Abstract
Literacy plays an important role in Alzheimer’s disease and related dementias (ADRD); however, less is known about how literacy is being used and defined in ADRD studies. This study reviewed terminology being used to describe types and definitions of literacy and instruments used to assess literacy in ADRD research. Among the 219 studies retrieved from 3 databases, 50 met our inclusion criteria. Literacy terms used in ADRD studies varied: literacy (n = 28), health literacy (n = 9), and dementia literacy (n = 7) were the most often used terms, followed by financial literacy (n = 4), dementia knowledge (n = 3), AD knowledge (n = 2), mental health literacy (n = 2), AD literacy, digital literacy, health literacy about incontinence, and financial knowledge (n = 1 each). Thirty studies did not define literacy terms used. Among the 20 studies defining literacy, definitions were inconsistent across studies even when they used the same term. Surveys (n = 30), open-ended questions, vignettes, or focus groups (n = 10), self-perceived (n = 3) or interviewer assessed (n = 1) literacy levels were used to assess literacy. Ten studies did not specify literacy measurement. Various literacies have been examined in ADRD research with unclear definitions and some inadequate measures. Well-defined terms with valid measures are needed to better understand the role of literacies in ADRD research.
Keywords: Alzheimer’s disease, dementia, literacy, health literacy, review
Introduction
Alzheimer’s disease (AD) is the most common type of dementia and the sixth leading cause of death in the United States (Alzheimer’s Association, 2018). About 5.7 million Americans are currently living with AD and related dementias (ADRD), and the prevalence of ADRD is increasing as baby boomers continue to age (Alzheimer’s Association, 2018). ADRD is impacted by more than genetics; lifestyle factors, such as diet, physical activity, and socioeconomic status may also play a role in the development of ADRD (Alzheimer’s Association, 2018).
Literacy often refers the ability to read or write. Beyond this fundamental literacy, literacy includes a broad range of abilities such as oral skills, numeracy, and how to access, learn, and apply knowledge and information (United Nations Educational, Scientific and Cultural Organization, 2005), and multiple domains of literacy have been proposed in various field. For example, the Institute of Medicine (Nielsen-Bohlman, Panzer, & Kindig, 2004) viewed that health literacy includes individuals’ capabilities of writing and reading, speaking and listening, cultural and conceptual knowledge, and numeracy. Others also included fundamental literacy (reading, writing, speaking, and numeracy), scientific literacy, civic literacy, and cultural literacy (Zarcadoolas, Pleasant, & Greer, 2009), and media and Internet literacy as components of health literacy (Norman & Skinner, 2006; Nutbeam, 1998; Zarcadoolas et al., 2009). Given that different type of literacies may link to different role of literacy in people’s ability to understand and utilize information, defining literacy is important to understand the role and impacts of literacy on people’s health.
Literacy is suggested to be an important predictor of cognitive decline and ADRD due to its relation to cognitive reserve (Manly, Schupf, Tang, & Stern, 2005). The cognitive reserve theory hypothesizes that individuals with different cognitive reserve, preexisting cognitive capacity, have different brain functions and thus their brains react differently to brain changes such as ADRD (Stern, 2002). This theory explained that individuals with more cognitive reserve can cope better with ADRD and maintain effective brain function than those with less cognitive reserve when brain changes are the same. Level of cognitive reserve is often measured by literacy. Commonly used instruments for literacy measurement include the Wide Range Achievement Test (WRAT), Rapid Estimate of Adult Literacy in Medicine (REALM), and Test of Functional Health Literacy in Adults (TOFHLA), which test various components of literacy ranging from word recognition, pronunciation, reading comprehension, and numeracy (Friedman & Hoffman-Goetz, 2006). Literacy has been investigated in ADRD research to understand the role of literacy in ADRD, and previous studies showed that literacy level may predict cognitive decline or ADRD (Boyle et al., 2013; Lee et al., 2016; Manly et al., 2005).
In addition, health literacy, defined as “the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions” (U.S. Department of Health and Human Services, 2000) has received much attention in recent years. Individuals with low health literacy are more likely to have negative health outcomes including cancer, diabetes, and ADRD (Bailey et al., 2014; Oldach & Katz, 2014; Yu, Wilson, Schneider, Bennett, & Boyle, 2017) as well as higher hospitalization rates, poor knowledge of health issues, and lower utilization of preventive services (Berkman, Sheridan, Donahue, Halpern, & Crotty, 2011; Diviani, Putte, Giani, & Weert, 2015). Improving health literacy has become increasingly important as health information and services including those related to ADRD have become more complex (Centers for Disease Control and Prevention, 2009). However, more than half of Americans over the age of 65 are considered to have a below-basic level of health literacy, and about 98% have health literacy skills that are below the proficient level (Kobylarz, Pomidor, & Pleasant, 2010). Limited literacy skills may hinder older populations from engaging in prevention and early detection of diseases, including ADRD, and from appropriate communication with health care providers and use of health care services (Suka et al., 2015; Suri, Majid, Chang, & Foo, 2015).
Although many aspects of literacies need to be considered to address ADRD, the term literacy and its multiple domains often used in different ways in each study. To better understand potential roles of various aspects of literacy in ADRD and compare results over previous research, it is important to understand how literacy is being used, defined, and measured in ADRD research. Thus, the purpose of this study was to examine types of literacy, literacy definitions, and instruments used to assess literacy in ADRD research.
Research Design
Search Strategy
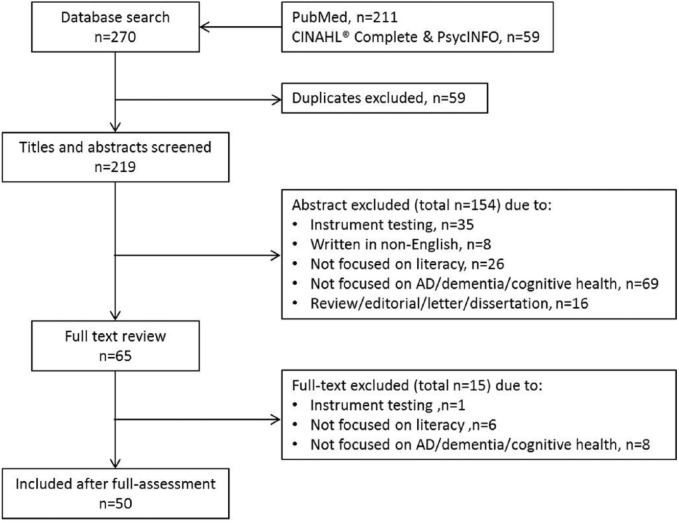
A scoping review of studies on ADRD and cognitive health with a literacy component was conducted. In September 2016, we searched PubMed, Cumulative Index to Nursing and Allied Health Literature (CINAHL)® Complete, and PsycINFO using the following combination of search terms: “Dementia” OR “Alzheimer’s disease” OR “Cognitive health” OR “Cognitive impairment” OR “Cognitive decline” AND “Literacy.” The search of titles and abstracts yielded a total of 270 abstracts across the three databases. After excluding duplicate studies, 219 studies remained.
Inclusion and Exclusion Criteria
We included studies that were (a) written in English, (b) empirical research examining literacy in studies of ADRD and cognitive health, and (c) published in a peer-reviewed journal. Studies were excluded if they were (a) written in other languages; (b) focused on other diseases; (c) reviews, editorials, letters, essays, case reports, conference abstracts, or dissertations; and (d) conducted specifically for the purpose of instrument or validity testing. We did not exclude studies based on publication year.
Study Selection
An initial review of titles and abstracts were done by two reviewers. They each reviewed half of abstracts and reviewed the same random 10% of abstracts independently. Any discrepancies between the two reviewers were discussed until a consensus was reached. If disagreement remained, another author served as a tiebreaker. After excluding 154 studies from the abstract reviews, the first author reviewed full texts of remaining studies and further excluded 15 studies that did not meet inclusion criteria. Of the 169 studies excluded, 36 studies focused on instrument testing, eight studies were not in English, 32 studies were not focused on or directly related to literacy (e.g., used education level as an indicator of literacy), 77 studies were not focused on dementia/AD/cognitive health, and 16 studies were reviews/editorials/letters/dissertations. A final total of 50 studies were included for analysis. The study selection process is presented in Figure 1.
Figure 1.
Flow diagram of the literature search.
Data Extraction
One author completed full-article coding of the 50 studies. Another author reviewed a 20% random sample of the studies to ensure quality coding. For each study, we identified what type of literacy was defined (e.g., literacy, health literacy, dementia/AD/cognitive health literacy, financial literacy) and if and how it was measured. Disease focus (e.g., dementia, AD, cognitive health), study location, and other characteristics of study populations, including sample size, age, sex, and rate of inadequate literacy, were coded during the full-text review.
Results
Characteristics of the studies reviewed, including literacy terms, definitions, and measurements used in each study, are presented in Table 1.
Table 1.
Literacy Terms, Definitions, Instruments, and Study Characteristics in Alzheimer’s Disease (AD) and Related Dementias Research (n = 50).
| References | Study location Population Age rangea Sample size |
Disease focus | Definition of literacy | Instrument(s) used to assess literacy | % low/inadequate literacy |
|---|---|---|---|---|---|
| AD literacy | |||||
| Sun, Gao, and Coon (2013) | The United States Community members/general population 55-100 385 |
AD | People’s knowledge and beliefs about AD | 24 AD knowledge items and 10 Chinese cultural beliefs of AD items | — |
| AD knowledge | |||||
| Stansbury, Marshall, Harley, and Nelson (2010)
Valle, Yamada, and Matiella (2006) |
The United States Community members/general population African American clergy 36-90 9-111 |
AD Dementia |
AD knowledge: 6 questions A vignette depicting an elder man experiencing symptoms of AD |
11.1% | |
| Dementia literacy | |||||
| Diamond and Woo (2014) Kim, Sargent, Cox, and Anstey (2015) Loi and Lautenschlager (2015) Low and Anstey (2009) Low et al. (2010) Millard, Kennedy, and Baune (2011) Noble, Hedmann, and Williams (2015) |
Australia The United States England Community members/general population Patients in general practices 9-94 34-2,000 |
Dementia AD |
A person’s knowledge regarding dementia Knowledge and beliefs regarding dementia that aid recognition, management, or prevention |
Focus group Vignette(s) describing dementia symptoms and behaviors of a person Self-reported adequateness of dementia knowledge True or false statements assessing comprehension of dementia symptoms, cause, treatment and prognosis Open-ended questions about dementia risk factor and risk reduction Questions related to intervention program content—AD symptoms, causes |
— |
| Dementia knowledge | |||||
| Lee et al. (2016)
Millard et al. (2011) Zheng and Woo (2016) |
Australia; England; South Korea; the United States Community members/general population AD/dementia/cognitive impairment patients Health care professionals 55+ / no age range 153-6,141 |
Dementia | Self-report “Do you consider your dementia knowledge adequate?” Questions regarding dementia causes, symptoms, treatment and prognosis |
78%-85% | |
| Health literacy | |||||
| Apolinario, Mansur, Carthery-Goulart, Brucki, and Nitrini (2015)
Bennett, Boyle, James, and Bennett (2012) Bliss et al. (2013) Gupta et al. (2016) Han, Boyle, James, Yu, and Bennett (2015) Kobayashi, Wardle, Wolf, and Wagner (2015) Nguyen et al. (2013) Stewart et al. (2018) Wilson, Yu, James, Bennett, and Boyle (2017) |
The United States; England; Brazil Community members/general population Older adults with diabetes Informal caregivers 18-100.8 48-5,256 |
Dementia AD Cognitive decline/impairment/health |
The ability to access, understand, and utilize health information and concepts in ways that promote good health outcomes. The cognitive and social skills which determine the motivation and ability of individuals to gain access to, understand and use information in ways which promote and maintain good health. The degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions. (Do not have trouble) accessing, understanding, and using information to make basic health decisions. |
9 items including questions on Medicare, following doctors’ prescription instructions, leading causes of death in older persons, and a question framing the same drug risk information in difference ways The Adult Literacy and Life Skills Survey Short Test of Functional Literacy in Adults (S-TOFHLA) Focus group interviews |
27.7%-54.8% |
| Financial literacy | |||||
| Bennett et al. (2012)
Han et al. (2015) Stewart et al. (2018) Wilson et al. (2017) |
The United States Community members/general population 58-100.8 487-755 |
AD44
Cognitive decline/impairment/health |
The ability to access, understand, and utilize financial information and concepts in ways that promote good financial outcomes. | 23 items, with simple arithmetic items to evaluate numeracy and question about financial concepts such as compound interest. | — |
| Financial knowledge | |||||
| Baird, Ford, and Podell (2007) | The United States Community members/general population Mean age: 75 129 |
Cognitive decline/impairment/health | — | The ILS Money Management Subscale | |
| Literacy | |||||
| Baird et al. (2007)
Barnes, Tager, Satariano, and Yaffe (2004) Black et al. (1999) Boyle et al. (2013) Brewster et al. (2014) Chandra et al. (1998a) Chandra et al. (1998b) Contador et al. (2017) Jitapunkul, Kunanusont, Phoolcharoen, and Suriyawongpaisal (2001) Kaup et al. (2014) Kaup et al. (2015) Kuczmarski, Cotugna, Mason, Evans, and Zonderman (2015) Lee et al. (2016) Manly, Touradji, Tang, and Stern (2003) Manly, Schupf, Tang, and Stern (2005) Mayeaux et al. (1995) Mehta et al. (2009) R. Pandav, Dodge, DeKosky, and Ganguli (2003) R. S. Pandav, Chandra, Dodge, DeKosky, and Ganguli (2004) Prince et al. (2012) Rovner, Casten, and Leiby (2016) Sachs-Ericsson and Blazer (2005) Scazufca et al. (2008) Scazufca, Almeida, and Menezes (2010) Stewart et al. (2018) Valle et al. (2006) Vivot et al. (2015) Yaffe et al. (2013) |
Brazil; China; Cuba; France; India; Mexico; Peru; South Korea; Spain; Thailand; the Dominican Republic; The United States; Venezuela Community members/general population Community dwelling older adults who are APOE ε4 carriers Community members/general population who reside in socially deprived areas Medicare recipients AD/dementia/cognitive impairment patients Patients with varying degrees of medical illnesses and cognitive impairment, including AD 30-105 105-12,887 |
AD Dementia Cognitive decline/impairment/health |
The ability to read and write; a dynamic, lifelong learning process that involves the acquisition and application of relevant knowledge to circumstances encountered in everyday life. The ability to identify, understand, interpret, create, communicate and compute, using printed and written materials associated with varying contexts. The ability to identify, understand, interpret, and use written materials to function effectively in varying context. Able to read and/or write English reading level Oral word reading Single word reading |
Total 32 items (9 for health literacy, 23 for financial literacy) National Adult Reading Test Reading Recognition Subtest of the Wide Range Achievement Test-Version 3 (WRAT-3) Rapid Estimate of Adult Literacy in Medicine (REALM) American version of the National Adult Reading Test for English speaking people Word Accentuation Test for Spanish speakers Reading written information, assessed by the interviewer. North American Adult Reading Test (NART) Self-assessed reading and/or writing ability |
4.0%-88.4% |
| Health literacy about incontinence | |||||
| Mullins, Bliss, Rolnick, Henre, and Jackson (2016) | The United States Informal caregivers Mean age: 64 48 |
AD | — | Focus group and interviews | — |
| Mental health literacy | |||||
| Chong et al. (2016)
Stansbury, Harley, and Brown-Hughes (2010) |
Singapore The United States African American clergy Community members/general population 18-68 9-3,006 |
Dementia AD |
Knowledge and beliefs about mental disorders which aid their recognition, management or prevention | Vignette(s) | 33.7% |
| Digital health literacy | |||||
| Xavier et al. (2014) | England Community members/general population 50-89 6,442 |
Cognitive decline/impairment/health | The ability to engage, plan, execute, and evaluate digital actions such as web browsing and exchanging E-mails as aids for dealing with daily life task. | Self-reported use Internet or email | 64.9% did not use Internet/email |
Age range and mean age were reported at base line if the study was a cohort study.
Characteristics of Studies Reviewed and Study Populations
Thirty-one studies were conducted in the United States, five in Australia, four in India, and three each in England and Brazil. Three studies were conducted in more than one country. Study populations were mainly community members/general population that might include ADRD patients (n = 45). Two studies each specifically focused only on individuals with mild cognitive impairment or AD and caregivers of individuals with ADRD. Two studies included African American clergy. Only one study included health care professionals, and two included more than one population.
Most studies included older adults (aged 65 years or more; n = 21) or individuals middle aged or older (aged 50 years or older; n = 16). Four studies included only adults (aged 18-65 years) and six studies included both adults and older adults. Only one study focused on only children. Sample size in each study varied with the smallest having nine participants and the largest study including 12,887 participants. The mean number of participants across studies was 1,789. Thirty-two studies reported percentages of low or inadequate literacy among study populations; percentages of low or inadequate literacy varied greatly in each study ranging from 4.0% to 88.4%.
Disease Focus
The disease focus was mainly cognitive impairment or cognitive health (n = 22) and dementia (n = 15). Fewer studies focused on AD only (n = 8), both dementia and AD (n = 4), and both AD and cognitive impairment/health (n = 1). Two studies discussed dementia and AD interchangeably.
Literacy Focus
Literacy was examined the most (n = 28), followed by health literacy (n = 9), dementia literacy (n = 7), financial literacy (n = 4), dementia knowledge (n = 3), AD knowledge (n = 2), mental health literacy (n = 2), and others (AD literacy, digital literacy, health literacy about incontinence, financial knowledge; each was examined in one study). Eight studies discussed multiple literacies or knowledge. Ten studies used the terms “literacy,” “knowledge,” or “skill” interchangeably.
Literacy Definition
Thirty studies did not define literacy. The definition of literacy varied among the remaining studies that defined the term (n = 20). Studies of literacy, health literacy, or digital literacy (n = 7) addressed people’s ability to access, understand, utilize information/materials to define the term. Studies of AD literacy, dementia literacy, or mental health literacy (n = 4) defined literacy as people’s knowledge and belief regarding AD/dementia/mental disorder. One study about dementia literacy (Low et al., 2010) only addressed knowledge when they defined the term dementia literacy while another study conducted by the same authors defined this term as people’s knowledge and beliefs (Low & Anstey, 2009). Eight studies of literacy defined the term as the ability to read and/or write. Four studies did not define the literacy terms they focused on.
Among the studies that defined literacy, 11 studies used definition from published research or reports (e.g., health literacy definition from Institute of Medicine (Nielsen-Bohlman, Panzer, & Kindig, 2004), or Nutbeam, 1998; mental health literacy from Jorm et al., 1997). One study stated that the definition was from a local registry, but did not provide a citation. Eight studies did not include a source for the definition that they provided.
Literacy Measurement
Ten studies did not specify how literacy was measured. Among the remaining studies that discussed measurement, four used multiple methods. Quantitative surveys were used most often (n = 30), including the WRAT version 3 (n = 6; word recognition and pronunciation test), REALM (n = 4; medical terminology reading and pronunciation test), shortened version of the TOFHLA (n = 3; reading comprehension and numeracy test), North American Adult Reading Test (n = 2; word recognition test), and true/false statements or questions regarding AD/dementia causes, symptoms, prognosis, and treatment (n = 2). Five studies used the same 32-item questionnaire to assess health literacy (nine items) and financial literacy (23 items) and considered sum of health literacy and financial literacy as a total literacy. Among the five studies, Boyle et al. (2013) did not separate health and financial literacy and used total literacy in the analysis. Six studies provided vignette(s) describing person(s) with ADRD and examined if study participants were able to recognize individuals’ symptoms. One study used open-ended questions for participants to describe dementia risk factors and risk reduction.
Qualitative studies did not use a specific instrument to assess literacy. Rather, literacy was the main focus of discussion groups or interviews or it emerged as a theme. Three qualitative studies examined participants’ perceived level of literacy and another study used interviewers’ perceived level of participants’ literacy.
Some studies measured a different type of literacy than the literacy they defined or used throughout the study. Sun, Gao, and Coon (2013) used the term “AD literacy,” but measured AD knowledge using 24 items about AD symptoms, course, risk factors, diagnosis and treatment, and caregiving. Noble, Hedmann, and Williams (2015) conducted an intervention program to increase AD knowledge among students. They used “dementia health literacy” in the title, used terms “AD health literacy,” “dementia literacy,” and “AD knowledge” in the main text, and assessed AD knowledge. In a multicountry study, literacy was only measured for participants in India (instrument not specified) and for participants in the United States, education level was used as an indicator for literacy level. Vivot et al. (2015) assessed literacy as a surrogate of cognitive reserve.
How Literacy Was Studied
Two fifths of the studies (n = 20) assessed literacy level and some (n = 13) also examined factors associated with literacy. APOE ε4 allele and decreased cognition, cognitive impairment, or dementia in old age were related to low levels of literacy (Boyle et al., 2013; Lee e016; Stewart et al., 2018); while duration in the United States among Chinese Americans was not related to dementia literacy (Diamond & Woo, 214). Higher literacy was associated with more participation in cognitive/social and physical activity among African Americans with mild cognitive impairment (Rovner, Casten, & Leiby, 2016). Higher level of AD knowledge was related to higher perceived threat of AD (Sun, Gao, & Coon, 2013). Lack of dementia knowledge was a barrier to change lifestyles and behaviors to reduce dementia risk (Kim, Sargent-Cox, & Anstey, 2015). Two studies implemented interventions aimed at increasing AD knowledge (Noble, Hedmann, & Williams, et al., 2015; Valle, Yamada, & Matiella, 2006).
Two fifths of the studies (n = 20) assessed literacy level and some (n = 13) also examined factors associated with literacy. APOE ε4 allele and decreased cognition, cognitive impairment, or dementia in old age were related to low levels of literacy, while duration in the United States among Chinese Americans was not related to dementia literacy. Higher literacy was associated with more participation in cognitive/social and physical activity among African Americans with mild cognitive impairment. Higher level of AD knowledge was related to higher perceived threat of AD (Sun, Gao, & Coon, 2013). Lack of dementia knowledge was a barrier to change lifestyles and behaviors to reduce dementia risk. Two studies implemented interventions aimed at increasing AD knowledge.
In some studies, literacy was not the main foci. Literacy was used as an adjustment variable in studies that examining associations between AD and self-assessed school performance, AD and hemoglobin level, cognitive impairment and blood pressure, cognitive impairment and neurological factors, or cognitive function and caffeine intake. In a study examining the association between AD-related genotypes and cognitive decline, literacy was considered one domain of cognitive decline (Vivot et al., 2015).
In two qualitative studies, health literacy was used to describe a lack of health literacy related to incontinence care among informal caregivers of people with ADRD and their health literacy needs related to incontinence and skin care (Bliss et al., 2013; Mullins, Blisss, Rolnick, Henre, & Jackson, 2016).
Discussion
This scoping review aimed to examine how literacy is being defined and used in ADRD studies. Our review revealed that multiple literacy types were examined in ADRD studies and that these literacies were measured by various tools and methods. Although terms were different, the purpose of examining literacy was similar: that is, literacy may have a role in people’s cognitive health and ADRD. Most studies in this review showed that higher literacy is associated with better cognitive health and lower prevalence of ADRD.
There was inconsistency in how the terms were defined as all studies that defined a term(s) addressed reading or writing skills. Reading/writing level alone, however, may not reflect a person’s literacy. Some studies that defined literacy actually addressed multiple literacies, for example, scientific literacy (AD knowledge), cultural literacy (people’s belief regarding AD), and ability to access, understand, and utilize information.
These varied literacies in studies reviewed, however, were not consistent in each study. In addition, more than half of studies did not define the literacy term used in the research. Inconsistency in definitions and using undefined terms may make study findings incomparable across studies. For example, literacy as an ability to read or write and literacy as ability to access, understand, and utilize information are different. Interestingly, all studies that used the term “knowledge” did not define that term. Given that we reviewed studies having “literacy” in the title or abstract, the studies using the term “knowledge” without a definition used either another type of literacy in the study (Baird, Ford, & Podell, 2007; Lee et al., 2016; Millard, Kennedy, & Baune, 2011; Valle, Yamada, & Matiella, 2006) or “knowledge” and “literacy” interchangeably (Stansbury, Marshall, Harley, & Nelson, 2010; Zheng & Woo, 2016).
Studies used various measurements even if they examined the same type of literacy. Furthermore, some studies measured different literacies compared with the literacy term actually defined in the study. This may be due in part to a lack of consistency in definition of the terms. Studies might have discussed the same type of literacy but present different definitions and different strategies for assessing literacy. We found studies used inappropriate tools to assess literacies such as a pronunciation test or self-perceived or interviewer-perceived level of literacy instead of a validated tool. These assessments, while useful, may not accurately reflect the person’s literacy.
Some types of literacy and populations that are potentially important were less studied. Due to the increased burden of disease in people’s later stages of life, older people as well as their caregivers often face financial issues resulting from health care costs (Riffin, Van Ness, Wolff, & Fried, 2017; Wolff, Spillman, Freedman, & Kasper, 2016). In addition, health and financial decisions for elders are often made with or only by their informal caregivers such as family members or friends (National Alliance for Caregiving & AARP Public Policy Institute, 2015; Riffin et al., 2017; Wolff et al., 2016). Thus, attention is being paid to improving financial literacy (“the ability to access, understand, and utilize financial information”) (James, Boyle, Bennett, & Bennett, 2012) among older adults and caregivers. Only five studies reviewed measured financial literacy/knowledge and two studies included caregivers of individuals with ADRD. Individuals living with ADRD spend about 4 times more out-of-pocket expenses for health care and long-term care services than others of the similar age (Alzheimer’s Association, 2016). In addition, their informal caregivers often spend significant amount of money to take care of ADRD patients and even cut back their own spending, saving, retirement saving, or work hours (Alzheimer’s Association, 2016). Given that individuals living with ADRD and their caregivers are at a risk of financial insecurity, financial literacy would be important to prepare them for care planning. Health literacy of caregivers of individuals with ADRD is also important because they perform numerous tasks that include managing medical situations, health information seeking, communication with health care providers, and making health decisions for their care recipients (National Alliance for Caregiving, & AARP Public Policy Institute, 2015; Spillman, Wolff, Freedman, & Kasper, 2014). The two studies that included caregivers highlighted lack of health literacy among caregivers and their need for improved caregiving-related health literacy (Bliss et al., 2013; Mullins, Bliss, Rolnick, Henre, & Jackson, 2016). Further research is needed to understand the importance of literacy among caregivers and to develop interventions to improve their literacy.
This study has two limitations. First, only studies written in English were included in the review. Second, we reviewed studies having search terms in the title or abstract; thus, we might have missed relevant literature.
Conclusion
This study presents and describes literacy terms and instruments that have been used in ADRD research. We did not intend to recommend a single definition of literacy or a gold standard for measuring literacy. We acknowledge that various aspects of literacies each may have unique roles in ADRD; thus, it is important to consider examining multiple literacies in ADRD research. Still, defining the literacy term and use of a valid instrument are critical to better understand which aspects of literacy are associated with ADRD. Future ADRD research needs to define literacy terms and use appropriate tools that can more accurately reflect individuals’ literacy. Understanding how people’s level of literacy is associated with ADRD would provide insights into how we can better reach high-risk populations (e.g., individuals with lower literacy levels) for early detection of ADRD and relevant prevention efforts.
Author Biographies
Seul Ki Choi, PhD, MPH, is a postdoctoral fellow at the Department of Health Promotion, Education, and Behavior, Arnold School of Public Health, University of South Carolina.
India D. Rose, PhD, MPH, CHES, is a manager at ICF, Health Research, Informatics and Technology Division. She is also an associate professor at Chamberlain University, Master of Public Health Online Program.
Daniela B. Friedman, PhD, is professor and chair of the Department of Health Promotion, Education, and Behavior and co-director of the Office for the Study of Aging in the Arnold School of Public Health at the University of South Carolina.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by the South Carolina Healthy Brain Research Network (HBRN) funded by the Centers for Disease Control and Prevention (CDC)’s Alzheimer’s Disease and Healthy Aging Program. The HBRN is a thematic network of CDC’s Prevention Research Centers Program (PRC). Research efforts were supported in part by cooperative agreement U48 DP005000. The findings and conclusions of this research are those of the authors and do not necessarily represent the official views of the CDC.
ORCID iD: Seul Ki Choi  https://orcid.org/0000-0002-3330-3652
https://orcid.org/0000-0002-3330-3652
References
- Alzheimer’s Association. (2016). 2016 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia: Journal of the Alzheimer’s Association, 12, 459-509. doi: 10.1016/j.jalz.2016.03.001 [DOI] [PubMed] [Google Scholar]
- Alzheimer’s Association. (2018). 2018 Alzheimer’s disease facts and figures. Alzheimer’s & Dementia: Journal of the Alzheimer’s Association, 14, 367-429. doi: 10.1016/j.jalz.2018.02.001 [DOI] [Google Scholar]
- Apolinario D., Mansur L. L., Carthery-Goulart M. T., Brucki S. M., Nitrini R. (2015). Cognitive predictors of limited health literacy in adults with heterogeneous socioeconomic backgrounds. Journal of Health Psychology, 20, 1613-1625. doi: 10.1177/1359105313520337 [DOI] [PubMed] [Google Scholar]
- Bailey S. C., Brega A. G., Crutchfield T. M., Elasy T., Herr H., Kaphingst K., . . . Pignone M. (2014). Update on health literacy and diabetes. The Diabetes Educator, 40, 581-604. doi: 10.1177/0145721714540220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baird A. D., Ford M., Podell K. (2007). Ethnic differences in functional and neuropsychological test performance in older adults. Archives of Clinical Neuropsychology, 22, 309-318. doi: 10.1016/j.acn.2007.01.005 [DOI] [PubMed] [Google Scholar]
- Barnes D. E., Tager I. B., Satariano W. A., Yaffe K. (2004). The relationship between literacy and cognition in well-educated elders. The Journals of Gerontology, Series A: Biological Sciences & Medical Sciences, 59, M390-M395. doi: 10.1093/gerona/59.4.M390 [DOI] [PubMed] [Google Scholar]
- Bennett J. S., Boyle P. A., James B. D., Bennett D. A. (2012). Correlates of health and financial literacy in older adults without dementia. BMC Geriatrics, 12, Article 30. doi: 10.1186/1471-2318-12-30 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman N. D., Sheridan S. L., Donahue K. E., Halpern D. J., Crotty K. (2011). Low health literacy and health outcomes: An updated systematic review. Annals of Internal Medicine, 155, 97-107. doi: 10.7326/0003-4819-155-2-201107190-00005 [DOI] [PubMed] [Google Scholar]
- Black S. A., Espino D. V., Mahurin R., Lichtenstein M. J., Hazuda H. P., Fabrizio D., . . . Markides K. S. (1999). The influence of noncognitive factors on the Mini-Mental State Examination in older Mexican-Americans: Findings from the Hispanic EPESE. Journal of Clinical Epidemiology, 52, 1095-1102. doi: 10.1016/S0895-4356(99)00100-6 [DOI] [PubMed] [Google Scholar]
- Bliss D., Rolnick C., Jackson J., Arntson C., Mullins J., Hepburn K. (2013). Health literacy needs related to incontinence and skin damage among family and friend caregivers of individuals with dementia. Journal of Wound Ostomy & Continence Nursing, 40, 515-523. doi: 10.1097/WON.0b013e3182a3ff24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyle P. A., Yu L., Wilson R. S., Segawa E., Buchman A. S., Bennett D. A. (2013). Cognitive decline impairs financial and health literacy among community-based older persons without dementia. Psychology and Aging, 28, 614-624. doi: 10.1037/a0033103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brewster P. W., Melrose R. J., Marquine M. J., Johnson J. K., Napoles A., MacKay-Brandt A., . . . Mungas D. (2014). Life experience and demographic influences on cognitive function in older adults. Neuropsychology, 28, 846-858. doi: 10.1037/neu0000098 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2009). Improving health literacy for older adults: Expert panel report 2009. Atlanta, GA: U.S. Department of Health and Human Services. [Google Scholar]
- Chandra V., DeKosky S. T., Pandav R., Johnston J., Belle S. H., Ratcliff G., Ganguli M. (1998. a). Neurologic factors associated with cognitive impairment in a rural elderly population in India: The Indo-US Cross-National Dementia Epidemiology Study. Journal of Geriatric Psychiatry and Neurology, 11, 11-17. doi: 10.1177/089198879801100104 [DOI] [PubMed] [Google Scholar]
- Chandra V., Ganguli M., Pandav R., Johnston J., Belle S., DeKosky S. (1998. b). Prevalence of Alzheimer’s disease and other dementias in rural India The Indo-US study. Neurology, 51, 1000-1008. doi: 10.1212/WNL.51.4.1000 [DOI] [PubMed] [Google Scholar]
- Chong S. A., Abdin E., Picco L., Pang S., Jeyagurunathan A., Vaingankar J. A., . . . Subramaniam M. (2016). Recognition of mental disorders among a multiracial population in Southeast Asia. BMC Psychiatry, 16, Article 121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contador I., del Ser T., Llamas S., Villarejo A., Benito-León J., Bermejo-Pareja F. (2017). Impact of literacy and years of education on the diagnosis of dementia: A population-based study. Journal of Clinical and Experimental Neuropsychology, 39, 112-119. doi: 10.1080/13803395.2016.1204992 [DOI] [PubMed] [Google Scholar]
- Diamond A. G., Woo B. K. (2014). Duration of residence and dementia literacy among Chinese Americans. International Journal of Social Psychiatry, 60, 406-409. doi: 10.1177/0020764013491742 [DOI] [PubMed] [Google Scholar]
- Diviani N., Putte B., Giani S., Weert J. (2015). Low health literacy and evaluation of online health information: A systematic review of the literature. Journal of Medical Internet Research, 17, e112. doi: 10.2196/jmir.4018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman D. B., Hoffman-Goetz L. (2006). A systematic review of readability and comprehension instruments used for print and web-based cancer information. Health Education & Behavior, 33, 352-373. doi: 10.1177/1090198105277329 [DOI] [PubMed] [Google Scholar]
- Gupta V. K., Winter M., Cabral H., Henault L., Waite K., Hanchate A., . . . Paasche-Orlow M. K. (2016). Disparities in age-associated cognitive decline between African-American and Caucasian populations: The roles of health literacy and education. Journal of the American Geriatrics Society, 64, 1716-1723. doi: 10.1111/jgs.14257 [DOI] [PubMed] [Google Scholar]
- Han S. D., Boyle P. A., James B. D., Yu L., Bennett D. A. (2015). Poorer financial and health literacy among community-dwelling older adults with mild cognitive impairment. Journal of Aging and Health, 27, 1105-1117. doi: 10.1177/0898264315577780 [DOI] [PMC free article] [PubMed] [Google Scholar]
- James B. D., Boyle P. A., Bennett J. S., Bennett D. A. (2012). The impact of health and financial literacy on decision making in community-based older adults. The Gerontology, 58, 531-539. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jitapunkul S., Kunanusont C., Phoolcharoen W., Suriyawongpaisal P. (2001). Prevalence estimation of dementia among Thai elderly: A national survey. Journal of the Medical Association of Thailand, 84, 461-467. [PubMed] [Google Scholar]
- Jorm A. F., Korten A. E., Jacomb P. A., Christensen H., Rodgers B., Pollitt P. (1997). Mental health literacy: A survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. The Medical Journal of Australia, 166, 182-186. [DOI] [PubMed] [Google Scholar]
- Kaup A. R., Nettiksimmons J., Harris T. B., Sink K. M., Satterfield S., Metti A. L., . . . Yaffe K. (2015). Cognitive resilience to apolipoprotein E ε4: Contributing factors in black and white older adults. JAMA Neurology, 72, 340-348. doi: 10.1001/jamaneurol.2014.3978 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaup A. R., Simonsick E. M., Harris T. B., Satterfield S., Metti A. L., Ayonayon H. N., . . . Yaffe K. (2014). Older adults with limited literacy are at increased risk for likely dementia. The Journals of Gerontology, Series A: Biological Sciences & Medical Sciences, 69, 900-906. doi: 10.1093/gerona/glt176 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim S., Sargent-Cox K. A., Anstey K. J. (2015). A qualitative study of older and middle-aged adults’ perception and attitudes towards dementia and dementia risk reduction. Journal of Advanced Nursing, 71, 1694-1703. doi: 10.1111/jan.12641 [DOI] [PubMed] [Google Scholar]
- Kobayashi L. C., Wardle J., Wolf M. S., Wagner C. (2015). Cognitive function and health literacy decline in a cohort of aging English adults. Journal of General Internal Medicine, 30, 958-964. doi: 10.1007/s11606-015-3243-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kobylarz F., Pomidor A., Pleasant A. (2010). Health literacy as a tool to improve the public understanding of Alzheimer’s disease. Annals of Long-Term Care, 18, 34-40. [Google Scholar]
- Kuczmarski A. V., Cotugna N., Mason M. A., Evans M. K., Zonderman A. B. (2015). Depression and cognitive impairment are associated with low education and literacy status and smoking but not caffeine consumption in urban African Americans and White adults. Journal of Caffeine and Adenosine Research, 5, 31-41. doi: 10.1089/jcr.2014.0019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee J.-Y., Park S., Kim K. W., Kwon J. E., Park J. H., Kim M. D., . . . Bae J. N. (2016). Differences in knowledge of dementia among older adults with normal cognition, mild cognitive impairment, and dementia: A representative nationwide sample of Korean elders. Archives of Gerontology and Geriatrics, 66, 82-88. doi: 10.1016/j.archger.2016.04.013 [DOI] [PubMed] [Google Scholar]
- Loi S. M., Lautenschlager N. T. (2015). Dementia literacy in older adults. Asia-Pacific Psychiatry, 7, 292-297. doi: 10.1111/appy.12153 [DOI] [PubMed] [Google Scholar]
- Low L.-F., Anstey K. J. (2009). Dementia literacy: Recognition and beliefs on dementia of the Australian public. Alzheimer’s & Dementia: Journal of the Alzheimer’s Association, 5, 43-49. doi: 10.1016/j.jalz.2008.03.011 [DOI] [PubMed] [Google Scholar]
- Low L.-F., Anstey K. J., Lackersteen S. M., Camit M., Harrison F., Draper B., Brodaty H. (2010). Recognition, attitudes and causal beliefs regarding dementia in Italian, Greek and Chinese Australians. Dementia and Geriatric Cognitive Disorders, 30, 499-508. doi: 10.1159/000321667 [DOI] [PubMed] [Google Scholar]
- Manly J. J., Schupf N., Tang M.-X., Stern Y. (2005). Cognitive decline and literacy among ethnically diverse elders. Journal of Geriatric Psychiatry and Neurology, 18, 213-217. doi: 10.1177/0891988705281868 [DOI] [PubMed] [Google Scholar]
- Manly J. J., Touradji P., Tang M.-X., Stern Y. (2003). Literacy and memory decline among ethnically diverse elders. Journal of Clinical and Experimental Neuropsychology, 25, 680-690. doi: 10.1076/jcen.25.5.680.14579 [DOI] [PubMed] [Google Scholar]
- Mayeaux E. J., Jr., Davis T. C., Jackson R. H., Henry D., Patton P., Slay L., Sentell T. (1995). Literacy and self-reported educational levels in relation to Mini-Mental State Examination scores. Family Medicine, 27, 658-662. [PubMed] [Google Scholar]
- Mehta K. M., Stewart A. L., Langa K. M., Yaffe K., Moody-Ayers S., Williams B. A., Covinsky K. E. (2009). “Below average” self-assessed school performance and Alzheimer’s disease in the aging, demographics, and memory study. Alzheimer’s & Dementia: Journal of the Alzheimer’s Association, 5, 380-387. doi: 10.1016/j.jalz.2009.07.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Millard F. B., Kennedy R. L., Baune B. T. (2011). Dementia: Opportunities for risk reduction and early detection in general practice. Australian Journal of Primary Health, 17, 89-94. doi: 10.1071/PY10037 [DOI] [PubMed] [Google Scholar]
- Mullins J., Bliss D. Z., Rolnick S., Henre C. A., Jackson J. (2016). Barriers to communication with a healthcare provider and health literacy about incontinence among informal caregivers of individuals with dementia. Journal of Wound Ostomy & Continence Nursing, 43, 539-544. doi: 10.1097/WON.0000000000000263 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Alliance for Caregiving, & AARP Public Policy Institute. (2015). Caregiving in the U.S. 2015. Retrieved from https://www.caregiving.org/caregiving2015/. [Google Scholar]
- Nguyen H. T., Kirk J. K., Arcury T. A., Ip E. H., Grzywacz J. G., Saldana S. J., . . . Quandt S. A. (2013). Cognitive function is a risk for health literacy in older adults with diabetes. Diabetes Research and Clinical Practice, 101, 141-147. doi: 10.1016/j.diabres.2013.05.012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nielsen-Bohlman L., Panzer A., Kindig D. Institute of Medicine, Committee on Health Literacy, & Board on Neuroscience and Behavioral Health. (2004). Health literacy: A prescription to end confusion. Washington, DC: National Academies Press. [PubMed] [Google Scholar]
- Noble J. M., Hedmann M. G., Williams O. (2015). Improving dementia health literacy using the FLOW mnemonic: Pilot findings from the Old SCHOOL Hip-Hop program. Health Education & Behavior, 42, 73-83. doi: 10.1177/1090198114537063 [DOI] [PubMed] [Google Scholar]
- Norman C. D., Skinner H. A. (2006). eHealth literacy: Essential skills for consumer health in a networked world. Journal of Medical Internet Research, 8, e9. doi: 10.2196/jmir.8.2.e9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nutbeam D. (1998). Health promotion glossary. Health Promotion International, 13, 349-364. doi: 10.1093/heapro/13.4.349 [DOI] [Google Scholar]
- Oldach B. R., Katz M. L. (2014). Health literacy and cancer screening: A systematic review. Patient Education and Counseling, 94, 149-157. doi: 10.1016/j.pec.2013.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pandav R., Dodge H. H., DeKosky S. T., Ganguli M. (2003). Blood pressure and cognitive impairment in India and the United States: A cross-national epidemiological study. Archives of Neurology, 60, 1123-1128. doi: 10.1001/archneur.60.8.1123 [DOI] [PubMed] [Google Scholar]
- Pandav R. S., Chandra V., Dodge H. H., DeKosky S. T., Ganguli M. (2004). Hemoglobin levels and Alzheimer disease: An epidemiologic study in India. The American Journal of Geriatric Psychiatry, 12, 523-526. doi: 10.1097/00019442-200409000-00011 [DOI] [PubMed] [Google Scholar]
- Prince M., Acosta D., Ferri C. P., Guerra M., Huang Y., Rodriguez J. J. L., Acosta I. (2012). Dementia incidence and mortality in middle-income countries, and associations with indicators of cognitive reserve: A 10/66 Dementia Research Group population-based cohort study. The Lancet, 380, 50-58. doi: 10.1016/S0140-6736(12)60399-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riffin C., Van Ness P. H., Wolff J. L., Fried T. (2017). Family and other unpaid caregivers and older adults with and without dementia and disability. Journal of the American Geriatrics Society, 65, 1821-1828. doi: 10.1111/jgs.14910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rovner B. W., Casten R. J., Leiby B. E. (2016). Determinants of activity levels in African Americans with mild cognitive impairment. Alzheimer Disease and Associated Disorders, 30, 41-46. doi: 10.1097/WAD.0000000000000096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sachs-Ericsson N., Blazer D. G. (2005). Racial differences in cognitive decline in a sample of community-dwelling older adults: The mediating role of education and literacy. The American Journal of Geriatric Psychiatry, 13, 968-975. doi: 10.1097/00019442-200511000-00007 [DOI] [PubMed] [Google Scholar]
- Scazufca M., Almeida O. P., Menezes P. R. (2010). The role of literacy, occupation and income in dementia prevention: The São Paulo Ageing & Health Study (SPAH). International Psychogeriatric, 22, 1209-1215. doi: 10.1017/S1041610210001213 [DOI] [PubMed] [Google Scholar]
- Scazufca M., Menezes P. R., Araya R., Di Rienzo V. D., Almeida O. P., Gunnell D., Lawlor D. A. (2008). Risk factors across the life course and dementia in a Brazilian population: Results from the Sao Paulo Ageing & Health Study (SPAH). International Journal of Epidemiology, 37, 879-890. doi: 10.1093/ije/dyn125 [DOI] [PubMed] [Google Scholar]
- Spillman B., Wolff J., Freedman V. A., Kasper J. D. (2014). Informal caregiving for older Americans: An analysis of the 2011 National Health and Aging Trends Study. Retrieved from https://aspe.hhs.gov/pdf-report/informal-caregiving-older-americans-analysis-2011-national-health-and-aging-trends-study
- Stansbury K. L., Harley D. A., Brown-Hughes T. (2010). African-American urban clergy’s literacy of Alzheimer’s disease. Social Work in Mental Health, 8, 254-266. doi: 10.1080/00981380902735033 [DOI] [Google Scholar]
- Stansbury K. L., Marshall G. L., Harley D. A., Nelson N. (2010). Rural African American clergy: An exploration of their attitudes and knowledge of Alzheimer’s disease. The Journal of Gerontological Social Work, 53, 352-365. doi: 10.1080/01634371003741508 [DOI] [PubMed] [Google Scholar]
- Stern Y. (2002). What is cognitive reserve? Theory and research application of the reserve concept. Journal of the International Neuropsychological Society, 8, 448-460. [PubMed] [Google Scholar]
- Stewart C. C., Boyle P. A., James B. D., Yu L., Han S. D., Bennett D. A. (2018). Associations of APOE ε4 with health and financial literacy among community-based older adults without dementia. The Journals of Gerontology, Series B: Psychological Sciences & Social Sciences, 73, 778-786. doi: 10.1093/geronb/gbw054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Suka M., Odajima T., Okamoto M., Sumitani M., Igarashi A., Ishikawa H., . . . Sugimori H. (2015). Relationship between health literacy, health information access, health behavior, and health status in Japanese people. Patient Education and Counseling, 98, 660-668. [DOI] [PubMed] [Google Scholar]
- Sun F., Gao X., Coon D. W. (2013). Perceived threat of Alzheimer’s disease among Chinese American older adults: The role of Alzheimer’s disease literacy. The Journals of Gerontology, Series B: Psychological Sciences & Social Sciences, 70, 247-257. doi: 10.1093/geronb/gbt095 [DOI] [PubMed] [Google Scholar]
- Suri V. R., Majid S., Chang Y.-K., Foo S. (2015). Assessing the influence of health literacy on health information behaviors: A multi-domain skills-based approach. Patient Education and Counseling, 99, 1038-1045. doi: 10.1016/j.pec.2015.12.017 [DOI] [PubMed] [Google Scholar]
- United Nations Educational, Scientific and Cultural Organization. (2005). Education for all: Literacy for life. Paris, France: Author. [Google Scholar]
- U.S. Department of Health and Human Services. (2000). Healthy people 2010 (2nd ed.) [With understanding and improving health (Vol. 1) and Objectives for improving health (Vol. 2)]. Washington, DC: U.S. Government Printing Office. [Google Scholar]
- Valle R., Yamada A.-M., Matiella A. C. (2006). Fotonovelas: A health literacy tool for educating Latino older adults about dementia. Clinical Gerontologist, 30, 71-88. doi: 10.1300/J018v30n01_06 [DOI] [Google Scholar]
- Vivot A., Glymour M., Tzourio C., Amouyel P., Chêne G., Dufouil C. (2015). Association of Alzheimer’s related genotypes with cognitive decline in multiple domains: Results from the Three-City Dijon study. Molecular Psychiatry, 20, 1173-1178. doi: 10.1038/mp.2015.62 [DOI] [PubMed] [Google Scholar]
- Wilson R. S., Yu L., James B. D., Bennett D. A., Boyle P. A. (2017). Association of financial and health literacy with cognitive health in old age. Aging, Neuropsychology, and Cognition, 24, 186-197. doi: 10.1080/13825585.2016.1178210 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff J. L., Spillman B. C., Freedman V. A., Kasper J. D. (2016). A national profile of family and unpaid caregivers who assist older adults with health care activities. JAMA Internal Medicine, 176, 372-379. doi: 10.1001/jamainternmed.2015.7664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xavier A. J., d’Orsi E., de Oliveira C. M., Orrell M., Demakakos P., Biddulph J. P., Marmot M. G. (2014). English longitudinal study of aging: Can Internet/e-mail use reduce cognitive decline? The Journals of Gerontology, Series A: Biological Sciences & Medical Sciences, 69, 1117-1121. doi: 10.1093/gerona/glu105 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yaffe K., Falvey C., Harris T. B., Newman A., Satterfield S., Koster A., . . . Simonsick E. (2013). Effect of socioeconomic disparities on incidence of dementia among biracial older adults: Prospective study. The British Medical Journal, 347, Article f7051. doi: 10.1136/bmj.f7051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yu L., Wilson R. S., Schneider J. A., Bennett D. A., Boyle P. A. (2017). Financial and health literacy predict incident Alzheimer’s disease dementia and pathology. Journal of Alzheimer’s Disease, 56, 1485-1493. doi: 10.3233/JAD-161132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zarcadoolas C., Pleasant A., Greer D. S. (2009). Advancing health literacy: A framework for understanding and action (Vol. 45). San Francisco: John Wiley. [Google Scholar]
- Zheng X., Woo B. K. (2016). Association between recognizing dementia as a mental illness and dementia knowledge among elderly Chinese Americans. World Journal of Psychiatry, 6, 233-238. doi: 10.5498/wjp.v6.i2.233 [DOI] [PMC free article] [PubMed] [Google Scholar]