Abstract
Osteofibrous dysplasia is a benign fibro-osseous lesion of bone which is most commonly occurred in cortical bone of anterior mid-shaft of the tibia of infancy and childhood. This study reported a case of osteofibrous dysplasia arising in the humerus of adult, resulting in good prognosis after a surgical treatment. A 34-year-old male had felt left upper arm pain and was suspected as having a bone tumor at the humeral shaft by X-ray pictures. The tumor was suspected as the osteofibrous dysplasia of the humerus by a core needle biopsy. Intralesional curettage, intraoperative anhydrous ethanol therapy, and artificial bone graft were performed. Surgical specimens showed fibro-osseous lesion, which strongly indicated osteofibrous dysplasia. Seven years after the surgery, he has lived without any local recurrence and complaints. It is important to recognize that osteofibrous dysplasia can arise in the humerus of an older patient for appropriate diagnosis.
Keywords: Osteofibrous dysplasia, humerus, ossifying fibroma, anhydrous ethanol
Introduction
Osteofibrous dysplasia (OFD) is a benign fibro-osseous lesion also referred to as ossifying fibroma of the long bones.1 It comprises 0.2% of all primary bone tumors.2 It is most commonly detected during infancy and childhood, and the cortical bone of the anterior mid-shaft of the tibia is the most frequent site.1 Frangenheim3 reported the first case of this disease as congenital osteitis fibrosa in 1921, and Kempson4 revised it to ossifying fibroma of the long bones with a differentiating form of fibrous dysplasia (FD) in 1966. Campanacci5 proposed the term “osteofibrous dysplasia” as a clinical entity in 1976. The histopathology shows irregular fragments of woven bone rimmed by osteoblast and fibrous components that consist of bland spindle cells with collagen production.1,5 Surgical treatment for OFD is controversial due to the rarity of the condition and variation in its progression.1,2 In cases with a risk of significant deformity, pathological fracture, or severe symptoms, a definitive diagnosis, as well as surgical treatment, is needed.1,5
In most cases, OFD occurs in the tibia and/or fibula.1,5 Involvement of other long bones, such as the humerus, is extremely rare, with only three previous reports.6–8 We report a case of OFD arising in the humerus, with a good prognosis after surgical treatment.
Case report
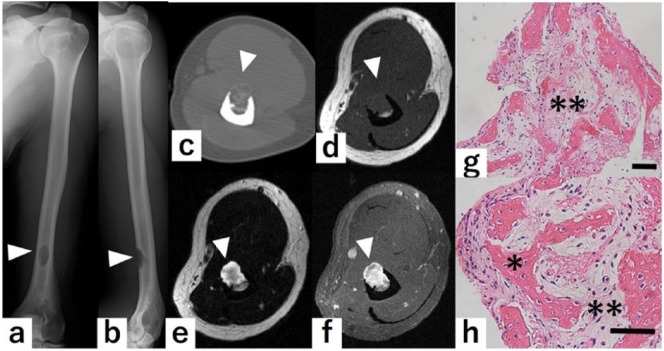
A 34-year-old male had upper arm pain, which persisted for 3 months; he had no history of arm trauma. He was suspected of having a bone tumor of the humeral shaft based on X-ray images and was referred to our hospital. At the initial visit, physical examination revealed a tenderness in the distal part of the upper arm with no swelling or restriction in the range of motion in the elbow joint. Plain X-ray images showed an osteolytic lesion with slight marginal sclerosis in the anterior cortical bone of the distal part of the humeral shaft (Figure 1(a) and (b)). A computed tomography (CT) scan revealed calcifications as well as marginal sclerosis in the lesion. Although the lesion protruded to the anterior side, it did not break the anterior cortical wall of the humerus and there was no invasion of the soft tissues (Figure 1(c)). The lesion had an intermediate signal intensity on T1-weighted magnetic resonance imaging (MRI) images and high signal intensity on T2-weighted images, and was enhanced by an injection of gadolinium (Figure 1(d)–(f)). The differential diagnosis was OFD, FD, classic adamantinoma, OFD-like adamantinoma, and non-ossifying fibroma (NOF). A core needle biopsy was performed under local anesthesia. The histological appearance showed a fibro-osseous lesion without malignancy, which could exclude NOF. Surgical treatment was performed for a definitive diagnosis and pain relief. A linear skin incision was made on the scar from the needle biopsy. After splitting the biceps brachii muscle, the bone tumor was curetted. The pathological diagnosis during surgery was the same as the core needle biopsy. After curettage, the cavity was painted with anhydrous ethanol for 5 min (intraoperative anhydrous ethanol therapy), and a graft using 2 g of artificial bone (OSferion; Olympus Co., Tokyo, Japan) was performed. Surgical specimens showed a fibro-osseous lesion and irregular fragments of woven bone rimmed with osteoblasts. There were many spindle-shaped osteoblasts in the fibrous component (Figure 1(g) and (h)), which strongly indicated OFD. He was free to use the right arm just after surgery. Seven years later, he has had no recurrence or symptoms (Figure 2(a) and (b)).
Figure 1.
Image analyses of the humerus and histological appearance of the tumor: Plain radiograph of (a) anteroposterior view and (b) lateral view shows an osteolytic lesion with slight marginal sclerosis in the anterior cortical bone of the distal part of the humeral shaft. (c) Computed tomography image revealed calcifications as well as marginal sclerosis in the lesion. The lesion protruded to the anterior side without breaking the anterior cortical wall of the humerus. Magnetic resonance imaging images show (d) intermediate signal intensity on T1-weighted images and (e) high signal intensity on T2-weighted images of the lesion. (f) The lesion was well enhanced with T1 fat suppression with an injection of gadolinium, axial image. Hematoxylin and eosin stained surgical specimen (g: 100×, h: 200×) shows fibro-osseous lesion with irregular fragments of woven bone rimmed by osteoblasts (*). Many spindle-shaped osteoblasts are observed in the fibrous component (**). Zonal architecture and storiform pattern were not detected. Arrow heads indicate the tumor. Scale bar = 200 µm.
Figure 2.

Plain radiograph of the humerus in 7 years after operation: Plain radiograph of (a) anteroposterior view and (b) lateral view shows no osteolytic lesion that shows recurrence.
Discussion
OFD is a benign fibro-osseous lesion which most commonly occurs in the anterior cortex of the proximal or middle third of the tibia,1 and the ipsilateral fibula is involved in about 20% of cases.1,5 OFD occurs almost exclusively in the tibia and fibula, and the involvement of other bones is extremely rare.1,5,9 The ulna, radius, clavicle, and humerus have been reported as unusual locations for OFD.5,9–11 Wang et al.9 reported cases of OFD arising in the ulna in a 7-year-old patient and in the radius in an 18-year-old patient. Ozaki et al.10 reported a case of OFD in which lesions were observed in the bilateral tibia and ulna and the right fibula. Gopinathan et al.11 reported a case of OFD arising in the clavicle. To the best of our knowledge, there are only three previous reports of OFD arising in the humerus (Table 1).6–8 In all cases, the tumor occurred in the diaphysis of the humerus in a teenager. Treatment methods for these cases were inconsistent, and the outcomes and follow-up could not be determined. In our case, although the tumor occurred in the diaphysis, as was the case in the previous reports, the patient was much older (34 years).
Table 1.
Literature review of osteofibrous dysplasia arising in the humerus.
| Authors | Age (years), gender | Location | Treatment |
|---|---|---|---|
| Schlitter6 | 12, male | Diaphysis | Uncertain |
| Blauth et al.7 | 13, female | Diaphysis | Extraperiosteal resection, autogenous bone graft, Kuntscher nail |
| Sissons et al.8 | 13, male | Diaphysis | Curettage, autogenous bone graft |
| Our case | 34, male | Diaphysis | Curettage, anhydrous ethanol therapy, artificial bone graft |
OFD is most commonly detected during the first two decades of life.1 However, there are some cases of OFD occurring in adults. Almeida et al.12 reported a case of OFD in the tibia of a 45-year-old female who was treated using curettage, bone grafting, and bone cement. Hahn et al.13 reported 65-year-old case of OFD treated by using en bloc excision. In addition, Park et al.14 reported seven OFD cases that occurred in patients over 20 years of age in a series of 80 cases. Although OFD stabilizes at around 15 years old and is followed by spontaneous healing,1,5,9 some cases have been detected after bone maturation,12–14 which indicates that OFD should not be excluded from the differential diagnosis of a bone tumor in adults.
The histopathology of OFD includes fibro-osseous lesions, with irregular fragments of woven bone rimmed by well-defined osteoblasts.1,5 Zonal architectures, which are characterized by delineation with thin and woven bone or fibrous tissue predominantly in the center of the lesion with more abundant anastomoses and lamellar bone peripherally, are also observed.1,5 The fibrous tissue also has a whorled, storiform pattern.5 In our case, the surgical specimen had fibro-osseous lesions including irregular fragments of woven bone rimmed by osteoblasts and many spindle-shaped osteoblasts in the fibrous component. However, there was no zonal architecture or storiform pattern evident because the specimens were removed by curette and the structures were crushed. However, OFD could be diagnosed by histological features as well as image findings.
In general, the main differential diagnosis for OFD is FD or adamantinoma.5 FD is a benign fibro-osseous lesion that occurs in adults and children.1 Although it occurs in almost any part of the bones, the craniofacial bone and the femur are the two most common sites.1,5 FD presents with endomedullary development in contrast with OFD, which occurs in the cortical bone.1,5 Its histopathology shows fibro-osseous lesions. The osseous component comprised irregular, curvilinear, trabeculae of woven bone. The woven bone is not rimmed by osteoblasts, in contrast with OFD.5 Adamantinoma is a low-grade malignant bone tumor which frequently occurs in the tibia in young to middle-aged adults.1 There are two types of adamantinoma, including classical (the more aggressive type) and differentiated (the more benign form). The latter one resembles OFD (OFD-like adamantinoma).1 The relationship between OFD and adamantinoma is important because they are in the same spectrum of diseases, and OFD is known to progress into adamantinoma in some cases.1,15 Therefore, it is difficult to differentiate the two diseases only by histologic analysis.15 In our case, FD was ruled out because the tumor was in the cortical bone, and woven bone rimmed by osteoblasts was observed histologically. However, the possibility of OFD-like adamantinoma should be considered in cases like ours. Therefore, this case requires careful observation for a long time.
It is known that OFD should not be treated surgically before bone maturity because the lesion may heal spontaneously and there is a high probability of recurrence after surgery.9,13,14 Surgery for the treatment of OFD is controversial.1,2 Although curettage and en bloc excision with bone grafting are treatment options for OFD, frequent recurrence has been reported.13,16 Lee et al.16 reported 16 cases in which recurrence occurred in 6 cases after curettage, and therefore recommended extraperiosteal excision as the surgical treatment for OFD. On the contrary, Ozaki et al.17 reported good results in six cases treated with curettage and bone grafting.
Recently, the safety and effectiveness of anhydrous ethanol for adjuvant therapy after intraregional curettage of bone tumor has been reported.18–20 In a locally aggressive tumor, Oh et al.18 and Solooki et al.19 reported that anhydrous ethanol treatment after curettage reduced local recurrence rate in giant cell tumor and aneurysmal bone tumor, respectively. In benign tumors, Cha et al.20 reported the efficacy of anhydrous ethanol for the treatment of enchondroma. However, there is no previous report regarding the use of anhydrous ethanol for OFD. In our case, intraoperative adjuvant therapy using anhydrous ethanol after curettage was effective and there has been no local recurrence for 7 years.
Conclusion
We reported an extremely rare case of OFD arising in the humerus of an adult patient that was treated with intralesional curettage, anhydrous ethanol therapy, and an artificial bone graft. This is the fourth case of OFD arising in the humerus that we know of, and the first case of OFD treated with anhydrous ethanol as intraoperative adjuvant therapy. It is important to recognize that OFD can arise in the humerus of an older patient, and anhydrous ethanol can be a treatment option.
Acknowledgments
The authors wish to thank Fumiyoshi Fujishima for reviewing the pathological diagnosis. S.Y. wrote the article. Masah. H., Masam. H., Mu. W., and K.H. treated the patient. S.H. performed the radiological diagnosis of the case. Mi. W. performed the pathological diagnosis of the case. Y.H. and E.I. supervised the writing of the article. All of them met all four criteria for authorship per International Committee of Medical Journal Editors (ICMJE) recommendations.
Footnotes
Conflict of interest: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The authors confirm that Ethical Committee approval was sought where necessary and is acknowledged within the text of the submitted manuscript.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: The authors confirm that informed consent to report an individual case has been sought, and a statement regarding whether written informed consent for patient’s information and images to be published has been provided by the patient and has been included within the text of the submitted manuscript.
References
- 1. Fletcher CDM, Bridge JA, Hogendoorn PCW, et al. WHO classification of tumors of soft tissue and bone. 4th ed. Lyon: International Agency for Research on Cancer (IARC), 2013, pp. 343–355. [Google Scholar]
- 2. Abraham VT, Marimuthu C, Subbaraj R, et al. Osteofibrous dysplasia managed with extraperiosteal excision, autologous free fibular graft and bone graft substitute. J Orthop Case Rep 2015; 5(1): 41–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Frangenheim P. Angeborene Ostitis fibrosa als Ursache einer intrauterinen Unterschenkelfraktur. Arch Klin Chir 1921; 117: 22–29 (In German). [Google Scholar]
- 4. Kempson RL. Ossifying fibroma of the long bones. A light and electron microscopic study. Arch Pathol 1966; 82(3): 218–233. [PubMed] [Google Scholar]
- 5. Campanacci M. Osteofibrous dysplasia of long bones. A new clinical entity. Ital J Orthop Traumatol 1976; 2(2): 221–237. [PubMed] [Google Scholar]
- 6. Schlitter HE. Zwei benigne Knochentumoren mit seltener Lokalisation und Spontanfraktur. Fortschr Geb Röntgenstr Nuklearmed 1958; 88(2): 195–200. [PubMed] [Google Scholar]
- 7. Blauth W, Meves H. Behandlungsprobleme bei der “aggressiven” Form der fibrösen Dysplasie. Z Orthop Ihre Grenzgeb 1974; 112(2): 230–235. [PubMed] [Google Scholar]
- 8. Sissons HA, Kancherla PL, Lehman WB. Ossifying fibroma of bone. Report of two cases. Bull Hosp Jt Dis Orthop Inst 1983; 43(1): 1–14. [PubMed] [Google Scholar]
- 9. Wang J-W, Shih C-H, Chen W-J. Osteofibrous dysplasia (ossifying fibroma of long bones). A report of four cases and review of the literature. Clin Orthop Relat Res 1992; 278: 235–243. [PubMed] [Google Scholar]
- 10. Ozaki T, Hamada M, Taguchi K, et al. Polyostotic lesions compatible with osteofibrous dysplasia. A case report. Arch Orthop Trauma Surg 1993; 113(1): 46–48. [DOI] [PubMed] [Google Scholar]
- 11. Gopinathan NR, Prakash M, Saibaba B, et al. Osteofibrous dysplasia of clavicle clinically mimicking chronic osteomyelitis. Indian J Radiol Imaging 2016; 26(2): 290–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Almeida Herrero F, Silvestre Muñoz A, Martinez Rodriguez M, et al. Ossifying fibroma of long bones in adults: a case report. Acta Orthop Belg 2006; 72(6): 786–789. [PubMed] [Google Scholar]
- 13. Hahn SB, Kim SH, Cho NH, et al. Treatment of osteofibrous dysplasia and associated lesions. Yonsei Med J 2007; 48(3): 502–510. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Park YK, Unni KK, McLeod RA, et al. Osteofibrous dysplasia: clinicopathologic study of 80 cases. Hum Pathol 1993; 24(12): 1339–1347. [DOI] [PubMed] [Google Scholar]
- 15. Most MJ, Sim FH, Inwards CY. Osteofibrous dysplasia and adamantinoma. J Am Acad Orthop Surg 2010; 18(6): 358–366. [DOI] [PubMed] [Google Scholar]
- 16. Lee RS, Weitzel S, Eastwood DM, et al. Osteofibrous dysplasia of the tibia. Is there a need for a radical surgical approach? J Bone Joint Surg Br 2006; 88(5): 658–664. [DOI] [PubMed] [Google Scholar]
- 17. Ozaki T, Hamada M, Sugihara S, et al. Treatment outcome of osteofibrous dysplasia. J Pediatr Orthop B 1998; 7(3): 199–202. [DOI] [PubMed] [Google Scholar]
- 18. Oh JH, Yoon PW, Lee SH, et al. Surgical treatment of giant cell tumour of long bone with anhydrous alcohol adjuvant. Int Orthop 2006; 30(6): 490–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Solooki S, Keikha Y, Vosoughi AR. Can ethanol be used as an adjuvant to extended curettage in order to reduce the recurrence rate of aneurysmal bone cyst? Rev Bras Ortop 2016; 52(3): 349–353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Cha SM, Shin HD, Kim KC, et al. Extensive curettage using a high-speed burr versus dehydrated alcohol instillation for the treatment of enchondroma of the hand. J Hand Surg Eur Vol 2015; 40(4): 384–391. [DOI] [PubMed] [Google Scholar]