Abstract
Objectives
We aimed to report outcomes of Bicondylar Tibial Plateau (BTP) fractures treated using Ilizarov fixation, and identify risk factors for developing post-traumatic radiographic osteoarthritis (ROA).
Methods
Retrospective study of 80 BTP fractures managed with Ilizarov fixation.
Results
All fractures united, with only 3 cases of deep infection. ROA was evident in 12.5% at average 13 months post-injury. Increased tibial articular-widening associated with risk of developing ROA (p = 0.02).
Conclusion
Ilizarov fixation is safe and reliable in the management of BTP fractures. Restoration of tibial articular-width at fixation associated with reduced risk of developing radiographic OA.
Keywords: Bicondylar, Tibial, Plateau, Fracture, Ilizarov, Osteoarthritis
1. Introduction
Tibial plateau fractures are serious peri-articular injuries with often inferior outcomes.1 Commonly the result of high-energy injuries, the allied condition of the surrounding soft tissues offers a challenging proposition to the surgeon. Associated injuries include: meniscal tears, ligamentous injury and compartment syndrome. Schatzker classified the injury from I to VI, with V and VI classified as bicondylar injuries.2
Limb alignment correction, articular surface restoration, and stable fixation enabling early knee motion, are the main goals of surgical treatment. Whilst the gold standard for surgical management has traditionally been viewed as open reduction internal fixation (ORIF), recent evidence has suggested that fine-wire external fixation may offer some advantages with regard to soft tissue healing, lower deep infection rates, and fewer incidences of compartment syndrome.3, 4, 5 Additionally, the use of external fixation permits immediate weight bearing. Whilst ORIF produces ‘good’ to ‘excellent’ radiological outcomes in upto 96%6, 7, 8 of patients, an incidence of compartment syndrome following surgery of up to 14.5% and a deep infection rate of up to 23.6% has been reported.9
The only randomised control trial to date comparing ORIF with circular external fixation in the treatment of bicondylar tibial plateau fractures was conducted by Hall et al.4 Circular external fixation resulted in a shorter hospital stay, a marginally faster return of function, and similar clinical outcomes to ORIF. The authors concluded that because the number and severity of complications was much higher with ORIF, that circular fixation should be seen as an attractive alternative for these cases.
Surgically managed tibial plateau fractures have an increased likelihood of developing osteoarthritis (OA) and requiring a subsequent TKA compared with a matched group from the general population.10 The importance of anatomic fracture reduction in preventing OA and maximizing functional outcomes is presently unclear however. Emphasis thus far has centred upon investigating the importance of postoperative articular surface restoration and mechanical axis. Less postoperative articular step-off and a normal mechanical axis of the lower leg after plate fixation in tibial plateau fractures appears to have a role in prevention of post-traumatic OA,11 but does not appear to predict clinical outcome12 at medium-term follow-up.
1.1. Aims & objectives
To our knowledge, this is the first study to date to attempt to identify clinical and radiological risk factors for early joint degeneration following Ilizarov fixation for both open and closed bicondylar tibial plateau fractures.
The primary aim of this study was therefore to determine the radiological, clinical, and functional outcomes of patients with unstable bicondylar tibial plateau fractures treated using the Ilizarov method. The secondary aim was to report the incidence of early radiographic OA, and identify potentially contributing risk factors, including malreduction.
2. Methods
All patients treated surgically for a bicondylar tibial plateau fracture in our Level 1 major trauma center, between 2008 and 2012 were included. Patients were identified from an existing trauma database and all were managed definitively using fine-wire external fixation using the Ilizarov technique.
The following data was collected; patient demographics, the initial presenting hospital following injury, time to temporary spanning external fixation (if used), time to definitive Ilizarov frame post injury, complications, and time to union. The date of fracture union was defined as the point of frame removal. Patient related outcome measures (PROMs) in the form of an Oxford Knee Score (OKS) were obtained at their most recent follow up appointment or over the telephone. Complete OKS data was obtained in 35 patients.
Fracture reduction was assessed radiologically on the immediate post-operative radiograph using the following methods. Several validated radiographic parameters of alignment (medial proximal tibial angle, joint line congruency angle (JLCA), and posterior tibial slope) were measured using PACS (Patient Archiving and Communications System (IMPAX 6.2.1.258, Agfa HealthCare, Brentford, UK)). Adequacy of fracture reduction was determined using the Rasmussen Radiological Score (RRS) (Table 1).13 In the absence of pre-injury radiographs for any of the cohort, the articular width of the tibial plateau was assumed to be equal to that of the distal femoral articular surface. This assumption is based upon studies that have reported an almost 1:1 width ratio between these surfaces.14 All measurements were performed on anonymised radiographs, on two separate occasions, by the first author (ST). The mean value for each parameter was taken forward for analysis. Finally, resulting degenerative disease was assessed from the latest available post-operative weight-bearing AP and lateral radiographs using the Kellgren Lawrence (KL) grading system. The KL system grades a joint from normal to severe (0–4) based upon the features of joint space narrowing, osteophytosis, and subchondral sclerosis and cysts.15 The presence of OA was defined as a KL score greater than 1. All radiological scores were measured by the first author (ST) on two separate occasions. Radiographs were anonymised. In the eventuality that there was discrepancy between the two readings – a second observer was used to provide a final decision. All patients were allowed to weight bear as tolerated through their Ilizarov frame. Thromboprophylaxis post-operatively consisted of intermittent foot, and calf (on the non-operated leg), pump compression usage until full weight-bearing was achieved. Standard pin-site care was performed by the patient under the guidance of a Specialist Nurse.
Table 1.
Rasmussen radiological score.
| Appearance | Excellent = 6 | Good - 4 | Fair = 2 | Poor = 0 |
|---|---|---|---|---|
| Depression | None | <6 mm | 6–10 mm | >10 mm |
| Tibial articular surface widening | None | <6 mm | 6–10 mm | >10 mm |
| Alignment (varus/valgus) | None | <10° | 10–20° | >20° |
Statistical analysis was performed with GraphPad Prism v6 (GraphPad Software).
3. Results
There were 80 adult patients (54 male) with 80 fractures, of which 78 were Schatzker VI injuries. The mean age was 43 (range 17–80). Thirty-four patients were smokers. Where a clear mechanism was recorded, 80% were high energy, with mechanisms including road traffic collisions, sports related injuries, and falls from height. There were associated bony injuries in 10.8% of patients, which included: acetabular, femoral, ipsilateral tibial shaft, forearm, hand, and calcaneal fractures. Other associated injuries included a chest and a head injury, neither of which required surgery. Four injuries were open - all were closed primarily following debridement at the application of temporary spanning external fixator. There were 4 cases of compartment syndrome, all requiring fasciotomies. Two of these required soft tissue coverage in the form of split skin grafting following fasciotomy.
Sixty-nine patients were initially managed in a temporary spanning external-fixator bridging the knee joint. Twenty-three patients presented directly to our unit and the remainder tertiary referrals from surrounding hospitals. For patients managed initially with a spanning external fixator across the knee, the mean time from injury to application of spanning external fixator was 3.28 days (range 0–5). Following temporary external fixation, the mean duration to Ilizarov was 9.96 days (range 2–35). Overall, the mean interval from injury to definitive Ilizarov frame was 12.16 days (range 0–42). Fracture reduction at the time of definitive fixation was good to excellent according to the RRS in 76.3% (Fig. 1, Fig. 2, Fig. 3) and fair in the remainder.
Fig. 1.
Computed tomography imaging of a patient pre-operatively.
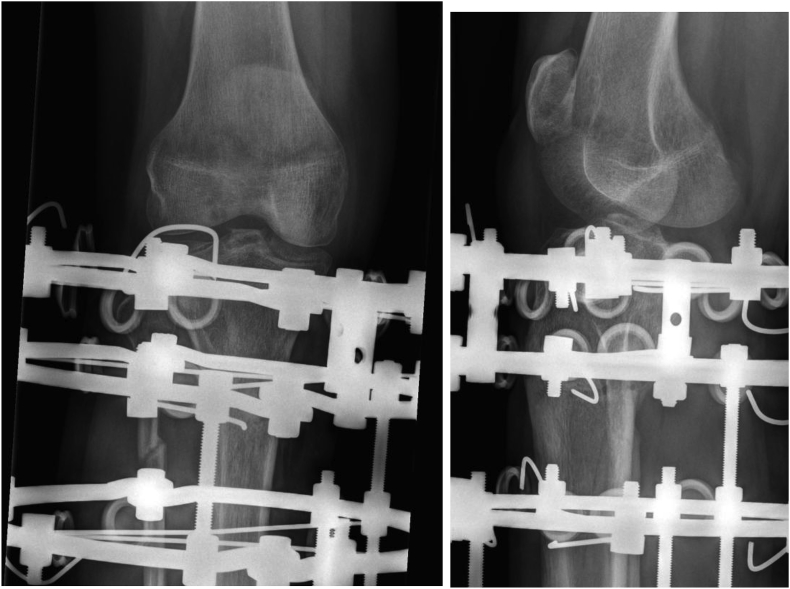
Fig. 2.
Post-operative radiographs of the same patient.
Fig. 3.
Final radiographs after union in the same patient with excellent Rasmussen Radiological Score.
Union was achieved in all cases, with a mean time to union of 3.9 months (range 1.8–12.1 months). The case that took the longest duration to unite (12.1 months) was over 100 days longer than any other patient. This patient required bone grafting (autograft) and the use of OP-1 implant (BMP-7, Stryker Corporation, MI, USA) prior to union being achieved. In our study, smoking-status did not correlate with an increased time to union (Mann-Whitney U test, p = 0.421).
A full list of complications is demonstrated in Table 2. Pin-site infection was the most common complication, present in 33.8% of all patients. All were managed with oral antibiotics as per local departmental guidance. Five patients required removal of wires for recalcitrant infection.
Table 2.
Table of complications.
| Complication | Frequency |
|---|---|
| Pin site infection | 27 (33.8%) |
| Neurapraxia | 3 (3.8%) |
| Synovial leak | 3 (3.8%) |
| Septic arthritis | 2 (2.5%) |
| Osteomyelitis | 1 (1.3%) |
| Haematoma | 1 (1.3%) |
| Mechanical knee symptoms | 1 (1.3%) |
| Pulmonary embolus | 1 (1.3%) |
There were 3 cases (3.75%) of deep infection. Two developed a septic arthritis of the knee that was successfully managed with arthroscopic washout and repositioning of wires. The third developed proximal tibial osteomyelitis caused by a Coagulase Negative Staphylococcus. The osteomyelitis was successfully treated with a Lautenbach procedure, followed by a 2-stage primary TKA. In this case, the initial closed injury was managed with a prompt temporary spanning external fixator applied in a local district general hospital. There was a subsequent 14-day interval to application of definitive Ilizarov frame. All cases of neurapraxia resolved. Three patients required removal of wires for synovial leakage, none of which developed septic arthritis. One patient subsequently underwent an arthroscopy for a medial meniscal tear.
For all patients with completed outcome scores, the mean Oxford Knee Score was 37.2 (range 12–48).
3.1. Risk factors for development of early OA
Thirteen percent of patients had evidence of radiographic OA at a mean of 13 months (range 3.2–53 months) after injury.
To achieve our secondary aim, patients who had developed radiographic OA following fixation (Fig. 5) were compared to those who had not. The demographic details of the two groups were not significantly different, with regard to age, gender, and smoking status (Table 3).
Fig. 5.
Post-operative and post-Ilizarov frame removal radiographs demonstrating evidence of osteoarthritis.
Table 3.
Table of differences between patients with and without radiographic OA.
| Non-OA cohort | OA cohort | P-value | |
|---|---|---|---|
| Male/Female | 47/23 | 7/3 | |
| Age (years) | 43.1 (17.8–85.4) | 43.6 (21–68.2) | 0.92 |
| Smoking (%) | 42.9 | 40 | 0.99 |
| Time to union (days) | 124.5 | 123 | 0.81 |
| RRS | 13.5 | 11 | |
| Medial proximal tibial angle (⁰) | 86 | 86.7 | 0.57 |
| Articular step-off (mm) | 2.3 | 4.1 | 0.09 |
| Tibial articular widening (mm) | 4 | 7.9 | 0.02 |
| Posterior tibial slope (⁰) | 83.4 | 83 | 0.78 |
A lower mean RRS following fixation was exhibited within the radiographic OA group (11 versus 13.5). When each of the separate constituent variables of the RRS were analysed, only an increase in the mean tibial articular width was significantly associated with early OA risk (7.9 mm vs. 4 mm, unpaired T-test p = 0.02). Proximal tibial angulation, the articular step-off, and the posterior tibial slope at the time of fixation, were statistically similar between the OA and non-OA groups.
We also found no statistically significant difference between the OKS within the OA and non-OA groups (unpaired T-test, p = 0.37).
3.2. Incidence of TKA
Only 3 patients progressed to TKA (Fig. 4) at a mean follow-up of 6.4 years (range 4.3–9.3). Of these, one patient developed a prosthetic joint infection, which was managed initially with a debridement and implant retention (DAIR) procedure, followed by a single stage revision.
Fig. 4.
Kaplan-Meier survival curve for patients requiring total knee arthroplasty.
4. Discussion
Bicondylar tibial plateau fractures are severe periarticular injuries often resulting from high-energy trauma and frequently with significant associated soft tissue injuries.
The perceived advantage of ORIF is direct anatomical reduction and stable fixation. This comes at a cost however, with recognized soft-tissue envelope complications including deep infection and compartment syndrome commonly seen2,3,8. Multifragmentary injuries in particular may be difficult or impossible to reconstruct fully with internal fixation, and further periosteal damage and soft tissue compromise may be best avoided in these cases. Circular external fixation methods avoid this secondary soft tissue insult and therefore may be expected to have reduced rates of deep infection and wound complications. A recent systematic review from Boutefnouchet would support this assertion.3 The authors conclude that fine wire frame external fixation offers an advantage of better soft tissue outcomes in comparison with ORIF. However, it also concludes that there is currently insufficient evidence to determine whether circular frame external fixation, in the treatment of bicondylar tibial plateau fractures, provides better outcomes and fewer complications when compared to ORIF.3 The only randomised study comparing ORIF versus circular external fixation in bicondylar fractures shows that circular external fixation is associated with less blood loss, fewer unplanned re-operations and a shorter hospital stay. There were no differences in two-year functional results between the groups.4
Circular external fixators utilize beam loading of the tensioned fine wires to provide stability across the whole length of the wire.16 The surgeon can exploit this by using several wires, to provide uniform support for the tibial plateau articular surface that may be likened to a bespoke construct personalised to each individual fracture configuration.16
All the patients in our series achieved bony union, which is consistent with the literature. Both Ferreira et al. and Kataria et al., achieved a 100% union rate in their series of 46 and 38 bicondylar fractures respectively treated with fine wire fixators.1,17 The mean time taken to union in our series (3.9 months) is also consistent with that in the literature (Ferreira et al. 3.9 months17 and Keightley et al., 2015 4.4 months18).
We found that the incidence of severe complications such as deep infection and compartment syndrome to be low in our series. Our series reports a deep infection rate of only 3.75%, of which 2 cases of septic arthritis were successfully managed with arthroscopic washout. Similar septic arthritis rates have been reported in multiple other studies employing external fixation.19,20 In fact deep infection rates of 0% have been reported in several studies supporting the theory that external fixation may be favourable at decreasing these potentially catastrophic complications.1,21,22
A relatively common complication of external fixation is pin-site infection. Whilst reported rates of pin-site infection in tibial plateau fractures treated with circular frames are as high as 57%,18,19 there are seldom reported cases of deep infection occurring as a result. Our series demonstrates an incidence of 34%, of which all were successfully managed with oral antibiotics or wire removal. Pin-site infection can be deemed therefore as a minor complication, managed with relatively simple measures.
A perceived disadvantage of circular external fixation is its inability to directly reduce fracture fragments, thereby providing potential difficulty in achieving anatomical articular congruity. It is unclear however, whether articular incongruity is indeed important in determining outcomes both radiologically and functionally. Even in those studies that demonstrate correlation, what degree of articular step-off that is significant to outcome is unknown. Articular incongruity in Schatzker I-III injuries, in particular, is well tolerated and has little effect upon outcome.23,24 Giannoudis reports that multiple other factors are likely to play a greater role upon outcomes than articular congruity, including knee stability, varus/valgus malalignment, and retention of the meniscus. The relatively thick cartilage on the tibial plateau relative to other joints, potentially protects against the risk of developing post-traumatic knee OA compared with injuries at other joints with a similar articular step-off.24 A previous study of 25 cases of open bicondylar fractures managed with external fixation demonstrated no significant difference in outcome in patients with greater or less than 4 mm of articular depression.21 In the setting of circular external fixation, our results did not show any association between articular step-off and the development of early radiographic OA. Konstantinos et al., reported the correlation between adequacy of reduction and patient-reported outcomes in a cohort of complex tibial plateau fractures treated with a hybrid external fixator (standard Ilizarov ring proximally and Schanz screws distally). Patients with residual joint depression of >4.5 mm displayed significantly inferior American Knee Society Score (AKSS) scores,25 whilst the postoperative mechanical axis was not an indicator of patient-related outcome.
To our knowledge, this is the first study to investigate the importance of restoring tibial articular width at the time of circular external fixation to prevent early joint degeneration. Much work thus far has centred upon the importance of articular step-off and alignment. We found that inability to restore the tibial articular width was associated with an increased risk of developing early radiographic OA. We hypothesise that knee stability may be deleteriously affected by an inability to restore the normal width of the tibial plateau. This may occur via its effect on the function of the collateral ligaments and/or menisci. As a direct consequence the femoral condyle may collapse into the defect leading to joint space narrowing and the development of OA. Care should thus be taken to restore the tibial articular width at the time of fixation. The distal femoral articular width can be used as a guide by the surgeon to judge appropriate tibial width reduction. Thamyongkit et al., in a study of 3D CT scans from 84 healthy knees identified that the mean ratio of tibial to femoral articular width was 1.01 ± 0.04.14
Despite 13% of patients having evidence of early radiographic OA, only 3 subsequently required a TKA at a mean follow up of 6.4 years. This aligns with a study by Wasserstein et al. From a large cohort of 8426 operatively treated tibial plateau fractures, they report that 10 years following any tibial plateau fracture fixation surgery, 7.3% of the patients had undergone TKA.10 Higher rates of TKA were associated with bicondylar fractures in particular (HR, 1.53 [1.26, 1.84]; p < 0.0001). An area for concern and certainly further investigation may be the fact that 1 of the TKA's in our cohort developed a prosthetic joint infection requiring an eventual 2-stage revision.
This study has several limitations. The dataset is retrospective with varying lengths of follow-up. The follow-up period is also relatively short for the development of OA. Despite this, our follow-up for conversion to TKA is acceptable at a mean of over 6 years, providing good mid-term prognostic data to clinicians and patients. The functional data is unfortunately incomplete for our cohort with only 44% of patients being able to provide completed PROM's. This is typical of trauma related studies particularly when a significant proportion of patients are residents outside the region. We would also argue that in the trauma setting a pre-operative PROM is seldom available, and therefore a single post-operative PROM is of limited use, especially in such a heterogenous patient group. Certainly we would advise caution when interpreting our results related to the functional data due to its sparse nature. When identifying radiographic OA post fixation we did this unsure as to the existence of pre-injury radiographic OA. Older patients in particular may have had pre-existing OA that could have required a TKA regardless of the injury.
5. Conclusion
This is one of the largest series of bicondylar tibial plateau fractures managed with Ilizarov external fixation in the literature. We demonstrate a low deep infection rate and union in all cases. This study supports the Ilizarov method as a safe and reliable treatment option for definitive management of bicondylar tibial plateau fractures. Our data has also highlighted the importance of restoring the tibial articular width at the time of fixation in order to minimize the risk of developing subsequent radiographic OA.
Conflicts of interest
None from any author.
Author contributions
S Thiagarajah: Concept, design, data acquisition, data analysis, statistical analysis, manuscript preparation and editing.
G Hancock: Literature search, data acquisition, data analysis, statistical analysis, manuscript preparation, manuscript editing.
E Mills: Contribution of patients, manuscript review.
J McGregor-Riley: Contribution of patients, manuscript review.
S Royston: Contribution of patients, manuscript review.
M Dennison: Contribution of patients, manuscript review.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jor.2018.12.016.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Kataria H., Sharma N., Kanojia R.K. Small wire external fixation for high-energy tibial plateau fractures. J Orthop Surg. 2007;15:137–143. doi: 10.1177/230949900701500202. [DOI] [PubMed] [Google Scholar]
- 2.Schatzker J., McBroom R., Bruce D. The tibial plateau fracture. The Toronto experience 1968--1975. Clin Orthop Relat Res. 1979:94–104. [PubMed] [Google Scholar]
- 3.Boutefnouchet T., Lakdawala A.S., Makrides P. Outcomes following the treatment of bicondylar tibial plateau fractures with fine wire circular frame external fixation compared to open reduction and internal fixation: a systematic review. J Orthop. 2016;13:193–199. doi: 10.1016/j.jor.2015.02.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Hall J.A., Beuerlein M.J., McKee M.D. Canadian Orthopaedic Trauma Society. Open reduction and internal fixation compared with circular fixator application for bicondylar tibial plateau fractures. Surgical technique. J Bone Joint Surg Am. 2009;91(Suppl 2 Pt 1):74–88. doi: 10.2106/JBJS.G.01165. [DOI] [PubMed] [Google Scholar]
- 5.Prat-Fabregat S., Camacho-Carrasco P. Treatment strategy for tibial plateau fractures: an update. EFORT Open Reviews. 2016;1:225–232. doi: 10.1302/2058-5241.1.000031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yao Y. Functional outcomes of bicondylar tibial plateau fractures treated with dual buttress plates and risk factors: a case series. Injury. 2014;45:1980–1984. doi: 10.1016/j.injury.2014.10.004. [DOI] [PubMed] [Google Scholar]
- 7.Chen X.-Z. Arthroscopy-assisted surgery for tibial plateau fractures. Arthroscopy. 2015;31:143–153. doi: 10.1016/j.arthro.2014.06.005. [DOI] [PubMed] [Google Scholar]
- 8.Biggi F., Di Fabio S., D'Antimo C., Trevisani S. Tibial plateau fractures: internal fixation with locking plates and the MIPO technique. Injury. 2010;41:1178–1182. doi: 10.1016/j.injury.2010.08.001. [DOI] [PubMed] [Google Scholar]
- 9.Ruffolo M.R., Gettys F.K., Montijo H.E., Seymour R.B., Karunakar M.A. Complications of high-energy bicondylar tibial plateau fractures treated with dual plating through 2 incisions. J Orthop Trauma. 2015;29:85–90. doi: 10.1097/BOT.0000000000000203. [DOI] [PubMed] [Google Scholar]
- 10.Wasserstein D., Henry P., Paterson J.M., Kreder H.J., Jenkinson R. Risk of total knee arthroplasty after operatively treated tibial plateau fracture: a matched-population-based cohort study. J Bone Joint Surg Am. 2014;96:144–150. doi: 10.2106/JBJS.L.01691. [DOI] [PubMed] [Google Scholar]
- 11.Singleton N., Sahakian V., Muir D. Outcome after tibial plateau fracture: how important is restoration of articular congruity? J Orthop Trauma. 2017;31:158–163. doi: 10.1097/BOT.0000000000000762. [DOI] [PubMed] [Google Scholar]
- 12.Parkkinen M. Factors predicting the development of early osteoarthritis following lateral tibial plateau fractures: mid-term clinical and radiographic outcomes of 73 operatively treated patients. Scand J Surg. 2014;103:256–262. doi: 10.1177/1457496914520854. [DOI] [PubMed] [Google Scholar]
- 13.Kulkarni S.G. Use of a raft construct through a locking plate without bone grafting for split-depression tibial plateau fractures. J Orthop Surg. 2015;23:331–335. doi: 10.1177/230949901502300315. [DOI] [PubMed] [Google Scholar]
- 14.Thamyongkit S. The distal femur is a reliable guide for tibial plateau fracture reduction: a study of measurements on 3D CT scans in 84 healthy knees. J Orthop Surg Res. 2018;13:224. doi: 10.1186/s13018-018-0933-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kellgren J.H., Lawrence J.S. Radiological assessment of osteo-arthrosis. Ann Rheum Dis. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Fragomen A.T., Rozbruch S.R. The mechanics of external fixation. HSS J. 2007;3:13–29. doi: 10.1007/s11420-006-9025-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ferreira N., Marais L.C. Bicondylar tibial plateau fractures treated with fine-wire circular external fixation. Strat Traum Limb Recon. 2014;9:25–32. doi: 10.1007/s11751-014-0185-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Keightley A.J. Ilizarov management of Schatzker IV to VI fractures of the tibial plateau: 105 fractures at a mean follow-up of 7.8 years. Bone Joint Lett J. 2015;97-B:1693–1697. doi: 10.1302/0301-620X.97B12.34635. [DOI] [PubMed] [Google Scholar]
- 19.Kumar A., Whittle A.P. Treatment of complex (Schatzker Type VI) fractures of the tibial plateau with circular wire external fixation: retrospective case review. J Orthop Trauma. 2000;14:339–344. doi: 10.1097/00005131-200006000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Stamer D.T. Bicondylar tibial plateau fractures treated with a hybrid ring external fixator: a preliminary study. J Orthop Trauma. 1994;8:455–461. [PubMed] [Google Scholar]
- 21.Ali A.M., Burton M., Hashmi M., Saleh M. Outcome of complex fractures of the tibial plateau treated with a beam-loading ring fixation system. J Bone Joint Surg Br. 2003;85:691–699. [PubMed] [Google Scholar]
- 22.Dendrinos G.K., Kontos S., Katsenis D., Dalas A. Treatment of high-energy tibial plateau fractures by the Ilizarov circular fixator. J Bone Joint Surg Br. 1996;78:710–717. [PubMed] [Google Scholar]
- 23.DeCoster T.A., Nepola J.V., el-Khoury G.Y. Cast brace treatment of proximal tibia fractures. A ten-year follow-up study. Clin Orthop Relat Res. 1988:196–204. [PubMed] [Google Scholar]
- 24.Giannoudis P.V., Tzioupis C., Papathanassopoulos A., Obakponovwe O., Roberts C. Articular step-off and risk of post-traumatic osteoarthritis. Evidence today. Injury. 2010;41:986–995. doi: 10.1016/j.injury.2010.08.003. [DOI] [PubMed] [Google Scholar]
- 25.Kateros K., Galanakos S.P., Kyriakopoulos G., Papadakis S.A., Macheras G.A. Complex Tibial Plateau Fractures Treated by Hybrid External Fixation System: a correlation of followup computed tomography derived quality of reduction with clinical results. Indian J Orthop. 2018;52:161–169. doi: 10.4103/ortho.IJOrtho_300_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.