Abstract
Although some atypical types of transient left ventricular apical ballooning syndrome have been reported, only a few atypical types of transient mid-ventricular ballooning have been reported. A 70-year-old female underwent surgery for urothelial carcinoma. At day 5 after the surgery, she was admitted to our department without cardiac symptoms because of ST elevation in leads I, II, III, aVF and V1–V6 indicating acute coronary syndrome. She was diagnosed with stress induced cardiomyopathy based on an angiographically normal coronary artery, newly developed extensive wall motion abnormality (hyperbasal contraction and akinesis from the mid-left ventricle to the apex without hypercontraction of the small area adjacent to the apex) based on left ventriculography, and a small elevation of myocardial enzymes incongruous with the area of contraction abnormality. Myocardial scintigraphy with 99mTc-tetrofosmin showed a severely reduced myocardial perfusion in an extensive mid-ventricular area without a left ventricular base and top of apex, in accord with a wall motion abnormality different from typical apical ballooning or typical mid-ventricular ballooning previously diagnosed in our hospital. This is the first report presenting an atypical mid-ventricular ballooning based on the myocardial atypical perfusion findings.
Keywords: Stress induced cardiomyopathy, Atypical mid-ventricular ballooning, Myocardial perfusion
Introduction
Transient left ventricular apical ballooning syndrome (ABS) is a cardiac syndrome characterized by transient left ventricular (LV) dysfunction with chest discomfort, electrocardiographic changes, and minimal release of myocardial enzymes, together mimicking acute myocardial infarction 1, 2, 3. Moreover, a variant of transient mid-LV ballooning has been reported 4, 5. Here, we report a case of atypical morphology and myocardial perfusion with mid-ventricular ballooning using myocardial scintigraphy.
Case report
In May 2010, a 70-year-old female underwent surgery for urothelial carcinoma. At day 5 after the surgery, she was admitted to our department without cardiac symptoms because of ST segment elevation in lead II of the electrocardiogram. She suffered from hypertension, diabetes mellitus type II, and diabetic nephropathy. Physical examination showed no peripheral edema of the lower limbs and no signs of raised jugular venous pressure. Heart rate was regular, 101 beats/min, and arterial blood pressure was 132/79 mmHg. Auscultation of the lungs and the heart revealed no inspiratory rales. A 12-lead electrocardiogram showed ST elevation in leads I, II, III, aVF, and V1–V6 indicating the diagnosis of extensive acute anterior septal ST elevation myocardial infarction (Fig. 1). Although emergency coronary angiography revealed a normal coronary artery, left ventriculography showed hyperbasal contraction and akinesis from the mid-left ventricle to the apex, except for hypercontraction of the small area adjacent to the apex (Fig. 2 and Video 1).
Figure 1.
Twelve lead electrocardiogram showed ST elevations in I, II, III, aVF and VI–V6 leads.
Figure 2.
Left ventriculography showed hyperbasal contraction, akinesis from the mid-left ventricle to the apex without hypercontraction of the small area adjacent to the apex.
A slightly damaged myocardium was indicated by a peak creatine phosphokinase level of 239 U/L and a peak tropinin I level of 3.33 ng/mL.
She was diagnosed with stress-induced cardiomyopathy based on an angiographically normal coronary artery, newly developed extensive wall motion abnormality, and a small elevation of myocardial enzymes incongruous with the area of contraction abnormality. At day 3 after the onset of stress-induced cardiomyopathy, myocardial scintigraphy with 99mTc-tetrofosmin (Tf) was performed. The area of reduced myocardial uptake showed an extensive mid-ventricular area except for a LV base and top of apex in accord with the wall motion abnormality (Fig. 3).
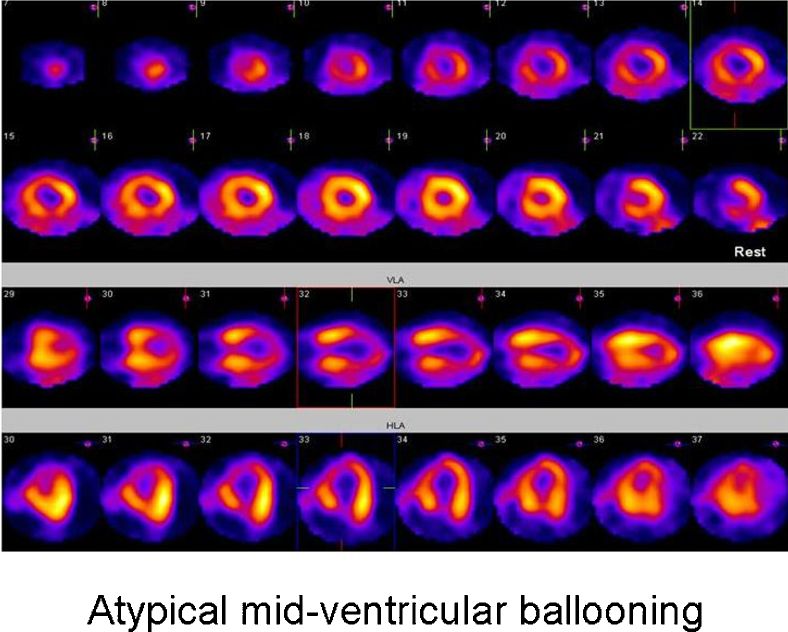
Figure 3.
Myocardial scintigraphy with 99mTc-Tf showed reduced myocardial uptake in an extensive mid-ventricular area without a left ventricular base and top of apex.
ST segment elevation was normalized without giant negative T waves at day 4, and wall motion abnormality was normalized with watchful waiting for 30 days after the onset of mid-ventricular ballooning.
Discussion
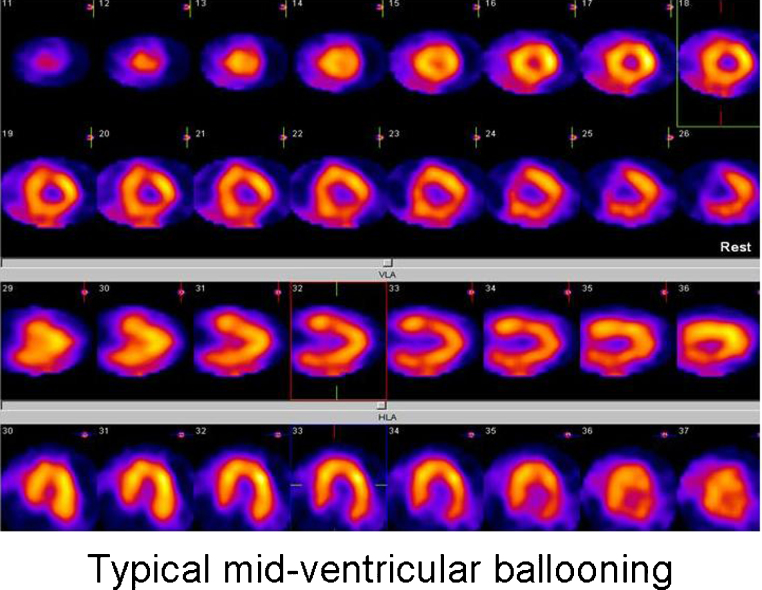
The present case showed transient mid-ventricular myocardial damage except for the small area adjacent to the LV apex, consistent with wall motion abnormality and myocardial perfusion abnormality. We believe that the patient belonged to mid-ventricular ballooning rather than ABS based on the observation considering that the top of the apex did not show ballooning insistently. Wall motion abnormality previously reported in many patients with typical mid-ventricular ballooning demonstrated mid-ventricular dilatation and akinesis with a hypercontractile LV apex and base 4, 5, 6. The typical mid-ventricular ballooning previously diagnosed in our hospital demonstrated mid-ventricular dilatation and akinesis with a hypercontractile LV apex and base (Video 2). We would like to emphasize that the characteristic of the wall motion in this case is different from the wall motion abnormality in typical mid-ventricular ballooning because of the difference in the area of hypercontraction in the LV apex.
Abe et al. reported that there was a significantly decreased myocardial uptake at the apex of the left ventricle in typical ABS using 99mTc-Tf study [1]. Similarly, ABS previously diagnosed in our hospital demonstrated a completely defective perfusion at the apex using 99mTc-Tf study (Fig. 4). However, the patient demonstrated severely reduced myocardial perfusion in the mid-ventricular and the apex except for the top of the apex. Therefore, we believe that the patient belonged to mid-ventricular ballooning rather than ABS based on the observation considering that the myocardial perfusion at the top of the apex was preserved insistently.
Figure 4.
Myocardial scintigraphy with 99mTc-Tf showed typical apical ballooning previously diagnosed in our hospital.
In a few reports, mid-ventricular ballooning diagnosed with 99mTc-Tf perfusion study demonstrated myocardial perfusion abnormality was limited in narrow basal and mid-ventricular area and maintained almost normally in the apical area 5, 7, 8. Similarly, previously diagnosed mid-ventricular ballooning in our hospital demonstrated moderately reduced perfusion in the small area of the mid-ventricle using 99mTc-Tf study (Fig. 5). However, myocardial reduced uptake area in this patient expanded to a wide range in the mid-ventricle and the apex indicating that the patient belonged to atypical mid-ventricular ballooning. We cannot fully conclude that the case is atypical mid-ventricular ballooning because there are not many reports showing myocardial perfusion with 99mTc single photon emission computed tomography in typical mid-ventricular ballooning. Therefore, we have to admit that there is insufficient evidence supporting that the patient had atypical mid-ventricular ballooning solely based on the information on myocardial perfusion abnormality. While inconclusive, we would like to suggest the possibility of atypical mid-ventricular ballooning because of the characteristics of the wall motion and the myocardial perfusion. Atypical patterns of apical ballooning have been reported in a few articles 3, 4. Furthermore, few cases of atypical patterns of mid-ventricular ballooning have been reported with the exception of atypical mid-ventricular ballooning with a posterior basal wall motion abnormality [5].
Figure 5.
Myocardial scintigraphy with 99mTc-Tf showed typical mid-ventricular ballooning previously diagnosed in our hospital.
Atypical mid-ventricular ballooning by scintigraphical evaluation has not been reported. We have to recognize scintigraphical evaluation as an effective complementary method combined with echocardiographical or left ventriculographic evaluation rather than a sufficient method in order to prove atypical types or subtypes of stress-induced cardiomyopathy. Our hypothesis regarding the cellular mechanism of stress-induced cardiomyopathy is that high levels of circulating epinephrine trigger a switch in intracellular signal trafficking in ventricular cardiomyocytes from Gs- to Gi-protein signaling via the β adrenergic receptor [9]. Atypical stress-induced cardiomyopathy based on atypical mid-ventricular ballooning may be associated with atypical β receptor signaling. Conversely, the localized defect of perfusion using 99mTc-Tf study cannot be explained by only systemic mechanisms and consideration of local factors is needed. From this viewpoint, we should have performed not only 99mTc-Tf scintigraphy but also cardiac iodine-123 metaiodobenzylguanidine scintigraphy to demonstrate the presence of atypical β receptor signaling.
Footnotes
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.jccase.2012.05.001.
Appendix A. Supplementary data
The following are the supplementary data to this article:
Atypical mid-ventricular ballooning in the present case.
Typical mid-ventricular ballooning previously diagnosed in our hospital.
References
- 1.Abe Y., Kondo M., Matsuoka R., Araki M., Dohyama K., Tanio H. Assessment of clinical features in transient left ventricular apical ballooning. J Am Coll Cardiol. 2003;41:737–742. doi: 10.1016/s0735-1097(02)02925-x. [DOI] [PubMed] [Google Scholar]
- 2.Bybee K.A., Kara T., Prasad A., Lerman A., Barsness G.W., Wright R.S., Rihal C.S. Systematic review: transient left ventricular apical ballooning: a syndrome that mimics ST-segment elevation myocardial infarction. Ann Intern Med. 2004;141:858–865. doi: 10.7326/0003-4819-141-11-200412070-00010. [DOI] [PubMed] [Google Scholar]
- 3.Tsuchihashi K., Ueshima K., Uchida T., Oh-mura N., Kimura K., Owa M., Yoshiyama M., Miyazaki S., Haze K., Ogawa H., Honda T., Hase M., Kai R., Morii I. Transient left ventricular apical ballooning without coronary artery stenosis: a novel heart syndrome mimicking acute myocardial infarction. Angina pectoris-myocardial infarction investigations in Japan. J Am Coll Cardiol. 2001;38:11–18. doi: 10.1016/s0735-1097(01)01316-x. [DOI] [PubMed] [Google Scholar]
- 4.Hurst R.T., Askew J.W., Reuss C.S., Lee R.W., Sweeney J.P., Fortuin F.D., Oh J.K., Tajik A.J. Transient midventricular ballooning syndrome: a new variant. J Am Coll Cardiol. 2006;48:579–583. doi: 10.1016/j.jacc.2006.06.015. [DOI] [PubMed] [Google Scholar]
- 5.Kurowski V., Kaiser A., von Hof K., Killermann D.P., Mayer B., Hartmann F., Schunkert H., Radke P.W. Apical and midventricular transient left ventricular dysfunction syndrome (tako-tsubo cardiomyopathy): frequency, mechanisms, and prognosis. Chest. 2007;132:809–816. doi: 10.1378/chest.07-0608. [DOI] [PubMed] [Google Scholar]
- 6.Aubert J.M., Ennezat P.V., Tricot O., Darchis J., Bauchart J.J., Auffray J.L., Lesenne M., Van Belle E., Goldstein P., Asseman P. Mid-ventricular ballooning heart syndrome. Echocardiography. 2007;24:329–334. doi: 10.1111/j.1540-8175.2007.00399.x. [DOI] [PubMed] [Google Scholar]
- 7.Davis M., Hardebeck C. Reverse Takotsubo syndrome diagnosed with Tc-99m SPECT perfusion study. J Nucl Cardiol. 2009;16:999–1002. doi: 10.1007/s12350-009-9089-6. [DOI] [PubMed] [Google Scholar]
- 8.Yoshikawa M., Yamamoto T., Shirakabe A., Ohno T., Tanaka K. Myocardial scintigraphy in a patient with transient mid-ventricular ballooning cardiomyopathy: case report. Int J Cardiol. 2007;119:e8–e10. doi: 10.1016/j.ijcard.2007.01.076. [DOI] [PubMed] [Google Scholar]
- 9.Kurowski V., Kaiser A., von Hof K., Killermann D.P., Mayer B., Hartmann F., Schunkert H., Radke P.W. Stress (Takotsubo) cardiomyopathy – a novel pathophysiological hypothesis to explain catecholamine-induced acute myocardial stunning. Nat Clin Pract Cardiovasc Med. 2008;5:22–29. doi: 10.1038/ncpcardio1066. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Atypical mid-ventricular ballooning in the present case.
Typical mid-ventricular ballooning previously diagnosed in our hospital.