Abstract
Introduction
Radial meniscus tears are seen in young patients, especially with anterior cruciate ligament ruptures. Repair of complete radial meniscus tear is necessary for the meniscus functions. The most important factor for success of the meniscus repair is primary stability, but it is still unknown which technique is ideal repair technique.
Aim
We developed a new suture technique named Horizontal Butterfly (HB). In this novel technique the contact between meniscal tissue and suture is more than Horizontal Loop (HL) that routinely used today. So, we think that this technique will provide better fixation than HL. We aimed to compare 2 repair techniques (HB vs. HL) using human lateral menisci biomechanically with cyclic loading and load to failure tests.
Material-method
We used 22 intact lateral meniscus obtained from patients that operated (total knee replacement) for varus gonarthrosis in our clinic. All menisci were cut radially. In the first group (n:11) menisci were repaired with standard horizontal loop technique, and in the second group (n:11) horizontal butterfly technique were used for repair. All specimens were tested with load to failure test after cyclic loading test (500 cycle X 5–30 N).
Results
Both groups have similar failure load (71,4 ± 17,52 N vs. 77,9 ± 28,49 N; p:0,559) and stiffness (24,46 ± 19,19 N vs. 24,48 ± 15,87 N; p:0,818). HB group has less peak displacement (6,26 ± 1,24 mm vs. 8,4 ± 1,92 mm; p:0,010).
Conclusion
This novel repair technique decreases the amount of displacement according to standard technique while as strong as standard technique routinely used. In this way; we believe that it will increase the rate of healing in clinical use.
Keywords: Radial meniscus tear, Repair techniques, Horizontal butterfly, Cyclic loading, Horizontal loop, Meniscus surgery
Introduction
Meniscus tears that require treatment constitute an important part of the sports surgery nowadays. Menisci are known to have many functions such as load distribution, lubrication, joint stability and proprioception.1, 2, 3, 4, 5, 6, 7 In many clinical trials, it has been shown that degenerative process in the knee joint is accelerated after meniscectomy, resulting in arthrosis. Radial meniscus tears are usually seen as a result of a trauma in younger patients and often coexist with other injuries such as anterior cruciate ligament rupture.8 Radial tears extending to the periphery of the meniscus have been shown to be equivalent to total meniscectomy because they reduce the meniscal tensile force.9
It is now a well-known and accepted reality that preserving the meniscus tissue, or repairing it if possible, slows down this degenerative process.10, 11, 12, 13, 14, 15, 16 A number of case series have been published on radial meniscus repair techniques. Positive results have been reported in repairs made with single or double horizontal sutures using the inside-out, outside-in or all-inside techniques.17 The horizontal loop technique is often used during the repair of radial tears.18, 19, 20, 21 Modifications such as cross-configurations have been investigated to increase initial stability. The transosseous repair technique, which is applied by opening the tibial tunnel, was also described.12
Our hypothesis is that we will be able to obtain less displacement and similar failure force with the new suture configuration we have designed -horizontal butterfly (HB)- than the horizontal loop (HL) suture technique used routinely, because of the increased contact between the sutures and the meniscus tissue.
Material and method
The study was approved by the Ethics Committee for Clinical Investigations (13-KAEK-208). A total of 22 intact and almost the same sized lateral menisci were obtained from patients who underwent total knee arthroplasty due to varus gonarthrosis in our clinic between 2010 and 2013. Menisci with macroscopic findings such as tear, fibrillation, degeneration or fragmentation were not included in the study. The menisci to be included in the study were stored in the −80° refrigerator until the day of the experiment. On the day of experiment, all menisci were kept in %0.9 saline solution for 6 h at room temperature and made ready for processing. A radial incision was made with a No. 10 scalpel on the corpus of meniscus and a radial tear extending to periphery of meniscus was created.
Suture technique
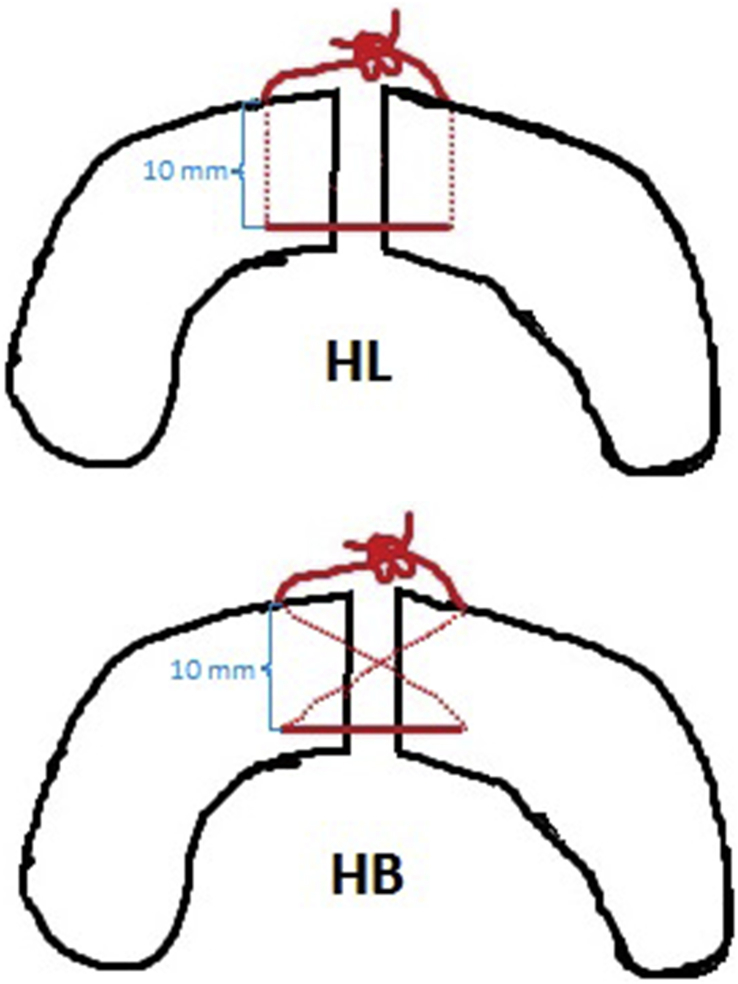
All menisci were repaired by an experienced orthopedic surgeon (TG) using a straight needle and the same suture material (No. 0 PDS, Ethicon Inc, Johnson & Johnson, Somerville, New Jersey). In the first group (HL group, n = 11), the standard horizontal loop technique was applied for repair. For this, the suture was passed with a distance of 5 mm from the tear edge, 10 mm inside the perimeter of the meniscus, using a straight needle. In the other group (HB group, n = 11), the horizontal butterfly technique was applied for repair. For this, the entry sites on the meniscus of the sutures in the first group were planned in the same way. The suture was tied by orienting the direction of the needle toward the periphery of the opposite fragment with an angle of about 45°, not towards the periphery of the meniscus, so that the suture was cross-configured within the meniscus tissue. In both groups, the suture ends were manually tied with 1 complet knot and 4 half-knots in the periphery of meniscus (Fig. 1).
Fig. 1.
Schematic drawings of HL (horizontal loop) and HB (horizontal butterfly) suture techniques.
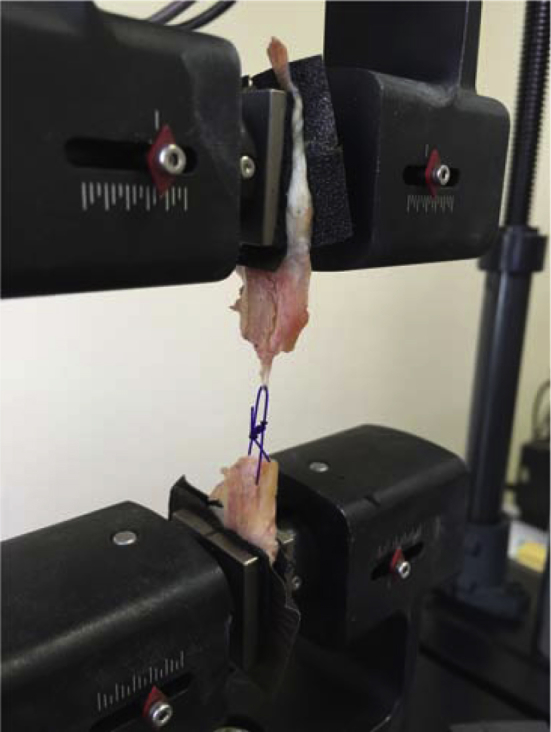
Cyclic loading test
All menisci were clamped to the biomechanical tester (MTS Acumen Electrodynamic Test System, USA). In order to prevent the menisci from slippage off the clamps, a 3 × 3 cm no. 0 sanding paper was placed between each meniscus and the clamp (Fig. 2). The tests were performed at room temperature. All menisci were subjected to 500 cyclic load tests at a speed of 1 Hz and a load range of 5–30 N, as described in previous studies.17, 22
Fig. 2.

Placement of the repaired meniscus on the biomechanical tester.
Load to failure test
All repaired menisci were subjected to a load to failure test immediately after the cyclic loading test. The force(N) and the amount of displacement (mm) were recorded by the computer during the test. Stiffness was automatically calculated by the biomechanical tester. The type of failure was visually identified.
Statistical analysis
Statistical software was used in the calculations (IBM SPSS Statistics 19, SPSS Inc., An IBM Co., Somers, NY). Values of the variables were given as mean ± standard deviation. Inter-group averages were compared using the Independent Samples t-test or the Mann–Whitney U Test. p values less than 0.05 were considered statistically significant.
Results
At the end of the cyclic loading test, there was a visible gap in the repair area in both groups. When these displacement amounts were compared, it was seen that there was less displacement in the HB group (6.26 ± 1.24 vs. 8.4 ± 1.92, p = 0.010), and this difference was statistically significant. Two repaired menisci from the HB group failed to complete the test due to the rupture of the suture during cyclic loading.
In the load to failure test, in both groups, all the specimens were observed to have failure in the form of peeling of the suture from the meniscus (Fig. 3). The HB group had less failure strength than the HL group (71.4 ± 17.52 vs. 77.9 ± 28.49, p = 0.559). However, this difference was not statistically significant. The stiffness of both groups was similar (24.46 ± 19.19 vs. 24.48 ± 15.87, p = 0.818) (Table 1).
Fig. 3.
The peeling of the suture from the meniscus after the failure test.
Table 1.
Distribution of radial tears by groups.
| Groups |
t/Z | p | ||||
|---|---|---|---|---|---|---|
| Horizontal Butterfly |
Horizontal Loop |
|||||
| n | Mean ± SD | n | Mean ± SD | |||
| Peak Displacement (mm) | 9 | 6,26 ± 1,24 | 11 | 8,4 ± 1,92 | 2880 | 0,010* |
| Static Peak Force (N) | 9 | 71,4 ± 17,52 | 11 | 77,9 ± 28,49 | 0,596 | 0559* |
| Stiffness (N/mm) | 6 | 24,46 ± 19,19 | 6 | 24,48 ± 15,87 | 0,320 | 0818 |
p < 0,05 is level of significance, *Independent Samples t-test.
Bold indicates the difference of peak displacement was significantly lesser in Horizontal Butterfly group.
Discussion
Smaller amount of displacement in the HB group -supporting our hypothesis-was achieved. This finding suggests that the described suture configuration provides more stiff repair. Our hypothesis was based on the claim that the HB suture technique would be more stable and stiff, and we listed our reasons, advantages and disadvantages for that. Statistically significant difference was not found between the failure strengths as a result of the biomechanical tests.
Most of the radial meniscus tears are seen on the meniscus body.23 It is important to preserve or restore the anatomical integrity of meniscus in order to maintain its functionality. In the study of Bedi et al,24 radial meniscus repair with the double horizontal suture technique on fresh cadaver's knees has been reported to reduce the contact pressure significantly compared to the partial meniscectomy group without causing significant changes in the medial compartment contact area. It is known that radial meniscus tears can be healed after repair and the mechanical properties of meniscus can be restored.16, 18, 19, 20, 21 Most of the studies on radial meniscus repairs in the literature are in the form of case series. The number of biomechanical studies is relatively small18, 19, 20, 22, 25, 26 and most of these biomechanical studies have been published more recently than the case series.
Ode et al27 compared 6 different models in fresh frozen cadaver knees. They found an increase in the joint surface contact area and decrease in the surface pressure after repair performed in full-thickness radial tears. It is obvious that this biomechanical effect should be reversed considering the relationship between these changes, which will develop in knee kinematics as the equivalent of meniscectomy, and early arthrosis.28, 29, 30
When designing the horizontal butterfly technique, two features were proposed: The first would provide more compression between the ends of the tear because when the suture is tied, the direction of the parts that are diagonal would be approximately 45° to the tear surface (90° in the standard horizontal loop technique). This can provide a better protection during the post-op rehabilitation period by increasing the primary stability. Another possible advantage is that the contact and frictional force between the suture and the meniscus tissue would be greater, since each piece of the suture in the meniscus tissue would cover a greater distance (Fig. 1) (while it is about 10 + 10 = 20 mm in HL, this value is about 14.14 + 14.14 = 28.28 mm in HB). This can increase the stability of the repair.
The possible disadvantage is that the loads applied to the tear area would be longitudinal on the meniscus. Because it would be less angled with respect to the pulling direction of the cross-suture pieces in HB (about 45°), it could cause the suture to cut the meniscus tissue and prematurely peel.
Herbort et al22 carried out a biomechanical study on the lateral menisci they obtained from 55 fresh frozen porcine knees. They compared double horizontal sutures and single sutures placed near the periphery of the meniscus in the 5 different groups with suture patterns that have different widths and depths at the medio-lateral distance. In this study, there were results showing that the double horizontal sutures were significantly stronger in biomechanical tests. It is seen that this study takes into account many factors, considering the fact that it also assesses the effects of suture width and its location at the medio-lateral meniscus distance, evaluates 5 different patterns, and the sufficient number of specimens in each group. It is clear that the biomechanical superiority of the double horizontal suture is significant in terms of providing a powerful alternative to meniscectomy especially in young age with radial full-thickness tears. It can be seen as a limitation that the biomechanical superiority of the double horizontal loop technique was ignored in our study. We wanted to make this assessment by comparing the single cross suture and the single horizontal suture because of the limited number of our specimen. Our aim was to compare the suture configurations, and we found that there was less displacement with a statistically significant difference during cyclic loading. We think that stabilization can be increased by increasing the number of sutures placed in clinical use.
In the biomechanical study of Branch et al31 comparing 4 different suture configurations performed on cadaver knees, it was found that double-sutured repairs made using the all-inside technique were stronger than those made using the inside-out technique. In addition, it has been reported that the cross-suture configuration has the highest failure strength. The results of this study, which very effectively simulates the clinical applications that we perform in radial tears today, demonstrate the superiority of the cross-suture configuration in a similar way to our study. Cross-configured sutures have the greatest failure strength, which promotes the clinical use of these sutures. In our study, the single suture configurations were compared and found to be more stable than the standard horizontal loop suture.
Matsubara et al17 thought that oblique sutures, which are tied by taking into account the orientation of the collagen fibers of the meniscus, would provide a more stable fixation. As a result, the failure strength and stiffness were significantly higher, and the amount of displacement was significantly lower in the cross-sutured group, which confirmed their hypotheses.
Although biomechanical time-zero studies do not meet in-vivo conditions, it is a fact that the most important factor in the success of meniscal repair is the primary stability. For this reason, various suture configurations have been described to increase primary stability, and to prevent suture breakage and peeling of suture from the tissue. When designing the HB suture configuration we described, we considered the suture-tissue contact, the compression in the tear line, the orientation of the collagen fibrils, and the orientation of the suture with these collagen fibers.17, 32
Also in support of the possible advantages described at the beginning of the article, the HB suture must have caused more compressive force on the ends of the tear, which resulted in less displacement compared to the HL group. It is possible that an increase in the frictional force due to the greater contact between the meniscus tissue and the suture material is also effective in reducing the displacement amount.
An attempt was made using the cyclic loading test to imitate the loads applied to menisci which were repaired in vivo. As described in previous publications, 500 cycles were repeatedly applied in the range of 5–30 N. This force simulates the exercises performed during the post-operative rehabilitation period.17, 22, 31
One of the limited aspects of our study is the use of lateral menisci of patients who operated with total knee arthroplasty due to gonarthrosis. However, when choosing the menisci, we paid attention to collect specimen from the patients who had no arthrosis in the lateral compartment and whose menisci were intact. There are also studies with porcine menisci in the literature. However, we think that porcine menisci cannot mimic human menisci because of its small size and increased thickness compared to human menisci. Besides that, by using our specific specimen collection technique, as stated in the study of Matsubara et al,17 fresh human menisci can be used in such experiments.
Another limitation may be the suture material used. No. 0 PDS suture is a preferred suture for meniscal repair in routine clinical use. The disadvantage of this suture is that it can exhibit more stretching than other polyethylene or polyester derived sutures due to its flexible structure. We think that the displacement amounts obtained as a result of the test may also be caused by this suture material. Another limitation is that clinical arthroscopic application of the HB suture configuration we described may be difficult. However, we think that it can be done with some patience by experienced hands with the outside-in and inside-out methods. And one more limitation is no data about menisci's histological integrity. As all the menisci obtained from arthrosic knees, each meniscus could present with different internal integrity. Histological investigation of each menisci was not performed. So we can not say anything about the homogeneity or heterogeneity of the meniscal integrity.
One of the strongest aspects of our study is that we performed the cyclic load test and did the load to failure test afterwards. Exercises performed during the rehabilitation period were simulated with the cyclic loading test.
It is obvious that the use of augmented techniques is necessary in repairs to be performed especially in avascular zones, as the promising result of our study, in which we evaluated the repair technique only biomechanically, will not guarantee its in vivo efficacy.
Conclusion
Findings in our study show that the HB suture technique is as strong as the HL sutures used in the routine. In addition to that, this technique reduces the amount of displacement. Although not supported by adequate clinical findings, this technique can be an alternative method for arthroscopic repair of radial tears.
Conflict of interest
The authors declared no conflict of interest.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
Contributor Information
Murat Aşçi, Email: muratasci55@gmail.com.
Orhan Balta, Email: drorhanbalta@hotmail.com.
Recep Kurnaz, Email: recepkurnaz@gmail.com.
Mehmet Burtaç Eren, Email: mehmetburtac@hotmail.com.
Yunus Emre Kuyucu, Email: yunusemre.kuyucu@gop.edu.tr.
Taner Güneş, Email: drtgunes@gmail.com.
References
- 1.Allen C.R., Wong E.K., Livesay G.A., Sakane M., Fu F.H., Woo S.L. Importance of the medial meniscus in the anterior cruciate ligament-deficient knee. J Orthop Res. 2000 Jan;18(1):109–115. doi: 10.1002/jor.1100180116. [DOI] [PubMed] [Google Scholar]
- 2.Allen P.R., Denham R.A., Swan A.V. Late degenerative changes after meniscectomy. Factors affecting the knee after operation. J Bone Joint Surg Br. 1984 Nov;66(5):666–671. doi: 10.1302/0301-620X.66B5.6548755. [DOI] [PubMed] [Google Scholar]
- 3.Krause W.R., Pope M.H., Johnson R.J., Wilder D.G. Mechanical changes in the knee after meniscectomy. J Bone Joint Surg Am. 1976 Jul;58(5):599–604. [PubMed] [Google Scholar]
- 4.McDermott I.D., Amis A.A. The consequences of meniscectomy. J Bone Joint Surg Br. 2006 Dec;88(12):1549–1556. doi: 10.1302/0301-620X.88B12.18140. [DOI] [PubMed] [Google Scholar]
- 5.Meakin J.R., Shrive N.G., Frank C.B., Hart D.A. Finite element analysis of the meniscus: the influence of geometry and material properties on its behaviour. Knee. 2003 Mar;10(1):33–41. doi: 10.1016/s0968-0160(02)00106-0. [DOI] [PubMed] [Google Scholar]
- 6.Amendola A., Bonasia D.E. The menisci: anatomy, healing response, and biomechanics. Knee Joint. 2012:5–9. [Google Scholar]
- 7.Seedhom B.B., Dowson D., Wright V. Proceedings: functions of the menisci. A preliminary study. Ann Rheum Dis. 1974 Jan;33(1):111. doi: 10.1136/ard.33.1.111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bin S.I., Kim J.M., Shin S.J. Radial tears of the posterior horn of the medial meniscus. Arthroscopy. 2004 Apr;20(4):373–378. doi: 10.1016/j.arthro.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 9.Messner K., Gao J. The menisci of the knee joint. Anatomical and functional characteristics, and a rationale for clinical treatment. J Anat. 1998 Aug;193(2):161–178. doi: 10.1046/j.1469-7580.1998.19320161.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Harper K.W., Helms C.A., Lambert H.S., Higgins L.D. Radial meniscal tears: significance, incidence, and MR appearance. AJR J Roentgenol. 2005 Dec;185(6):1429–1434. doi: 10.2214/AJR.04.1024. [DOI] [PubMed] [Google Scholar]
- 11.Kidron A., Thein R. Radial tears associated with cleavage tears of the medial meniscus in athletes. Arthroscopy. 2002 Mar;18(3):254–256. doi: 10.1053/jars.2002.30650. [DOI] [PubMed] [Google Scholar]
- 12.Kim Y.M., Rhee K.J., Lee J.K., Hwang D.S., Yang J.Y., Kim S.J. Arthroscopic pullout repair of a complete radial tear of the tibial attachment site of the medial meniscus posterior horn. Arthroscopy. 2006 Jul;22(7) doi: 10.1016/j.arthro.2005.12.040. 795.e1–e4. [DOI] [PubMed] [Google Scholar]
- 13.Smith J.P., Barrett G.R. Medial and lateral meniscal tear patterns in anterior cruciate ligament-deficient knees. A prospective analysis of 575 tears. Am J Sport Med. 2001 Jul–Aug;29(4):415–419. doi: 10.1177/03635465010290040501. [DOI] [PubMed] [Google Scholar]
- 14.Tao S.S., Beach W.R. Use of a Caspari suture punch to repair a radial tear of the lateral meniscus. Arthroscopy. 2002 Feb;18(2):206–210. doi: 10.1053/jars.2002.26858. [DOI] [PubMed] [Google Scholar]
- 15.Voloshin A.S., Wosk J. Shock absorption of meniscectomized and painful knees: a comparative in vivo study. J Biomed Eng. 1983 Apr;5(2):157–161. doi: 10.1016/0141-5425(83)90036-5. [DOI] [PubMed] [Google Scholar]
- 16.Yoo J.C., Ahn J.H., Lee S.H., Lee S.H., Kim J.H. Suturing complete radial tears of the lateral meniscus. Arthroscopy. 2007 Nov;23(11) doi: 10.1016/j.arthro.2006.07.056. 1249.e1–e7. [DOI] [PubMed] [Google Scholar]
- 17.Matsubara H., Okazaki K., Izawa T., Tashiro Y., Matsuda S., Nishimura T. New suture method for radial tears of the meniscus: biomechanical analysis of cross-suture and double horizontal suture techniques using cyclic load testing. Am J Sport Med. 2012 Feb;40(2):414–418. doi: 10.1177/0363546511424395. [DOI] [PubMed] [Google Scholar]
- 18.Choi N.H., Kim T.H., Son K.M., Victoroff B.N. Meniscal repair for radial tears of the midbody of the lateral meniscus. Am J Sport Med. 2010 Dec;38(12):2472–2476. doi: 10.1177/0363546510376736. [DOI] [PubMed] [Google Scholar]
- 19.Haklar U., Kocaoglu B., Nalbanoglu U., Tuzuner T., Guven O. Arthroscopic repair of radial lateral menicus tear by double horizontal sutures with inside–outside technique. Knee. 2008 Oct;15(5):355–359. doi: 10.1016/j.knee.2008.05.012. [DOI] [PubMed] [Google Scholar]
- 20.van Trommel M.F., Simonian P.T., Potter H., Wickiewicz T.L. Arthroscopic meniscal repair with fibrin clot of complete radial tears of the lateral meniscus in the avascular zone. Arthroscopy. 1998 May–Jun;14(4):360–365. doi: 10.1016/s0749-8063(98)70002-7. [DOI] [PubMed] [Google Scholar]
- 21.Ra H.J., Ha J.K., Jang S.H., Lee D.W., Kim J.G. Arthroscopic inside-out repair of complete radial tears of the meniscus with a fibrin clot. Knee Surg Sports Traumatol Arthrosc. 2013 Sep;21(9):2126–2130. doi: 10.1007/s00167-012-2191-3. [DOI] [PubMed] [Google Scholar]
- 22.Herbort M., Siam S., Lenschow S., Petersen W., Zantop T. Strategies for repair of radial tears close to the meniscal rim-biomechanical analysis with a cyclic loading protocol. Am J Sport Med. 2010 Nov;38(11):2281–2287. doi: 10.1177/0363546510382847. [DOI] [PubMed] [Google Scholar]
- 23.Noyes F.R., Barber-Westin S.D. Arthroscopic repair of meniscal tears extending into the avascular zone in patients younger than twenty years of age. Am J Sport Med. 2002 Jul–Aug;30(4):589–600. doi: 10.1177/03635465020300042001. [DOI] [PubMed] [Google Scholar]
- 24.Bedi A., Kelly N.H., Baad M., Fox A.J., Brophy R.H., Warren R.F. Dynamic contact mechanics of the medial meniscus as a function of radial tear, repair, and partial meniscectomy. J Bone Joint Surg Am. 2010 Jun;92(6):1398–1408. doi: 10.2106/JBJS.I.00539. [DOI] [PubMed] [Google Scholar]
- 25.Noyes F.R., Barber-Westin S.D. Arthroscopic repair of meniscus tears extending into the avascular zone with or without anterior cruciate ligament reconstruction in patients 40 years of age and older. Arthroscopy. 2000 Nov;16(8):822–829. doi: 10.1053/jars.2000.19434. [DOI] [PubMed] [Google Scholar]
- 26.Magee T., Shapiro M., Williams D. MR accuracy and arthroscopic incidence of meniscal radial tears. Skeletal Radiol. 2002 Dec;31(12):686–689. doi: 10.1007/s00256-002-0579-8. [DOI] [PubMed] [Google Scholar]
- 27.Ode G.E., Van Thiel G.S., McArthur S.A., Dishkin-Paset J., Leurgans S.E., Shewman E.F. Effects of serial sectioning and repair of radial tears in the lateral meniscus. Am J Sport Med. 2012 Aug;40(8):1863–1870. doi: 10.1177/0363546512453291. [DOI] [PubMed] [Google Scholar]
- 28.Rangger C., Kathrein A., Klestil T., Glötzer W. Partial meniscectomy and osteoarthritis. Sports Med. 1997 Jan;23(1):61–68. doi: 10.2165/00007256-199723010-00006. [DOI] [PubMed] [Google Scholar]
- 29.Knights C.B., Gentry C., Bevan S. Partial medial meniscectomy produces osteoarthritis pain-related behaviour in female C57BL/6 mice. Pain. 2012 Feb;153(2):281–292. doi: 10.1016/j.pain.2011.09.007. [DOI] [PubMed] [Google Scholar]
- 30.Roos H., Lauren M., Adalberth T., Roos E.M., Jonsson K., Lohmander L.S. Knee osteoarthritis after meniscectomy: prevalence of radiographic changes after twenty-one years, compared with matched controls. Arthritis Rheum. 1998 Apr;41(4):687–693. doi: 10.1002/1529-0131(199804)41:4<687::AID-ART16>3.0.CO;2-2. [DOI] [PubMed] [Google Scholar]
- 31.Branch E.A., Milchteim C., Aspey B.S., Liu W., Saliman J.D., Anz A.W. Biomechanical comparison of arthroscopic repair constructs for radial tears of the meniscus. Am J Sport Med. 2015 Sep;43(9):2270–2276. doi: 10.1177/0363546515591994. [DOI] [PubMed] [Google Scholar]
- 32.Petersen W., Tillmann B. Collagenous fibril texture of the human knee joint menisci. Anat Embryol (Berl) 1998 Apr;197(4):317–324. doi: 10.1007/s004290050141. [DOI] [PubMed] [Google Scholar]