Introduction
Purple urine bag syndrome (PUBS) is a rare and disturbing situtation for patient's relative and the care team. It's mainly observed in long term bedridden with an indwelling urinary cathter use patients. PUBS is usually harmless and asymptomatic, but it may lead to severe conditions with a considerable morbidity and mortality.
Authors report a case occurring in a 78 years old male patient, describing clinical and evolutive features, and discussing physiopathology and managment of PUBS.
Case report
A 78 years old north african patient, with an history of hypertension, diabetes mellitus and a prostatic adenocarcinoma with vertebral metastasis, treated by triptorelin, consulted for a right back pain associated to a recent purple discoloration of the indwelling urine bag (Fig. 1). The patient was bedridden few weeks before hospitalization for a reduction of autonomy, with a permanent indwelling catheter. Temperature was at 38,5° Celsius. Conscience and hemodynamic state were stable. Acute pyelonephritis signs were concomittant to a purple discoloration of urine bag, three days before the emergency consult. Withe blood cells count was at 13500 elements/ml and platelet count at 220000 elements/ml. C-reactive protein was at 35 mg/l, and procalcitonin at 4 ng/ml. Abdominal ultrasound concluded to a densification of the peri-renal and pelviureteric fat. There weren't obstructive signs on the upper urinary tract or peri-renal collection in ultrasound. The patient got a probabilist antibiotherapy after bacteriological sampling of urine: cefotaxim 2 g, three times a day, and gentamycin 240 mg once a day. The indwelling catheter was changed, and the purple coloration disappeared. The urine were turbid in the bag. The indwelling Urine culture concluded to an Escherichia Coli, the count was at 15 5 elements/ml, the sensitivity to β-lactam and aminoglycoside antibiotics was confirmed in the antibiogram. A sediment appeared in the urine tube few minutes after bacteriological sampling. A semi-quantitative spectophotometric analysis of the sediment was performed. Ammonuim urate acide and struvite were detected (Fig. 2).
Fig. 1.
Purple discoloration of urine bag.
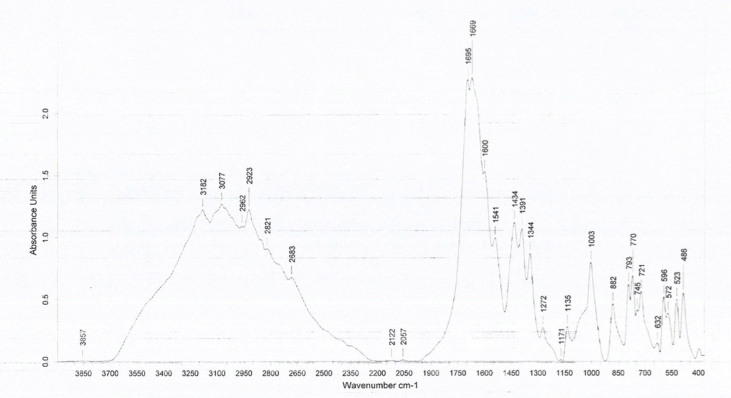
Fig. 2.
Spectrophotometry: presence of ammomuim urate acid and struvite.
Evolution was favourable during hospitalization. Back pain and fever disappeared in two days. Urine culture, after three days on treatment, was negative. The patient was discharged in the fifth day, he had cefixim for two weeks. Physical exmination in the outpatient clinic was normal. Ultrasonographic abnormalities disappeared a month later.
Discussion
PUBS is a rarely reported situation, that's mostly seen in long term nursing institutions.
The oldest historical description of PUBS dates back to 1812. The first medical description of PUBS was 1978, by Barlow and Dickson.1
The prevalence of PUBS is variable, depending on patients population and bacterial epidemiology. It has been evaluated around 10–15% of patients with long term indwelling catheter. It's important to metion that the urine itself isn't discolored. Urine bacteriological sampling is usually dark brown and turpid. The purple aspect concern urine contained in the catheter and its collecting bag.2
This discoloration is related to the combination of two pigments, indigo and indirubine, providing from the metabolism of tryptophan. Production of the pigments arises from the action of an enzyme, the indoxyl sulphatase, procuced by a spectrum of bacteria like Escherichia Coli and Klebsiella Pneumoniae, upon the indowyl sulphate. Pigments adhere to the catheter and the bag, and urine is discolored from red to blue to become purple. Urine may be differently discolored between the catheter and the urine bag.3
PUBS itself is not a severity sign, but it reflects bacteriuria. In some cases, PUBS may be associated to severe and life-threatening conditions related to comorbidities and long-term bed rest.
The same phenomenon may be observed in infants, known as Drummond Syndrom, or the blue diaper syndrom. It's secondary to a disorder in tryptophan intestinal absortion, wich is eliminated and metabolised in urine, causing it's discoloration.3
Risk factors are female gender, dementia, chronic constipation, chronic renal disease, alcaline urine, increased urine bacterial load and the use of polyvinyl chloride unrine bags. PUBS is observed in permanent urinary catheterization, either urethral or supra-pubic.2
Dementia is the most related to recurrence of PUBS. Female gneder exposes to PUBS as the urethra is shorter, closer to the anus and more exposed to bacterial infections than in men. Intestinal hypo-motility in chronic constipated patients leads to bacterial overgrowth with an increase in tryptophan metabolism. PUBS is more reported in chronic kidney disease, as indoxyl sulphate is bound to albumin with a limited removal during dialysis and an increase of its serum concentration. Alcaline urine facilitate pigments precipitation in the synthetic materials of the urine catheter and bag, even though some reports described PUBS in acidic urines.2
Spectrophotometry was performed only in the case reported by Ficher et al. They found indigo pigment in the urine sediment.4 Antibiotherapy is not systematic once PUBS is observed, it depends on the presence of septic signs. PUBS may disappear once the indwelling cathteter is changed. Intensive antibiotherapy is necessary once PUBS is associated to a severe urinary infection. In some reports, PUBS was associated to a scrotal gangrene and to a septic shock, justifying a thourough follow-up once PUBS is diagnosed.4,5
There aren't consensual guidelines about PUBS. It's managed on a case-by-case basis. An early diagnosis and managment avoids invasive explorations without particular findings, such as cystoscopy. Prevention include appropriate indications of urine drainage, and avoidance of unecessary ones, the catheter care, the use of silver impregnated Foley catheter, that recude bacterial culture and growth, and therefore PUBS. Constipation treatment may also reduce the incidence and the reccurence of PUBS in risk population.
Conclusion
Despite its benign appearance and physiopathologie, PUBS is still a disturbing little-known condition for health-care team and patient's relatives. A knowledge of risk factors and metabolic mechanisms is required by geriatricians, urologists and emergency doctors in order to plan an adequate management. Association to comorbodities may lead PUBS to a life-threatening septic condition, justifying a watchful surveillance. Once prevented and correctly managed, PUBS is usually resolutive uneventfully.
References
- 1.Barlow G., Dickson J. Purple urine bags. Lancet. 1978;28:220–221. [Google Scholar]
- 2.Peters P., Merlo J., Beech N. The purple urine bag syndrome: a visually striking side effect of highly alkaline urinary tract infection. Can Urol assoc J. 2011;5:233. doi: 10.5489/cuaj.10177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Gautam G., Kothari A., Kumar R., Dogra P.N. Purple urine bag syndrome: a rare clinical entity in patients with long term ind- welling catheters. Int Urol Nephrol. 2007;39:155–156. doi: 10.1007/s11255-006-6667-2. [DOI] [PubMed] [Google Scholar]
- 4.Ficher K., Araújo A., Houly S., Lins P., Silva M., Jr., Góis A. Purple urine bag syndrome: case report for Streptoccocus agalactiae and literature review. J. Bras. Nefrol. 2016;38(4) doi: 10.5935/0101-2800.20160075. [DOI] [PubMed] [Google Scholar]
- 5.Tasi Y.M., Huang M.S., Yang C.J., Yeh S.M., Liu C.C. Purple urine bag syndrome, not always a benign process. Am J Emerg Med. 2009;27(7):895–897. doi: 10.1016/j.ajem.2009.01.030. [DOI] [PubMed] [Google Scholar]