Abstract
Effective delivery of healthcare is highly interdependent within and between interprofessional (IP) care teams and the patients they serve. This is particularly true for complex health conditions such as advanced heart failure (AHF). Our Academic Practice Partnership received funding to carry out IP workforce development with inpatient AHF care teams. Our objectives were to (a) identify challenges in team functioning that affected communication and relationships among the AHF care teams, (b) collaboratively identify a focal work process in need of improvement, and (c) test whether facilitated implementation of team training and work process changes would lead to improvements in team communication, relationships, and process outcomes. The healthcare team identified implementation of structured IP bedside rounds (SIBR) as the preferred approach to improving collaborative care.
Utilizing a cross-sectional pre/post design changes in team communication and relationships before and after a team intervention that included TeamSTEPPS training and SIBR implementation using a validated Relational Coordination (RC) survey were assessed. The study population included AHF care team members (n~100) representing seven workgroups (e.g., nurses, pharmacists) from two inpatient cardiology units at a 450-bed academic medical center in the Pacific Northwest during 2015–2016.
Improvements in RC scores were demonstrated across all seven RC dimensions from baseline (Year 1) to follow-up (Year 2). Percent change on each of the seven dimensions ranged from 3.57%–9.85%. Changes were statistically significant for improvements between baseline and follow-up on all but one of the seven RC dimensions (shared knowledge).
The IP team intervention was associated with improvements in RC from baseline to follow-up. Additional research is needed to assess patient perspectives and outcomes of the IP team intervention. Findings of this study are consistent with the growing body of RC and SIBR research and provide a useful model of an IP team-based intervention in clinical practice.
Keywords: Interprofessional collaboration, professional relations, team-based care, team culture, health services research
Introduction
Because health care systems are complex, achieving positive outcomes for patients, healthcare teams, and health systems requires collaboration among multiple health professionals, the patient, and the family (Institute of Medicine, 2000; Institute of Medicine, 2012; Cox, Cuff, Brandt, Reeves, & Zierler, 2016). The need to transform practice to achieve Quadruple Aim goals is widely recognized and is particularly relevant in the management of advanced heart failure (AHF) care (Bodenheimer & Sinsky, 2014). The Quadruple Aim extends the Triple Aim goals of improving patient experience of care, improving health of populations, and reducing the per capita cost of health care by adding a focus on improvement of work-life for clinicians and staff (Berwick, Nolan, Whittington, 2008; Bodenhiemer & Sinsky, 2014). Heart failure (HF) is a particulary challenging diagnosis for patients and healthcare teams as the patient’s status is constantly in flux and care is highly interdependent within and between IP care teams (Von der Heidt et al., 2014). HF is a progressive illnessthat transitions to AHF when patients with HF “experience persistent severe symptoms that interfere with daily life despite maximum evidence-based medical therapy” (Colucci & Dunlay, 2018). Despite the importance of team-based care, relatively little attention has been paid to assessing and intentionally improving the quality of team functioning (Cox, et al., 2016; Reeves, Pelone, Harrison, Goldman, & Zwarenstein, 2017).
Relational Coordination (RC) is a theory of organizational performance used across industries including aviation, banking, manufacturing, and healthcare that describes the management of interdependence between tasks and people (Gittell, Cameron, Lim, & Rivas, 2006; Gittell, Godfrey, & Thistlethwaite, 2013). Relational Coordination is defined as “coordinating work through relationships of shared goals, shared knowledge, and mutual respect.” (Gittell et al., 2006, p. 74). The concept of RC was first identified in a study of flight departure times within the commercial aviation industry (Gittell, 2003) and has since been found to be extremely relevant in patient care settings where work is highly interdependent, uncertain, and time-constrained (Azar et al., 2017; Gittell et al., 2000; Gittell, Beswick, Goldmann, & Wallack, 2015; Manski-Nankervis et al., 2014). This study describes changes to RC scores following an IP team intervention that included Team Strategies and Tools to Enhance Performance and Patient Safety (TeamSTEPPS) communication training, quarterly leadership workshops, and the implementation of structured IP bedside rounding (SIBR) processes to improve AHF care team communication and relationships in an inpatient setting (Zierler et al., 2018; TEAMSTEPPS, n.d.). Structured Interprofessional Bedside Rounds is a team process that brings multiple health care disciplines together at the patient’s bedside, using a structured format to collaborate and develop a daily plan of care with the patient and family (Burdick, Kara, Ebright, & Meek, 2017; Gonzalo, Wolpaw, Lehman, & Chuang, 2014; White, 2013). Prior studies of SIBR have found associations between SIBR implementation and improved team communication, length of stay, and patient experience (Bhamidipati et al., 2016; O’Leary, et al., 2011; Ratelle et al., 2018).
Background
The IP Learning Continuum Model (Cox et al., 2016) and the Relational Model of Organizational Change (Gittell et al., 2013; Relational Model of Change, n.d.) guided this study. The IP Learning Continuum Model situates practice-based care transformation efforts as part of a continuum of IP education. The model describes a spectrum from foundational learning among prelicensure learners (e.g., medical students, nursing students) through graduate education (e.g., nurse practitioner students, residents) to continuing professional development (with clinical team members in practice). Highlighted in the Institute of Medicine report, where the model was first published, was the need to move IP education and collaborative practice research into clinical settings (Cox et al., 2016). The IP healthcare and education field has responded to this and earlier charges with tremendous growth of IPE in clinical practice (continuing professional development) (Cox et al., 2016; Paradis & Reeves, 2012). Cox et al. (2016) and other articles lay out not only the growing body of evidence connecting IP education and collaborative practice to Quadruple Aim goals but also highlight the need for additional work in this area that is theory-driven and rigorous (Brandt, Lutfiyya, King, & Chioreso, 2014; Havens, Gittell, & Vasey, 2018; Reeves, Clark, Lawton, Ream, & Ross, 2017; Reeves, Pelone, et al., 2017).
The Relational Model of Organizational Change builds on earlier RC theory of the importance of shared goals, shared knowledge and relationships to successful coordination in work environments (Gittell, et al., 2006; Gittell, et al., 2013). The Relational Model of Organizational Change was first published in 2013 as a way to think about improving RC in teams and describe relationships between “relational, structural, and work process interventions as leverage points for changing deep-seated patterns of interaction” (Gittell, et al., 2013; Relational Model of Change, n.d.). The concept of RC has been operationalized as a fully validated survey with documented internal consistency, interrater agreement and reliability, structural validity and content validity (RC Survey Validation, n.d.; Gittell, 2003; Gittell, Seidner, and Wimbush, 2010). The RC survey has seven dimensions—four of which measure the frequency, timeliness, accuracy, and problem-solving nature of communication and three of which asses the quality of the underlying relationships: specifically the degree of shared goals, shared knowledge, and mutual respect. Prior studies have shown positive, significant relationships between RC in the quality and efficicency of work (e.g. in airlines as well as patient car) (Cramm & Nieboer, 2012; Gittell et al, 2008; Havens, Vasey, Gittell, 2018;). For example, Cramm and Nieboer found positive associations between RC score and quality of chronic care delivery in outpatient settings (self-management support r=0.217, p<0.01, decision support r=0.190, p<0.01) while Gittell, et al. (2008) found lower RC scores to be associated with excess length of stay (r=−0.46, p<0.01) in inpatient areas. More recently, Havens, et al., (2018) found positive relationships between RC and personal efficacy and job satisfaction among hospital nurses (efficacy: r=0.25, p=0.00; job satisfaction: r=0.27, p=0.00). However, few studies have specifically examined change in RC scores over time following an intervention aimed at improving team communication and relationships.
The impetus for this study was a desire to improve team functioning and efficiency of work among inpatient AHF care teams at a large academic medical center in the Pacific Northwest. The AHF care teams were encountering challenges with team communication, task integration, readmission rates, and poor nurse satisfaction as identified during a required needs assessment conducted in preparation for writing a grant to support the study (Zierler et al., 2018). Heart Failure is a highly prevalent and complex illness that requires multiple professions to provide safe coordinated care. Currently, six million Americans, primarily older adults (≥75 years of age), have HF (Heidenreich et al., 2013). As the population ages, HF is increasingly prevalent, with over eight million people expected to be living with HF by 2030 (Heidenreich et al., 2013). Heart Failure is the most common cause for hospital admission and readmission in the United States—with nearly 25% of HF patients readmitted within 30 days (Avery et al., 2012; Suter, et al., 2014). HF treatments are also the most expensive of all Medicare diagnoses (Avery et al., 2012; Titler et al., 2008). Well-coordinated team-based care and communication are needed to ensure that patients are discharged at the right time with the right knowledge and resources to continue to thrive after going home (Browne, et al., 2014).
Advanced HF is diagnosed when a patient’s disease has progressed to the point that usual therapies are no longer effective (Colucci & Dunlay, 2018). Treatment for patients with AHF includes heart transplantation, implantation of a ventricular assist device, or palliative medical management. Heart transplantation or implantation of a ventricular assist devices are options only available to a small percentage of patients who medically qualify for the treatment. Care of patients with AHF requires good team communication as the patient’s health status is tenous and in constant flux. This paper is one of a series that helps answer the research question: “Can a purposeful IP team intervention improve communication and relationships among practicing health care teams?”
Methods
Methodology/Research design.
A cross-sectional pre/post design was utilized to assess change in team communication and relationships over time using a validated web-based RC survey (see Table 1). The primary outcomes of interest include changes in RC score at baseline (Time 1) and a one-year follow-up (Time 2) on an overall RC index as well as for each of the seven dimensions of RC using a 5-point Likert-type scale.
Table 1.
RC Questions Included in AHF Care Team Survey
| Dimensions | Survey Questions |
|---|---|
| 1. Frequent Communication | How frequently do people in each of these groups communicate with you about care implementation and management for advanced heart failure patients? |
| 2. Timely Communication | Do they communicate with you in a timely way about care implementation and management for advanced heart failure patients? |
| 3. Accurate Communication | Do they communicate with you accurately about care implementation and management for advanced heart failure patients? |
| 4. Problem solving communication | When there is a problem with care implementation and management for advanced heart failure patients, do people in each of these groups blame others or work with you to solve the problem? |
| 5. Shared goals | Do people in each of these groups share your goals for care implementation and management for advanced heart failure patients? |
| 6. Shared knowledge | Do people in each of these groups know about the work you do with care implementation and management for advanced heart failure patients? |
| 7. Mutual Respect | Do people in each of these groups respect the work you do with care implementation and management for advanced heart failure patients? |
Note: Respondents were asked to rate each of the workgroups (including their own) for each dimension using a 5-point Likert-type scale.
Identification of workgroups and focal work process.
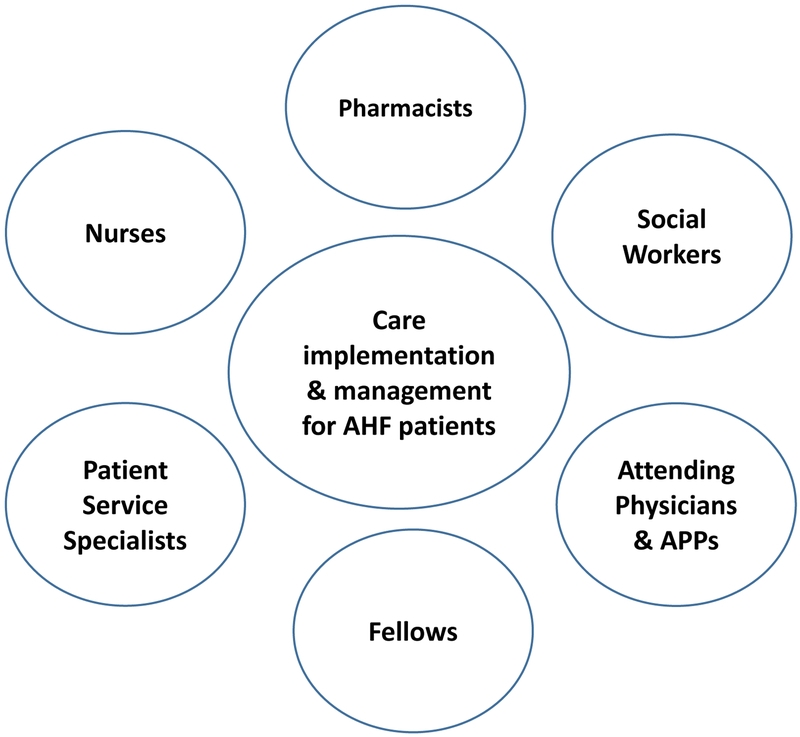
Using coaching and other interactive team facilitation approaches (Zierler et al., 2018), a small dedicated care team (called “the AHF Inpatient Change Team”) identified workgroups involved in AHF care (e.g., registered nurses (RNs), advanced practice providers (APPs), social workers, physicians, pharmacists) and a focal work process around which the workgroups need to communicate in their daily work (“care implementation and management for AHF patients”) (see Figure 1). Following definition of included workgroups and identification of a focal work process, a baseline RC survey was carried out in April/May 2015 (Time 1) with a one-year follow-up survey administered in May/June 2016 (Time 2).
Figure 1.
Workgroups and focal work process identified by AHF Care Teams for RC survey
IP Team Intervention.
Between the baseline survey (Time 1) and the one-year follow-up survey (Time 2) an IP team intervention was carried out that included quarterly leadership workshops to review baseline RC results and facilitated change management strategies that would help the team determine how to address the results. The team determined that changing the structure of morning rounds to be IP and to be carried out at the patient’s bedside as opposed to in a conference room or in the hallway (the previous practice) would help the team to improve the lowest RC scores (i.e. Timely Communication, Shared Knowledge). To help the team shift to the SIBR process the grant team partnered with the AHF care team to provide TeamSTEPPS training and simulated practice of the new SIBR process. Five four-hour IP team trainings occurred in March of 2016 and provided an opportunity to train all of the members of the IP care team (on the AHF units) together. The AHF Change Team members and department leadership participated in the quarterly leadership workshops, and all other members of the AHF care teams participated in the 4-hour TeamSTEPPS communication trainings and simulations of the SIBR process. A more detailed description of the team intervention is described by Zierler et al. (2018).
Study setting and survey participants.
Survey participants included healthcare professionals from two inpatient units—a step-down cardiovascular telemetry unit and a critical care unit (CCU)—both of which house AHF patients in partnership with the AHF service line. Professions represented in the two units included patient service specialists, registered nurses (RNs), social workers, pharmacists, advanced practice providers (nurse practitioners and/or physician assistants), and physicians (fellows and attendings). At the beginning of this project a single AHF provider service covered patients on both the cardiovascular telemetry unit as well as the CCU. During the first year of the project the single AHF service split into two distinct service lines—one team that managed step-down/telemetry patients and one team that managed patients in the CCU. The CCU and service are closed meaning the only service provided and patients attended to on this specific unit are critical care AHF patients. In contrast, multiple cardiology services have patients on the step-down cardiovascular telemetry floor (e.g. post-myocardial infarction, congenital cardiomyopathies). For this reason, only one provider workgroup was represented in the data (representing the original AHF service which is comprised of attending physicians and APP’s that continue to manage AHF patients on the step-down/telemetry unit).
Ethical considerations.
The context in which surveys were carried out was part of a larger quality improvement project. Human subjects approval was sought for this project and was deemed exempt. All results have been reported at aggregate levels to ensure confidentiality of individual responses.
Data collection.
Data were collected via confidential web-based surveys (delivered via email). Surveys of inpatient AHF care team members were carried out at baseline (Time 1) and at a one-year follow-up (Time 2); surveys were open for one month each in spring of 2015 and 2016. The entire population of inpatient AHF care team members were surveyed (as opposed to a sample). Participation was encouraged via flyers posted on the units, weekly email reminders, and periodic announcements at staff meetings. Participation was incentivized with $5 coffee cards (for all survey completers) and entry into a drawing to receive one of ten $50 gift cards.
The annual team surveys included the RC survey, the TeamSTEPPS Team Perception Questionnaire (TPQ) (results of TPQ will be reported elsewhere), and an open-ended question soliciting additional comments or feedback from participants. A total of fifty questions were asked each year—seven RC survey questions (each question included multiple workgroups; see Figure 1); forty-two TPQ questions; and one open-ended question. Survey completion was estimated to take fifteen to twenty minutes per respondent. This paper reports on the findings of the RC survey at baseline and at the one-year follow-up.
Data analysis.
Data were analyzed using Microsoft Excel 2013 and Stata version 14 statistical software (Stata Corporation Inc., College Station, TX, USA) to assess response rates for each workgroup as well as to calculate RC scores. Stata was used to carry out both the RC analysis for each year of data and the comparison of baseline and follow-up data. In carrying out these analyses, both complete and partial responses were included (e.g., if a respondent did not provide answers to all of the survey questions). Partial responses counted for approximately 5% of responses.
Relational Coordination was measured using the RC Survey. Relational Coordination data were analyzed according to the analytic procedures detailed by the instrument’s developer; permission was granted for use in this study for research purposes (Gittell, 2012). Relational Coordination data were first constructed at the individual respondent level for each of the seven dimensions of RC. Data was then aggregated to the group level (i.e. role) based on the seven dimensions (e.g. frequent, timely, accurate) and as an aggregate index (RC Index).
Within the RC literature, cut-points for strengths of ties have been established for scores to categorize them as weak (<3.5), moderate (3.5–4.0), or strong (>4.0) based on norms established from other data (RC Survey, 2017). Last updated with 2012–2015 data, terciles for each dimension of RC and the RC index (the aggregate of the seven dimensions) correspond to each partitioned third of aggregate RC survey data.
Internal consistency and structural validity.
Previous research has established Cronbach’s Alpha and Factor Analysis levels to determine RC index internal consistency and structural validity. These tests are recommended to be carried out as a first step in any RC analysis to determine whether further analysis is appropriate (Gittell, 2012). Cronbach’s alpha tests internal consistency of whether seven dimensions of RC belong in a single construct. The Crohnbach’s alpha for this dataset was 0.90 which exceeds the 0.80 needed for an already validated construct (Gittell, 2012). Factor analysis also confirmed that the seven dimensions of RC form a single factor and the RC index met the test of structural validity with factor loadings on Factor 1 for all seven dimensions were more than 0.95 and the proportion of variance captured by Factor 1 was 0.95. These results exceeded the minimum requirements for structural validity of at least 0.50 for factor loadings and above 0.80 for proportion of variance (Gittell, 2012). These tests provide preliminary evidence that RC in this study is a single factor construct with high internal consistency. These results are similar to previous studies that have used the RC construct and indicated that further analysis was appropriate (Gittell, 2012).
Comparison of Time 1 vs. Time 2.
To examine statistical differences in the RC index means at the two time points, two-sample t-tests and paired t-tests were performed. When respondents in Time 1 and Time 2 were not identical (i.e. group membership changed from Time 1 to Time 2), an independent group t-test was performed. When the variable of interest for comparison was collected from the same individual more than one time, and therefore the observations were not independent of one another, a paired t-test was performed. For example, a paired t-test was used for the analysis with the study sample of 44 survey respondents who participated in the survey at both Time 1 and Time 2 (see Appendix).
Results
Overall, 193 respondents completed the survey at Time 1 and Time 2 with an overall response rate of 52.4% (total n = 368; year 1: 93/185 = 50% response rate; year 2: 100/183 = 55% response rate) (see Table 2). Of those who completed the survey at Time 2 (n = 100), 44 (44%) had also completed the survey at Time 1.
Table 2.
Response Rates at Time 1 and Time 2
| Baseline (Time 1) | 1-Year Follow-Up (Time 2) | |||||
|---|---|---|---|---|---|---|
| Workgroups | Invited | Responded | Percentage | Invited | Responded | Percentage |
| RNs (Unit 1) | 58 | 40 | 69% | 65 | 40 | 62% |
| RNs (Unit 2)a | 95 | 30 | 32% | 68 | 28 | 41% |
| Patient Services Specialists (PSS) | 7 | 2 | 29% | 8 | 4 | 50% |
| Pharmacists | 3 | 2 | 67% | 7 | 4 | 57% |
| Social Workers | 1 | 1 | 100% | 3 | 3 | 100% |
| Fellows | 9 | 6 | 67% | 16 | 8 | 50% |
| Providersb | 12 | 12 | 100% | 16 | 13 | 81% |
| Total | 185 | 93 | 50% | 183 | 100 | 55% |
Numbers of invited Nurses in Unit 2 change from Year 1 to Year 2 due to a unit re-organization
Individuals in workgroups APPs and Attending Physicians were counted as Providers.
RC analysis and comparison of RC scores at Time 1 vs. Time 2.
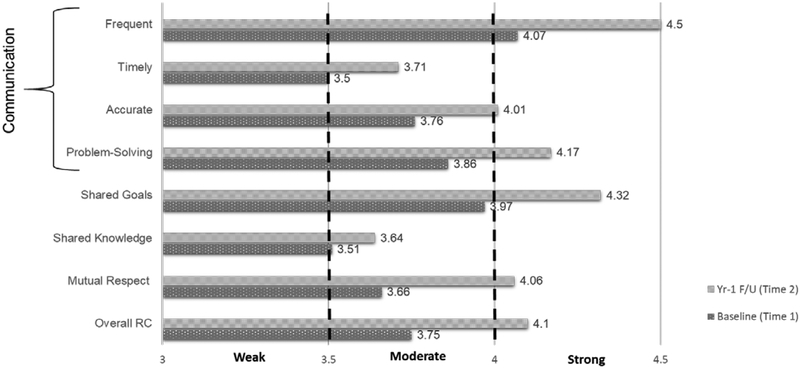
At Time 1 within RC scores for individual dimensions ranged from 3.50–4.07 with an overall RC index of 3.75 on a five-point scale from one (lowest) to five (highest) (see Figure 2 and Table 3). At Time 2, the overall RC index score ranged from 3.64–4.50 with an overall RC index of 4.10.
Figure 2.
Change in 7 RC dimensions and RC index from baseline (Time 1) to 1-year follow-up (Time 2) with cut-points for weak, moderate, and strong ties indicated
Table 3.
Independent Groups t-Test Comparisons of Seven RC Dimensions and Overall RC Index at Time 1 and Time 2
| Baseline (Time 1) |
Follow-Up (Time 2) |
|||||
|---|---|---|---|---|---|---|
|
Mean (SD) |
Mean (SD) |
Mean Difference | Percent Increase | t-test | p-value | |
| Frequent Communication | 4.07 (0.65) | 4.50 (0.61) | +0.43 | 9.55% | −4.77 | 0.000 |
| Timely Communication | 3.50 (0.60) | 3.71 (0.65) | +0.21 | 5.67% | −2.30 | 0.022 |
| Accurate Communication | 3.76 (0.69) | 4.01 (0.67) | +0.25 | 6.23% | −2.54 | 0.012 |
| Problem-Solving Communication | 3.86 (0.53) | 4.17 (0.54) | +0.31 | 7.43% | −3.93 | 0.000 |
| Shared Goals | 3.97 (0.60) | 4.32 (0.58) | +0.35 | 8.10% | −3.83 | 0.000 |
| Shared Knowledge | 3.51 (0.62) | 3.64 (0.56) | +0.13 | 3.57% | −1.54 | 0.125 |
| Mutual Respect | 3.66 (0.71) | 4.06 (0.63) | +0.40 | 9.85% | −3.86 | 0.000 |
| Overall RC Index | 3.75 (0.47) | 4.10 (0.49) | +0.35 | 8.54% | −5.07 | 0.000 |
Note: SD indicates Standard Deviation; “n” ranges from 91–93 at baseline and 79–100 at follow-up
Improvements in scores were observed between Time 1 and the one Time 2 on all RC dimensions. In almost all cases these improvements shifted the “strength of ties” categoriziation into another category (e.g., from moderate to strong) (Figure 2). The largest percent change from Time 1 to Time 2 was in Mutual Respect (9.85%) and Frequency of Communication (9.55%). The smallest percent change was in Shared Knowledge (3.57%).
Means between Time 1 and Time 2 were significantly different for the overall RC index (p <0.01) and six of the seven RC dimensions. Shared Knowledge is the only dimension for which the increase was not significantly different (p = 0.125) (see Table 3). A sensitivity analysis carried out by analyzing results of those who only participated at both Time 1 and Time 2 found similar results (see Appendix).
Discussion
This study provides one of the first documented examples of a purposeful IP team intervention leading to improvements in team communication and relationships with a practicing IP AHF care team. Using validated RC surveys, improvements in all seven RC dimensions from Time 1 to Time 2 were demonstrated. The purposeful IP team intervention included quarterly leadership workshops, targeted TeamSTEPPS communication training, and implementation of the SIBR process. An innovative aspect of this study was the use of baseline RC results as a diagnostic tool of team functioning and as an intervention (motivation to improve various aspects of how the AHF team functioned). Aggregate level results of the RC survey (seven dimensions and RC index) were shared with the AHF care teams at leadership workshops to facilitate development of a shared understanding of their challenges in team functioning and to identify possible strategies for improvement. After several leadership workshops the AHF teams determined that they needed team training and new ways of working together to improve timely communication, mutual respect, and shared knowledge. This approach empowered the AHF teams to develop processes and structures to improve their RC.
The results of this study have had an impact on patient satisfaction, provider and nurse satisfaction. Although we did not specifically measure patients’ experience of care, the per capita cost of healthcare, or population health of HF patients (three components of the Quadruple Aim), our practice partners have reported notable increased in patient satisfaction scores and that implementation of the SIBR process improved work process efficiencies (start time and duration of rounds). In addition, nurse job satisfaction scores improved significantly from before to after the IP intervention (Baik & Zierler, 2018a). The IP AHF care team has reported more satisfaction in their work and have been recognized by the healthcare system for their dedication to improve the quality and safety of care for patients with AHF by changing the way the function as a team.
These findings are consistent with the Relational Model of Organizational Change which links structural (i.e., teamwork training), relational (creating safe spaces for relationships to form and be maintained), and work process (i.e., implementation of SIBR) changes with improvements in RC (Gittell, 2013). For example, parallel with our RC surveys, patient satisfaction survey results for the involved units shifted from the lowest ranking at the academic medical center to consistently ranking among the highest, reflecting a positive development.
Although the overall RC index and six of the seven RC dimension scores were significantly improved pre/post the IP intervention, the dimension of ‘shared knowledge’ was not significantly improved. This result was surprising because one goal of SIBR is to have the team together each day at the patient’s bedside to share information about the plan of care. We had anticipated that this approach would contribute to substantive increases in shared knowledge. While a small increase in shared knowledge was identified, it was not statistically significant (Figure 2), and has been a topic of continued interest for the AHF care teams as well as the broader Academic Practice Partnership. One possible explanation for the modest increase in shared knowledge may be a lack of collective understanding of long-term plans for patient care. In this same study population recently, (names removed for blinding, ref #3) (2018), found that nurses appreciated the focus on the daily plan of care during SIBR but identified a gap between what information was needed to provide care that day and long-term plans for the patient. Additional research is needed to better understand the complex interrelationships between the multiple dimensions of team communication, shared goals, mutual respect and shared knowledge.
This study adds to the growing evidence for SIBR implementation as an effective approach to improving team communication and relationships (Beaird et al., 2017; Bhamidipati et al., 2016; Gonzalo et al., 2014; Mercedes, Fairman, Hogan, Thomas, & Slyer, 2016; Pannick et al., 2015; Reeves, Pelone, et al., 2017; Walton, Hogden, Johnson, & Greenfield, 2016; Baik & Zierler, 2018b). Patient safety errors—such as medication errors or adverse events—are the third leading cause of death in the United States (Makary and Daniel, 2016). Poor communicationis a leading driver of these types of patient safety errors (IOM, 2000; James, 2013). Changes in work processes (such as SIBR implementation) that improve care team communication hold great potential as a means to reduce patient patient safety errors.
Previous point in time cross-sectional studies have found associations between strength of RC ties and patient perceptions of care (Azar et al., 2017), care team climate (Deneckre et al., 2013), and quality of care (Cramm & Nieboer, 2012). Our study builds on these findings by demonstrating improvements in RC following a purposeful IP team intervention and associated SIBR implementation, providing a model approach for care teams/settings with low RC scores.
Limitations.
As with any study there are limitations to these findings. One of the biggest concerns is that health care is in a constant state of change. For example, during the time of this study a number of changes occurred including a shift in the organization of the AHF services (splitting one service into two) and associated changes in service and unit leadership as well formation of a new Accountable Care Organization at the academic health center administration level. Despite these changes in staffing and organizational models we were still able to carry out the purposeful IP team intervention and RC scores improved. It is likely that these changes influenced AHF care team communication and relationships in ways that supported positive changes as well as contributed to challenges. Preliminary positive results have been well received and there is increasing executive support for this type of intervention as a way to support implementation of team-based practice transformation efforts as well as interest in becoming a more intentional learning healthcare system.
Another limitation encountered is related to response rates and changes in respondents over time. The RC survey is long and may feel burdensome to participants, leading to lower than desired response rates. From baseline (Time 1) to the one-year follow-up (Time 2) a number of RNs shifted units due to the clinical reorganization. Due to the training nature of the Fellows’ rotation schedule there were different Fellows from Time 1 to Time 2. Despite these changes, 44% of respondents were the same from Time 1 to Time 2 and a sensitivity analysis of the RC results for these paired respondents was very similar to the results that included all respondents (see Appendix). Additionally, respiratory therapists were initially included in the RC survey prior to the selection of SIBR as the intervention focus. Respiratory therapists do not participate in daily SIBR rounds so their was excluded in this analysis to be able to see the explicit impact of the IP intervention.
Finally, the results that described in this paper represent aggregates of all workgroups and may not represent variation within and between workgroups. These variations were not within the scope of this paper and we plan to delve further into these variations in a subsequent paper.
Conclusion
The purposeful IP team training intervention was associated with improvements in IP team communication and relationships between workgroups. Improvements in RC across all seven dimensions were found from baseline to follow-up. Percent change in RC score ranged from 3.7%–10.93%. Changes were statistically significant for improvements between baseline and follow-up on all but one (shared knowledge) of the RC survey’s seven dimensions. Additional research is needed to assess relationships between RC improvements and behavior change as well as patient perspectives and outcomes. There is also a need to the study strategies that promote consistency and sustainability of the SIBR process and associated increases in RC for members of the IP healthcare workforce over time. Approaches to standardizing and scaling-up implementation of team-based interventions such as the model described above also requires additional investigation. Findings of this study are consistent with the growing body of RC and SIBR research and provide a useful model of a purposeful IP team intervention in clinical practice settings.
Supplementary Material
Acknowledgements
The authors would like to acknowledge the invaluable partnerships and collaborations with our clinical partners at the University of Washington (UW) Medical Center, the UW WWAMI Institute for Simulation in Healthcare (WISH), grant team members from the UW Schools of Nursing, Medicine, and Pharmacy, and the UW Center for Health Sciences Interprofessional Education, Research, and Practice. We also appreciate the assistance of Jody Hoffer Gittell, Saleema Moore, Hyosin Kim, Lyoung Kim and other members of the Relational Coordination (RC) Research Collaborative for their technical assistance with RC survey set-up and analysis. Also acknowledged is financial support the project has received from the Health Resources Services Administration (HRSA) grant # UD7HP26909.
References
- Avery CL, Loehr LR, Baggett C, Chang PP, Newton AM, Matsushita K, Rosamond WD,… Heiss G (2012). The population burden of heart failure attributable to modifiable risk factors: The atherosclerosis risk in communities study. Journal of the American College of Cardiology, 60(17):1640–1646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azar JM, Johnson CS, Frame AM, Perkins SM, Cottingham AH, & Litzelman DK (2017). Evaluation of interprofessional relational coordination and patients’ perception of care in outpatient oncology teams. Journal of Interprofessional Care, 31(2), 273–276. 10.1080/13561820.2016.1248815 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baik D, & Zierler B. (2018a). RN job satisfaction and retention after an interprofessional. Western Journal of Nursing Research, 0193945918770815. doi 10.1177/0193945918770815. [DOI] [PubMed] [Google Scholar]
- Baik D, & Zierler B. (2018b). Clinical nurses’ experiences and perceptions after the implementation of an interprofessional team intervention: A qualitative study. Journal of Clinical Nursing. 0193945918770815. doi 10.1111/jocn.14605. [DOI] [PubMed] [Google Scholar]
- Beaird G, Dent JM, Keim-Malpass J, Muller AGJ, Nelson N, & Brashers V (2017). Perceptions of Teamwork in the Interprofessional Bedside Rounding Process. Journal for Healthcare Quality: Official Publication of the National Association for Healthcare Quality, 39(2), 95–106. 10.1097/JHQ.0000000000000068 [DOI] [PubMed] [Google Scholar]
- Berwick DM, Nolan TW, & Whittington J (2008). The triple aim: care, health, and cost. Health Affairs (Project Hope), 27(3), 759–769. 10.1377/hlthaff.27.3.759 [DOI] [PubMed] [Google Scholar]
- Bhamidipati VS, Elliott DJ, Justice EM, Belleh E, Sonnad SS, & Robinson EJ (2016). Structure and outcomes of interdisciplinary rounds in hospitalized medicine patients: A systematic review and suggested taxonomy. Journal of Hospital Medicine, 11(7), 513–523. 10.1002/jhm.2575 [DOI] [PubMed] [Google Scholar]
- Bodenheimer T, & Sinsky C (2014). From Triple to Quadruple Aim: Care of the patient requires care of the provider. The Annals of Family Medicine, 12(6), 573–576. 10.1370/afm.1713 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brandt B, Lutfiyya MN, King JA, & Chioreso C (2014). A scoping review of interprofessional collaborative practice and education using the lens of the Triple Aim. Journal of Interprofessional Care, 28(5), 393–399. 10.3109/13561820.2014.906391 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Browne S, Macdonald S, May CR, Macleod U, & Mair FS (2014). Patient, carer and professional perspectives on barriers and facilitators to quality care in advanced heart failure. PloS One, 9(3), e93288 10.1371/journal.pone.0093288 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burdick K, Kara A, Ebright P, & Meek J (2017). Bedside interprofessional rounding: The view from the patient’s side of the bed. Journal of Patient Experience, 4(1), 22–27. 10.1177/2374373517692910\ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cramm JM, & Nieboer AP (2012). Relational coordination promotes quality of chronic care delivery in Dutch disease-management programs. Health Care Management Review, 37(4), 301–309. 10.1097/HMR.0b013e3182355ea4 [DOI] [PubMed] [Google Scholar]
- Colucci WS, & Dunlay SM (2018). Clinical manifestations and diagnosis of advanced heart failure. UpToDate. Retrieved October 16, 2018: https://www.uptodate.com/contents/clinical-manifestations-and-diagnosis-of-advanced-heart-failure
- Cox M, Cuff P, Brandt B, Reeves S, & Zierler B (2016). Measuring the impact of interprofessional education on collaborative practice and patient outcomes. Journal of Interprofessional Care, 30(1), 1–3. 10.3109/13561820.2015.1111052 [DOI] [PubMed] [Google Scholar]
- Deneckere S, Euwema M, Van Herck P, Lodewijckx C, Panella M, Sermeus W, & Vanhaecht K (2012). Care pathways lead to better teamwork: results of a systematic review. Social Science & Medicine (1982), 75(2), 264–268. 10.1016/j.socscimed.2012.02.060 [DOI] [PubMed] [Google Scholar]
- Gittell J (2003). The Southwest Airlines way: Using the power of relationships to achieve high performance. Industrial & Labor Relations Review, 57 10.2307/4126671 [DOI] [Google Scholar]
- Gittell J (2012). Relational coordination: Guidelines for theory, measurement and analysis. Relational Coordination Research Collaborative. Brandeis University: Author. [Google Scholar]
- Gittell JH, Cameron K, Lim S, & Rivas V (2006). Relationships, layoffs, and organizational resilience: Airline industry responses to September 11. The Journal of Applied Behavioral Science, 42(3), 300–329. 10.1177/0021886306286466 [DOI] [Google Scholar]
- Gittell JH, Fairfield KM, Bierbaum B, Head W, Jackson R, Kelly M, … Zuckerman J (2000). Impact of relational coordination on quality of care, postoperative pain and functioning, and length of stay: A nine-hospital study of surgical patients. Medical Care, 38(8), 807–819. [DOI] [PubMed] [Google Scholar]
- Gittell JH, Godfrey M, & Thistlethwaite J (2013). Interprofessional collaborative practice and relational coordination: Improving healthcare through relationships. Journal of Interprofessional Care, 27(3), 210–213. 10.3109/13561820.2012.730564\ [DOI] [PubMed] [Google Scholar]
- Gittell JH, Weinberg DB, Bennett AL, & Miller JA (2008). Is the doctor in? A relational approach to job design and the coordination of work. Human Resource Management, 47(4), 729–755. 10.1002/hrm.20242 [DOI] [Google Scholar]
- Gittell JH, Logan C, Cronenwett J, Foster TC, Freeman R, Godfrey M, & Vidal DC (2018). Impact of relational coordination on staff and patient outcomes in outpatient surgical clinics. Health Care Management Review. 10.1097/HMR.0000000000000192 [DOI] [PubMed] [Google Scholar]
- Gittell JH, (2002). Coordinating Mechanisms in Care Provider Groups: Relational Coordination as a Mediator and Input Uncertainty as a Moderator of Performance Effects | Management Science. Retrieved October 16, 2018, from https://pubsonline.informs.org/doi/10.1287/mnsc.48.11.1408.268
- Gittell JH, Seidner R, & Wimbush J (2009). A Relational Model of How High-Performance Work Systems Work. Organization Science, 21(2), 490–506. 10.1287/orsc.1090.0446 [DOI] [Google Scholar]
- Gonzalo JD, Wolpaw DR, Lehman E, & Chuang CH (2014). Patient-centered interprofessional collaborative care: Factors associated with bedside interprofessional rounds. Journal of General Internal Medicine, 29(7), 1040–1047. 10.1007/s11606-014-2817-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Havens DS, Gittell JH, & Vasey J (2018). Impact of relational coordination on nurse job satisfaction, work engagement and burnout: Achieving the quadruple aim. The Journal of Nursing Administration, 48(3), 132–140. 10.1097/NNA.0000000000000587 [DOI] [PubMed] [Google Scholar]
- Havens DS, Vasey J, Gittell JH, & Lin W-T (2010). Relational coordination among nurses and other providers: Impact on the quality of patient care. Journal of Nursing Management, 18(8), 926–937. 10.1111/j.1365-2834.2010.01138.x [DOI] [PubMed] [Google Scholar]
- Heidenreich PA, Albert NM, Allen LA, Bluemke DA, Butler J, Fonarow GC, … Stroke Council. (2013). Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circulation. Heart Failure, 6(3), 606–619. 10.1161/HHF.0b013e318291329a [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (US) Committee on Quality of Health Care in America. (2000). To Err is Human: Building a Safer Health System. (Kohn LT, Corrigan JM, & Donaldson MS, Eds.). Washington (DC): National Academies Press (US) Retrieved from http://www.ncbi.nlm.nih.gov/books/NBK225182/ [PubMed] [Google Scholar]
- Institute of Medicine. (2012). Best care at lower cost: The path to continuously learning health care in America. Retrieved from https://tinyurl.com/ydy4dxlf [PubMed]
- James JT (2013). A New, Evidence-based Estimate of Patient Harms Associated with Hospital Care: Journal of Patient Safety, 9(3), 122–128. 10.1097/PTS.0b013e3182948a69 [DOI] [PubMed] [Google Scholar]
- Makary MA, & Daniel M (2016). Medical error—the third leading cause of death in the US. BMJ, 353, i2139 10.1136/bmj.i2139 [DOI] [PubMed] [Google Scholar]
- Manski-Nankervis J-A, Furler J, Blackberry I, Young D, O’Neal D, & Patterson E (2014). Roles and relationships between health professionals involved in insulin initiation for people with type 2 diabetes in the general practice setting: A qualitative study drawing on relational coordination theory. BMC Family Practice, 15, 20 10.1186/1471-2296-15-20 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mercedes A, Fairman P, Hogan L, Thomas R, & Slyer JT (2016). Effectiveness of structured multidisciplinary rounding in acute care units on length of stay and satisfaction of patients and staff: A quantitative systematic review. JBI Database of Systematic Reviews and Implementation Reports, 14(7), 131–168. 10.11124/JBISRIR-2016-003014 [DOI] [PubMed] [Google Scholar]
- O’Leary KJ, Haviley C, Slade ME, Shah HM, Lee J, & Williams MV (2011). Improving teamwork: impact of structured interdisciplinary rounds on a hospitalist unit. Journal of Hospital Medicine, 6(2), 88–93. 10.1002/jhm.714 [DOI] [PubMed] [Google Scholar]
- Pannick S, Davis R, Ashrafian H, Byrne BE, Beveridge I, Athanasiou T, … Sevdalis N (2015). Effects of interdisciplinary team care interventions on general medical wards: A systematic review. JAMA Internal Medicine, 175(8), 1288–1298. 10.1001/jamainternmed.2015.2421 [DOI] [PubMed] [Google Scholar]
- Paradis E, & Reeves S (2012). Key trends in interprofessional research: A macrosociological analysis from 1970 to 2010. Journal of Interprofessional Care, 27(2), 113–122. 10.3109/13561820.2012.719943 [DOI] [PubMed] [Google Scholar]
- Ratelle JT, Sawatsky AP, Kashiwagi DT, Schouten WM, Erwin PJ, Gonzalo JD, … West CP (2018). Implementing bedside rounds to improve patient-centred outcomes: a systematic review. BMJ Qual Saf, bmjqs-2017–007778. 10.1136/bmjqs-2017-007778 [DOI] [PubMed] [Google Scholar]
- Relational Model of Change. (n.d.). Retrieved October 17, 2018, from https://rcrc.brandeis.edu/about-rc/model.html
- RC Survey | Relational Coordination Analytics. (n.d.). Retrieved March 16, 2018, from http://rcanalytic.com/rc-survey/
- The RC Survey: Measuring Relational Coordination. (n.d.). Retrieved September 24, 2018, from https://rcrc.brandeis.edu/survey/validation-and-survey-items.html
- Reeves S, Clark E, Lawton S, Ream M, & Ross F (2017). Examining the nature of interprofessional interventions designed to promote patient safety: A narrative review. International Journal for Quality in Health Care: Journal of the International Society for Quality in Health Care, 29(2), 144–150. 10.1093/intqhc/mzx008 [DOI] [PubMed] [Google Scholar]
- Reeves S, Pelone F, Harrison R, Goldman J, & Zwarenstein M (2017). Interprofessional collaboration to improve professional practice and healthcare outcomes. The Cochrane Database of Systematic Reviews, 6, CD000072 10.1002/14651858.CD000072.pub3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Relational Model of Change. (n.d.). Retrieved March 15, 2018, from https://rcrc.brandeis.edu/about-rc/model.html
- Suter LG, Li S-X, Grady JN, Lin Z, Wang Y, Bhat KR, … Bernheim SM (2014). National patterns of risk-standardized mortality and readmission after hospitalization for acute myocardial infarction, heart failure, and pneumonia: update on publicly reported outcomes measures based on the 2013 release. Journal of General Internal Medicine, 29(10), 1333–1340. 10.1007/s11606-014-2862-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- TeamStepps | Agency for Healthcare Research & Quality. (n.d.). Retrieved July 20, 2018, from https://www.ahrq.gov/teamstepps/index.html
- Titler MG, Jensen GA, Dochterman JM, Xie X-J, Kanak M, Reed D, & Shever LL (2008). Cost of hospital care for older adults with heart failure: medical, pharmaceutical, and nursing costs. Health Services Research, 43(2), 635–655. 10.1111/j.1475-6773.2007.00789.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- White A (2013). Structured Interprofessional Bedside Rounds. Retrieved from https://depts.washington.edu/uwmedres/pdf/orientation/Structured%20Interprofessional%20Bedside%20Rounding%20(SIBR).pdf
- Von der Heidt A, Ammenwerth E, Bauer K, Fetz B, Fluckinger T, Gassner A, … Poelzl G (2014). HerzMobil Tirol network: Rationale for and design of a collaborative heart failure disease management program in Austria. Wiener Klinische Wochenschrift, 126(21–22), 734–741. 10.1007/s00508-014-0665-7 [DOI] [PubMed] [Google Scholar]
- Walton V, Hogden A, Johnson J, & Greenfield D (2016). Ward rounds, participants, roles and perceptions: Literature review. International Journal of Health Care Quality Assurance, 29(4), 364–379. 10.1108/IJHCQA-04-2015-0053 [DOI] [PubMed] [Google Scholar]
- Zierler BK, Abu-Rish Blakeney E, O’Brien KD, & AHF Teams. (2018). An interprofessional collaborative practice approach to transform heart failure care: An overview. Journal of Interprofessional Care, 1–4. 10.1080/13561820.2018.1426560. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.