Abstract
Introduction
The toxinotyping and antimicrobial susceptibility of Clostridium perfringens strains isolated from processed chicken meat were determined.
Material and Methods
Two hundred processed chicken meat samples from luncheon meats, nuggets, burgers, and sausages were screened for Clostridium perfringens by multiplex PCR assay for the presence of alpha (cpa), beta (cpb), epsilon (etx), iota (ia), and enterotoxin toxin (cpe) genes. The C. perfringens isolates were examined in vitro against eight antibiotics (streptomycin, amoxicillin, ampicillin, ciprofloxacin, lincomycin, cefotaxime, rifampicin, and trimethoprim-sulfamethoxazole)
Results
An overall of 32 C. perfringens strains (16%) were isolated from 200 processed chicken meat samples tested. The prevalence of C. perfringens was significantly dependent on the type of toxin genes detected (P = 0.0), being the highest in sausages (32%), followed by luncheon meats (24%), burgers (6%), and nuggets (2%). C. perfringens type A was the most frequently present toxinotype (24/32; 75%), followed by type D (21.9 %) and type E (3.1%). Of the 32 C. perfringens strains tested, only 9 (28%) were enterotoxin gene carriers, with most representing type A (n = 6). C. perfringens strains differed in their resistance/susceptibility to commonly used antibiotics. Most of the strains tested were sensitive to ampicillin (97%) and amoxicillin (94%), with 100% of the strains being resistant to streptomycin and lincomycin. It is noteworthy that the nine isolates with enterotoxigenic potential had a higher resistance than the non-enterotoxigenic ones.
Conclusion
The considerably high C. perfringens isolation rates from processed chicken meat samples and resistance to some of the commonly used antibiotics indicate a potential public health risk. Recent information about the isolation of enterotoxigenic C. perfringens type E from chicken sausage has been reported.
Keywords: processed chicken meat, Clostridium perfringens, enterotoxin, antimicrobial resistance
Introduction
The microbiological quality and safety of meat are significant for the health of consumers around the world (25). Anaerobic bacteria constitute an important group of microorganisms that are responsible for many public health hazards. C. perfringens is a member of this group that is more widely spread than others, since its principal habitats are the soil and intestinal contents of humans and animals (18). Disease flare-up due to C. perfringens can have various origins, one of which is poultry (15).
In poultry, C. perfringens constitutes a human health hazard through the food chain and is one of the most frequently isolated bacterial pathogens from chicken meat, constituting up to 70%-98% of the cases (7, 9). C. perfringens is an omnipresent pathogen of the intestinal tract of poultry, associated with different phases of poultry growth and production. Chicken carcasses and meat parts may likewise be contaminated with C. perfringens during evisceration in the slaughterhouse (29).
C. perfringens causes a number of human diseases ranging from necrotic enteritis to wound infection and life-threatening gas gangrene (21). C. perfringens has been grouped into five types (A-E) based on toxins produced (alpha, beta, epsilon, and iota). The alpha toxin is produced by all the types of Clostridium perfringens. The toxin is a necrotising toxin which is believed to be a virulence marker (4, 22). In addition, C. perfringens produces other minor toxins, such as enterotoxins, which are not associated with a specific strain and are responsible for causing the gastrointestinal disorders that may be food- or non-food-borne.
The enterotoxin gene (cpe) exists on either a chromosome in food-poisoning isolates or a large conjugative plasmid in non-food-borne gastrointestinal disease (12).
Our study aimed to detect the presence of C. perfringens in processed chicken meat samples (luncheon, nuggets, burger, and sausage) and characterise the isolates for the existence of enterotoxin gene. In addition, the in vitro resistance of C. perfringens isolates against certain antibiotics was determined.
Material and Methods
Samples
In total, 200 processed chicken meat samples of luncheon, nuggets, burger, and sausage (n = 50 each) were collected from different markets in Cairo during the period from March to April 2015. When collected, the samples were directly transferred in iceboxes to the laboratory.
C. perfringens isolation and identification
Ten grams of each sample was diluted in 90 mL of sterile 0.1% peptone water and homogenised in a blender at 2000 rpm for 1 -2 min. About 1 mL of each homogenised food suspension was inoculated into cooked meat broth tubes and incubated anaerobically at 37°C for 48 h. A loopful form each tube was streaked on neomycin sulphate sheep blood agar plates and incubated anaerobically for a further 48 h. Suspected colonies were examined microscopically and biochemically (9).
DNA extraction and PCR assay
DNA was extracted from pure colonies of C. perfringens that showed a double zone of haemolysis on blood agar by using an extraction kit (QIA amp Mini Kit, Qiagen, Germany). Specific oligonucleotide primers for the alpha (cpa), beta (cpb), epsilon (etx), iota (ia), and enterotoxin toxin (cpe) genes of C. perfringens were used as described in Table 1. Multiplex PCR assay was carried out in a reaction mixture (25 uL) containing 1 uL of template DNA, 12.5 uL of Dream Taq Green PCR Master mix, 0.5 uL of each primer (10 pmol/uL), and 10.5 uL of DNase-free water. PCR amplification was carried out in a Biometra PCR thermal cycler. Following initial denaturation for 3 min at 94°C, the samples were subjected to 35 cycles of denaturation at 94°C for 1 min, annealing at 55°C for 1 min, extension at 72°C for 1 min, and final extension for 10 min at 72°C (28). The PCR reaction mixtures were analysed by electrophoresis using 1.5% (w/v) agarose gel in the presence of 100 bp DNA ladder (Fermentas Life Science, EU) (14). Types D and E, and positive-control of national C. perfringens strains were also included in the PCR.
Table 1.
Multiplex PCR primers for five toxins genes of C. perfringens
| Gene | Primer Sequence | Amplified size (bp) | Reference |
|---|---|---|---|
| cpa | GCTAATGTTACTGCCGTTGA CCTCTGATACATCGTGTAAG |
324 | |
| cpb | GCGAATATGCTGAATCATCTA GCAGGAACATTAGTATATCTTC |
196 | |
| etx | GCGGTGATATCCATCTATTC CCACTTACTTGTCCTACTAAC |
655 | (14) |
| ia | ACTACTCTCAGACAAGACAG CTTTCCTTCTATTACTATACG` |
446 | |
| cpe | ACTACTCTCAGACAAGACAG CTTTCCTTCTATTACTATACG` |
233 | |
Antimicrobial sensitivity test
Thirty-two C. perfringens isolates were examined in vitro against eight antibiotics, which included streptomycin (10 μg), amoxicillin (10 μg), ampicillin (10 μg), ciprofloxacin (5 μg), lincomycin (30 μg), cefotaxime (30 μg), rifampicin (5 μg), and trimethoprim-sulfamethoxazole (1.25 + 23.75 μg) (Oxoid, UK). The test was carried out using the agar disc diffusion test, (17, 26). The isolates were cultured anaerobically at 37° for 24 h in 10% neomycin sheep blood agar, then suspended in 0.9% NaCl to a 0.5 McFarland standard. Every isolate was inoculated onto Mueller-Hinton agar plates (Remel, USA) and the antibiotic discs were applied. The plates were incubated anaerobically at 37° for 24 h. The interpretation of the results was performed according to CLSI, 2012 (8).
Statistical analysis
PASW Statistics, Version 18.0. software (SPSS Inc., USA) was used to analyse the data. The Chi square (x2) test was applied (provided that at least 80% of the cells had an expected frequency of five or greater, and that no cell had an expected frequency smaller than 1.0). Otherwise, the Fisher-Freeman-Halton Exact test was used (i.e. the Fisher's Exact test for contingency tables larger than 2x2). A value of P < 5 was considered as significant.
Results
Overall, 32 C. perfringens isolates were obtained from 200 processed chicken meat samples (luncheon, nuggets, burger, and sausage; 50 of each with an incidence of 16%, Table 2). There was a relationship between the kind of meat and the occurrence of C. perfrigens. A high isolation rate was observed in sausage samples (16/50), followed by luncheon (12/50), while nuggets showed the lowest rate (1/50). The results in Table 2 show that the rate of C. perfringens type A was high (24/32), followed by that of type D (7/32), and then the unprecedented isolation of type E in sausage (1/32).
Table 2.
Occurrence of C. perfringens among examined samples and typing of C. perfringens isolates by using multiplex PCR
| C. perfringens type | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sample | Number of samples | |||||||||||
| Positive samples | A | D | E | P-Value | ||||||||
| Number | % | Number | % | Number | % | Number | % | |||||
| Luncheon | 50 | 12 | 24 | 9 | 75 | 3 | 25 | 0 | 0 | 0.0* | ||
| Nuggets | 50 | 1 | 2 | 1 | 100 | 0 | 0 | 0 | 0 | 1.0 | ||
| Burger | 50 | 3 | 6 | 3 | 100 | 0 | 0 | 0 | 0 | 0.035* | ||
| Sausage | 50 | 16 | 32 | 11 | 69 | 4 | 25 | 1 | 6 | 0.0* | ||
| Total | 200 | 32 | 16 | 24 | 75 | 7 | 21.9 | 1 | 3.1% | 0.0* | ||
| P-value | 0.000* | 0.885 | 0.999 | 1.000 | ||||||||
a significant difference
Fig. 1A shows the amplification of alpha toxin gene at 324 bp, representing C. perfringens type A, while amplifications of epsilon toxin gene at 655 bp and alpha toxin gene represented C. perfringens type D. In addition, Fig. 1A shows the presence of enterotoxigenic C. perfringens gene (cpe) at 233 bp. In Fig. 1B, type C was used as a positive control revealing two bands, one at 324 bp for the alpha gene and another at 196 bp for the beta gene. Fig. 1B also shows the amplification of iota toxin gene at 446 bp and alpha toxin gene representing the isolated C. perfringens type E. The cpe gene was represented in Fig. 1 by amplification at 233 bp for enterotoxigenic C. perfringens type A (Fig. 1A) and C. perfringens enterotoxin type E (Fig. 1B). According to Table 3, the enterotoxigenic isolates which carried cpe gene amounted to 9 out of 32 C. perfringens isolates with an incidence of 28 %. Enterotoxigenic C. perfringens type A was most frequently isolated (6/24), followed by type D (2/7), and then type E (1/1).
Fig. 1.
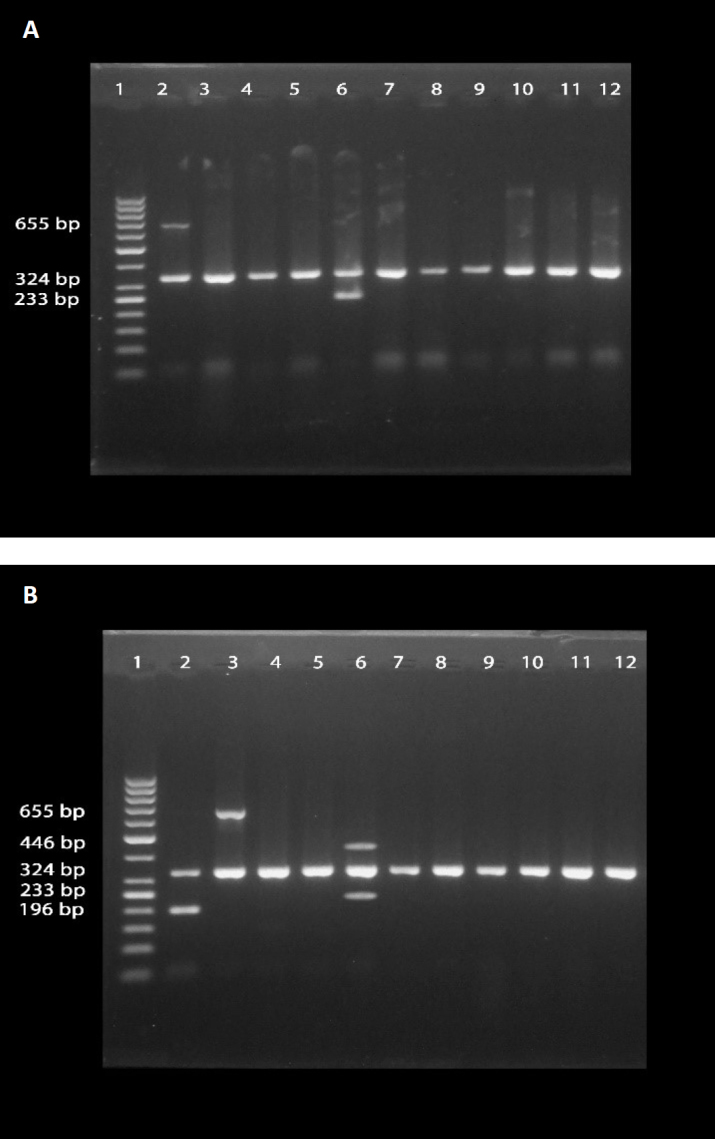
Agarose gel electrophoresis of multiplex PCR products of C. perfringens strains isolated from selected chicken meat products and a positive control
A) Lane 1 – 50bp DNA ladder. Lane 2 – C. perfringens type D (positive control). Lane 6 – C. perfringens type A, enterotoxin. Lanes 3, 4, 5, and 7 to 12 – C. perfringens type A
B) Lane 1 – 50bp DNA ladder. Lane 2 – C. perfringens type C (positive control). Lane 3 – C. perfringens type D. Lane 6 – C. perfringens type E, enterotoxin. Lanes 4, 5, and 7 to 12 – C. perfringens type A
Table 3.
Occurrence of C. perfringens enterotoxin in different toxin types
| C. perfringens enterotoxin type | ||||||
|---|---|---|---|---|---|---|
| Sample | A | D | E | |||
| Number | % | Number | % | Number | % | |
| Luncheon | 2(9) | 22 | 1(3) | 33 | 0(0) | 0 |
| Nuggets | 0(1) | 0 | 0(0) | 0 | 0(0) | 0 |
| Burger | 1(3) | 33 | 0(0) | 0 | 0(0) | 0 |
| Sausage | 3(11) | 27 | 1(4) | 25 | 1(1) | 100 |
| Total | 6 | 25 | 2 | 28 | 1 | 100 |
| P-value | 0.999 | 0.999 | 1.000 | |||
| 9 out of 32 (28%) | ||||||
Antibiotic sensitivity test
The occurrence of antibiotic resistance among 32 C. perfringens isolates was as follows: streptomycin (100%), lincomycin (100%), trimethoprim-sulfamethoxazole (94%), ciprofloxacin (41%), cefotaxime (34%), and rifampicin (31%). On the other hand, the isolates showed high sensitivity to amoxicillin (94%) and ampicillin (97%). Out of 32 C. perfringens isolates, the nine that harboured the enterotoxin gene, demonstrated a higher resistance to the antibiotics compared to non-enterotoxigenic isolates (Table 4).
Table 4.
Antibiogram of Clostridium perfringens strains isolated from processed chicken meat products
| Antimicrobials | Antibiotic profile | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Resistant | Sensitive | |||||||||||
| *a CPE+ | *b CPE- | Total | CPE+ | CPE- | Total | |||||||
| (9) | (23) | (32) | (9) | (23) | (32) | |||||||
| No. | % | No. | % | No. | % | No. | % | No. | % | No. | % | |
| Streptomycin | 9 | 100 | 23 | 100 | 32 | 100 | 0 | 0 | 0 | 0 | 0 | 0 |
| Lincomycin | 9 | 100 | 23 | 100 | 32 | 100 | 0 | 0 | 0 | 0 | 0 | 0 |
| Trimethoprim-sulfamethoxazole | 9 | 100 | 21 | 91 | 30 | 94 | 0 | 0 | 2 | 9 | 2 | 6 |
| Ciprofloxacin | 6 | 67 | 7 | 30 | 13 | 41 | 3 | 33 | 16 | 70 | 19 | 59 |
| Cefotaxime | 4 | 44 | 7 | 30 | 11 | 34 | 5 | 56 | 16 | 70 | 21 | 66 |
| Rifampicin | 5 | 56 | 5 | 22 | 10 | 31 | 4 | 44 | 18 | 78 | 22 | 69 |
| Amoxicillin | 1 | 11 | 1 | 4 | 2 | 6 | 8 | 89 | 22 | 96 | 30 | 94 |
| Ampicillin | 1 | 11 | 0 | 0 | 1 | 3 | 8 | 89 | 23 | 100 | 31 | 97> |
CPE+ – C. perfringens enterotoxin positive
CPE- – C. perfringens enterotoxin negative
Discussion
Food can be a source of different human ailments, therefore identification and control of food pathogens are a fundamental part of nourishment microbiology. C. perfringens was responsible for food poisoning in the 1940s; ever since, cases of food poisoning due to C. perfringens contamination have been reported (6).
According to our results, C. perfringens was isolated in 16% of 200 processed chicken meat samples collected from the Egyptian markets. This result is similar to that of Nasr et al. (23) who reported an isolation rate of 14.3%, while in another study, a high 37% prevalence was noted (20). In our study, the occurrence of C. perfringens may be possibly attributed to the method adapted in preparing chicken meat products. Moreover, the occurrence of C. perfringens may be ascribed to a high protein content in sampled products (13).
As shown in Table 2 and Figs 1A and 1B, C. perfringens type A was the most predominant type among C. perfringens isolates. The percentages of isolation of that type from luncheon, nuggets, burger, and sausage were 75, 100, 100, and 69, respectively. C. perfringens type D was isolated in 25%, 0%, 0%, and 25% of the cases, respectively. C. perfringens type E was only isolated from sausage samples, constituting 6% of isolates. These results are in accordance with results of Nasr et al. (23) who found that 70.8% of toxigenic isolates from processed chicken meat products proved to be C. perfringens type A, while 12.9% of the isolates belonged to type D.
A small percentage of C. perfringens produces the enterotoxin (CPE), which is responsible for food poisoning. CPE has been also associated with sporadic diarrhoea and in some cases with sudden infant death syndrome (5).
Table 3shows that out of 32 C. perfringens strains, six of enterotoxigenic strains belonged to type A, two to type D, and one to type E. This is similar to observations of Khan et al. (16) who toxinotyped six C. perfringens isolates from raw chicken meat and found that three of them were of type A and one each of the remaining three belonged to types B, C, and D. Likewise, the recognition of enterotoxin genes in type A isolates collected from raw and processed chicken meat products was reported by Guran and Oksuztepe (13). Moreover, the prevalence of C. perfringens exotoxin and enterotoxin was not related to the type of product (P > 0.05) (Tables 2 and 3). In fact, C. perfringens type A was isolated in almost all studies in which poultry meat was examined (24). Additionally, cpe gene was identified in C. perfringens isolates of all types (A-E), but type A was unusually common (18).
Interestingly, our results (Fig. 1B) provided some novel information about the isolation of C. perfringens enterotoxin type E from chicken sausage. This observation may account for several foodborne C. perfringens outbreaks that could be linked mainly to chromosomal cpe type A strains with heat-resistant spores, or occasionally less heat-resistant spore-forming plasmid cpe type A strains; both can be found in retail foods (21).
Furthermore, we examined the occurrence of resistance of 32 C. perfringens isolates to eight antibiotics which are widely used in poultry farms (Table 4). It was found that antibiotic sensitivity was highly related to the type of antibiotic used, either in C. perfringens enterotoxin-positive or -negative strains. The resistance to streptomycin, lincomycin, and trimethoprim-sulfamethoxazole was 100%, 100%, and 94% respectively, while appropriate percentages for ciprofloxacin, cefotaxime, and rifampicin were 41, 34, and 31, respectively. On the other hand, C. perfringens isolates showed high sensitivity to amoxicillin (94%) and ampicillin (97%).
These results are in agreement with those of Osman and Elhariri (26) who mentioned that C. perfringens isolates showed high resistance to streptomycin (100%), lincomycin (100%), and trimethoprim-sulfametho-xazole (98%). Furthermore, previously reported results (27, 2) showed intermediate sensitivity of C. perfringens to cefotaxime, ciprofloxacin, and low sensitivity to lincomycin. Abd-El Gwad and Abd El-Kader (1) demonstrated that C. perfringens isolates were highly sensitive to ampicillin, ciprofloxacin, and amoxicillin, which is consistent with our results suggesting that ampicillin and amoxicillin may be the drugs of choice for C. perfringens infection (3). Moreover, we found that C. perfringens isolates which carried enterotoxin gene showed a higher resistance to the antibiotics than non-enterotoxigenic isolates.
The frequent isolation of C. perfringens from processed chicken meat makes a public health risk. Its prevalence may be due to unhygienic measures not only during chicken rearing, but also during industrial processing. C. perfringens in poultry seems to occur very early and can be transmitted within the broiler chicken production, starting from the hatchery (10). Notably, C. perfringens is found in eggshell cracks, chicken fluff, and paper pads present in the hatchery (11).
Our study affirmed that there is a noticeable increase in the occurrence of enterotoxigenic C. perfringens in processed chicken meat, especially sausage. Moreover, we identificated C. perfringens enterotoxin type E in chicken meat. The study also contends that enterotoxigenic isolates of C. perfringens are more resistant to antibiotics than non-enterotoxigenic isolates.
Acknowledgements
We would like to express our deepest thanks to Dr. Elshaimaa Ismael, Faculty of Veterinary Medicine, Cairo University, Egypt, for her kind help in statistical analysis.
Footnotes
Conflict of Interests Statement: The authors declare that there is no conflict of interests regarding the publication of this article.
Financial Disclosure Statement: This work was not funded by any organisation.
Animal Rights Statement: None required.
References
- 1.Abd-El Gwad A.M., Abd El-Kader H.A.. The occurrence of Clostridium perfringens in the intestine of broiler chickens Assiut governorate. Ass Univ Bull Environ Res. 2001;4:13–22. [Google Scholar]
- 2.Abd El-Hamid H.S., Ellakany H.F., Aboelmagd B.A., Elbestawy A.R., Bedawy Sh.. Clinical and laboratory studies on chicken isolates of Clostridium perfringens in El-Behera, Egypt. J World's Poult Res. 2015;5:21–28. [Google Scholar]
- 3.Agunos A., Leger D., Carson C.. Review of antimicrobial therapy of selected bacterial diseases in broiler chickens in Canada. Can Vet J. 2012;53:1289–300. [PMC free article] [PubMed] [Google Scholar]
- 4.Ata N., Khairy E.A., Dorgham S.M., Zaki M.S.. Clostridium perfringens disease. Life Sci J. 2013;10:1599–1602. [Google Scholar]
- 5.Bos J., Smithee L., McClane B., Distefano R.F., Uzal F.. Fatal necrotizing colitis following a foodborne outbreak of enterotoxigenic Clostridium perfringens type A infection. Clin Infect Dis. 2005;40:78–83. doi: 10.1086/429829. [DOI] [PubMed] [Google Scholar]
- 6.Brynestad S., Granum P.E.. Clostridium perfringens and foodborne infections. Int J Food Microbiol. 2002;74:195–202. doi: 10.1016/s0168-1605(01)00680-8. [DOI] [PubMed] [Google Scholar]
- 7.Cakmak O., Ormanc F.S.D., Tayfur M., Erol I.. Presence and contamination level of Clostridium perfringens in raw frozen ground poultry and poultry burgers. Turk J Vet Anim Sci. 2006;30:101–105. [Google Scholar]
- 8.Villanova, USA: 2012. CLSI: Performance standards for antimicrobial susceptibility testing, Twenty-Fourth Informational supplement. M100-S24. [Google Scholar]
- 9.Collee J.G., Fraser A.G., Marmion B.P., Simmons A. Practical medical microbiology. 14th education. Churchill Living Stone, New York: 1996. [Google Scholar]
- 10.Craven S.E., Cox N.A., Bailey J.S., Cosby D.E.. Incidence and tracking of Clostridium perfringens through an integrated broiler chicken operation. Avian Dis 2003. 47:707–711. doi: 10.1637/6010. [DOI] [PubMed] [Google Scholar]
- 11.Craven S.E., Cox N.A., Stern N.J., Mauldin J.M.. Prevalence of Clostridium perfringens in commercial broiler hatcheries. Avian Dis. 2001;45:1050–1053. [PubMed] [Google Scholar]
- 12.Freedman C.J., Archana S., Bruce A., McClane B.A.. Clostridium perfringens enterotoxin: action, genetics, and translational applications. Toxins. 2016;8:73. doi: 10.3390/toxins8030073. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Guran H.S., Oksuztepe G.. Detection and typing of Clostridium perfringens from retail chicken meat parts. Lett Appl Microbiol. 2013;57:77–82. doi: 10.1111/lam.12088. [DOI] [PubMed] [Google Scholar]
- 14.Hamza D.A., Ghoneim N.H.. Epidemiological studies on Clostridium perfringens food poisoning, Scholar press. Omniscriptum Marketing DEU, Germany. 2015 doi: 10.20506/rst.36.3.2734. [DOI] [PubMed] [Google Scholar]
- 15.Hook D., Jalaludin B., Fitzsimmons G.. Clostridium perfringens food-borne-outbreak: an epidemiological investigation. Aust NZ J Public Health. 1996;20:119–122. doi: 10.1111/j.1753-6405.1996.tb01804.x. [DOI] [PubMed] [Google Scholar]
- 16.Khan M., Nazir J., Anjum A.A., Ahmad M.U., Nawaz M.. Toxinotyping and antimicrobial susceptibility of enterotoxigenic Clostridium perfringens isolates from mutton, beef and chicken meat. J Food Sci Technol. 2015;52:5323–5328. doi: 10.1007/s13197-014-1584-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Martel A., Devriese L.A., Cauwerts K., De-Gussem K., Decostere A.. Susceptibility of Clostridium perfringens isolates from broiler chickens to antibiotics and anti-coccidials. Avian Pathol. 2004;31:3–7. doi: 10.1080/0307945031000163291. [DOI] [PubMed] [Google Scholar]
- 18.McClane B.A. Doyle M.P., Beuchat L.R. Food Microbiology. ASM press; Washington: 2007. Clostridium perfringens; pp. 423–444. [Google Scholar]
- 19.Miki Y., Kaneko-Hirano I., Fujiuchi K., Akimoto S.. Prevalence and characterization of enterotoxin gene carrying Clostridium perfringens from retail meat products in Japan. Appl Environ Microbiol. 2008;74:5366–5372. doi: 10.1128/AEM.00783-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miwa N., Nishina T., Kubo S., Atsumi M, Honda H.. Amount of enterotoxigenic Clostridium perfringens in meat detected by nested PCR. Int J Food Microbiol. 1998;42:195–200. doi: 10.1016/s0168-1605(98)00082-8. [DOI] [PubMed] [Google Scholar]
- 21.Miyamoto K., Li J., McClane B.A.. Enterotoxigenic Clostridium perfringens: detection and identification. Microbes Environ. 2012;27:343–349. doi: 10.1264/jsme2.ME12002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Murray P.R., Baron E.J.O., Pfaller M.A.J., Orgensen J.H., Yolken R.H. Clostridium, Manual of Clinical Microbiology. Vol. 1. ASM Press; Washington: 2003. pp. 940–966. [Google Scholar]
- 23.Nasr E.M., Shehta A.A., Amer A.H.. Enterotoxigenicity and typing of Clostridium perfringens isolates from some poultry products in Egypt. J Appl Sci Res. 2007;3:1804–1808. [Google Scholar]
- 24.Nowell V.J., Poppe C., Parreira V.R., Jiang Y.F., Reid-Smith R.. Clostridium perfringens in retail chicken. Anaerobe. 2010;16:314–315. doi: 10.1016/j.anaerobe.2009.11.004. [DOI] [PubMed] [Google Scholar]
- 25.Okolocha E.C., Ellerbroek L.. The influence of acid and alkaline treatments on pathogens and the shelf life of poultry meat. Food Control. 2005;16:217–225. [Google Scholar]
- 26.Osman K.M., Elhariri M.. Antibiotic resistance of Clostridium perfringens isolates from broiler chickens in Egypt. Rev Sci Tech Off Int Epiz. 2013;32:841–850. doi: 10.20506/rst.32.2.2212. [DOI] [PubMed] [Google Scholar]
- 27.Silva R.O.S., Francisco C.F.J., Marcus V.R.M., Carlos A.O.J., Nelson R.M.. Genotyping and antimicrobial susceptibility of Clostridium perfringens isolated from Tinamidae, Cracidae and Ramphastidae species. Brazil Cienc Rural. 2014;44:486–491. [Google Scholar]
- 28.van Asten A.J., van der Wiel C.W., Nikolaou G., Houwers D.J., Grone A.A.. Multiplex PCR for toxin typing of C. perfringens. Vet Microbiol. 2009;136:411–412. doi: 10.1016/j.vetmic.2008.11.024. [DOI] [PubMed] [Google Scholar]
- 29.Voidarou C., Vassos D., Rozos G., Alexopoulos A., Plessas A.. Microbial challenges of poultry meat production. Anaerobe. 2011;17:341–343. doi: 10.1016/j.anaerobe.2011.05.018. [DOI] [PubMed] [Google Scholar]


