Abstract
Background
Emergency department (ED) attendance for older people towards the end of life is common and increasing, despite most preferring home-based care. We aimed to review the factors associated with older people’s ED attendance towards the end of life.
Methods
Systematic review using Medline, Embase, PsychINFO, CINAHL and Web of Science from inception to March 2017. Included studies quantitatively examined factors associated with ED attendance for people aged ≥65 years within the last year of life. We assessed study quality using the QualSyst tool and determined evidence strength based on quality, quantity and consistency. We narratively synthesized the quantitative findings.
Results
Of 3824 publications identified, 21 were included, combining data from 1 565 187 participants. 17/21 studies were from the USA and 19/21 used routinely collected data. We identified 47 factors and 21 were included in the final model. We found high strength evidence for associations between ED attendance and palliative/hospice care (adjusted effect estimate range: 0.1–0.94); non-white ethnicity (1.03–2.16); male gender (1.04–1.83, except 0.70 in one sub-sample) and rural areas (0.98–1.79). The final model included socio-demographic, illness and service factors, with largest effect sizes for service factors.
Conclusions
In this synthesis, receiving palliative care was associated with lower ED attendance in the last year of life for older adults. This has implications for service models for older people nearing the end of life. However, there is limited evidence from European countries and none from low or middle-income countries, which warrants further research.
Introduction
Most older people who are approaching the end of life prefer to be cared for and die in their usual place of care,1 remaining in familiar surroundings with family nearby and autonomy preserved.2 However, half of people aged 65 years and over in the USA attend the emergency department (ED) in the month before death.3 Trends in the UK show that ED attendances in the last year of life are increasing.4 Unplanned transitions to hospital may enable timely access to health care services, but are often distressing and associated with poor outcomes. Approximately 70% of ED visits in the last months of life end in hospital admission.3 Hospitalization exposes patients to iatrogenic complications, such as hospital-acquired delirium (prevalence 6–56%)5 and medication errors (median prevalence 18%)6 and increases the chance of in-hospital death.
Older people, while representing a heterogeneous population group, are characterized by clinical and social factors that increase their risk of poor care at the end of life.7 Living to advanced age is associated with presence of multiple chronic conditions, frailty and unpredictable illness trajectories.8 This presents challenges for the care of older people, such as polypharmacy, symptom management9 and uncertainty around initiating advance care planning.10 Social isolation and neglect are also more common for people at older ages, which influence health service use.11
From a public health perspective, a focus on older people’s ED utilization towards the end of life is important and timely, given that hospital utilization rises exponentially towards death,12 and the population of older people reaching the end of life is increasing. The global population aged over 65 years is projected to more than double to 1.6 billion in the next 30 years,13 presenting one of the major public health challenges of the century.14 ED attendance and subsequent inpatient hospital care accounts for the highest expenditure in end of life healthcare,15 while many people prefer home-based care.1 It is therefore timely to understand older adults’ ED use towards the end of life to optimize care provision for current and future populations.
The factors associated with ED attendance in the months preceding death for older people with non-cancer conditions have never been synthesized. A review focussed on cancer patients found that male gender, black ethnicity, lung cancer and low socioeconomic status were associated with ED attendances at the end of life.16 However, as people live into advanced age there is increased prevalence of chronic non-malignant disease and multi-morbidity17 with different end of life trajectories and health care use.8 This limits generalization of findings from patients with cancer to those with non-cancer conditions. We aimed to review factors associated with ED attendance for people aged 65 years and over within the last year of life to identify opportunities to improve end of life care.
Methods
Design
Systematic review following the PRISMA statement and based on a pre-agreed protocol. The review was guided by well-established theory on determinants of health service use18 and of place of care at the end of life.19 Andersen’s behavioural theory posits that an individual’s use of services is a function of ‘pre-disposing’, ‘enabling’ and ‘need’ factors, at individual and contextual levels.18 Gomes and Higginson’s model applied these theoretical principles to determinants of place of care at the end of life, categorizing factors as demographic, illness, and environment.19
Eligibility criteria
Inclusion criteria
Population aged 65 years and over (at least 90% of the sample aged >65 years, or mean age of 70+ years where age range not provided); examination of one or more factors associated with outcome of ED attendance within the last year of life (including any time-period before death).
Exclusion criteria
Case series, case reports and qualitative study designs. Studies examining cancer patients only were excluded, because of limited generalizability from cancer populations to non-cancer populations and to allow for comparison of findings with a review on cancer patients’ ED attendance towards the end of life.16
Data sources
We searched electronic databases (Medline, Embase, PsychINFO, CINAHL and Web of Science) from inception to March 2017, with no restrictions on time or language. We searched reference lists from included and relevant studies, and articles citing these studies. We also sought to identify grey literature by searching websites of key not for profit organizations (Nuffield Trust, The King’s Fund) and charitable organizations relating to end of life care (Marie Curie, Macmillan).
Search strategy and study selection
Prior scoping in Medline and Embase ensured optimal sensitivity and specificity of the search terms (Supplementary tables S1–S5). Search results were screened initially by title and abstract, and then full text. We screened against the stated eligibility criteria at both stages. Articles for which there was uncertainty were double reviewed (A.E.B. and S.N.E.), with disagreements discussed and resolved within the research team.
Data extraction
One reviewer (A.E.B.) extracted data according to a pre-agreed pro-forma and a 20% random sample was independently assessed for accuracy (S.N.E.). We extracted information on study design, setting, participant eligibility, population characteristics, sample size, outcome definition, statistical analysis, explanatory variables and effect sizes with confidence intervals (CIs). Unadjusted estimates were recorded only when no adjusted estimates were available.
Quality assessment
We assessed study quality using the validated tool QualSyst, which is flexible to study design.20 The assessment includes 14 criteria, each scored from 0 to 2. Percentage of the total possible score indicates quality grade: <50% low; ≥50 and <70% medium; and ≥70% high (Supplementary table S6). A second author (S.N.E.) assessed a random 10% sample. Scores that diverged by >10% were discussed within the research team.
Strength of evidence
We assessed the strength of evidence for each factor using an adapted existing algorithm 19 based on the quality, quantity and consistency of evidence (Supplementary figure S1). We independently double-assessed (A.E.B. and S.N.E.) the strength of evidence for each factor, rating each as high, moderate, low or very low.
Data synthesis
Based on the underpinning models, we grouped factors as (i) socio-demographic and pre-disposing factors (e.g. gender); (ii) illness-related and need factors (.e.g. diagnoses) and (iii) service-related and enabling factors (e.g. healthcare received).18,19 We converted estimates of effect to odds ratios where possible and graphically presented adjusted estimates only, including odds ratios, risk ratios and rate ratios. We carried out a narrative synthesis of the quantitative data, reporting the range of point estimates for adjusted estimates only. Pooling estimates using meta-analysis was considered. We developed a theoretical model of ED attendance of older people in the last year of life underpinned by the principles of existing theoretical models,18,19 excluding factors with very low strength evidence.
Results
Characteristics of included studies
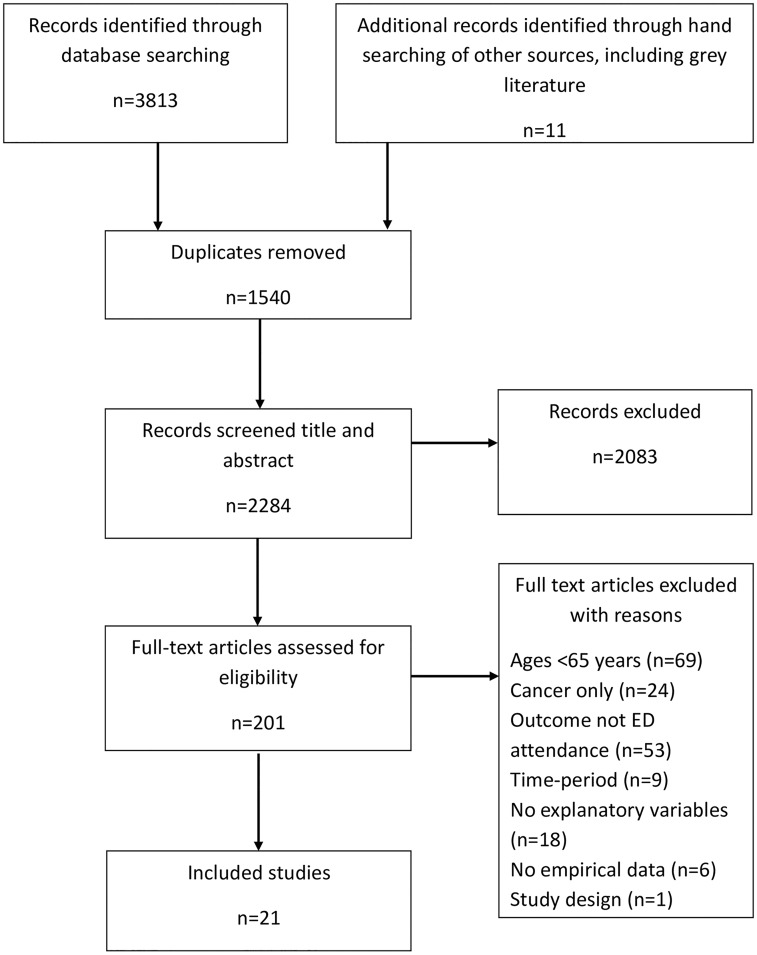
We identified 3824 articles (figure 1) Following full-text screening (n = 201) and double-review where there was uncertainty (n = 33), 21 articles were included with a combined sample of 1 565 187 participants (table 1). Of the 21 included studies, 17 were from the USA, three from Europe and one from Australia. Just under half of the studies were rated as high quality (n = 10) while the remaining were medium (n = 8) or low (n = 3) (Supplementary table S6). Most used routinely collected population-based data, with retrospective analysis (table 1, Supplementary table S7). Four studies examined interventions relating to palliative care;21–24 however, none used experimental designs. Four studies examined nursing home residents only,23,25–27 and one study stratified findings by nursing home and community.28 Four studies focussed on single non-cancer conditions (dementia29–31 and heart failure32).
Figure 1.
PRISMA Flow diagram of study selection
Table 1.
Summary of characteristics of included studies
| Study characteristic | Number of studies (n = 21) | Study references (first author, year)a |
|---|---|---|
| Study setting | ||
| North America | 17 | Aldridge, 2016; Bischoff, 2013; Brumley, 2003; Cheung, 2013; Davis, 2016; Feng, 2014; Lustbader, 2017; Miller, 2015; Miller, 2016; Mitchell, 2004; Nakashima, 2016; Setoguchi, 2010; Smith, 2012; Stevenson, 2013; Unroe, 2012; Volicer, 2003; Wang, 2016. |
| Australia | 1 | Rosenwax, 2015. |
| Europe | 3 | Purdy, 2015; Morin, 2014; Sleeman, 2017. |
| Publication year | ||
| 2016–17 | 7 | Aldridge, 2016; Davis, 2016; Lustbader, 2017; Miller, 2016; Nakashima, 2016; Sleeman, 2017; Wang, 2016. |
| 2011–15 | 10 | Bischoff, 2013; Cheung, 2013; Feng, 2014; Miller, 2015; Morin, 2014; Purdy, 2015; Rosenwax, 2015; Smith, 2012; Stevenson, 2013; Unroe, 2012. |
| 2001–10 | 4 | Brumley, 2003; Mitchell, 2004; Setoguchi, 2010; Volicer, 2003. |
| Study population diagnoses | ||
| Mixed diagnoses | 17 | Aldridge, 2016; Bischoff, 2013; Brumley, 2003; Cheung, 2013; Davis, 2016; Feng, 2014; Lustbader, 2017; Miller, 2015; Miller, 2016; Morin, 2014; Nakashima, 2016; Purdy, 2015; Rosenwax, 2015; Setoguchi, 2010; Smith, 2012; Stevenson, 2013; Wang, 2016. |
| Dementia only | 3 | Mitchell, 2004; Sleeman, 2017; Volicer, 2003. |
| Heart failure only | 1 | Unroe, 2012. |
| Study population care setting | ||
| Mixed | 17 | Aldridge, 2016; Bischoff, 2013; Brumley, 2003; Cheung, 2013; Davis, 2016; Feng, 2014; Lustbader, 2017; Mitchell, 2004; Purdy, 2015; Rosenwax, 2015; Setoguchi, 2010; Smith, 2012; Sleeman, 2017; Stevenson, 2013; Unroe, 2012; Volicer, 2003; Wang, 2016. |
| Care home or long-term care facility | 4 | Miller, 2015; Miller, 2016; Morin, 2014; Nakashima, 2016. |
| Time-period prior to death | ||
| ≤1 month | 7 | Bischoff, 2013; Lustbader, 2017; Smith, 2012; Miller, 2016; Morin, 2014; Purdy, 2015; Setoguchi, 2010. |
| >1 month and ≤3 months | 4 | Miller, 2015; Mitchell, 2004; Nakashima, 2016; Volicer, 2003. |
| >3 months and ≤6 months | 1 | Wang, 2016. |
| >6 months and ≤12 months | 5 | Davis, 2016; Feng, 2014; Rosenwax, 2015; Sleeman, 2017; Stevenson, 2013. |
| From hospice enrolment to death | 4 | Aldridge, 2016; Brumley, 2003; Cheung, 2013; Unroe, 2012. |
| Outcome of interest | ||
| Proportion any ≥1 ED visit | 12 | Aldridge, 2016; Cheung, 2013; Feng, 2014; Miller 2015; Morin, 2014; Mitchell, 2004; Purdy, 2015; Setoguchi, 2010; Sleeman, 2017; Smith, 2012; Unroe, 2012; Volicer, 2003. |
| Proportion any >1 ED visit | 1 | Bischoff, 2013. |
| Proportion ≥1 ED visit without admission | 2 | Miller, 2016; Nakashima, 2016. |
| Proportion ≥1 ED visit with admission | 1 | Wang, 2016. |
| Mean number of any ED visits | 1 | Brumley, 2003. |
| Mean number of ED visits without admission | 1 | Davis, 2016. |
| Daily rate of any ED use | 1 | Rosenwax, 2015. |
| Any ED visits per 1000 decedents | 2 | Lustbader, 2017; Stevenson, 2013. |
| Study quality | ||
| High | 10 | Aldridge, 2016; Bischoff, 2013; Feng, 2014; Miller, 2016; Mitchell, 2004; Nakashima, 2016; Purdy, 2015; Rosenwax, 2015; Sleeman, 2017; Smith, 2012. |
| Medium | 8 | Brumley, 2003; Cheung, 2013; Davis, 2016; Miller, 2015; Setoguchi, 2010; Stevenson, 2013; Unroe, 2012; Wang, 2016. |
| Low | 3 | Lustbader, 2017; Morin, 2014; Volicer, 2003. |
aAll references for included studies are presented in Supplementary table S6.
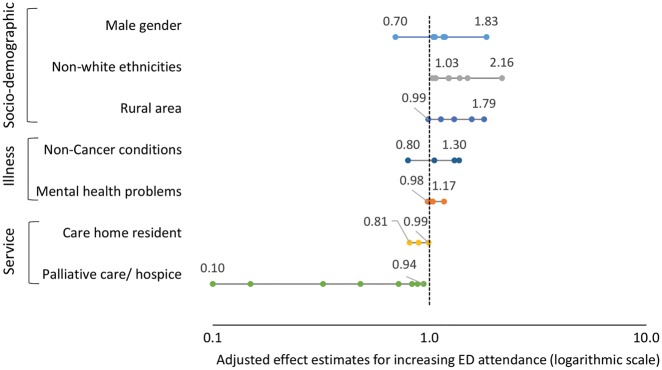
Most studies defined the outcome as the proportion of people attending the ED, including those with and without a subsequent admission, while some focussed on only attendances with33 or without admission.23,27 Variation in definitions of the end of life time-period, and explanatory factors complicated the comparison across studies. Additionally, heterogeneity in populations and a mix of estimate measures (odds ratios and rate ratios) precluded pooling of estimates (Supplementary tables S7 and S8). Figure 2 presents the range of adjusted effect estimates for factors with high or moderate evidence. For further details, Supplementary figure S2 presents a forest plot of effect estimates with 95% CIs for selected variables, without quantitative synthesis.
Figure 2.
Adjusted effect estimates for socio-demographic, illness and service factors with high and moderate strength of evidence. Numbers detail minimum and maximum adjusted effect estimates for each factor
Socio-demographic factors
We found high strength evidence that men were more likely to attend ED than women in the last year of life.3,28,31,34,35 In five of the six samples (all high-quality studies), men were more likely to attend ED, four significantly so with adjusted odds ratios (AORs) ranging from 1.04 to 1.83. Conversely, for one sample, community-dwelling men with dementia were less likely to attend than women (AOR 0.70). There was high strength evidence that Black, Asian and Minority Ethnic people were more likely to attend ED (versus white ethnicity), with a stronger effect observed for black ethnicity. Four high-quality studies3,28,31,34 and one medium quality32 examined this relationship; AORs ranged from 1.03 to 2.16. In four of the five high-quality studies reporting the effect of age, older age was associated with reduced likelihood of attending ED (moderate evidence), however these findings were mostly non-significant.3,28,31,34,35 We found high strength evidence that rurality increased the likelihood of ED attendance from four high-quality studies3,28,34,35; AORs ranged from 1.57 to 1.79.
Education (one study, overall very low strength evidence)28 and income (two studies, overall low strength evidence)3,28 were rarely assessed, but no associations with ED attendance were reported. Two high-quality studies investigated marital status28,35 finding that people living in the community with a partner were more likely to attend ED (low strength evidence).
Service-related factors
Six studies investigated associations between receipt of community palliative care21–23,35 or hospice care3,33 or its timing, and ED attendance in the last year of life, including three high-quality studies. All studies found lower ED attendance in the palliative/hospice care group, with AORs ranging from 0.1 to 0.94 (high strength evidence). Three studies specifically investigated timing of palliative or hospice care, finding that early referral reduced ED attendance. Wang et al.33 found that late hospice enrolment (≤7 days before death) was associated with higher ED use compared to no hospice (AOR 1.23, 95% CI, 1.12–1.26), while medium (8–179 days) and long length (>180 days) enrolment was associated with reduced ED use (AOR 0.88, 95% CI 0.82–0.95; AOR 0.83, 95% CI 0.72–0.96, respectively).
Three high-quality studies presented the effect of being in a care home on ED attendance (AORs 0.89–0.99).3,30,31 Overall, we found moderate strength of evidence for no effect. The relationship between advance care planning and ED attendance was examined in two high-quality studies,3,36 both finding non-significant lower odds of attending the ED for patients with advance care planning (low strength evidence). Out of hours access to hospice physician34 or advice line24 were each examined by a high-quality study. These studies found no relationship and a significant reduction in ED attendance respectively (very low strength evidence).
Illness-related factors
Four studies examined primary diagnosis of cardiovascular disease,3,28,37,38 three of which found cardiovascular disease increased ED attendance3,37,38 (moderate strength evidence). Two studies report the effect of cancer versus non-cancer on ED attendance,3,34 and two report cancer versus heart failure.37,38 All found that people with non-cancer diagnoses were more likely to attend ED than those with cancer (AORs 1.05–1.37; moderate strength evidence). Two studies each examined the effect of dementia27,28, stroke3,28and lung disease3,28 (versus no dementia/stroke/lung disease), and one study examined arthritis or rheumatism.28 None found evidence of an association with ED attendance (low/very low strength evidence). Three high-quality studies reported the relationship between mental health and ED attendance, finding no evidence of effect (moderate strength evidence).28,31,34 One study examined depression among dementia patients and found a significant association with higher likelihood of ED attendance.31
We found little evidence that number of comorbidities was associated with ED28,34 (low strength evidence). One study examined the effect of having different comorbidities alongside dementia, and found positive associations with ED attendance, with the strongest effect for hypertension (very low strength evidence).35 There was low strength evidence that cognitive impairment was associated with lower ED attendance3,31 and very low strength evidence relating to physical symptoms (pain).3
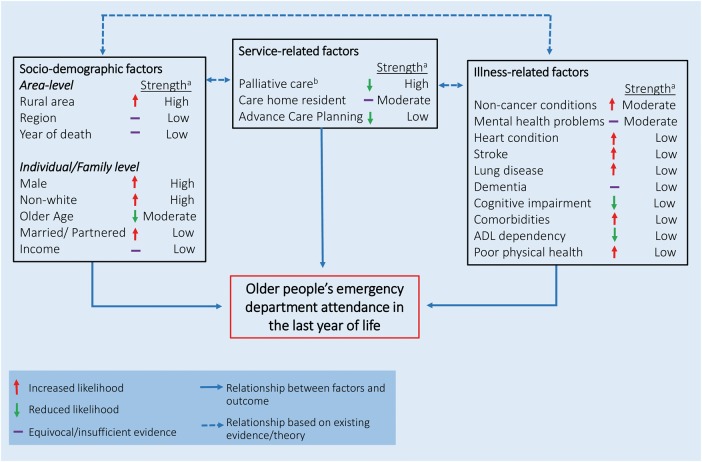
Theoretical model of older adults’ ED attendance in the last year of life
We present the synthesized findings in figure 3. Service-related factors include factors potentially amenable to modification by policy, commissioners, or practitioners. The socio-demographic factors represent area- or individual-level targets for services, while the illness-related factors are potential targets for intervention at a clinical level. The solid lines represent associations from our findings, while dotted lines represent associations between the factor groups based on existing evidence or theory. There is evidence that socio-demographic and illness factors are related to access to services. For example, older patients, ethnic minority patients and non-cancer primary diagnoses are each associated with lower access to specialist palliative care services.39–41 Similarly, there are well-established relationships between socio-demographic factors, particularly age and gender, and illness factors such as diagnoses and comorbidities.42
Figure 3.
Model of factors related to emergency department attendance by people aged 65+ years in the last year of life. aStrength of evidence, graded according to algorithm; bpalliative care includes specialist, generalist or hospice care; ADL=activities of daily living
Discussion
In this systematic review, we extend knowledge by synthesizing evidence from 21 studies including more than 1.5 million older people, to identify service-related, socio-demographic, and illness-related factors that are associated with ED attendance towards the end of life. Identifying service factors is of particular importance given that such factors are amenable to change. We present the strongest evidence to date that provision of palliative or hospice care to older people is associated with lower ED attendance within the last year of life with mostly large effect sizes, and that earlier provision strengthens this relationship. This corroborates findings from a randomized controlled trial (RCT) of home palliative care for older people expected to be towards the end of life, which showed significant reductions in ED attendance.43 This finding has potential implications for service development for older people with non-cancer conditions, who have historically not been the primary recipients of specialist palliative care.
We found low strength evidence that advance care planning or discussing preferences for place of care is associated with lower ED attendance for older people towards the end of life, indicating that high-quality future research is required to understand this relationship. For family members who expected their relative to die, the odds of attending ED were lower than those who did not expect it. These findings suggest that recognition of end of life is important, and family is key to involve in end of life discussions.
Provision of community care by generalist nurses and physicians is likely to be an important factor relating to ED attendance, but was not considered among included studies. A previous systematic review on determinants of ED visits among older people (not necessarily towards the end of life) found that perceived low availability of physicians was related to greater ED use.44 There is also an important gap in evidence on the impact of ‘general palliative care’ provision by primary care practitioners, who are typically older adults’ main care providers. In addition, whether variation in social care explains ED attendance towards the end of life was not reported, despite over a quarter of people receiving social care in the last year of life, and the proportion increasing with age.15
Examination of socio-demographic and illness factors are important for understanding inequalities in care and to identify potential targets for services. We found high strength evidence that male gender, and black or minority ethnicity increased likelihood of attending ED towards the end of life. A surprising finding was the high strength of evidence for people in rural areas being more likely to attend ED than in urban areas, despite lower proximity to hospitals. These results do however corroborate findings for cancer patients only, increasing confidence in these findings.16 We found little evidence on patient-reported factors such as breathlessness and anxiety, which are potentially key to our understanding of why older people present to the ED towards the end of life. Breathlessness is a prominent symptom in advanced disease, which can be distressing for patients and their families. Qualitative research has found disease-related anxiety to be an important factor contributing to cancer patients’ ED attendance towards the end of life.45
Three-quarters of included papers were published in the last five years, demonstrating an increasingly strong evidence base, but gaps in our understanding remain. The evidence is predominantly from the USA, based on large routinely collected datasets. It is important to interpret the findings with this context in mind, given the differences between the health system in USA and elsewhere. Despite knowledge that hospitalizations in the last year of life are common across European countries,46 few studies examining ED attendance were conducted in European countries and there is a notable lack of evidence from low- or middle-income countries. Most factors with high strength evidence were those that are easily measurable in routine data, not necessarily those that are most clinically important, or amenable to change.
There has been a recent move to include ED attendance as a quality indicator for end of life care. In North America, ED attendance is already included as a key measure of intensity of end of life care for cancer patients.16 However, whether or not high ED attendance is a cause or consequence of poor quality care is untested. Qualitative research has found that cancer patients and carers perceive hospital as a place of safety and security during times of crisis and when care at home breaks down.45 There is limited investigation of the views of older people with non-cancer conditions on ED attendance towards the end of life, which is a key area for future research.
A strength of this review is its robust and systematic methods, which enabled comprehensive review of the evidence, with no restrictions on time or language. Building on existing theoretical models, this study has developed our understanding of ED attendance of older people, including non-cancer conditions, a group which has previously been excluded. Including older people with varying diagnoses and not focussing on a single disease type is a strength, as it is more reflective of the population of older people who increasingly have multiple problems and conditions. We extracted data on both significant and non-significant associations to minimize bias against negative findings.
This systematic review also has limitations. It was not possible to make judgement about the appropriateness of ED admissions with the data available. The strict focus on the last year of life for comparability meant that the inclusion of studies was weighted towards observational studies, as RCTs at the end of life are less commonly conducted and less likely to follow patients until death. Synthesis across studies was limited by the variation in outcome definitions, time-period before death, and population heterogeneity, precluding meta-analysis. Additionally, causation between identified factors and ED attendance cannot be inferred due to the nature of the evidence. The dominance of evidence from the USA limits the generalizability of our findings to other countries.
Conclusions
Receiving palliative or hospice care is associated with lower ED attendance in the last year of life for older adults. These services may enable older people to remain in their usual place of care and reduce unplanned hospital ED attendance, in line with their preferences, by receiving timely care and treatment responsive to changing needs. Focussing on improving access to palliative or hospice care for non-cancer populations, and non-white ethnicities may also reduce the inequalities we observed in end of life care. Our understanding of what drives the association between palliative or hospice care services and ED in the last year of life remains limited, suggesting a need for better evidence on the effectiveness of models of community care for older adults towards the end of life. There is also a need for better high-quality international evidence on factors associated with older people’s ED attendance from other European countries and beyond, particularly in low- and middle-income countries, to optimize end of life care in different healthcare systems.
Supplementary Material
Acknowledgements
With thanks to collaborators and advisors, including service users, and members of the International Access, Rights and Empowerment II study group: Lara Klass, Bridget Johnston, Peter May, Regina McQuillan, Karen Ryan, Diane Meier, Sean Morrison, Charles Normand, Deokhee Yi, Melissa Aldridge.
Funding
This work is independent research funded by Cicely Saunders International and The Atlantic Philanthropies (grant number 24610). The sponsor had no role in the design, methods, subject recruitment, data collection, analysis or preparation of this paper.
This research was supported by the Collaboration for Leadership in Applied Health Research and Care (CLAHRC) South London, which is part of the National Institute for Health Research (NIHR), and is a partnership between King’s Health Partners, St. George’s, University London, and St George’s Healthcare NHS Trust. C.J.E. holds a HEE/NIHR Senior Clinical Lectureship and I.J.H. is an Emeritus NIHR Senior Investigator. B.G.’s contribution was supported by the Calouste Gulbenkian Foundation.
Disclaimer
The views expressed in this publication are those of the author(s) and not necessarily those of the NHS, the National Institute for Health Research or the Department of Health.
Conflicts of interest: None declared.
Key points
We have synthesized evidence from 21 studies including over 1.5 million people on factors associated with ED attendance for older people towards the end of life.
Palliative/hospice care is associated with reduced ED attendance, supported by high strength evidence and mostly large effect sizes, suggesting that investment in these services for older people may prevent ED attendance towards the end of life.
Non-white ethnicity, male gender, living in a rural area and non-cancer conditions are associated with higher ED attendance, highlighting inequalities in end of life care that require further attention.
References
- 1. Higginson IJ, Daveson BA, Morrison RS et al. Social and clinical determinants of preferences and their achievement at the end of life: prospective cohort study of older adults receiving palliative care in three countries. BMC Geriatr 2017;17:271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Gott M, Seymour J, Bellamy G et al. Older people’s views about home as a place of care at the end of life. Palliat Med 2004;18:460–7. [DOI] [PubMed] [Google Scholar]
- 3. Smith AK, McCarthy E, Weber E et al. Half of older Americans seen in emergency department in last month of life; most admitted to hospital, and many die there. Health Aff (Millwood) 2012;31:1277–85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Marie C. Emergency admissions: data briefing. 2018. Available at:https://www.mariecurie.org.uk/globalassets/media/documents/policy/policy-publications/2018/emergency-admissions-briefing-paper-2018.pdf.
- 5. Fong TG, Tulebaev SR, Inouye SK. Delirium in elderly adults: diagnosis, prevention and treatment. Nat Rev Neurol 2009;5:210–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lavan AH, Gallagher PF, O’Mahony D. Methods to reduce prescribing errors in elderly patients with multimorbidity. Clin Interv Aging 2016;11:857–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Department of Health. More care less pathway: a review of the Liverpool Care Pathway. 2013. Available at:https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/212450/Liverpool_Care_Pathway.pdf.
- 8. Murray SA, Kendall M, Boyd K et al. Illness trajectories and palliative care. BMJ 2005;330:1007–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Aparasu RR, Mort JR. Inappropriate prescribing for the elderly: beers criteria-based review. Ann Pharmacother 2000;34:338–46. [DOI] [PubMed] [Google Scholar]
- 10. Sharp T, Moran E, Kuhn I et al. Do the elderly have a voice? Advance care planning discussions with frail and older individuals: a systematic literature review and narrative synthesis. Br J Gen Pract 2013;63:e657–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rolls L, Seymour JE, Froggatt KA et al. Older people living alone at the end of life in the U.K.: research and policy challenges. Palliat Med 2011;25:650–7. [DOI] [PubMed] [Google Scholar]
- 12. Van den Block L, Deschepper R, Drieskens K et al. Hospitalisations at the end of life: using a sentinel surveillance network to study hospital use and associated patient, disease and healthcare factors. BMC Health Serv Res 2007;7:1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. He W, Goodkind D, Kowal P. An Aging World: 2015. International Population Reports. 2016. Available at:https://www.census.gov/content/dam/Census/library/publications/2016/demo/p95–16–1.pdf.
- 14. Hall S, Petkova H, Tsouros A et al. Palliative care for older people: better practices. World Health Organisation Regional Office for Europe, 2011. Available at:http://www.euro.who.int/__data/assets/pdf_file/0017/143153/e95052.pdf. [Google Scholar]
- 15. Georghiou T, Davies S, Davies A, Bardsley M. Understanding patterns of health and social care at the end of life. Nuffield Trust, 2012. Available at:https://www.nuffieldtrust.org.uk/files/2017–01/understanding-patterns-health-social-care-end-of-life-full-web-final.pdf.
- 16. Henson LA, Gao W, Higginson IJ et al. Emergency department attendance by patients with cancer in their last month of life: a systematic review and meta-analysis. J Clin Oncol 2015;33:370–6. [DOI] [PubMed] [Google Scholar]
- 17. Barnett K, Mercer SW, Norbury M et al. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet 2012;380:37–43. [DOI] [PubMed] [Google Scholar]
- 18. Andersen RM, Davidson PL. Improving access to care in America: individual and contextual indicators. In: Andersen RM RT, Kominski E, editors. Changing the US Health Care System: Key Issues in Health Services, Policy, and Management. San Francisco, CA: Jossey-Bass, 2001: 3–30. [Google Scholar]
- 19. Gomes B, Higginson IJ. Factors influencing death at home in terminally ill patients with cancer: systematic review. BMJ 2006;332:515–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kmet LLR, Cook L. Standard Quality Assessment Criteria for Evaluating Primary Research Papers from a Variety of Fields. Edmonton: Alberta Heritage Foundation for Medical Research, 2004. Available at:https://www.biomedcentral.com/content/supplementary/1471–2393–14–52-s2.pdf. [Google Scholar]
- 21. Brumley RD, Enguidanos S, Cherin DA. Effectiveness of a home-based palliative care program for end-of-life. J Palliat Med 2003;6:715–24. [DOI] [PubMed] [Google Scholar]
- 22. Lustbader D, Mudra M, Romano C et al. The impact of a home-based palliative care program in an accountable care organization. J Palliat Med 2017;20:23–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Miller SC, Lima JC, Intrator O et al. Palliative care consultations in nursing homes and reductions in acute care use and potentially burdensome end-of-life transitions. J Am Geriatr Soc 2016;64:2280–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Purdy S, Lasseter G, Griffin T et al. Impact of the Marie Curie cancer care delivering choice programme in Somerset and North Somerset on place of death and hospital usage: a retrospective cohort study. BMJ Support Palliat Care 2015;5:34–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Miller SC, Lima JC, Thompson SA. End-of-life care in nursing homes with greater versus less palliative care knowledge and practice. J Palliat Med 2015;18:527–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Morin L, Rotelli-Bihet L. Hospital deaths and emergency admission of nursing homes’ residents at the end of life: results from a retrospective cross-sectional study in France. Palliat Med 2014;28:718. [Google Scholar]
- 27. Nakashima T, Young Y, Hsu WH. Are Hospital/ED transfers less likely among nursing home residents with do-not-hospitalize orders? J Am Med Dir Assoc 2016;18:438–41. [DOI] [PubMed] [Google Scholar]
- 28. Feng Z, Coots LA, Kaganova Y et al. Hospital and ED use among medicare beneficiaries with dementia varies by setting and proximity to death. Health Aff (Millwood) 2014;33:683–90. [DOI] [PubMed] [Google Scholar]
- 29. Volicer L, Hurley AC, Blasi ZV. Characteristics of dementia end-of-life care across care settings. Am J Hosp Palliat Care 2003;20:191. [DOI] [PubMed] [Google Scholar]
- 30. Mitchell SL, Morris JN, Park PS et al. Terminal care for persons with advanced dementia in the nursing home and home care settings. J Palliat Med 2004;7:808–16. [DOI] [PubMed] [Google Scholar]
- 31. Sleeman KE, Perera G, Stewart R et al. Predictors of emergency department attendance by people with dementia in their last year of life: retrospective cohort study using linked clinical and administrative data. Alzheimers Dement 2018;14:20. [DOI] [PubMed] [Google Scholar]
- 32. Unroe KT, Greiner MA, Johnson KS et al. Racial differences in hospice use and patterns of care after enrollment in hospice among medicare beneficiaries with heart failure. Am Heart J 2012;163:987. [DOI] [PubMed] [Google Scholar]
- 33. Wang SY, Aldridge MD, Gross CP et al. End-of-life care intensity and hospice use. Med Care 2016;54:672–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Aldridge MD, Epstein AJ, Brody AA et al. The impact of reported hospice preferred practices on hospital utilization at the end of life. Med Care 2016;54:657–63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Rosenwax L, Spilsbury K, Arendts G et al. Community-based palliative care is associated with reduced emergency department use by people with dementia in their last year of life: a retrospective cohort study. Palliat Med 2015;29:727–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Bischoff KE, Sudore R, Miao Y et al. Advance care planning and the quality of end-of-life care in older adults. J Am Geriatr Soc 2013;61:209–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Setoguchi S, Glynn RJ, Stedman M et al. Hospice, opiates, and acute care service use among the elderly before death from heart failure or cancer. Am Heart J 2010;160:139–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Cheung WY, Schaefer K, May CW et al. Enrollment and events of hospice patients with heart failure vs. cancer. J Pain Symptom Manage 2013;45:552–60. [DOI] [PubMed] [Google Scholar]
- 39. Burge FI, Lawson BJ, Johnston GM et al. A Population-based study of age inequalities in access to palliative care among cancer patients. Med Care 2008;46:1203–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Seow H, O’Leary E, Perez R et al. Access to palliative care by disease trajectory: a population-based cohort of Ontario decedents. BMJ Open 2018;8:e021147. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.