Abstract
Objective Closed reduction and percutaneous pinning (CRPP) is losing popularity as a treatment modality for distal radius fractures. However, in select cases, CRPP may have advantages relative to open reduction and internal reduction. We aimed to retrospectively assess the outcomes after CRPP for the treatment of distal radius fractures.
Study Design This is a retrospective cohort study.
Methods We used billing records to identify all skeletally mature patients with a distal radius fracture who were treated with CRPP by a single surgeon at a level I trauma center in an urban city in the United States. We assessed the medical charts and recorded demographics, trauma and treatment characteristics, radiographic characteristics, and outcomes.
Results All patients had a good or excellent range of motion regarding forearm rotation, and almost 80% had good or excellent range of motion regarding flexion or extension of their wrist. One patient had a concern for pin tract infection, and one had subcutaneous migration of a pin, which were both treated by pin removal.
Conclusion CRPP is a good option in patients with few and sizeable fracture fragments in patients with a distal radius fracture, and it should be considered as an effective tool to restore radiographic parameters and functional outcomes.
Keywords: closed reduction and percutaneous pinning, Kirschner wire, open reduction and internal fixation, distal radius fracture
Introduction
It is acknowledged that different fracture types of the distal radius merit different fixation methods, but specific recommendations based on fracture type are unavailable due to the absence of convincing scientific evidence. 1 2 3 4 Despite the absence of a consistent treatment algorithm for distal radius fractures, there seems to be a collective tendency among orthopaedic trauma surgeons to treat distal radius fractures with open reduction and internal fixation (ORIF)—even though ORIF does not always seem to result in superior long-term results when compared with closed reduction and percutaneous pinning (CRPP), 5 6 and the results of CRPP are comparable to those of ORIF. 7 The advantages that CRPP can have relative to ORIF in selected fractures seem to play a subordinate role in surgical decision making, as CRPP appears to be losing popularity among surgeons. 5 Apart from being less invasive and possibly a technically less demanding procedure compared with ORIF, CRPP also seems to be more economical than ORIF. 6 8 This advantage will become more and more elemental as the treatment of distal radius fractures is increasingly challenging the financial allocations in health care, both due to aging population and the rising use of (costly) ORIF as a primary treatment modality. 9 Despite these advantages and despite evidence suggesting superior results of CRPP compared with plaster casting, 4 we noticed that the use of CRPP in our institutions is relatively unpopular compared with treatment of distal radius fractures by ORIF.
We therefore aimed to retrospectively assess the outcomes after closed reduction and percutaneous Kirschner wire pinning for the treatment of distal radius fractures and to compare these with the results of previous studies.
Methods
After approval by our institutional review board, we used billing records to identify all skeletally mature patients with a distal radius fracture who were treated with closed reduction and percutaneous Kirschner wire pinning by a single surgeon at a level I trauma center in an urban city in the United States from 2012 to 2016. We excluded one patient who had fractures on the same extremity that required surgical treatment in the same surgery and two patients who had less than 6 weeks of follow-up. Our final study cohort consisted of 34 patients. We manually assessed the charts, operative reports and radiographs of each of these patients and recorded basic demographics, trauma characteristics, treatment characteristics, and outcomes. We measured radiographic parameters of the radius fractures on the pre-reduction and the final follow-up radiographs.
Patient and Injury Characteristics
We included 34 patients in this study with a mean age of 47 ± 18 years (range: 22–85 years). Our cohort consisted mostly of females ( n = 28; 82%) and the majority of the patients ( n = 25; 74%) had an AO-Müller type C fracture Table 1 . The mean duration of follow-up was 19 weeks (range: 6–89 weeks).
Table 1. Patient, trauma, diagnosis, and treatment characteristics.
| Variable | All patients ( n = 34) |
|---|---|
| Abbreviations: BMI, body mass index; SD, standard deviation. | |
| Patient characteristics | |
| Sex, n (%) | |
| Male | 6 (18) |
| Female | 28 (82) |
| Age, mean ± SD, years | 47 ± 18 |
| BMI mean ± SD | 24 ± 4.5 |
| Smoker, n (%) | 4 (12) |
| Trauma characteristics | |
| Mechanism of injury, n (%) | |
| Fall from standing height | 18 (53) |
| Fall from stairs | 5 (15) |
| Motor vehicle accident | 3 (8.9) |
| Sports | 8 (24) |
| Dominant wrist injured, n (%) | 22 (63) |
| Diagnosis and treatment characteristics | |
| AO Müller fracture classification, n (%) | |
| A | 8 (24) |
| B | 1 (2.9) |
| C | 25 (74) |
| Days from injury to surgery, mean ± SD | 6.7 ± 3.4 |
| Duration of surgery, mean ± SD, minutes | 24 ± 7.5 |
| Days from surgery to pin removal, mean ± SD | 41 ± 6.0 |
| Rehabilitation protocol, n (%) | 34 (100) |
| Number of pins used, n (%) | |
| 2 | 17 (50) |
| 3 | 13 (38) |
| 4 | 4 (12) |
| Size of pins used, n (%) | |
| 0.062 inch | 22 (65) |
| Combination of 0.045 and 0.062 inch | 12 (35) |
| Total duration of follow-up, mean ± SD, weeks | 19 ± 14 |
Treatment Characteristics
All patients were treated within the first 2 weeks after their injury. The pinning procedure was performed using mini C-arm image intensification ( Fig. 1 ). The distal radius fracture was reduced with a combination of traction, wrist flexion, and ulnar deviation. The fractures that could not be reduced anatomically, including fractures affecting the volar lunate facet, were deemed to be unsuitable for this technique and were converted to ORIF. After confirming that the fracture could be reduced anatomically, a small incision was made just distal to the tip of the radial styloid. We then performed subcutaneous dissection to expose the tip of the radial styloid. Using a soft tissue protector, a 0.062-in Kirschner wire was placed initially from the tip of the radial styloid across the fracture site into the proximal fragment under direct vision. An oscillating attachment was used for placement of all wires. After confirming the position of the first Kirschner wire to be satisfactory, this was usually augmented with a second wire placed in a similar fashion. In the patients who required additional wire placement in the die punch fragment (the dorsoulnar corner of the intermediate column), an additional incision was made distal and ulnar to the die punch fragment. Dissection was performed carefully between the extensor tendons to expose the dorsal ulnar lip of the radius. A 0.045-in Kirschner wire was then placed from the die punch fragment across the fracture site into the proximal fragment to create an X-shaped construct. After confirming the position of the wires to be satisfactory on orthogonal radiographic views, the wires were cut and bent.
Fig. 1 (A–C).
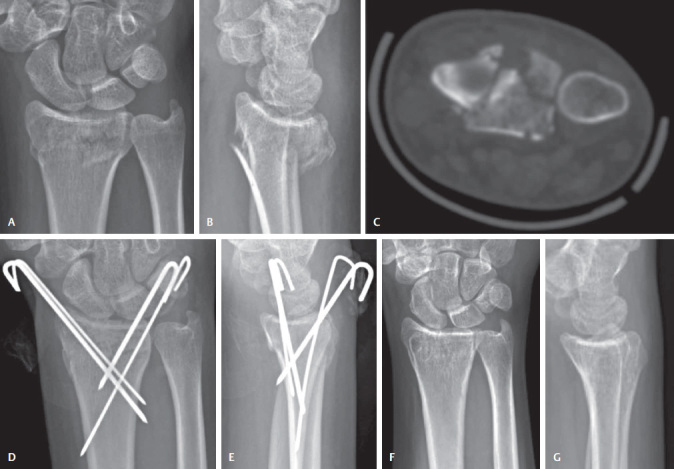
Preoperative radiographs and CT scan demonstrated a multifragmentary intra-articular fracture of the distal radius. (D, E) Posttreatment radiographs after pinning of the dorsal ulnar corner to restore the intermediate column, and pinning of the radial styloid to restore the radial column. (F, G) Final follow-up radiographs, 5½ months after the procedure date.
The patient’s upper limb was supported in splints for the first 5 to 7 days after surgery. Patients were then transitioned to a plaster cast, which was maintained for between 5 and 6 weeks. During this time, they were given rehabilitative exercises to maximize digital range of motion and perform edema control measures. The Kirschner wires were removed after an average of 41 ± 6 days (range: 26–48 days; Table 1 ). The injured wrist was then placed in a custom fabricated thermoplastic wrist splint, and a formal rehabilitation program supervised by certified hand therapists was started. Strengthening was commenced 3 weeks after starting the rehabilitation exercises and at this stage, all splinting was discontinued.
Results
Radiographic evaluation of the final follow-up radiographs showed a 32% improvement of the mean radial height and a mean difference of 19 degrees in the palmar tilt Table 2 . Almost 80% of the patients demonstrated a good or excellent range of motion in terms of flexion/extension of the wrist, and all patients had a good or excellent range of motion in terms of forearm rotation Table 3 . One patient had a pin tract infection 5 weeks after pin placement, which was treated by pin removal. One patient required a minor additional procedure due to subcutaneous migration of a radial styloid pin, where 6.5 weeks after the initial procedure a small incision was made and the pin was identified and removed without any difficulty.
Table 2. Radiographic parameters of the distal radius fractures.
| Radiographic parameter, mean ± SD | Pre-reduction | Final follow-up |
|---|---|---|
| Abbreviation: SD, standard deviation. | ||
| Radial height, mm | 7.3 ± 8.5 | 9.6 ± 2.1 |
| Radial inclination, degrees | 15 ± 5.5 | 20 ± 3.9 |
| Articular gap, mm | 1.5 ± 1.4 | 0.052 ± 0.22 |
| Articular step, mm | 0.64 ± 0.82 | 0.043 ± 0.18 |
| Anteroposterior distance, mm | 19 ± 4.3 | 19 ± 2.4 |
| Palmar tilt, degrees | −18 ± 12 | 0.39 ± 8.3 |
| Teardrop angle, degrees | 43 ± 14 | 60 ± 6.9 |
Table 3. Range of motion after percutaneous Kirschner wire pinning of distal radius fractures.
| Range of motion, n (%) | All patients ( n = 34) |
|---|---|
| Wrist flexion/extension | |
| Excellent (arc > 140°) | 17 (50) |
| Good (arc 120–140°) | 10 (29) |
| Fair (arc 100–120°) | 6 (18) |
| Poor (arc < 100°) | 1 (2.9) |
| Forearm rotation | |
| Excellent (arc > 140°) | 28 (82) |
| Good (arc 120–140°) | 6 (18) |
Discussion
In the contemporary setting, distal radius fractures are not treated on the basis of well-established guidelines or algorithms. Rather, ORIF with a volar-locked plate has become the procedure of choice for most surgeons. Despite the fact that in some cases of distal radius fractures CRPP seems superior when compared with other treatment options, 4 6 8 it is losing popularity among orthopaedic surgeons. 5 We aimed to evaluate our results of CRPP of distal radius fractures and to compare these with the prior literature.
Our finding that CRPP is a satisfactory technique for restoring radiographic parameters is supported by multiple studies. 10 11 12 We found that nearly 80% of the patients who received CRPP for their distal radius fracture demonstrated good to excellent range of motion at their final follow-up appointment. This high proportion of patients showing good to excellent range of motion is consistent with prior studies reporting range of motion after CRPP. 6 10 12 13 14 15 16
Of the 34 patients, 2 (5.9%) had complications: 1 patient showed signs of superficial pin tract infection and 1 had subcutaneous migration of one pin.
Prior published data regarding (superficial) pin tract infections after CRPP of distal radius fractures indicate pin tract infection rates varying from 1.7 to 9.5%, 10 16 17 18 19 nearly always resolving after removal of the pins. In situ time of the pins appears to be a risk factor for infection and burying the pins in for prolonged in situ time may help reduce infection rates. 20 While pin migration leading to fracture redisplacement has been reported in prior literature, 12 we did not encounter this in our cohort.
The debate regarding the need for and the type of operative fixation of distal radius fractures is an ongoing process. 1 2 3 4 This is largely a debate between physicians, because patients do not always seem to have a strong preference for a specific fixation method. 21 Published data indicate that less invasive treatment methods may lead to better subjective outcomes in specific fracture types. 22 23 This is in contrast with a prospective randomized trial indicating that the early postoperative functional outcomes seem to be in favor of ORIF, although none of these two treatment methods showed superiority in terms of long-term radiographic or functional outcomes. 24 A prospective randomized trial comparing the results of early rehabilitation after ORIF to delaying rehabilitation for 6 weeks showed no difference in clinical outcomes after 6 months. 25 It would therefore seem intuitive that CRPP followed by 6 weeks of casting would have similar outcomes for carefully selected fractures that could be treated either with ORIF or CRPP.
These discussions regarding the role of CRPP in the treatment of distal radius fractures are mainly exclusively informed by clinical variables. Since the burden of distal radius fractures on the health care resource allocations is expected to grow, 9 it is becoming increasingly important to also explore our treatment strategies for distal radius fractures from a resource allocation perspective. Despite an abundance of literature on distal radius fractures, the financial aspect of this very common fracture is relatively underexposed. The very few studies that assessed resource allocation in the treatment of distal radius fractures show consistent results: the financial burden of distal radius fractures is increasing, mainly due to the prevailing use of volar-locked plating in the treatment of these fractures. 6 8 9 21
Prior research has established that, depending on the number of fracture fragments, CRPP leads to satisfactory results in the treatment of distal radius fractures. 14 Pins placed in the distal radius seem to be less prone for complications compared with pins placed in the metacarpals or the phalanges, 18 and proper knowledge of the anatomy of the wrist may aid in minimizing the already low number of adverse events after CRPP even further. 26
In addition, when one considers allocation of health care expenditure, one also has to consider reimbursements to treating physicians. In the contemporary setting, ORIF is reimbursed by Medicare at nearly twice the rate as CRPP. Therefore, one has to carefully consider the influence that such inequity may have on treatment choices. Future research should aid this discussion by providing more insights in the differences in costs between different treatments of distal radius fractures.
This study should be interpreted in light of its strengths and limitations. As with every database study, we rely on the accuracy of the coding and there may be a small amount of miscoding errors. Based on prior published data, it is unlikely that this will have a consequential influence on our results. 27 Second, our sample size was not large enough to allow us to perform a meaningful statistical analysis. However, a statistical analysis would be beyond the scope of this article as we aimed to describe the outcomes of a single surgeon’s experience with CRPP and to compare these to previously published data. Last, we also acknowledge that since we selected this cohort based on the CPT-code for CRPP, there may be some selection bias—excluding fracture types that do not qualify for treatment through CRPP such as certain displaced volar lunate facet fractures. Our strengths include an adequate time of follow-up, the fact that all patients were treated by the same surgeon, which eliminated interobserver bias, and the increasing clinical relevancy of CRPP in the setting of distal radius fractures.
In conclusion, our results show that CRPP can be an effective tool for restoring radiographic parameters after carefully selected types A and C distal radius fractures, and that most patients demonstrate a good or excellent range of wrist motion after treatment with CRPP. We acknowledge that ORIF is a good surgical option in multifragmentary fractures or fractures in patients with poor bone quality. However, in light of comparable radiographic and long-term functional outcomes for carefully chosen fractures, we encourage considering CRPP more prominently in (young) patients with few and large fracture fragments.
Footnotes
Conflict of Interest None.
References
- 1.American Academy of Orthopaedic Surgeons . Rosemont, IL: 2009. AAOS Guideline: The Treatment of Distal Radius Fractures. [Google Scholar]
- 2.Handoll H H, Huntley J S, Madhok R. External fixation versus conservative treatment for distal radial fractures in adults. Cochrane Database Syst Rev. 2007;(03):CD006194. doi: 10.1002/14651858.CD006194.pub2. [DOI] [PubMed] [Google Scholar]
- 3.Handoll H H, Huntley J S, Madhok R. Different methods of external fixation for treating distal radial fractures in adults. Cochrane Database Syst Rev. 2008;(01):CD006522. doi: 10.1002/14651858.CD006522.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Handoll H H, Vaghela M V, Madhok R. Percutaneous pinning for treating distal radial fractures in adults. Cochrane Database Syst Rev. 2007;(03):CD006080. doi: 10.1002/14651858.CD006080.pub2. [DOI] [PubMed] [Google Scholar]
- 5.Koval K J, Harrast J J, Anglen J O, Weinstein J N. Fractures of the distal part of the radius. The evolution of practice over time. Where’s the evidence? J Bone Joint Surg Am. 2008;90(09):1855–1861. doi: 10.2106/JBJS.G.01569. [DOI] [PubMed] [Google Scholar]
- 6.Dzaja I, MacDermid J C, Roth J, Grewal R. Functional outcomes and cost estimation for extra-articular and simple intra-articular distal radius fractures treated with open reduction and internal fixation versus closed reduction and percutaneous Kirschner wire fixation. Can J Surg. 2013;56(06):378–384. doi: 10.1503/cjs.22712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lozano-Calderón S A, Doornberg J N, Ring D. Retrospective comparison of percutaneous fixation and volar internal fixation of distal radius fractures. Hand (NY) 2008;3(02):102–110. doi: 10.1007/s11552-007-9078-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Shyamalan G, Theokli C, Pearse Y, Tennent D. Volar locking plates versus Kirschner wires for distal radial fractures—a cost analysis study. Injury. 2009;40(12):1279–1281. doi: 10.1016/j.injury.2009.02.018. [DOI] [PubMed] [Google Scholar]
- 9.Shauver M J, Yin H, Banerjee M, Chung K C. Current and future national costs to Medicare for the treatment of distal radius fracture in the elderly. J Hand Surg Am. 2011;36(08):1282–1287. doi: 10.1016/j.jhsa.2011.05.017. [DOI] [PubMed] [Google Scholar]
- 10.Azzopardi T, Ehrendorfer S, Coulton T, Abela M. Unstable extra-articular fractures of the distal radius: a prospective, randomised study of immobilisation in a cast versus supplementary percutaneous pinning. J Bone Joint Surg Br. 2005;87(06):837–840. doi: 10.1302/0301-620X.87B6.15608. [DOI] [PubMed] [Google Scholar]
- 11.Alm-Paulsen P S, Rod O, Rød K, Rajabi B, Russwurm H, Finsen V. Percutaneous pinning of fractures of the distal radius. J Plast Surg Hand Surg. 2012;46(03)(04):195–199. doi: 10.3109/2000656X.2012.685623. [DOI] [PubMed] [Google Scholar]
- 12.Gupta R, Raheja A, Modi U. Colles’ fracture: management by percutaneous crossed-pin fixation versus plaster of Paris cast immobilization. Orthopedics. 1999;22(07):680–682. [PubMed] [Google Scholar]
- 13.Chen C E, Juhn R J, Ko J Y. Treatment of distal radius fractures with percutaneous pinning and pin-in-plaster. Hand (NY) 2008;3(03):245–250. doi: 10.1007/s11552-008-9093-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Clancey G J. Percutaneous Kirschner-wire fixation of Colles fractures. A prospective study of thirty cases. J Bone Joint Surg Am. 1984;66(07):1008–1014. [PubMed] [Google Scholar]
- 15.Wong T C, Chiu Y, Tsang W L, Leung W Y, Yam S K, Yeung S H. Casting versus percutaneous pinning for extra-articular fractures of the distal radius in an elderly Chinese population: a prospective randomised controlled trial. J Hand Surg Eur Vol. 2010;35(03):202–208. doi: 10.1177/1753193409339941. [DOI] [PubMed] [Google Scholar]
- 16.Rodríguez-Merchán E C. Plaster cast versus percutaneous pin fixation for comminuted fractures of the distal radius in patients between 46 and 65 years of age. J Orthop Trauma. 1997;11(03):212–217. doi: 10.1097/00005131-199704000-00013. [DOI] [PubMed] [Google Scholar]
- 17.Allain J, le Guilloux P, Le Mouël S, Goutallier D. Trans-styloid fixation of fractures of the distal radius. A prospective randomized comparison between 6- and 1-week postoperative immobilization in 60 fractures. Acta Orthop Scand. 1999;70(02):119–123. doi: 10.3109/17453679909011247. [DOI] [PubMed] [Google Scholar]
- 18.Hsu L P, Schwartz E G, Kalainov D M, Chen F, Makowiec R L. Complications of K-wire fixation in procedures involving the hand and wrist. J Hand Surg Am. 2011;36(04):610–616. doi: 10.1016/j.jhsa.2011.01.023. [DOI] [PubMed] [Google Scholar]
- 19.Lenoble E, Dumontier C, Goutallier D, Apoil A. Fracture of the distal radius. A prospective comparison between trans-styloid and Kapandji fixations. J Bone Joint Surg Br. 1995;77(04):562–567. [PubMed] [Google Scholar]
- 20.Hargreaves D G, Drew S J, Eckersley R. Kirschner wire pin tract infection rates: a randomized controlled trial between percutaneous and buried wires. J Hand Surg [Br] 2004;29(04):374–376. doi: 10.1016/j.jhsb.2004.03.003. [DOI] [PubMed] [Google Scholar]
- 21.Shauver M J, Clapham P J, Chung K C. An economic analysis of outcomes and complications of treating distal radius fractures in the elderly. J Hand Surg Am. 2011;36(12):1912–1918. doi: 10.1016/j.jhsa.2011.09.039. [DOI] [PubMed] [Google Scholar]
- 22.Lalone E A, Rajgopal V, Roth J, Grewal R, MacDermid J C. A cohort study of one-year functional and radiographic outcomes following intra-articular distal radius fractures. Hand (NY) 2014;9(02):237–243. doi: 10.1007/s11552-013-9586-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kreder H J, Hanel D P, Agel J et al. Indirect reduction and percutaneous fixation versus open reduction and internal fixation for displaced intra-articular fractures of the distal radius: a randomised, controlled trial. J Bone Joint Surg Br. 2005;87(06):829–836. doi: 10.1302/0301-620X.87B6.15539. [DOI] [PubMed] [Google Scholar]
- 24.Rozental T D, Blazar P E, Franko O I, Chacko A T, Earp B E, Day C S. Functional outcomes for unstable distal radial fractures treated with open reduction and internal fixation or closed reduction and percutaneous fixation. A prospective randomized trial. J Bone Joint Surg Am. 2009;91(08):1837–1846. doi: 10.2106/JBJS.H.01478. [DOI] [PubMed] [Google Scholar]
- 25.Lozano-Calderón S A, Souer S, Mudgal C, Jupiter J B, Ring D. Wrist mobilization following volar plate fixation of fractures of the distal part of the radius. J Bone Joint Surg Am. 2008;90(06):1297–1304. doi: 10.2106/JBJS.G.01368. [DOI] [PubMed] [Google Scholar]
- 26.Santoshi J A, Chaware P N, Pakhare A P, Rathinam B A. An anatomical study to demonstrate the proximity of Kirschner wires to structures at risk in percutaneous pinning of distal radius fractures. J Hand Microsurg. 2015;7(01):73–78. doi: 10.1007/s12593-015-0181-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Mackenney P J, McQueen M M, Elton R. Prediction of instability in distal radial fractures. J Bone Joint Surg Am. 2006;88(09):1944–1951. doi: 10.2106/JBJS.D.02520. [DOI] [PubMed] [Google Scholar]


