Abstract
Background
Movement disorder is common in Wilson's disease (WD), but there is no report on oromandibular dystonia (OMD). We report on frequency, severity, and MRI correlation of OMD in Wilson's disease with neurological manifestations (WDNM) and its response to treatment.
Methods
Consecutive WDNM patients were included and their clinical, hematological, serum chemistry, and MRI findings were noted. Neurological severity of WD and OMD were assessed. Burke‐Fahn‐Marsden (BFM) score for dystonia was noted. Patients were treated with penicillamine, zinc, and multiple antidystonic drugs. Clinical improvement at 3 and 6 months was noted.
Results
Overall, 61 of 67 (91%) WDNM patients had OMD, whose median age was 13.5 years. Median severity of OMD was 2.5 (range, 1–4). Thirteen patients were anarthric and 12 unable to eat. Severity of OMD correlated with drooling (r = 0.29; P = 0.02), BFM score (r = 0.63; P < 0.001), pancytopenia (r = −0.26; P = 0.04), and serum ceruloplasmin (r = 0.33; P = 0.01), but not with location and number of MRI lesions. Compared to baseline, severity of OMD improved at 6 months (P < 0.001), but not at 3 months. None became asymptomatic. Improvement in OMD paralleled with improvement in severity grade of WDNM (r = 0.26; P = 0.04) and with BFM score (r = 0.31; P = 0.02).
Conclusion
OMD was a common manifestation of WDNM occurring in 91% patients, and OMD improved partially over the study period.
Keywords: Wilson's disease, oromandibular dystonia, movement disorder, MRI, penicillamine, outcome, dystonia
Oromandibular dystonia (OMD) is a focal dystonia characterized by repetitive, sustained spasm of masticatory, lingual, and facial muscles, leading to involuntary jaw opening, closing, retraction, protrusion, or a combination of these movements.1 OMD may occur in isolation or in combination of limb or trunk dystonia resulting from various toxic, neurodegenerative, metabolic, infective, stroke, status epilepticus, postanoxic, post‐traumatic, primary faciobrachial, or generalized dystonia. In some patients, the cause could not be ascertained.1, 2 Movement disorder is a dominant feature in Wilson's disease (WD) with neurological manifestation (WDNM).3, 4 There is, however, a paucity of reports evaluating the pattern of OMD, its association with other movement disorders, and response to treatment. OMD is not only an esthetic concern, but also interferes with eating and speaking. MRI correlates of OMD in encephalitis have been reported.2 Dystonia has been postulated to loss of surround inhibition, which is a major function of basal ganglia.5, 6 Inhibitory control of globus pallidus (GP) interna on the thalamus may be released, which may be a result of corpus striatal or GP lesion.7, 8 The interruption in functioning of the thalamocortical connection has also been postulated as a mechanism of dystonia.9 In Japanese encephalitis (JE), dystonia has been attributed to the interruption of these anatomical connections.2 WD is a treatable hereditary metabolic disorder, and the location of MRI lesion is somewhat similar to JE.3, 4, 10, 11 It is likely that WDNM may also have OMD, but severity and response to treatment may not be similar to JE because JE is a monophasic disease and WD is an inherited disease with variable response to treatment.3, 12 In this communication, we report on the frequency and severity of OMD in WDNM, its MRI and biochemical correlation, and response to treatment.
Subjects and Methods
Consecutive WD patients with neurological manifestations attending to the neurology service of a tertiary care teaching institute during 2008–2014 were included. This is a retrospective analysis of data retrieved from a prospectively maintained neurological WD registry. Diagnosis of neurological WD was based on characteristic clinical findings, low serum ceruloplasmin (<20 mg/dL), Kayser‐Fleischer ring on slit‐lamp examination, and urinary excretion of copper (>40 μg/24 hours).13 The study was approved by the institute ethics committee. All patients were personally examined by two of the investigators (J.K. and U.K.M.). Patients with incomplete data and whose MRI scans were not available for review were excluded. The baseline MRI scan, which was done when they visited first to our institute, was analyzed. A detailed clinical history, including history of jaundice, age at onset, and duration of illness, was noted. A pedigree chart of the index patient was drawn. On examination, pallor, pedal edema, ascites, cataract, and organomegaly were noted. Severity of WDNM was based on activities of daily living (ADL) and sum score of five neurological signs, which included dysarthria, tremor, ataxia, rigidity/bradykinesia, and chorea/dystonia. Each neurological sign was given a score of 0 to 3 (0 = none and 3 = severe). Severity of WDNM was graded into grade 0: absent, grade I (mild, sum score 1); grade II (moderate, sum score of 2–7 and the patient was independent for ADL) and grade III (severe, sum score >7, dependent for ADL).14 Cognitive functions were evaluated by Mini–Mental State Examination (MMSE) scale and was considered abnormal based on population norms as well as age and education level.15 Presence of dystonia, its topographic involvement, and severity were noted. Severity of dystonia was assessed by Burke‐Fahn‐Marsden (BFM) score. Presence of OMD and its pattern were noted. Severity of OMD was graded on a 0 to 4 scale (0 = none, 1 = mild, 2 = moderate, 3 = severe, and 4 = markedly severe).2, 16 Muscle tone, tendon reflexes, cerebellar sign, and sensations of touch, vibration, joint position, and pin prick were noted.
Investigations
Patients were also evaluated for hematological, liver, and kidney involvement. Blood counts, hemoglobin, and international normalized ratio were done. Serum chemistry, including fasting and postprandial blood sugar, blood urea nitrogen, serum creatinine, bilirubin, serum glutamic‐pyruvic transaminase (SGPT), serum glutamic oxaloacetic transaminase, albumin, alkaline phosphatase (ALP), calcium, sodium, and potassium, were measured. Ultrasound abdomen was done and evidence of chronic liver disease, ascites, and organomegaly were noted. Cranial MRI was done using a 3T MRI machine (Signa GE Medical system; GE Healthcare, Waukesha, WI). T1, T2 and fluid‐attenuated inversion recovery (FLAIR) sequences were performed, and the location of abnormal signal changes was noted.
Treatment and Outcome
The patients were treated with penicillamine, zinc, or both. Penicillamine was started in a dose of 250 mg daily and increased gradually up to 250 mg thrice‐daily. Zinc sulphate was used in a dose of 50 mg thrice‐daily. They also received various antidystonic drugs, such as trihexyphenidyl, clonazepam, diazepam, or tetrabenazine, in isolation or in various combinations. Patients were followed up at 3 and 6 months or earlier, if indicated. During follow‐up, their clinical findings were noted, including severity of OMD and BFM score. Hematological and biochemical parameters were also repeated. If there was any deterioration post‐treatment, penicillamine was stopped and zinc continued.
Statistical Analysis
Severity of OMD was correlated with various clinical and biochemical parameters using Spearman's or Karl‐Pearson's correlation test to evaluate its relationship with hematological and kidney and liver dysfunction. Severity of OMD at baseline as well as 3 and 6 months were compared by analysis of variance. The variable was considered significant if the two‐tailed P value was less than 0.05. All statistical analysis was done using SPSS software (version 16; SPSS, Inc., Chicago, IL) and GraphPad software (Prism 5; GraphPad Software Inc., La Jolla, CA).
Results
There were 67 patients with WDNM and 61 (91%) of these had OMD. One patient with OMD had incomplete data; therefore, this study is based on 60 patients. Age ranged between 9 and 41 years (median, 13.5) and 12 were females. Median duration of illness was 19.5 months (range, 1–156). History of jaundice was present in 26 (43.3%) patients and 40 (66.7%) had affected siblings in their family. Twenty‐five (41.7%) patients had splenomegaly and 25 (41.7%) had hepatic dysfunction.
MMSE was possible in 44 patients, which ranged between 4 and 30 (median, 26), and 16 (26.7%) had MMSE score below 22. Muscle tone was increased in 47 (78.3%) patients, and tendon reflexes were exaggerated in 39 (65%). Cerebellar functions and sensations were normal. Severity grade of WDNM ranged between I and III (median, II).
OMD
Severity of OMD ranged between mild to markedly severe (median, 2.5). A majority of patients had moderate (22 patients) and severe (28 patients) OMD (see Video 1). Thirteen patients were anarthric, who had grade 3 or 4 OMD; 10 of them needed trick movement for feeding (see Video 2) and 2 needed nasogastric feeding. Involvement of lingual muscles and muscles of mastication resulted in more disability in feeding and speaking. All had a vacuous smile, which may be owing to involvement of facial muscles. There was no jaw retraction, protrusion, or lateral deviation. OMD was associated with various other movement disorders, including limb, trunk, or neck dystonia in 58 (96.7%). BFM score ranged between 4 and 108 (median, 47). Choreoathetosis was present in 20 (33.2%) patients, myoclonus in 7 (11.7%), and tremor in 26 (43.3%).
Cranial MRI was done in 51 patients and was abnormal in 50. Abnormal signal changes were noted in corpus striatum in 45 (75%) patients, GP in 30 (50%), thalamus in 29 (48.3%), brain stem in 26 (43.3%), cerebellum in 2 (3.3%), subcortical white matter in 10 (16.7%), and cortical involvement in 11 (18.3%). Basal ganglia and thalamic lesions were bilateral, whereas lesions in other locations were asymmetrical or unilateral. These lesions were usually hyperintense on T2 and FLAIR sequence.
Correlation
Severity of OMD correlated significantly with drooling (r = 0.29; P = 0.02), BFM score (r = 0.63; P < 0.001), severity grade of WDNM (r = 0.718; P < 0.001), pancytopenia (r = −0.26; P = 0.04), and serum ceruloplasmin (r = 0.33; P = 0.01). Details are shown in Figure 1. Severity of OMD, however, did not significantly correlate with age (r = −0.17; P = 0.20), duration of illness (r = 0.02; P = 0.82), MMSE score (r = −0.02; P = 0.92), hemoglobin (r = −0.14; P = 0.29), leucocyte count (r = −0.16; P = 0.21), platelet count (r = −0.002; P = 1.0), SGPT (r = −0.12; P = 0.41), serum calcium (r = −0.17; P = 0.21), ALP (r = 0.13; P = 0.34), and albumin (r = 0.04; P = 0.75). The location of MRI lesions, such as thalamus (r = −0.05; P = 0.73), putamen (r = −0.04; P = 0.76), GP (r = 0.19; P = 0.17), brainstem (r = −0.09; P = 0.53), cerebellum (r = 0.02; P = 0.86), and number of MRI lesions (r = 0.06; P = 0.67) were also not significantly correlated with severity of OMD.
Figure 1.

Severity of OMD in WD significantly correlated with drooling, BFM score, pancytopenia, and serum ceruloplasmin level.
Follow‐up
Severity of OMD did not reduce significantly at 3 months, compared with baseline (2.40 ± 0.76 vs. 2.34 ± 0.69; nonsignificant). Severity of OMD at 6 months (1.78 ± 0.74), however, was reduced significantly, compared with baseline (P < 0.001) and 3 months (P < 0.001; Figs. 2, 3, 4). At 6 months, 8 (13.3%) patients had a 1‐grade improvement in OMD severity from baseline, 14 (23.3%) had 2‐grade improvement, and 1 (1.7%) had a more than 2‐grade improvement. None of the patients, however, were free from OMD. Details are shown in Table 1. Improvement in OMD paralleled with improvement in severity grade of WDNM (r = 0.26; P = 0.04) and BFM score (r = 0.31; P = 0.02; Fig. 5). Thirty‐one (51.7%) patients were on penicillamine and zinc, 23 (38.3%) on penicillamine, and 6 (10%) were on zinc. Within 3 months, 21 (35%) patients had deterioration for which penicillamine had to be stopped; however, they continued zinc therapy. For movement disorders, 51 patients received trihexyphenidyl (6–36 mg), 20 clonazepam (0.5–2.0 mg), 9 diazepam (4–30 mg), and 25 tetrabenazine (25–75 mg). Eighteen of these patients received multiple drugs.
Figure 2.

Error bar diagram shows severity of OMD at different time points.
Figure 3.
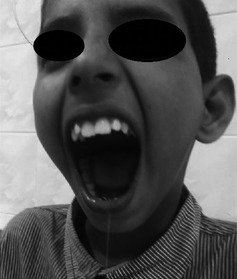
Fourteen‐year‐old boy with severe OMD and drooling resulting from WD.
Figure 4.

MRI of the same patient in T2 (A, B, D, and F) and DWI (C and E) shows (A) corpus striatal and thalamic hyperintensity, (B) SN hyperintensity, (C and D) midbrain hyperintensity in T2 and DWI, and (E and F) pontine hyperintensity in DWI and T2 sequence.
Table 1.
Number of neurological WD patients with different severity of OMD at different time points
| Severity of OMD | Baseline, N (%) | 3 Months, N (%) | 6 Months, N (%) |
|---|---|---|---|
| Mild | 8 (13.3) | 7 (11.7) | 25 (41.7) |
| Moderate | 22 (36.7) | 24 (40) | 24 (40) |
| Severe | 28 (46.7) | 29 (48.3) | 11 (18.3) |
| Markedly severe | 2 (3.3) | 0 (0) | (0) |
Figure 5.

Improvement in OMD at 6 months from baseline significantly correlated with improvement in BFM score and severity grade of WD. Graph shows difference of 6 mo score from baseline.
Discussion
In the present study, OMD was the dominant feature in WDNM, occurring in 91% patients. Severity of OMD correlated with drooling, severity of WDNM, BFM score, leucocyte count, pancytopenia, and liver dysfunction. Severity of OMD at 6 months was reduced in 60% patients, although none became asymptomatic. Severe OMD was difficult to treat and needed multiple drugs. This study, for the first time, reports the frequency, pattern, and severity of OMD in WDNM, its correlation with clinical, hematological, hepatic, and kidney dysfunction, and response to treatment. Drooling and vacuous smile have been described as characteristic clinical features of WD. These features may suggest OMD. Dystonia of lingual muscles and muscles of mastication may result in drooling, and dystonia of facial muscles may result in vacuous smile. Variable frequency of drooling (30%–68%), dysarthria (62%–92%), dystonia (36%–96%), tremor (47%–91%), and choreoathetosis (10%–24%) have been reported in WDNM.4, 17, 18, 19, 20 None of these studies, however, comprehensively evaluated the severity, pattern, and response to treatment. Higher frequency of OMD and movement disorder in our study may be owing to higher proportion of patients with moderate‐to‐severe severity and late reporting. A study from Eastern India also reported dystonia in 96%, silly smile in 92%, and dysarthria in 80% patients.20 In our study, none of the MRI lesions correlated with severity of OMD, which may be the result of frequent involvement of basal ganglia, thalamus, and brainstem in WDNM. In a study on WDNM, the putamen was involved in 72%, caudate in 61%, thalamus in 58%, and midbrain in 49% patients.4 Corpus striatal lesion has been reported to result in choreoathetosis, pallidal lesion to dystonia, thalamic lesion to dystonia, and brainstem lesion to OMD.2, 21 In the present study, brainstem, however, was involved in 43.3% patients only. More recently, impaired surrounding inhibition of basal ganglia and impaired thalamocortical connections have been attributed to dystonia.2, 5, 6 Functional MRI and PET might have revealed some information to understand the mechanism of OMD. We, however, have not done functional MRI (fMRI) and PET in our patients.18F‐fluorodopa PET study revealed reduced uptake in the striatum, indicating loss of the dopaminergic nigrostriatal pathway.22 fMRI is helpful in detecting white matter connection abnormalities between basal ganglia nuclei and cortex to understand the postulated mechanism of dystonia in WDNM. Diffusion tensor imaging in WD revealed frequent lobar white mater lesion and thalamic abnormality, compared to conventional MRI.23, 24 FLAIR sequence is more sensitive in revealing abnormality, compared to diffusion‐weighted imaging (DWI).25 MR spectroscopy in WDNM revealed reduced N‐acetylaspartate/creatine and increased myoinsitol/creatine ratio in basal ganglia, compared to controls.26 Infective and metabolic brain disease may not be an appropriate model for localization of movement disorder. A similar observation has also been reported in encephalitis, in which 17 of 209 patients had OMD. All but 3 were the result of JE, and their MRI revealed thalamic lesion in 9 patients, SN in 10, caudate in 3, GP and putamen in 2 each, and pons in 1. At 6 months, OMD improved completely in 6 patients, by 1 grade in 2, and remained static in 7.2 In the present study, none of the WD patients were free of OMD, although severity of OMD improved significantly at 6 months. WD is a hereditary metabolic disease, whereas JE is a monophasic illness. In JE, there is progressive improvement both at 3 and 6 months, but improvement in WDNM was not significant at 3 months, but 60% improved to some extent at 6 months. The lack of significant improvement at 3 months was owing to neurological worsening after chelating treatment in WD. Thirty‐five percent of our patients had deterioration with penicillamine treatment. In WDNM, treatment‐related deterioration has been reported in up to 50% of patients, especially after chelating agents.3, 12 In a study from the United States, neurodegenerative diseases were the cause of OMD in 1.8% of patients. The other causes of OMD were drug induced in 22.8%, peripheral causes in 9.3%, post‐traumatic in 2.5%, head injury in 0.8%, and no cause could be ascertained in 63%.27 OMD has also been reported in critically ill patients. In a study on 165 critically ill neurological patients, 5 had OMD, 14 cervical dystonia, and 2 had both. Spontaneous improvement occurred in 7 of 11 survived patients. Four patients received botulinum toxin (BoTN) injection.28 None of our patients received BoTN because almost all had generalized dystonia. Severity of OMD correlated with pancytopenia and 41% patients had liver dysfunction, which reflects that manifestation of WD is a generalized phenomenon with predominant liver damage at the early stage, and the surviving patients may manifest with hepatolenticular degeneration. The ATP7B gene was expressed mostly in the liver and other visceral organs and helps in transporting copper from cells. Impairment of these functions results in accumulation of copper in the respective organs. In brain, transport of copper from the astrocyte to neurons is primarily mediated by ATP7A. In an experimental study on milk mice, a genetic model of WD, expression of ATP7A in the choroid plexus was increased.29 This may facilitate increased copper availability to neurons, resulting in brain damage. Mutation of ATP7A results in Menkes disease, in which neurons suffer from copper deficiency as a result of impaired transport of copper from astrocyte to the neurons.30 Further studies are needed to evaluate the effect of ATP7B mutation on ATP7A activity, which may elucidate the mechanism of neuronal injury in WD.
The present study is limited by retrospective analysis of prospectively maintained data, heterogeneous disease duration, and treatment protocol. We have not done global score, but have done hematological, liver, and kidney involvement separately by appropriate investigations. The strength of this study is the large database of relatively rare disease from a single center and all the patients were personally examined by two of the investigators.
From this study, it can be concluded that OMD occurs in more than 90% patients with neurological WD and 60% of these patients improve by 6 months post‐treatment. Further studies are needed to understand the basis of OMD and its treatment.
Author Roles
(1) Research Project: A. Conception, B. Organization, C. Execution; (2) Statistical Analysis: A. Design, B. Execution, C. Review and Critique; (3) Manuscript Preparation: A. Writing of the First Draft, B. Review and Critique.
J.K.: 1A, 1B, 1C, 3A, 3B
A.R.: 2A, 2B, 2C
U.K.M.: 3A
Disclosures
Funding Sources and Conflicts of Interest: The authors report no sources of funding and no conflicts of interest.
Financial Disclosures for previous 12 months: The authors declare that there are disclosures to report.
Supporting information
A video accompanying this article is available in the supporting information here.
Video 1. A child with WD with severe (grade III) generalized dystonia including grade 4 OMD at baseline. At 3 months post‐treatment, he improved significantly in limb and axial dystonia, but still had grade 3 OMD.
Video 2. A girl with WD having generalized dystonia and severe OMD. She used a trick maneuver for feeding herself.
Acknowledgments
The authors thank Mr. Rakesh Kumar Nigam and Deepak Kumar Anand for secretarial help.
Relevant disclosures and conflicts of interest are listed at the end of this article.
References
- 1. Balasubramaniam R, Ram S. Orofacial movement disorders. Oral Maxillofac Surg Clin North Am 2008;20:273–285. [DOI] [PubMed] [Google Scholar]
- 2. Kalita J, Misra UK, Pradhan PK. Oromandibular dystonia in encephalitis. J Neurol Sci 2011;304:107–110. [DOI] [PubMed] [Google Scholar]
- 3. Kalita J, Kumar V, Chandra S, Kumar B, Misra UK. Worsening of Wilson disease following penicillamine therapy. Eur Neurol 2014;71:126–131. [DOI] [PubMed] [Google Scholar]
- 4. Sinha S, Taly AB, Ravishankar S, Prashanth LK, Venugopal KS, Arunodaya GR, et al. Wilson's disease: cranial MRI observations and clinical correlation. Neuroradiology 2006;48:613–621. [DOI] [PubMed] [Google Scholar]
- 5. Sohn YH, Hallett M. Disturbed surround inhibition in focal hand dystonia. Ann Neurol 2004;56:595–599. [DOI] [PubMed] [Google Scholar]
- 6. Mink JW. The basal ganglia: focused selection and inhibition of competing motor programs. Prog Neurobiol 1996;50:381–425. [DOI] [PubMed] [Google Scholar]
- 7. Burton K, Farrell K, Li D, Calne DB. Lesions of the putamen and dystonia: CT and magnetic resonance imaging. Neurology 1984;34:962–965. [DOI] [PubMed] [Google Scholar]
- 8. Münchau A, Mathen D, Cox T, Quinn NP, Marsden CD, Bhatia KP. Unilateral lesions of the globus pallidus: report of four patients presenting with focal or segmental dystonia. J Neurol Neurosurg Psychiatry 2000;69:494–498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Marsden CD, Obeso JA, Zarranz JJ, Lang AE. The anatomical basis of symptomatic hemidystonia. Brain 1985;108:463–483. [DOI] [PubMed] [Google Scholar]
- 10. Kalita J, Misra UK, Pandey S, Dhole TN. A comparison of clinical and radiological findings in adults and children with Japanese encephalitis. Arch Neurol 2003;60:1760–1764. [DOI] [PubMed] [Google Scholar]
- 11. Kalita J, Misra UK. Markedly dystontonia in Japanese encephalitis. Mov Disord 2000;15:1168–1172. [DOI] [PubMed] [Google Scholar]
- 12. Brewer GJ, Terry CA, Aisen AM, Hill GM. Worsening of neurologic syndrome inpatients with Wilson's disease with initial penicillamine therapy. Arch Neurol 1987;44:490–493. [DOI] [PubMed] [Google Scholar]
- 13. Roberts EA, Schilsky ML; American Association for Study of Liver Diseases (AASLD) . Diagnosis and treatment of Wilson disease: an update. Hepatology 2008;47:2089–2111. [DOI] [PubMed] [Google Scholar]
- 14. Grimm G, Prayer L, Oder W, et al. Comparison of functional and structural brain disturbances in Wilson's disease. Neurology 1991;41:272–276. [DOI] [PubMed] [Google Scholar]
- 15. Crum RM, Anthony JC, Bassett SS, Folstein MF. Population‐based norms for the Mini‐Mental State Examination by age and educational level. JAMA 1993;269:2386–2391. [PubMed] [Google Scholar]
- 16. Fahn S. Assessment of primary dystonia In: Munset TL, ed. Quantification of Neurologic Deficit. Boston: Butterworth; 1989:241–270. [Google Scholar]
- 17. Rodrigo Agudo JL, Valdés Mas M, Vargas Acosta AM, Ortiz Sánchez ML, Gil del Castillo ML, Carballo Alvarez LF, et al. Clinical presentation, diagnosis, and long‐term outcome of 29 patients with Wilson's disease. Rev Esp Enferm Dig 2008;100:456–461. [DOI] [PubMed] [Google Scholar]
- 18. Machado A, Chien HF, Deguti MM, Cançado E, Azevedo RS, Scaff M, et al. Neurological manifestations in Wilson's disease: report of 119 cases. Mov Disord 2006;21:2192–2196. [DOI] [PubMed] [Google Scholar]
- 19. Noureen N, Rana MT. Neurological Wilson disease in children: a three years' experience from Multan. J Pak Med Assoc 2011;61:743–748. [PubMed] [Google Scholar]
- 20. Sinha S, Jha DK, Sinha KK. Wilson's disease in Eastern India. J Assoc Physicians India 2001;49:881–884. [PubMed] [Google Scholar]
- 21. Bhatia KP, Marsden CD. The behavioural and motor consequences of focal lesions of the basal ganglia in man. Brain 1994;117:859–876. [DOI] [PubMed] [Google Scholar]
- 22. Snow BJ, Bhatt M, Martin WR, Li D, Calne DB. The nigrostriatal dopaminergic pathway in Wilson's disease studied with positron emission tomography. J Neurol Neurosurg Psychiatry 1991;54:12–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Jadav R, Saini J, Sinha S, Bagepally B, Rao S, Taly AB. Diffusion tensor imaging (DTI) and its clinical correlates in drug naïve Wilson's disease. Metab Brain Dis 2013;28:455–462. [DOI] [PubMed] [Google Scholar]
- 24. Li G, Zhou X, Xu P, Pan X, Chen Y. Microstructure assessment of the thalamus in Wilson's disease using diffusion tensor imaging. Clin Radiol 2014;69:294–298. [DOI] [PubMed] [Google Scholar]
- 25. Favrole P, Chabriat H, Guichard JP, Woimant F. Clinical correlates of cerebral water diffusion in Wilson disease. Neurology 2006;66:384–389. [DOI] [PubMed] [Google Scholar]
- 26. Lucato LT, Otaduy MC, Barbosa ER, et al. Proton MR spectroscopy in Wilson disease: analysis of 36 cases. AJNR Am J Neuroradiol 2005;26:1066–1071. [PMC free article] [PubMed] [Google Scholar]
- 27. Gandhi YR. Oro‐mandibular dystonia. Natl J Maxillofac Surg 2010;1:150–152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Lo SE, Rosengart AJ, Novakovic RL, Kang UJ, Shah DN, Khan MA, et al. Identification and treatment of cervical and oromandibular dystonia in acutely brain‐injured patients. Neurocrit Care 2005;3:139–145. [DOI] [PubMed] [Google Scholar]
- 29. Chen DB, Feng L, Lin XP, Zhang W, Li FR, Liang XL, et al. Penicillamine increases free copper and enhances oxidative stress in the brain of toxic milk mice. PLoS One 2012;7:e37709. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Pase L, Voskoboinik I, Greenough M, Camakaris J. Copper stimulates trafficking of a distinct pool of the Menkes copper ATPase (ATP7A) to the plasma membrane and diverts it into a rapid recycling pool. Biochem J 2004;378:1031–1037. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
A video accompanying this article is available in the supporting information here.
Video 1. A child with WD with severe (grade III) generalized dystonia including grade 4 OMD at baseline. At 3 months post‐treatment, he improved significantly in limb and axial dystonia, but still had grade 3 OMD.
Video 2. A girl with WD having generalized dystonia and severe OMD. She used a trick maneuver for feeding herself.


