Abstract
The mortality rate in patients suffering from non-small cell lung cancer (NSCLC) is quite high. This type of cancer mainly occurs due to rearrangements in the anaplastic lymphoma kinase (ALK) gene which leads to form an oncogene of fused gene NPM-ALK. Brigatinib is recently approved by FDA in April 2017 as a potent tyrosine kinase inhibitor (TKI) for the NSCLC therapy. In the present scenario, it is no less than a wonder drug because it is indicated for the treatment of advanced stages of metastatic ALK positive NSCLC, a fatal disease to overcome the resistance of various other ALK inhibitors such as crizotinib, ceritinib and alectinib. In addition to ALK, it is also active against multiple types of kinases such as ROS1, Insulin like growth factor-1Receptor and EGFR. It can be synthesized by using N-[2-methoxy-4-[4-(dimethylamino) piperidin-1-yl] aniline] guanidine and 2,4,5-trichloropyrimidine respectively in two different ways. Its structure consists of mainly dimethylphosphine oxide group which is responsible for its pharmacological activity. It is active against various cell lines such as HCC78, H2228, H23, H358, H838, U937, HepG2 and Karpas- 299. Results of ALTA (ALK in Lung Cancer Trial of AP26113) phase ½ trial shows that 90 mg of brigatinib for 7 days and then 180 mg for next days is effective in the treatment of NSCLC. Brigatinib has been shown to have favorable risk benefit profile and is a safer drug than the available cytotoxic chemotherapeutic agents. In comparison to other FDA approved drugs for the same condition, it causes fewer minor adverse reactions which can be easily managed either by changing the dose or by providing good supportive care. This article is intended to provide readers with an overview of chemistry, pharmacokinetic, pharmacodynamic and safety profile of brigatinib, which addresses an unmet medical need.
Keywords: ALK inhibitors, Brigatinib, Lung cancer, Kinase, Lymphoma
Abbreviations: NPM, nucleophosmin; ALK, anaplastic lymphoma kinase; NSCLC, non-small cell lung cancer; EGFR, epidermal growth factor receptor; EML4, echinoderm microtubule associated protein; TKI’s, tyrosine kinase inhibitors; P-gp, P-glycoprotein; BCRP, breast cancer resistance protein; ORR, objective response rate; ALTA-1L, ALK in lung cancer trial of Brigatinib in1st Line; DMPO, dimethyl phosphine oxide; SAR, structure activity relationship; MIC, minimum inhibitory concentration; ALCL, anaplastic extensive cell lymphoma; FLT3, fem like tyrosine kinase-3; FDA, Food and Drug Administration; LCC, Large Cell Carcinoma
1. Introduction
Lung cancer is one of the deadliest forms of cancer. It is associated with high death rate accounting alone for 1/5th of total cancer mortality worldwide (Chan and Hughes, 2015). It has a very poor survival rate and prognosis, as more than half of the diagnosed patients die within one year of diagnosis. Lung cancer is subdivided into two types; Small cell lung carcinoma (SLCC) and Non-small cell lung cancer (NSCLC). NSCLC is the most common kind of lung cancer which is associated with an increase in production of epithelial lung cells and accounts approximately for 85–90% of all lung cancer cases (Sher et al., 2008).
The most widely recognized subtypes of NSCLC are pulmonary adeno-carcinoma, squamous cell carcinoma (SCC) and large cell carcinoma (LCC) (West et al., 2012). Glandular cancer (pneumonic glandular cancer) or adeno-carcinoma is a typical microscopical type in which there are alterations in tissue cell and sub-atomic structures and components, together with organ and channel development as well as the creation of noteworthy measures of bodily fluid (Travis et al., 2010). It comprises of around 40% of all lung cancers and is diagnosed in both genders whether smokers or non-smokers. Malignant cells in lung adeno-carcinoma grow and spread at a much slower rate than the other lung cancers and have better chances of detection in screening (Zappa and Mousa, 2016).
Squamous cell lung tumours, as a rule, happen in one of the left or right bronchus and smoking is considered as the main risk factor for this type. The tumour’s area oversees manifestations, for example, difficulty in breathing, chest torment, and blood in the sputum (Travis et al., 2010). Around 25–30% of lung cancer cases are diagnosed as SCC (Zappa and Mousa, 2016).
Large cell carcinoma (LCC) is a heterogeneous gathering of undifferentiated threatening neoplasms that do not have the cytologic and compositional elements of small cell carcinoma, glandular or squamous separation. LCC begins from central epithelial cells of the lung and spread to distant organs. A number of studies have shown a strong association between LCC and smoking which accounts for approximately 5–10% of all lung cancers (Zappa and Mousa, 2016).
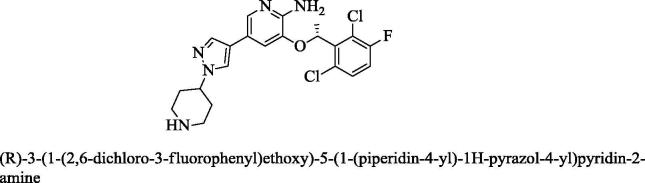
Anaplastic lymphoma kinase (ALK), also known as CD246, is a part of super family of insulin receptors which plays an important role in normal development and oncogenesis (Webb et al., 2009). It is a transmembrane tyrosine receptor kinase that can cause cancer – either by forming a combined gene NPM-ALK or by increasing the replication or duplication of the real DNA code. The 60% of anaplastic large cell lymphomas (ALCL) is the result of alteration in 2nd and 5th chromosome. This alteration makes a combination gene NPM-ALK, which comprises half of the portion of ALK (3′ half end) and half of the NPM, a potential oncogene (Mologni, 2012). This fused or combination of gene is responsible for about 75% of the cases of ALCL (Chiarle et al., 2008). In addition to NPM-ALK oncogene, several reports have also identified echinoderm microtubule-associated protein-like 4 (EML4)–ALK fusion protein in 2–7% of lung cancer patients suffering from NSCLC adeno-carcinomas (Wong et al., 2009). Therefore, ALK rearrangements or fusions seem to be viable therapeutic target in NSCLC. The search for simple molecules capable of inhibiting a highly attractive target ALK intensified since 2007 to develop potent anticancer agents (Iams and Lovly, 2015). Many first generations and multiple second generation ALK inhibitors were developed and approved for NSCLC therapy. However, treatment of patients with ALK-rearranged NSCLC with crizotinib (Fig. 1), a first-generation oral inhibitor of tyrosine kinases ALK, failed mainly because of; (i) acquired resistance to ALK inhibition mainly by target modification and ‘by pass’ signaling within one to two years of treatment (Katayama et al., 2012) and (ii) due to severe toxicity caused by its ability to enter into the CNS (Costa et al., 2011). Some of the second generation ALK inhibitors such as ceritinib (Fig. 2), alectinib showed better therapeutic efficacy than crizotinib in clinical trials but subsequently these developed resistance in clinical setting (Friboulet et al., 2014, Tanimoto et al., 2014).
Fig. 1.
Chemical structure of crizotinib, a 1st generation ALK inhibitor.
Fig. 2.
Chemical structure of ceritinib, a 2nd generation ALK inhibitor.
ARIAD Pharmaceuticals eventually succeeded in developing a new drug entity, a second generation ALK inhibitor, to combat the lung cancer which is named as brigatinib. It causes an effective dual inhibition of CD246 (ALK) and a trans-membrane protein EGFR or HER-1 (Human epidermal growth factor receptor) in humans (Huang et al., 2016). The inhibition of EGFR or HER-1 and ALK is mandatory to treat the cancer in lungs of a patient. Brigatinib was considered as an orphan drug in 2016 by the U.S. Food and Drug Administration for the treatment of NSCLC (www.ariad.com). It can be administered in a combination with anti-EGFR monoclonal antibody such as cetuximab or panitumumab and helps to overcome resistance to osimertinib (Uchibori et al., 2017). On 28th of April 2017, the U.S. FDA allowed quickened endorsement to brigatinib (Alunbrig tablets, Takeda Pharmaceutical Company Limited, through its completely claimed backup ARIAD Pharmaceuticals, Inc.) in order to treat the patients that are suffering from lung cancer caused due to alterations in the ALK and EGFR arrangement and the patients that are already resistant to other inhibitors (www.fda.gov), brigatinib is administered in the dose of 90 mg tablets (OD) orally during initial week; if endured, dose can be increased to 180 mg (OD)orally (www.en.pharmacodia.com) (Table 1).
Table 1.
The type of mutant variants of ALK and EGFR associated with lung cancer. It was reported that these variants are involved in resistance to common inhibitors but sensitive to Brigatinib.
| (A) ALK mutant variants | (B) EGFR mutant variants |
|---|---|
| → L1152R → C1156Y → V1180L → L1196M → G1202R → R1275Q |
→ T790M → C797S → L858R |
Brigatinib is represented by IUPAC name 5-chloro-4-N-(2-dimethylphosphorylphenyl)-2-N-(2-methoxy-4-(4-(4-methylpiperazin-1-yl) piperidin-1-yl] phenyl] pyrimidine-2,4-diamine. Brigatinib (Fig. 3) is considered as a wonder drug because it is active against the cases in which all the other ALK inhibitors such as osimertinib, loratinib (Fig. 4), etc. are ineffective. Specifically, the mutation in the arrangement of ALK space represents most of the cases that are resistant to the other ALK inhibitors (Hatcher et al., 2015). Investigation of all the preclinical data showed viability and greater activity of brigatinib against the various types of agent that cause G1202R and L1196M mutations in ALK when compared with other established inhibitors (Zhang et al., 2016).
Fig. 3.

Chemical structure of brigatinib.
Fig. 4.
Chemical structure of loratinib, a 3rdgeneration ALK Inhibitor.
2. Approval and development history of brigatinib
Mutations in EGFR and ALK genetic arrangements are the leading cause of death in lung cancer patients. Currently it is the drug of choice for providing treatment to patients that are resistant to other ALK inhibitors (Chiarle et al., 2008). The general information about brigatinib and its development history are summarized in Table 2, Table 3, respectively.
Table 2.
General information about brigatinib.
| S. No. | Category | General information |
|---|---|---|
| 1. | FDA Approval | It is first approved by FDA on 28 April 2017 |
| 2. | Brand name | Alunbrig |
| 3. | Active drug name | Brigatinib |
| 4. | Dosage and intake pattern | It is administered orally in the form of Tablets (90 mg OD) |
| 5. | Manufacturing company | This drug is manufactured by a Takeda Pharmaceuticals, USA., Inc |
| 6. | Indication | It is used to combat the cancer present in the non-small cells of lung (NSCLC) |
Table 3.
Developmental history of brigatinib.
| S. No. | Update on Brigatinib from 2015 to 2017 |
|---|---|
| 1. | On 17th April 2015, ARIAD pharmaceuticals showed updated information on the ongoing clinical trials of brigatinib in patients that were suffering from NSCLC caused due to ALK genetic rearrangements |
| 2. | In April 2016, phase ½ trial was completed and company updated the latest information about this trial |
| 3. | After completion of clinical trial studies, the ARIAD pharmaceuticals filed a New Drug Application for brigatinib in U.S. and FDA on 17th June 2016 |
| 4. | On 30th August 2016, completion of submission of New Drug Application in U.S. and Food and Drug Administration |
| 5. | On 31st October 2016, the manufacturer announced that FDA accepted the new drug application file |
| 6. | On April 28th 2017 TAKEDA announced that FDA has approved the brigatinib for market usage |
3. Safety profile of brigatinib
Brigatinib has proven to be successful in the management of various intracranial metastatic diseases. In phase ½ trial, it was noticed that it is effective in most of the subjects with quantifiable cerebral illness and some of the subjects with non-quantifiable pattern cerebral sickness (Gettinger et al., 2016). To check the effectiveness of brigatinib in patients with lung cancer in non-small cells, the toxic effect of brigatinib must have to be considered. The safety profile of brigatinib is based on the study done on the 79 patients suffering from lung cancer. Severe pulmonary adverse reactions consistent with interstitial lung disease or pneumonitis have occurred with 90 mg brigatinib therapy in 3.7% of patients and 9.1% of patients in the 90 → 180 mg group. These events mainly occur within the seven days of initiation of treatment. In comparison to other inhibitors such as crizotinib, the percentage of adverse effects were reduced such as 61% of looseness of bowels gets reduced to 13% with brigatinib and other adverse effects such as spewing, accumulation of fluid, blockage also decreased (Solomon et al.,2014).
4. Preclinical data of brigatinib
4.1. Drug discovery and chemical features of brigatinib
The synthesis of molecule that inhibits the ALK is difficult due to its high resemblance to the structure of various proteins that are member of group of receptors of insulin. Later on, results of various studies indicated that there are molecules that can suppress the ALK without compromising the selectivity over the insulin growth factor-1 receptor (Shakespeare et al., 2009). These studies resulted in discovery of brigatinib which can inactivate the ALK and insulin growth factor-1 receptor. The minimal inhibitory concentration (MIC) value of brigatinib was found to be 0.6 nmol/L individually. To test the activity in animals, brigatinib was administered orally to mice suffering from lung cancer and it showed the complete antitumor effect in the dose of 50–100 mg/kg. This dose also proved successful to combat the lung cancer in rats without compromising the selectivity over ALK (Shakespeare et al., 2009).
The structure of brigatinib (Fig. 3) differs from crizotinib (Fig. 1) as it contains a bis-anilino-pyrimidine moiety in place of amino-pyridine framework in comparison to crizotinib. This gives a U-shaped platform to the brigatinib so that it can bind to the ATP attachment site of ALK. The structure of brigatinib contains two NH2 groups attached to a phenyl ring which is further attached to carbon 2 and 4. The presence of —OCH3 group and the chlorine atom on carbon number 5 also help in communicating with the ALK (Huang et al., 2014, Huang et al., 2016). Another unique structural feature of brigatinib is that it contains dimethyl phosphine oxide (DMPO) moiety which is attached to the —NH2 group of phenyl ring present at carbon-4. The selectivity profile of brigatinib over ALK has been shown to be due to the dimethyl phosphine oxide moiety only. The chemical features of brigatinib are responsible for its properties like expanded fluid solvency, diminished lipophilicity and decreased protein binding (Huang et al., 2016).
4.2. Brigatinib activity against mutations in ALK
The resistance to ALK inhibitors is caused due to transformations in the ALK kinase area. Zhang et al. (2014) investigated the resistance by an in vitro experiment in Ba/F3 cells having different convergences of ALK inhibitors. They showed that brigatinib in concentration of 500 nmol/L was sufficient to overcome the resistance to other ALK inhibitors. In a similar study (Zhang et al., 2016), cell lines containing all the mutagenic substances that can cause the ALK resistance were developed. It was noted that brigatinib was more powerful against the mutagenic variations than all the other ALK inhibitors such as alectinib, crizotinib etc. with MIC value of <200 nmol/L. This drug also exhibited selectivity over other ALK mutant variants such as G1202R. The results of the study revealed brigatinib as the strongest ALK inhibitor that could effectively be used in all the ALK resistant cases where other ALK inhibitors are ineffective and thus could improve the life of patients suffering from NSCLC.
4.3. Brigatinib in pre-treated and resistant cases of crizotinib
Brigatinib is an orally active tyrosine kinase inhibitor (TKI) that represses ALK kinase with 12-times more noteworthy power than crizotinib (Zhang et al., 2016). It additionally inhibits ROS1 kinase and showed preclinical activity against several ALK mutations that underlie clinically-procured imperviousness to crizotinib. Multiple dosages of brigatinib (30–300 mg) evaluated in phase ½ of the clinical trial found an objective response rate (ORR) of 72% in the 71 enlisted patients with crizotinib-pretreated ALK-positive progressed NSCLC (Gettinger et al., 2016). In any case, in view of the occurrence of pulmonary toxicity with higher beginning measurements of brigatinib, the dosages of 90 mg OD and 180 mg OD followed by a 7-day treatment at 90 mg were both chosen for additional testing in the “ALTA” stage 2 (Camidge et al., 2017). The “ALTA” trial included 222 ALK-positive NSCLCs pre-treated with crizotinib (n = 112 in the 90-mg group; n = 110 in the 180-mg group). Significantly, ORR was numerically higher in the 180-mg group, being 54% when compared with 45% in the 90 mg group. Similarly, median progression-free survival was 12.9 months versus 9.2 months, separately. Generally, this information was extremely convincing, and bolstered the utilization of brigatinib in the crizotinib-resistant case at the dose of 180 mg with 7-day lead-in at 90 mg. On this premise, brigatinib got FDA leap forward treatment assignment in October 2014 to treat the patients that were resistant to other ALK inhibitors. In the “ALTA” trial, brigatinib additionally demonstrated a pharmacological activity in the CNS in comparison to other second-generation ALK-TKIs, with an intra-cranial ORR of 67% in patients (n = 18) with quantifiable CNS metastases (Camidge et al., 2017).
4.4. Brigatinib combination with anti EGFR monoclonal antibody to overcome resistance to osimertinib
NSCLC is also induced due to mutation in the epidermal growth factor receptor (EGFR). The mutated EGFR accounts for about 60–70% cases of NSCLC (Kohno et al., 2013). EGFR mutated lung cancer in non-small cells can be cured with inhibitors that efficiently inhibit EGFR. These inhibitors produce their action by inhibiting the down signaling mechanism by binding with adenosine triphosphate (ATP) site of EGFR (Giaccone, 2005, Maemondo et al., 2010, Mitsudomi et al., 2010, Melosky, 2014, Gao et al., 2012, Zhou et al., 2011, Rosell et al., 2012). Many clinical trials have been conducted involving EGFR-TKI that are active or used to treat EGFR activating mutation- positive lung cancer patients (Yang et al., 2015, Yoshioka et al., 2014, Inoue et al., 2012). The resistance against the first-generation EGFR-TKIs inhibitors is developed due to the gatekeeper mutations represented by the substitution of threonine with methionine at the position 790 (T790M) as well as the substitution of cysteine with serine at the position 797 (C797S) which both lead to hinder the binding of inhibitor at the ATP binding site (Kobayashi et al., 2005, Kosaka et al., 2006, Thress et al., 2015). Furthermore, Ercan et al. (2015) also suggested that L844V, L718Q and C797S amino acid substitutions also account for 60–70% resistant cases (Yu et al., 2013, Camidge et al., 2014). So, to treat EGFR-mutated NSCLC patients resistant to first and second generation ALK inhibitors, the third generation ALK inhibitor showing specific action toward the T790M were developed (Zhou et al., 2009, Cross et al., 2014, Walter et al., 2013).
Uchibori et al. (2017) reported that a unique allosteric inhibitor can be used to treat resistance to osimertinib if administered with an EGFR antibody cetuximab. Finally, the combination of EGFR inhibitor brigatinib with anti EGFR antibody cetuximab showed a satisfactory result to treat EGFR-mutated cases in Xenograft bearing mice. Cetuximab also reduced the IC50 value of brigatinib.
5. ALTA-1L trial of brigatinib
The ALTA-1L trial was intended to assess the potency of brigatinib versus crizotinib in patients having NSCLC due to rearrangement in ALK. In stage 1/2 clinical trial, brigatinib showed promising clinical results, both systemically and in the cerebrum, in ALK + NSCLC patients, including those with earlier crizotinib therapy and those who were crizotinib-resistant. In view of the consequences of a continuous crucial randomized stage 2 trial investigating 2 regimens of brigatinib (90 and 180 mg OD daily followed by treatment with 90 mg in next week), exhibited generous adequacy in patients with crizotinib-safe ALK + NSCLC and a worthy safety profile.
5.1. Phase I
The Phase I study was done in subjects suffering from lung cancer to achieve the essential goal of building up the dose of brigatinib that can be used in the further studies of phase II. The phase II heightening dose of the brigatinib extended from 30 to 300 mg day by day. Dosage constraining harmfulness observed at 240 and 300 mg day by day, and the prescribed phase II measurement was resolved to be 180 mg day by day. Due to the adverse effect in pulmonary area (happening inside initial week of treatment) at 180 mg, two extra regimens were evaluated: 90 mg once every day and 180 mg once day by day followed by a week in which 90 mg of brigatinib is administered day by day. Between September 2011 and July 2014, approx. 140 patients were studied within the two phases of clinical trials.
5.2. Phase II
In phase II there were five groups in which efficacy of brigatinib was determined by administering three different doses of brigatinib 90 mg, 180 mg and then a week with 90 mg OD. This study reported that 66% of subjects suffered from lung cancer showed improvement and 72% of patients that were already treated with the other ALK inhibitors showed good results. All the patients that were suffering from lung cancer due to genetic rearrangement in EGFR also showed the promising result with brigatinib. Brigatinib also proved successful in patients that were suffering from cerebral illness in addition to the lung cancer. The summary of five groups and their response to brigatinib is illustrated in the Table 4 (Gettinger et al., 2016):
Table 4.
Objective response rate (ORR) of five different cohorts treated with brigatinib.
| S. No. | Cohort | Category of patient | Objective response rate |
|---|---|---|---|
| 1 | Cohort 1 | ALK-inhibitor-naïve | ORR of 100% (4/4) |
| 2 | Cohort 2 | Patients that were already with other ALK inhibitor such as crizotinib | ORR of 74% (31/42) |
| 3 | Cohort 3 | Egfrt790m | 0% |
| 4 | Cohort 4 | Patients that were suffering from other cancers in addition to lung cancer | ORR of 17% (3/18) |
| 5 | Cohort 5 | Pre-treated with crizotinib | ORR of 50% (3/6). |
There are two dosage patterns that can be used to overcome the lung cancer in normal or in mutated cases. The patients that do not show any response to ALK inhibitors were used to receive brigatinib 90 mg OD and number of patients taken for study was found to be 12, also there were some patients who were administered 180 mg of brigatinib. There were 745 patients that were having treatment of cerebral illness and 66% of those patients were resistant to crizotinib. After completion of trial it was found that 42% of patients recovered from the lung cancer with 90 mg of brigatinib and 67% of patients with 180 mg of the drug (US FDA, 2017, Kim et al., 2017).
5.3. Results of phase ½ trial
Results of phase ½ trial showed that brigatinib have anticancer activity in patients suffering from NSCLC caused due to genetic rearrangements in ALK. There was 71% response rate in patients that used brigatinib as first line therapy, 53% in patients suffering from cerebral illness. These results were seen due to dosage regimen that contained 90 mg or 180 mg of brigatinb OD (Camidge et al., 2015).
6. Chemistry of brigatinib
Phosphorus is abundantly present in the human body but it is occasionally found in structure of therapeutic agents. This element in comparison to sulphur, oxygen, and nitrogen is underutilized and its clinical usefulness has been limited to small number of phosphonic or bisphosponic acid based drugs, in fewer phosphate-containing prodrugs as well as in phosphonates and phosphinate compounds (Smith et al., 2014).
Phosphorus atom if converted to different functionalities may help in designing of novel drugs with potent pharmacological actions. Rivera et al., in 2011 carried out dimethyl-phosphorylation of rapamycin at C43-OH which resulted in the discovery of a new drug molecule named as Ridaforolimus, a more stable mTOR inhibitor (Rivera et al., 2011). Recently, medicinal chemists have also explored phosphine oxide (P O) bond by incorporating dimetylphosphine oxide [(CH3)2P O; DMPO] moiety as a hydrogen bond acceptor in drug design of kinase inhibitors which lead to the discovery of brigatinib. Presence of DMPO moiety in brigatinib structure increases its potency about 70 folds than other un-substituted analogs (O'Hare et al., 2004, Dalgarno et al., 2006). The P O bond is easy to synthesize and becomes inert after incorporation into a structure. It also does not show much redox chemistry in comparison to carbonyls and alcohols functional groups, and its capacity to act as an H-bond acceptor makes it an alternative choice to existing more regular H-bond acceptors like carbonyls and sulfones (Laurence et al., 2009).
Brigatinib due to the presence of DMPO is hydrophilic in nature and it also contains a basic amine side chains that help in increasing cellular potency (Marsilje et al., 2013). The ALK-brigatinib binding complex shows that brigatinib binds to ALK in the ATP binding unit by adopting a U-shaped conformation. While the pyrimidine centre of brigatinib binds to the adenosine site, its methoxy group and DMPO aniline bind close to the hinge and DFG sites, separately. The power of brigatinib against ALK is attributed to the chemical substituents introduced on the bisanilino-pyrimidine scaffold. In addition, the DMPO moiety encourages intramolecular collaborations and settles the U-moulded adaptation of brigatinib through an O⋯NH hydrogen bond (Fig. 5). Following is the reported synthetic scheme for the synthesis of brigatinib (Scheme 1). The synthesis can be accomplished in the following steps:
-
(1)
2,4,5-Trichloropyrimidine (1) reacts with (2-aminophenyl)dimethyl-phosphine-oxide (a) in the presence of 54–72% of (i) K2CO3, NaH or LiHMDS, DMF at 65 °C to form 2-(2,5-Dichloropyrimidin-4-yl)amino)phenyl) dimethyl phosphine oxide (2).
-
(2)
2-(2,5-Dichloropyrimidin-4-yl)amino)phenyl)dimethylphosphineoxide(2) further reacts in the presence of 2-methoxy-4-(4-(4-Methylpiperazin-1-yl)piperidin-1-yl)aniline(a) and 48–86% of (ii) Pd(OAc)2, Xantphos, Cs2CO3, DMF at 110 °C to form 5-Chloro-4-N-(2-dimethylphosphorylphenyl)-2-N-[2-methoxy-4-[4-(4-methylpiperazin-1-yl)piperidin-1-yl] phenyl] pyrimidine-2,4-diamine i.e. Brigatinib (3)(Huang et al., 2016, Patel et al., 2017, Jang et al., 2017).
Fig. 5.
Interaction of brigatinib with the ATP binding site of ALK (pdb:5J7H).
Scheme 1.
Synthesis of brigatinib.
An economic alternative synthetic route for the industrial preparation of brigatinib is also reported in which the trichloropyrimidine ring was substituted with pyrimidine ring in the starting materials. The patent method for the synthesis involves following steps (i) synthesis of N-[2-methoxy-4-[4-(dimethylamino) piperidin-1-yl] aniline] guanidine starting from 2-methoxy-4-[4-(dimethylamino) piperidin-1-yl] aniline and cyanamide (ii) reaction of N-[2-methoxy-4-[4-(dimethylamino) piperidin-1-yl] aniline] guanidine and N-Methyl methacrylate or N,N dimethylformamide to obtain off solid compound namely N2-[4-[4-(dimethylamino)-1-piperidinyl]-2-methoxyphenyl] 1H) –pyrimidinone (iii) to the mixture of N2- [4-[4-(dimethylamino)-1-piperidinyl]-2-methoxyphenyl] amino-4 (1H) –pyrimidinone, benzotriazol-1-yloxytris (dimethylamino) phosphonium hexafluorophosphate and acetonitrile, Diazabicyclo [5.4.0] -undec-7-ene (DBU) was added drop wise and on usual workup N2-[4-[4-(dimethylamino)-1-piperidinyl]-2-methoxyphenyl]-N4-[2-(dimethylphosphono) phenyl]-2,4-pyrimidinediamine is obtained (iv) the N2- [4-[4-(dimethylamino)-1-piperidinyl]-2-methoxyphenyl]-N4-[2-(dimethylphosphono) phenyl]-2,4-pyrimidinediamine with a chlorinating agent in the presence of a base furnishes brigatinib (New patent, 2017)
7. Pharmacology of brigatinib
Brigatinib shows its activity against lung cancer by inhibiting the ALK, insulin growth factor receptor-1, EGFR and other kinases such as CD135 also called fem like tyrosine kinase-3 (FLT3). It primarily inhibits attachment of phosphate group to the ALK and thereby stops the phosphorylation of other proteins that are involved in the lung cancer (Markham, 2017). Various studies on mice revealed that in addition to these activities brigatinib also inhibits the growth of various cell lines and prevents the formation of fused gene of Nucleophosmin and ALK (Markham, 2017). The various mutants such as G1202R, L1196M were also inhibited by the brigatinib. Brigatinib can also improve the life of the patient suffering from cerebral illness in addition to lung cancer. The concentration of brigatinib that is used to hinder the potency of cells to cause cancer and activity against the cases that are resistant to other ALK inhibitors was found to be <500 nM (www.ndrugs.com). Though, brigatinib is comparatively a safer drug but ≥10% of all patients receiving approved dose of it showed some common side effects including increased blood glucose (43%), nausea (40%), diarrhoea (38%), cough (30%), headache (27%) etc. Some of the less common toxic effects observed in <10% patients of all grades include hypertension (6%), pneumonia (5%), interstitial lung disease/pneumonitis (9.1%) and visual disturbances (7.3%) (Mann, 2018, Sabari et al., 2017, Gettinger et al., 2016).
8. Pharmacokinetic profile
The geometric mean concentration (CV%) and steady-state maximum concentration (Cmax) of 552 ng/ml and 452 ng/ml were observed at the dose of 90 and 180 mg OD of brigatinib, respectively, and the related AUC was 8165 (57%) ng∙h/mL and 20,276 (56%) ng∙h/mL. After the repetitive exposure to the dose of brigatinb, the concentration of accumulated brigatinib within the body was found to be 1.9–2.4 (ARIAD Pharmaceuticals, 2017).
8.1. Absorption
After oral administration of a single dose, 30–240 mg of brigatinib, the median time peak concentration (Tmax) was observed to be 1–4 h (ARIAD Pharmaceuticals, 2017).
8.2. Distribution
Brigatinib has high affinity toward the proteins present in plasma of human and 66% of it gets attached to the proteins. The ratio of blood-plasma concentration was found to be 0.69. After 180 mg once daily oral administration of brigatinib, the mean apparent volume of distribution (Vz/F) at a steady rate was 153 L (ARIAD Pharmaceuticals, 2017).
8.3. Metabolism
Brigatinib is mainly metabolised by two cytochrome enzymes such as CYP2C8 and CYP3A4 in vitro. After single oral administration of 180 mg, brigatinib is metabolised by two major metabolic pathways N-demethylation and cysteine conjugation. About 3.5% of brigatinib gets metabolised to its primary metabolite and 92% remain unchanged. The metabolite of brigatinib is less potent than brigatinib and binds to ALK with fewer efficacies (ARIAD Pharmaceuticals, 2017).
8.4. Excretion
After 180 mg of oral administration of brigatinib, 65% of administered dose can be recovered from faeces and 25% can be recovered from urine. The concentration of unchanged form of brigatinib in faeces and urine was found to be 41% and 86%, respectively. At steady state, the mean apparent oral clearance and mean plasma elimination half-life was 12.7 L/h and 25 h respectively (ARIAD Pharmaceuticals, 2017).
8.5. Drug and food interactions with brigatinib
Administration of food exerts a considerable effect on the steady state maximum concentration (Cmax) of brigatinib. The Cmax was reduced to be about 13% by administered brigatinib after high fat meal compared to Cmax after overnight fasting (Kadi et al., 2018). The presence of fatty meal does not have any effect on AUC, therefore, brigatinib can be taken with or without food. However, grape fruit can increase the blood levels of brigatinib and may lead to an increase in side effects such as nausea, vomiting, diarrhoea, hypertension, visual disturbances etc. Therefore, patients on brigatinib therapy should avoid consumption of grape fruit or its juice. Moreover, there are some drugs that may negatively affect brigatinib metabolism such as:
-
(a)
Gemfibrozil: Administration of about 600 mg BD of gemfibrozil with 90 mg OD dose of brigatinib results in decrease of Cmax of brigatinib to about 41% and AUC by 12% (Kadi et al., 2018).
-
(b)
Rifampin In comparison to administration of 180 mg dose of brigatinib alone, co-administration of brigatinib with a strong CYP3A inducer such as rifampin 600 mg twice daily result in decrease in plasma concentration of brigatinib about 60% and AUC about 80% (Kadi et al., 2018)
8.6. Effect of hepatic impairment
After a population pharmacokinetic analysis in which brigatinib is administered to 49 patients with mild hepatic impairment and 377 patients with normal hepatic function, it was observed that, brigatinib is mainly eliminated by liver and hepatic impairment result in an increase in plasma concentration of brigatinib (Kim et al., 2017).
8.7. Effect of renal impairment
To check the effect of renal impairment on pharmacokinetic profile of brigatinib, a study was carried out involving 125 subjects with very less renal dysfunction, 34 subjects with moderate renal impairment and 270 subjects with normal renal function. Based on this study results, authors concluded that renal impairment has no major effect and there is no need to adjust the dose of brigatinib in patients having kidney dysfunction because it has no effect on the pharmacokinetic profile of brigatinb as it is mainly eliminated by the liver (Kadi et al., 2018).
9. Drug combination therapy with brigatinib
Combination therapy has been studied and considered as an attractive approach in oncology and proved successful in the treatment of cancer. Drug combinations have the potential to improve therapeutic efficacy, reduce development of drug resistance and lower the incidence of side effects resulting from the individual use of anticancer agents. The use of drug combination therapy with lung cancer has been proven effective (Wu et al., 2017). One successful example of combination is brigatinib with itraconazole. In comparison to the administration of 90 mg dose of brigatinib alone, co-administration of brigatinib with itraconazole 200 mg twice daily, a strong CYP3A inhibitor, result in increase in plasma concentration of brigatinib about 21% and AUC about 101%. It is because brigatinib is majorly metabolised to its primary metabolite with the help of CYP3A enzyme (Kadi et al., 2018).
10. Pharmacodynamics of brigatinib
Brigatinib shows its action by inhibiting attachment of phosphate group to the ALK and results in inhibition of proteins such as STAT3, AKT, ERK1/2, and S6 both in vitro and in vivo (Jang et al., 2017). According to in vitro kinase assays, brigatinib proved potent against ALK with inhibitory concentration-50 value of 0.6 nmol/L including the mutant variants C1156Y (0.6 nmol/L) and R1275Q (6.6 nmol/L). Brigatinib causes inhibition of CD135, mutant variants of FLT3 (D835Y) and epidermal growth factor receptor (L858R; IC50 1.5–2.1 nmol/L) and to a lesser extent EGFR with a T790M resistance mutation (L858R/T790M), native EGFR, IGF-R1, and INSR (IC50 values 29–160 nmol/L). Brigatinib hindered development of different anaplastic extensive cell lymphoma (ALCL) and NSCLC cell lines expressing fused gene combinations of nucleophosmin and ALK [growth inhibition of half of cells (GI50) 4–31 nmol/L]; the ALK phosphorylation IC50 of the medication in these cell lines was 1.5–12 nmol/L. Brigatinib effectively inhibits the mutated receptors that stops to respond to other ALK inhibitors such as crizotinib, alectinib and ceritinib. It is more potent than crizotinib by 2.2-to 77-crease and three times more potent than the inhibitor ceritinib. It effectively inhibits the mutants like L1152R and V1180L and represses the tumour development in ALK positive lung cancer (Kadi et al., 2018).
11. Conclusion and future directions
Brigatinib is a novel molecule that is quite effective in the treatment of NSCLC and in certain resistant cases where other ALK inhibitors are ineffective. The potent anti-cancer activity of brigatinib is attributed to its chemical structure which contains various functionalities along with Phosphorus atom that binds to target protein. However, incidents of pulmonary toxicity in some patients have been reported which may be life threatening. Therefore, more research should be carried out on a priority basis to identify the group of patients who are at risk to overcome this side effect of brigatinib and to improve its safety spectrum. This can be approached in different ways: (1) design, synthesise and evaluate new derivatives and analogues of brigatinib to improve its selectivity against all mutant variants of ALK causing lung cancer, and (2) the use of brigatinib in combination with anti-cancer natural products/herbal drugs to assess their efficacy and safety in the treatment of lung cancer.
A currently ongoing phase II trial of brigatinib in patients previously treated with 2nd generation ALK inhibitors will further establish its role in overcoming the resistance to these inhibitors.
Footnotes
Peer review under responsibility of King Saud University.
References
- ARIAD Pharmaceuticals Inc., 2017. ALUNBRIGTM (brigatinib): US prescribing information. https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/208772lbl.pdf (accessed 14.02.18).
- Camidge D.R., Bazhenova L., Salgia R., Langer C.J., Gold K.A., Rosell R., Shaw A.T., Weiss G.J., Narasimhan N.I., Dorer D.J., Rivera V.M. Safety and efficacy of brigatinib (AP26113) in advanced malignancies, including ALK+ non–small cell lung cancer (NSCLC) J. Clin. Oncol. 2015;33(15):8062. [Google Scholar]
- Camidge D.R., Pao W., Sequist L.V. Acquired resistance to TKIs in solid tumours: learning from lung cancer. Nat. Rev.Clin. Oncol. 2014;11(8):473–481. doi: 10.1038/nrclinonc.2014.104. [DOI] [PubMed] [Google Scholar]
- Camidge D.R., Tiseo M., Ahn M.J., Reckamp K.L., Hansen K.H., Kim S.W., Huber R.M., West H.L., Groen H.J., Hochmair M.J., Leighl N.B. Brigatinib in crizotinib-refractory ALK+ NSCLC: Central assessment and updates from ALTA, a pivotal randomized phase 2 trial. J. Thorac. Oncol. 2017;12(1):1167–1169. [Google Scholar]
- Chan B.A., Hughes B.G.M. Targeted therapy for non-small cell lung cancer: current standards and the promise of the future. Transl. Lung Cancer Res. 2015;4(1):36–54. doi: 10.3978/j.issn.2218-6751.2014.05.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chiarle R., Voena C., Ambrogio C., Piva R., Inghirami G. The anaplastic lymphoma kinase in the pathogenesis of cancer. Nat. Rev. Cancer. 2008;8:11–23. doi: 10.1038/nrc2291. [DOI] [PubMed] [Google Scholar]
- Costa D.B., Kobayashi S., Pandya S.S., Yeo W.L., Shen Z., Tan W., Wilner K.D. CSF concentration of the anaplastic lymphoma kinase inhibitor crizotinib. J. Clin. Oncol. 2011;29(15):e443–e445. doi: 10.1200/JCO.2010.34.1313. [DOI] [PubMed] [Google Scholar]
- Cross D.A., Ashton S.E., Ghiorghiu S., Eberlein C., Nebhan C.A., Spitzler P.J., Orme J.P., Finlay M.R., Ward R.A., Mellor M.J., Hughes G. AZD9291, an irreversible EGFR TKI, overcomes T790M-mediated resistance to EGFR inhibitors in lung cancer. Cancer Discov. 2014;4(9):1046–1061. doi: 10.1158/2159-8290.CD-14-0337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dalgarno D., Stehle T., Narula S., Schelling P., Van Schravendijk M.R., Adams S., Andrade L., Keats J., Ram M., Jin L., Grossman T., MacNeil I., Metcalf C., Shakespeare W., Wang Y., Keenan T., Sundaramoorthi R., Bohacek R., Weigele M., Sawyer T. Structural basis of Src tyrosine kinase inhibition with a new class of potent and selective trisubstituted purine-based compounds. Chem. Biol. Drug Des. 2006;67:46–57. doi: 10.1111/j.1747-0285.2005.00316.x. [DOI] [PubMed] [Google Scholar]
- Ercan D., Choi H.G., Yun C.H., Capelletti M., Xie T., Eck M.J., Gray N.S., Jänne P.A. EGFR mutations and resistance to irreversible pyrimidine-based EGFR inhibitors. Clin. Cancer Res. 2015;21(17):3913–3923. doi: 10.1158/1078-0432.CCR-14-2789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friboulet L., Li N., Katayama R., Lee C.C., Gainor J.F., Crystal A.S., Michellys P.Y., Awad M.M., Yanagitani N., Kim S., Pferdekamper A.C. The ALK inhibitor ceritinib overcomes crizotinib resistance in non–small cell lung cancer. Cancer Discov. 2014;4(6):662–673. doi: 10.1158/2159-8290.CD-13-0846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gao G., Ren S., Li A., Xu J., Xu Q., Su C., Guo J., Deng Q., Zhou C. Epidermal growth factor receptor-tyrosine kinase inhibitor therapy is effective as first-line treatment of advanced non-small cell lung cancer with mutated EGFR: a meta-analysis from six phase III randomized controlled trials. Int. J. Cancer. 2012;131(5):822–829. doi: 10.1002/ijc.27396. [DOI] [PubMed] [Google Scholar]
- Gettinger S.N., Bazhenova L.A., Langer C.J., Salgia R., Gold K.A., Rosell R., Shaw A.T., Weiss G.J., Tugnait M., Narasimhan N.I., Dorer D.J. Activity and safety of brigatinib in ALK-rearranged non-small-cell lung cancer and other malignancies: a single-arm, open-label, phase 1/2 trial. Lancet Oncol. 2016;17(12):1683–1696. doi: 10.1016/S1470-2045(16)30392-8. [DOI] [PubMed] [Google Scholar]
- Giaccone G. Epidermal growth factor receptor inhibitors in the treatment of non–small-cell lung cancer. J. Clin. Oncol. 2005;23(14):3235–3242. doi: 10.1200/JCO.2005.08.409. [DOI] [PubMed] [Google Scholar]
- Hatcher J.M., Bahcall M., Choi H.G., Gao Y., Sim T., George R., Jänne P.A., Gray N.S. Discovery of inhibitors that overcome the G1202R anaplastic lymphoma kinase resistance mutation. J. Med. Chem. 2015;58(23):9296–9308. doi: 10.1021/acs.jmedchem.5b01136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- http://en.pharmacodia.com/web/drug/1_849.html (accessed 04.01.18).
- http://www.ariad.com/research-development/brigatinib (accessed 02.01.18).
- http://www.ndrugs.com/?s=brigatinib&t=actions (accessed 12.02.18).
- https://www.fda.gov/Drugs/InformationOnDrugs/ApprovedDrugs/ucm555841.htm (accessed 04.01.18).
- Huang Q., Johnson T.W., Bailey S., Brooun A., Bunker K.D., Burke B.J., Collins M.R., Cook A.S., Cui J.J., Dack K.N., Deal J.G. Design of potent and selective inhibitors to overcome clinical anaplastic lymphoma kinase mutations resistant to crizotinib. J. Med. Chem. 2014;57(4):1170–1187. doi: 10.1021/jm401805h. [DOI] [PubMed] [Google Scholar]
- Huang W.S., Liu S., Zou D., Thomas M., Wang Y., Zhou T., Romero J., Kohlmann A., Li F., Qi J., Cai L. Discovery of brigatinib (AP26113), a phosphine oxide-containing, potent, orally active inhibitor of anaplastic lymphoma kinase. J. Med. Chem. 2016;59(10):4948–4964. doi: 10.1021/acs.jmedchem.6b00306. [DOI] [PubMed] [Google Scholar]
- Iams W.T., Lovly C.M. Anaplastic Lymphoma Kinase (ALK) as a therapeutic target in non-small cell lung cancer. Cancer J. 2015;21(5):378–382. doi: 10.1097/PPO.0000000000000142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Inoue A., Kobayashi K., Maemondo M., Sugawara S., Oizumi S., Isobe H., Gemma A., Harada M., Yoshizawa H., Kinoshita I., Fujita Y. Updated overall survival results from a randomized phase III trial comparing gefitinib with carboplatin–paclitaxel for chemo-naïve non-small cell lung cancer with sensitive EGFR gene mutations (NEJ002) Ann. Oncol. 2012;24(1):54–59. doi: 10.1093/annonc/mds214. [DOI] [PubMed] [Google Scholar]
- Jang J., Son J.B., To C., Bahcall M., Kim S.Y., Kang S.Y., Mushajiang M., Lee Y., Jänne P.A., Choi H.G., Gray N.S. Discovery of a potent dual ALK and EGFR T790M inhibitor. Eur. J. Med. Chem. 2017;136:497–510. doi: 10.1016/j.ejmech.2017.04.079. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kadi A.A., Attwa M.W., Darwish H.W. LC-ESI-MS/MS reveals the formation of reactive intermediates in brigatinib metabolism: elucidation of bioactivation pathways. RSC Adv. 2018;8(3):1182–1190. doi: 10.1039/c7ra10533a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Katayama, R., Shaw, A.T., Khan T.M., Mino-Kenudson, M., Solomon, B.J., Halmos, B., Jessop, N.A., Wain, J.C., Yeo, A.T., Benes, C., Drew, L., Saeh, J.C., Crosby, K., Sequist, L.V., Iafrate, A.J., Engelman, J.A., 2012. Mechanisms of acquired crizotinib resistance in ALK-rearranged lung cancers. Sci. Transl. Med. 4(120), 120ra l7. [DOI] [PMC free article] [PubMed]
- Kim D.W., Tiseo M., Ahn M.J., Reckamp K.L., Hansen K.H., Kim S.W., Huber R.M., West H.L., Groen H.J., Hochmair M.J., Leighl N.B. Brigatinib in patients with crizotinib-refractory anaplastic lymphoma kinase–positive non–small-cell lung cancer: a randomized, multicenter phase II trial. J. Clin. Oncol. 2017;35(22):2490–2498. doi: 10.1200/JCO.2016.71.5904. [DOI] [PubMed] [Google Scholar]
- Kobayashi S., Boggon T.J., Dayaram T., Jänne P.A., Kocher O., Meyerson M., Johnson B.E., Eck M.J., Tenen D.G., Halmos B. EGFR mutation and resistance of non–small-cell lung cancer to gefitinib. N. Engl. J. Med. 2005;352(8):786–792. doi: 10.1056/NEJMoa044238. [DOI] [PubMed] [Google Scholar]
- Kohno T., Tsuta K., Tsuchihara K., Nakaoku T., Yoh K., Goto K. RET fusion gene: translation to personalized lung cancer therapy. Cancer Sci. 2013;104(11):1396–1400. doi: 10.1111/cas.12275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosaka T., Yatabe Y., Endoh H., Yoshida K., Hida T., Tsuboi M., Tada H., Kuwano H., Mitsudomi T. Analysis of epidermal growth factor receptor gene mutation in patients with non–small cell lung cancer and acquired resistance to gefitinib. Clin. Cancer Res. 2006;12(19):5764–5769. doi: 10.1158/1078-0432.CCR-06-0714. [DOI] [PubMed] [Google Scholar]
- Laurence C., Brameld K.A., Graton J., Le Questel J.Y., Renault E. The p K BHX database: toward a better understanding of hydrogen-bond basicity for medicinal chemists. J. Med. Chem. 2009;52(14):4073–4086. doi: 10.1021/jm801331y. [DOI] [PubMed] [Google Scholar]
- Maemondo M., Inoue A., Kobayashi K., Sugawara S., Oizumi S., Isobe H., Gemma A., Harada M., Yoshizawa H., Kinoshita I., Fujita Y. Gefitinib or chemotherapy for non–small-cell lung cancer with mutated EGFR. N. Engl. J. Med. 2010;362(25):2380–2388. doi: 10.1056/NEJMoa0909530. [DOI] [PubMed] [Google Scholar]
- Markham, A., 2017. Brigatinib: First global approval. Drugs. 2017 June 8: 1-5 (accessed 02.02.18). [DOI] [PubMed]
- Marsilje T.H., Pei W., Chen B., Lu W., Uno T., Jin Y., Jiang T., Kim S., Li N., Warmuth M., Sarkisova Y., Sun F., Steffy A., Pferdekamper A.C., Li A.G., Joseph S.B., Kim Y., Liu B., Tuntland T., Cui X., Gray N.S., Steensma R., Wan Y., Jiang J., Chopiuk G., Li J., Gordon W.P., Richmond W., Johnson K., Chang J., Groessl T., He Y.Q., Phimister A., Aycinena A., Lee C.C., Bursulaya B., Karanewsky D.S., Seidel H.M., Harris J.L., Michellys P.Y. Synthesis, structure–activity relationships, and in vivo efficacy of the novel potent and selective anaplastic lymphoma kinase (ALK) inhibitor 5-Chloro-N 2-(2-isopropoxy-5-methyl-4-(piperidin-4-yl) phenyl)-N 4-(2-(isopropylsulfonyl) phenyl) pyrimidine-2, 4-diamine (LDK378) currently in phase 1 and phase 2 clinical trials. J. Med. Chem. 2013;56(14):5675–5690. doi: 10.1021/jm400402q. [DOI] [PubMed] [Google Scholar]
- Mann J.E. Brigatnib (Alunbrig®) Oncol. Times. 2018;40(4):23. [Google Scholar]
- Melosky B. Review of EGFR TKIs in metastatic NSCLC, including ongoing trials. Front. Oncol. 2014;4:244. doi: 10.3389/fonc.2014.00244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mitsudomi T., Morita S., Yatabe Y., Negoro S., Okamoto I., Tsurutani J., Seto T., Satouchi M., Tada H., Hirashima T., Asami K. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol. 2010;11(2):121–128. doi: 10.1016/S1470-2045(09)70364-X. [DOI] [PubMed] [Google Scholar]
- Mologni L. Inhibitors of the anaplastic lymphoma kinase. Expert Opin. Investig. Drugs. 2012;21(7):985–994. doi: 10.1517/13543784.2012.690031. [DOI] [PubMed] [Google Scholar]
- New Patent . Suzhou MiracPharma Technology Co Ltd; Brigatinib, WO: 2017. Preparation method for antitumor drug AP26113; p. 2017016410. [Google Scholar]
- O'Hare T., Pollock R., Stoffregen E.P., Keats J.A., Abdullah O.M., Moseson E.M., Rivera V.M., Tang H., Metcalf C.A., Bohacek R.S., Wang Y. Inhibition of wild-type and mutant Bcr-Abl by AP23464, a potent ATP-based oncogenic protein kinase inhibitor: implications for CML. Blood. 2004;104(8):2532–2539. doi: 10.1182/blood-2004-05-1851. [DOI] [PubMed] [Google Scholar]
- Patel H., Pawara R., Ansari A., Surana S. Recent updates on third generation EGFR inhibitors and emergence of fourth generation EGFR inhibitors to combat C797S resistance. Eur. J. Med. Chem. 2017;142:32–47. doi: 10.1016/j.ejmech.2017.05.027. [DOI] [PubMed] [Google Scholar]
- Rivera V.M., Squillace R.M., Miller D., Berk L., Wardwell S.D., Ning Y., Pollock R., Narasimhan N.I., Iuliucci J.D., Wang F., Clackson T. Ridaforolimus (AP23573; MK-8669), a potent mTOR inhibitor, has broad antitumor activity and can be optimally administered using intermittent dosing regimens. Mol. Cancer Ther. 2011;10(6):1059–1071. doi: 10.1158/1535-7163.MCT-10-0792. [DOI] [PubMed] [Google Scholar]
- Rosell R., Carcereny E., Gervais R., Vergnenegre A., Massuti B., Felip E., Palmero R., Garcia-Gomez R., Pallares C., Sanchez J.M., Porta R. Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): a multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2012;13(3):239–246. doi: 10.1016/S1470-2045(11)70393-X. [DOI] [PubMed] [Google Scholar]
- Sabari J.K., Santini F.C., Schram A.M., Bergagnini I., Chen R., Mrad C., Lai W.V., Arbour K.C., Drilon A. The activity, safety, and evolving role of brigatinib in patients with ALK-rearranged non-small cell lung cancers. OncoTargets Ther. 2017;10:1983–1992. doi: 10.2147/OTT.S109295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shakespeare W., Fantin V., Wang F., Kohlmann A., Liu S., Huang W.S., Wang Y., Zou D., Thomas M., Li F., Qi J. Discovery of potent and selective orally active inhibitors of anaplastic lymphoma kinase (ALK) Cancer Res. 2009;69:3738. [Google Scholar]
- Sher T., Dy G.K., Adjei A.A. Small cell lung cancer. Mayo Clin. Proc. 2008;83:355–367. doi: 10.4065/83.3.355. [DOI] [PubMed] [Google Scholar]
- Smith B.R., Eastman C.M., Njardarson J.T., Beyond C.H.O. Analysis of the elemental composition of US FDA approved drug architectures: Miniperspective. J. Med. Chem. 2014;57(23):9764–9773. doi: 10.1021/jm501105n. [DOI] [PubMed] [Google Scholar]
- Solomon B.J., Mok T., Kim D.W., Wu Y.L., Nakagawa K., Mekhail T., Felip E., Cappuzzo F., Paolini J., Usari T., Iyer S. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N. Engl. J. Med. 2014;371(23):2167–2177. doi: 10.1056/NEJMoa1408440. [DOI] [PubMed] [Google Scholar]
- Tanimoto A., Yamada T., Nanjo S., Takeuchi S., Ebi H., Kita K., Matsumoto K., Yano S. Receptor ligand-triggered resistance to alectinib and its circumvention by Hsp90 inhibition in EML4-ALK lung cancer cells. Oncotarget. 2014;5(13):4920–4928. doi: 10.18632/oncotarget.2055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thress K.S., Paweletz C.P., Felip E., Cho B.C., Stetson D., Dougherty B., Lai Z., Markovets A., Vivancos A., Kuang Y., Ercan D. Acquired EGFR C797S mutation mediates resistance to AZD9291 in non–small cell lung cancer harboring EGFR T790M. Nat. Med. 2015;21(6):560–562. doi: 10.1038/nm.3854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Travis, W.D., Brambilla, E., Müller-Hermelink. H.K., Harris, C.C., 2010. Pathology and genetics of tumours of the lung, pleura, thymus and heart. World Health Organization Classification of Tumours. IARC Press, Lyon. ISBN 92-832-2418-3.
- Uchibori K., Inase N., Araki M., Kamada M., Sato S., Okuno Y., Fujita N., Katamyama R. Brigatinib combined with anti-EGFR antibody overcomes osimertinib resistance in EGFR-mutated non-small-cell lung cancer. Nature Commun. 2017;13(8):14768. doi: 10.1038/ncomms14768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- US FDA, 2017. Brigatinib [media release] 28 April 2017. http://www. fda.gov (accessed 30.01.18).
- Walter A.O., Sjin R.T., Haringsma H.J., Ohashi K., Sun J., Lee K., Dubrovskiy A., Labenski M., Zhu Z., Wang Z., Sheets M. Discovery of a mutant-selective covalent inhibitor of EGFR that overcomes T790M-mediated resistance in NSCLC. CancerDiscov. 2013;3(12):1404–1415. doi: 10.1158/2159-8290.CD-13-0314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Webb T.R., Slavish J., George R.E., Look A.T., Xue L., Jiang Q., Cui X., Rentrop W.B., Morris S.W. Anaplastic lymphoma kinase: role in cancer pathogenesis and small-molecule inhibitor development for therapy. Expert Rev. Anticancer Ther. 2009;9(3):331–356. doi: 10.1586/14737140.9.3.331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- West L., Vidwans S.J., Campbell N.P. A novel classification of lung cancer into molecular subtypes. PLoS One. 2012;7:e31906. doi: 10.1371/journal.pone.0031906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wong D.W., Leung E.L., So K.K., Tam I.Y., Sihoe A.D., Cheng L.C., Ho K.K., Au J.S., Chung L.P., Wong M., Pik The EML4–ALK fusion gene is involved in various histologic types of lung cancers from non-smokers with wild-type EGFR and KRAS. Cancer. 2009;115(8):1723–1733. doi: 10.1002/cncr.24181. [DOI] [PubMed] [Google Scholar]
- Wu L., Leng D., Cun D., Foged C., Yang M. Advances in combination therapy of lung cancer: Rationales, delivery technologies and dosage regimens. J. Control. Release. 2017;260:78–91. doi: 10.1016/j.jconrel.2017.05.023. [DOI] [PubMed] [Google Scholar]
- Yang J.C., Wu Y.L., Schuler M., Sebastian M., Popat S., Yamamoto N., Zhou C., Hu C.P., O'Byrne K., Feng J., Lu S. Afatinib versus cisplatin-based chemotherapy for EGFR mutation-positive lung adenocarcinoma (LUX-Lung 3 and LUX-Lung 6): analysis of overall survival data from two randomised, phase 3 trials. Lancet Oncol. 2015;16(2):141–151. doi: 10.1016/S1470-2045(14)71173-8. [DOI] [PubMed] [Google Scholar]
- Yoshioka H., Mitsudomi T., Morita S., Yatabe Y., Negoro S., Okamoto I., Seto T., Satouchi M., Tada H., Hirashima T., Asami K. Final overall survival results of WJTOG 3405, a randomized phase 3 trial comparing gefitinib (G) with cisplatin plus docetaxel (CD) as the first-line treatment for patients with non-small cell lung cancer (NSCLC) harboring mutations of the epidermal growth factor receptor (EGFR) J. Clin. Oncol. 2014;32(15):8117. [Google Scholar]
- Yu H., Arcila M.E., Rekhtman N., Sima C.S., Zakowski M.F., Pao W., Kris M.G., Miller V.A., Ladanyi M., Riely G.J. Analysis of mechanisms of acquired resistance to EGFR TKI therapy in 155 patients with EGFR-mutant lung cancers. Clin. Cancer Res. 2013;19:2240–2247. doi: 10.1158/1078-0432.CCR-12-2246. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zappa C., Mousa S.A. Non-small cell lung cancer: current treatment and future advances. Transl. Lung Cancer Res. 2016;5(3):288–300. doi: 10.21037/tlcr.2016.06.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang S., Anjum R., Squillace R., Nadworny S., Zhou T., Keats J., Ning Y., Wardwell S.D., Miller D., Song Y., Eichinger L. The potent ALK inhibitor brigatinib (AP26113) overcomes mechanisms of resistance to first-and second-generation ALK inhibitors in preclinical models. Clin. Cancer Res. 2016;22(22):5527–5538. doi: 10.1158/1078-0432.CCR-16-0569. [DOI] [PubMed] [Google Scholar]
- Zhang, S., Wang, F., Keats, J., Ning, Y., Wardwell, S.D., Moran, L., Mohemmad, Q.K., Anjum, R., Wang, Y., Zhu, X., Miret, J.J., 2014. A potent ALK inhibitor overcomes mutations in EML4-ALK that confer resistance to PF-02341066 (PF1066). Cancer Res. 70(8), LB-298.
- Zhou C., Wu Y.L., Chen G., Feng J., Liu X.Q., Wang C., Zhang S., Wang J., Zhou S., Ren S., Lu S. Erlotinib versus chemotherapy as first-line treatment for patients with advanced EGFR mutation-positive non-small-cell lung cancer (OPTIMAL, CTONG-0802): A multicentre, open-label, randomised, phase 3 study. Lancet Oncol. 2011;12(8):735–742. doi: 10.1016/S1470-2045(11)70184-X. [DOI] [PubMed] [Google Scholar]
- Zhou W., Ercan D., Chen L., Yun C.H., Li D., Capelletti M., Cortot A.B., Chirieac L., Iacob R.E., Padera R., Engen J.R. Novel mutant-selective EGFR kinase inhibitors against EGFR T790M. Nature. 2009;462(7276):1070–1074. doi: 10.1038/nature08622. [DOI] [PMC free article] [PubMed] [Google Scholar]