947. doi: 10.2106/JBJS.I.00849. [DOI] [PubMed] [Google Scholar]
- 47.Zhou Z, Zhang X, Tian S, Wu Y. Minimally invasive versus conventional dynamic hip screw for the treatment of intertrochanteric fractures in older patients. Orthopedics. 2012;35:e244–e249. doi: 10.3928/01477447-20120123-42. [DOI] [PubMed] [Google Scholar]