Abstract
Congenital malformations of the seminal vesicle are uncommon, and most of them are cystic malformations. If an insult occurs during the first trimester of gestation, the embryogenesis of the kidney, ureter, seminal vesicle, and vas deferens could be altered. The mutual embryological origins of the seminal vesicle and ureteral bud from the mesonephric (Wolffian) duct result in association between ipsilateral renal agenesis and seminal vesical cysts. Zinner syndrome is a rare condition comprising a triad of unilateral renal agenesis, ipsilateral seminal vesicle obstruction and ipsilateral ejaculatory duct obstruction. This syndrome were first described by Zinner in 1914, and 200 cases have been reported in the literature. Most patients with this anomaly are asymptomatic until the second or third decade of life. Some cases have nonspecific symptoms such as prostatism, urinary urgency, dysuria, painful ejaculation, and perineal discomfort. In this paper, we present a uncommon case of a 21-year-old patient which the initial presentation of this condition was intermittent scrotal pain. A brief review of the literature is undertaken, regarding the main clinical, imaging implications, and the developmental anomalies that are involved in this congenital anomaly.
Keywords: Zinner syndrome, Hemospermia, Ejaculation, Infertility, Mesonephric duct abnormality, Genital diseases
Introduction
Congenital malformations of the seminal vesicle are uncommon, and most of them are cystic malformations. If an insult occurs during the first trimester of gestation, the embryogenesis of the kidney, ureter, seminal vesicle, and vas deferens could be altered.
The mutual embryological origins of the seminal vesicle and ureteral bud from the mesonephric (Wolffian) duct result in association between ipsilateral renal agenesis and seminal vesical cysts.
Zinner syndrome is a rare condition comprising a triad of unilateral renal agenesis, ipsilateral seminal vesicle obstruction and ipsilateral ejaculatory duct obstruction.
This syndrome were first described by Zinner in 1914, and 200 cases have been reported in the literature.
Most patients with this anomaly are asymptomatic until the second or third decade of life. Some cases have nonspecific symptoms such as prostatism, urinary urgency, dysuria, painful ejaculation, and perineal discomfort.
In this paper, we present an uncommon case of a 21-year-old patient which the initial presentation of this condition was intermittent scrotal pain.
A brief review of the literature is undertaken, regarding the main clinical, imaging implications, and the developmental anomalies that are involved in this congenital anomaly.
Case report
A 21-year-old male was referred to urology department for repetitive episodes of intermittent scrotal pain during 4 months. He denied trauma, hemospermia, or hematuria.
Physical exploration was normal, revealing just a little thickening of right spermatic cord. Laboratory evaluation was normal. Luteinizing hormone, follicle-stimulating hormone, total, and free testosterone were also unchanged.
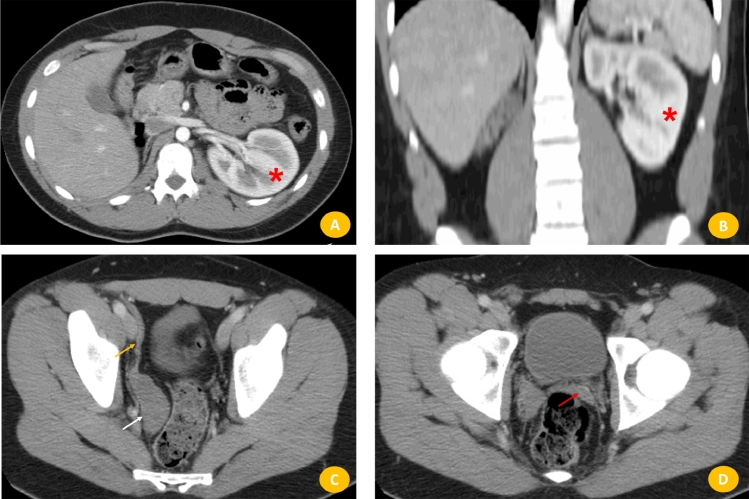
He brought a computerized tomography (CT) imaging from outside which revealed a homogeneous liquid mass with polylobed contours not taking contrast in retrovesical seat (Fig. 1), molding the posterior surface of the bladder, measuring 80 × 60 mm. The right kidney was absent, and the left vicariant kidney was shown. There is no lymphadenopathy iliac or pelvic effusion.
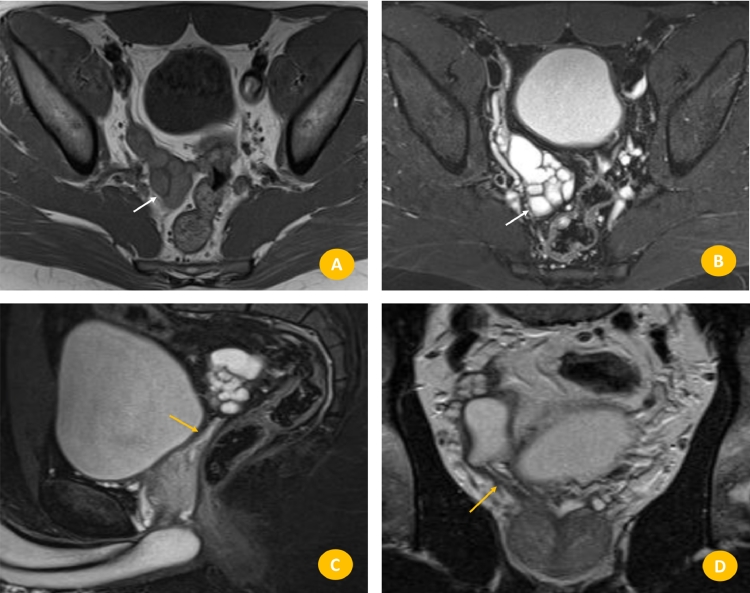
Fig. 2.
Pelvic MRI. (A and B) Axial T1- and T2-weighted MRI image showing dilated and cystic right seminal vesicle, which reveals hyperintensity in T1-weighted images (A). (C and D) Saggital and coronal T2-weighted MRI image with fat saturation showing enlargement of ejaculatory duct (orange arrow). (Color version of figure is available online.)
Fig. 1.
Abdominopelvic computerized tomography. (A and B) Axial and coronal CT-enhanced phase, reveal vicariant left kidney (*) and right kidney fossa empty. (C and D) Axial CT-enhanced phases reveal, seminal vesical asymmetric, right seminal vesicle is enlarged (white arrow) and efferent duct (orange arrow). Left seminal vesicle is normal morphology (red arrow). (Color version of figure is available online.)
To better characterize anatomic relationships of the seminal vesicle cyst the patient was submitted to a magnetic resonance imaging (MRI) scan which confirmed cystic–tubular retrovesical structures with T1 and T2 hyperintense content, and a fluid level suggesting proteinaceous or hematic content.
Knowing the influence of such syndrome in the fertility status, the patient was asked to undergo a semen analysis which was normal.
As patient was not planning to have children for the moment, so we kept him in a follow-up program, until the developing of complaints or clinical infertility. He was consulted 6 months after the treatment and remained asymptomatic.
Background
Seminal vesicle cysts were first identified in 1872 by Smith, while the association between renal unilateral agenesis and homolateral seminal vesicle cyst was described by Zinner only in 1914.
This syndrome comprises the triad of ipsilateral renal agenesis, cystic seminal vesicle, and ejaculator channel obstruction [1]. 200 cases of seminal vesicle cysts associated with ipsilateral renal agenesis have been reported in the literature [2].
While unilateral renal agenesis is observed in approximately 0.1% of adults, bilateral renal agenesis occurs in 1 in 3000 to 1 in 4000 of newborns.
This association derives from an anomalous development of the mesonephric or wolffian duct between 4 and 13 weeks of embryogenesis. Both the mesonephros and mesonephric duct develop during the fourth week, forming the primitive mesonephric renal corpuscle. In female this corpuscle involutes completely during the second month, whereas in males it persists partially, participating in the formation of the genital system.
The most caudal portion of the mesonephric duct, near the cloaca, forms an outgrowth, called the ureteric bud. This structure is vital in the cascade that will finally form the metanephros, definitive kidney.
In Zinner syndrome, the maldevelopment of the distal mesonephric duct and associated absence of the ureteric bud results in renal agenesis and atresia of the ejaculator duct. The gonad continues to develop, and insufficient drainage causes the characteristic cystic dilatations of the seminal vesicle.
The dilatations of the seminal vesicle tend to be small and asymptomatic. Cysts larger than 8 cm are associated with increased symptoms. Symptomatic cases usually present during the period of utmost sexual reproductive activity during the second or third decade of life, when these cysts increase in size.
Symptomatology described in the literature is varied and include voiding symptoms as dysuria, urinary frequency, urgency, but also hematuria, hypogastric, perineal or scrotal pain, epididymitis, painful ejaculation or defecation, and hematospermia
A high index of suspicion should be raised if a male patient presents symptoms of lower urinary tract and has renal unilateral agenesis [3].
Another important association is infertility (45% of cases), so fertility status should always be investigated in the presence of a Zinner's syndrome. It may be caused by ejaculatory duct obstruction, which results in a low ejaculatory volume, usually lesser than 1 ml, typically associated with azoospermia, alkaline pH, low concentration of carnitine and fructose in the seminal plasma, and high citrate level.
The diagnosis is based principally on imaging techniques, finding the characteristic cystic dilatations of the seminal vesicle and ipsilateral renal agenesis. The differential diagnosis is wide and includes mainly other causes of pelvic cysts, including true cysts of the prostate, prostatic utricle cysts, ejaculatory duct cysts, mullerian cysts, bladder diverticuli, and ureterocele. Other causes to consider are pelvic abscesses, hydronephrotic pelvic kidneys, and regional cystic neoplasms.
To the authors’ knowledge, no studies have analyzed the risk of malignant degeneration.
The diagnostic procedures to evaluate a patient with Zinner's syndrome may include blood analysis and endocrine profile (FSH, LH, testosterone), urinalysis and urine culture, renal and pelvic/transrectal ultrasonography, CT or MRI, sperm analysis and eventually cyst aspiration [4].
Transrectal ultrasonography is one of the most commonly recommended method for the diagnosis and initial evaluation of seminal vesicle cysts. Findings include an anechoic pelvic mass with a thick, irregular wall, and occasional wall calcifications, or the mass may contain internal debris reflecting prior hemorrhage or infection.
CT shows kidney agenesis and seminal vesicle cyst but may be insufficient to confirm the diagnosis.
MRI is the best technique in making the definitive diagnosis of seminal vesicle cysts without the need to resort to more invasive investigations. Typically, seminal vesicle cysts appear as T2-weighted signal hyperintensity structures and T1-weighted signal hypointensity structures. MRI scan gives excellent definition of the soft tissues and permits the best anatomic study with multiplanar demonstration of the relations between the surrounding pelvic structures and is recommendable to confirm the diagnosis and to do the planning of a surgical management.
Percutaneous fine-needle puncture may reconfirm the diagnosis by revealing spermatozoa.
The management of this syndrome should be clinically oriented and follow-up in asymptomatic and minimally symptomatic cases [5]. Antibiotics, transurethral aspiration of the seminal vesicle cyst or transurethral aspiration combined with substance instillation (alcohol and minocycline) are proposed as conservative treatment [6]. Invasive treatment should be restricted to symptomatic cases or patients who failed conservative measures and usually consists in seminal way disclosure through transurethral resection of the ejaculatory duct or balloon dilatation and open, laparoscopic or robotic vesiculectomy.
Conclusion
Seminal vesicle cysts combined with ipsilateral renal agenesis are a rare anomaly in the development of the urogenital system. These usually occur in males between the second to fourth decades of their life. The usual symptoms that are caused by the seminal vesicle cysts are bladder irritation and obstruction as well as pain in the perineum and scrotum. The diagnostic work-up consists of transrectal and abdominal ultrasonography, CT scan and MRI. For the removal of the seminal vesicle cyst there are techniques that are used nowadays due to advanced technologies such as open surgery and transurethral deroofing of the cyst.
Although Zinner syndrome is an infrequent condition, its characteristic presentation should be enough for the knowledgeable radiologist to be able to make a satisfactory diagnosis and contribute to its management.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.radcr.2018.08.012.
Appendix. Supplementary materials
References
- 1.Zinner A. Ein fall von intravesikaler samenblasenzyste. Weien Med Wschr. 1914;64:604–610. [Google Scholar]
- 2.Pereira BJ, Sousa L, Azinhais P, Conceição P, Borges R, Leão R. Zinner's syndrome: an up-to-date review of the literature based on a clinical case. Andrologia. 2009;41(5):322–330. doi: 10.1111/j.1439-0272.2009.00939.x. [DOI] [PubMed] [Google Scholar]
- 3.Beeby DI. Seminal vesicle cyst associated with ipsilateral renal agenesis: case report and review of literature. J Urol. 1974;112:120–122. doi: 10.1016/s0022-5347(17)59657-3. [DOI] [PubMed] [Google Scholar]
- 4.Levisay GL, Holder J, Weigel JW. Ureteral ectopia associated with seminal vesicle cyst and ipsilateral renal agenesis. Radiology. 1975;114(3):575–576. doi: 10.1148/114.3.575. [DOI] [PubMed] [Google Scholar]
- 5.King BF, Hattery RR, Lieber MM, Berquist TH, Williamson B, Jr., Hartman GW. Congenital cystic disease of the seminal vesicle. Radiology. 1991;178(1):207–211. doi: 10.1148/radiology.178.1.1984306. [DOI] [PubMed] [Google Scholar]
- 6.Williams RD, Sandlow JI. Surgery of the seminal vesicles. In: Walsh PC, Retik AB, Vaughan ED Jr., Wein AJ, editors. Campbell's urology. 7. Saunders; Philadelphia: 1998. pp. 3299–3307. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.