Abstract
Purpose
To evaluate agreement between pre- and post-laparoscopy gynecological diagnosis in order to demonstrate the rationality of this minimally invasive technique use in gynecological propaedeutics.
Methods
Retrospective chart review study conducted between March 2010 and October 2016 based on a convenience sample. 315 patients undergoing surgical laparoscopy at the Center of Gynecologic Endoscopy and Family Planning of Botucatu Medical School/UNESP. Pre- and postoperative diagnoses were compared by the diagnosis agreement test considering the proportions of events.
Results
Laparoscopy contributed to diagnosis in 59.6% of infertility cases (P>0.05), in 93.7% of chronic pelvic pain of undetermined origin (P<0.01) and conclusively elucidated the diagnosis of acute abdomen and the ruling out of tubo-ovarian abcess (P<0.05). Laparoscopy also increased the diagnosis of pelvic-abdominal adhesions in 76.7% (P>0.05).
Conclusion
The use of laparoscopy considerably contributed to diagnostic elucidation, especially in cases of undetermined chronic pelvic pain.
Key words: Laparoscopy; Endometriosis; Infertility, Female; Pelvic Pain; Techniques; Education, Medical
Introduction
Diagnosis plays a crucial role in clinical practice. It is the basis for developing an adequate treatment plan and establishing effective patient management strategies 1 . Accurate diagnosis reduces the risk of unnecessary therapies and optimizes the use of resources, particularly when they are limited, bringing benefits throughout the medical assistance process 1 , 2 . In the field of Gynecology, a careful diagnosis is especially critical because a great part of the symptoms and diseases that affect women may directly correlate with other specialties. Thus, misdiagnosis can shortly lead to the worsening of a patient’s condition, aggravating morbidity and causing higher costs to the healthcare system3, 4 .
Over the past years, laparoscopy has become a powerful propedeutic as well as therapeutic tool of modern gynecological practice. It can reduce the number of innappropiate procedures and unnecessary treatments with very low complication rates 5 - 9 . In conjunction with other propedeutic procedures, laparoscopy may change the diagnostic conclusion in many gynecological cases with increased efficiency in the diagnosis of conditions undetected during previous clinical and ultrasound examinations 5 - 9 ,9- 12 .
Nonetheless, in many countries, medical residency programs in gynecology do not include laparoscopic training, be it for surgical therapeutic or even purely diagnostic procedures. Therefore, this study aimed to assess patients underwent laparoscopy to evaluate the consistency of agreement between pre- and post-laparoscopy gynecological diagnosis in order to demonstrate the rationality of laparoscopy use in gynecological propaedeutics, and thus expand the discussion about the basis of the training of future gynecologists.
Methods
Study design and sample selection
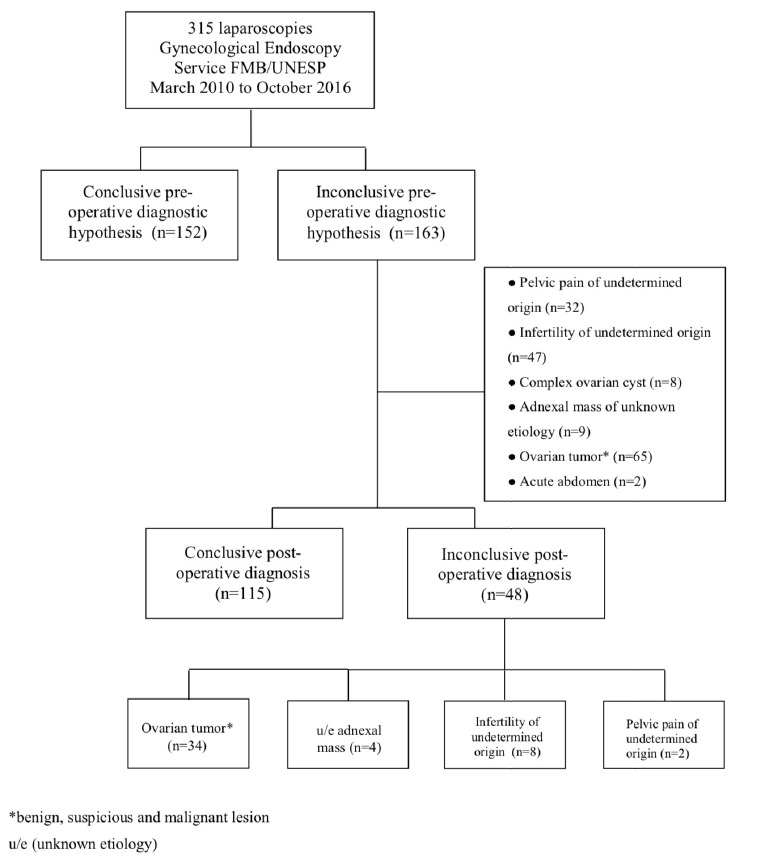
This retrospective chart review study was conducted to evaluale all patients undergoing surgical laparoscopy at the Center of Gynecologic Endoscopy and Family Planning of Botucatu Medical School/UNESP, Brazil between March 2010 and October 2016 (Fig. 1). Pre- and postoperative data were retrieved from the electronic database of the Botucatu Medical School Hospital/UNESP. The study was approved by the institution’s Committee of Research Ethics and was exempted from the requirement for informed consent as it involved deidentified data acquired during routine care, and did not involve any biological material or contact with the patients.
Figure 1. Flowchart of diagnosis in 315 patients who underwent surgical laparoscopy between March 2010 and October 2016 in the Gynecologic Endoscopy Service of Botucatu Medical School/UNESP.
Data collection
Data, such as age, body mass index (BMI= kg/m²), parity, abortion, age at menarche, date of last menstruation, menstrual pattern, use of hormone therapy, history of pelvic inflammatory disease (PID), presence of systemic arterial hypertension (SAH), diabetes mellitus, thiroid diseases, dyslipidemia and smoking were transcribed into an Excel spreadsheet for analysis. Information on patients’ clinical complaints, transvaginal-pelvic ultrasound findings, anatomopathological findings, type of surgical procedures performed, and the rate of complications observed before, during and after laparoscopy were also comparatively assessed.
Statistical analysis
Descriptive statistical analysis was performed. The absolute and relative frequencies of the study parameters were assessed. Mean, standard deviation, and minimum-maximum values of quantitative variables, as well as the absolute frequency and percentage of qualitative variables were estimated. Pre- and postoperative diagnoses were compared by the diagnosis agreement test considering the proportions of events 13 .
Results
Patient mean age was 35 years. The majority of women were overweight (BMI= 26.94 ±5.52) and in reproductive age (84.1%) (Table 1). Hormone contraceptives were used by 34.6%, and history of treatment for uterine infection was reported by 11.4% of the patients. The most frequently reported complaint was chronic pelvic pain (34%), followed by dysmenorrhea (15.9%), desire for definitive contraception (15.6%), and desire for reproduction (13%) (Table 2). Eleven per cent of the women complained of significantly increased menstrual flow, while 14.3% had no clinical complaint and were referred to surgery due to incidental image findings, notably regarding adnexal formations. Nineteen per cent of the patients reported more than one clinical complaint of relevance.
Table 1. Clinical and epidemiological characteristics of 315 patients who underwent surgical laparoscopy between March 2010 and October 2016 in the Gynecologic Endoscopy Service of Botucatu Medical School/UNESP.
| Age | 35 (13;72) |
| BMI | 26.94 (±5.52) |
| Gestation | 2 (0;11) |
| Parity | 1 (0;8) |
| Abortion | 0 (0;3) |
| C-section | 0 (0;4) |
| Menacme | 265 (84.1) |
| Menopause | 50 (15.9) |
| Hormone contraceptive | 109 (34.6) |
| PID history | 36 (11.4) |
| SAH | 53 (16.8) |
| Diabetes | 13 (4.1) |
| Thireoidpathy | 18 (5.7) |
| Dislipidemia | 12 (3.8) |
| Smoking | 39 (12.4) |
Median (minimum and maximum); Mean values (± standard deviation)
Frequency Distribution in absolute numbers and percentages n(%)
BMI= Body mass index; PID= Pelvic inflammatory disease; SAH= systemic arterial hypertension.
Table 2 . Clinical characteristics of 315 patients who underwent surgical laparoscopy between March 2010 and October 2016 in the Gynecologic Endoscopy Service of Botucatu Medical School/UNESP.
| Chronic pelvic pain | 107 (34) |
| Dysmenorrhea | 50 (15.9) |
| Desire for definitive contraception | 49 (15.6) |
| Asymptomatic | 45 (14.3) |
| Reproduction desire | 41 (13) |
| Increased menstrual flow | 36 (11.4) |
| Acute pelvic pain | 15 (4.8) |
| Dyspareunia | 14 (4.4) |
| Irregular menstrual cycle | 8 (2.5) |
| Dyschezia | 5 (1.6) |
| Postmenopausal bleeding | 4 (1.3) |
| Dysuria | 1 (0.3) |
Frequency distribution in absolute numbers and percentages n(%)
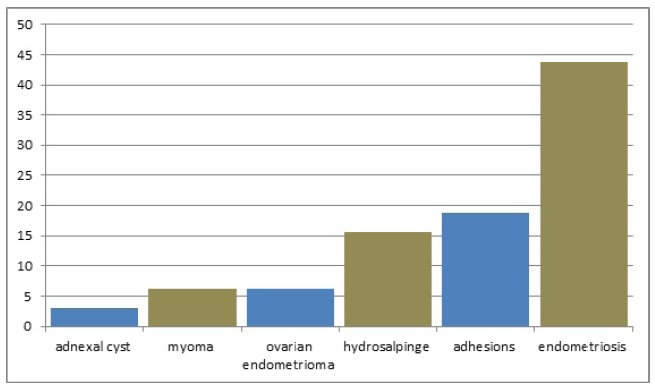
Laparoscopy was inconclusive in 17% of the patients assessed due to infertility with no apparent cause. However, in 83% of these cases it was essential for establishing the diagnosis of polycystic ovary (2.1%) with no other reason for infertility, ovarian endometrioma (6.4%), adhesions (17%), and endometriosis (57.5%) (P>0.05) (Fig. 2). The diagnosis of chronic pelvic pain of undetermined origin was postoperatively diagnosed as adnexal cyst (3.1%), myoma (6.3%), ovarian endometrioma (6.3%), hydrosalpinge (15.6%), adhesions (18.7%), and endometriosis (43.7%) (Fig. 3).
Figure 2. Post-laparoscopy diagnosis of preoperative undefined infertility.
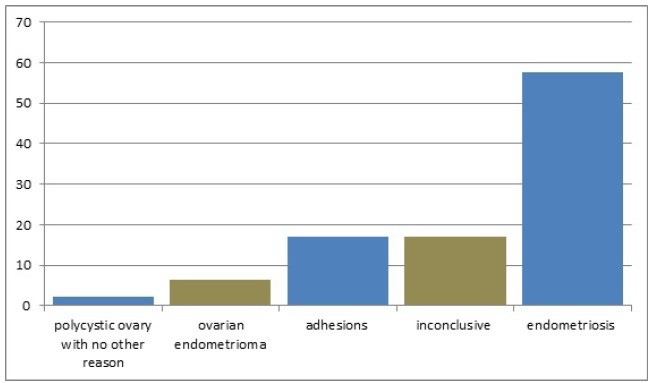
Figure 3. Post- laparoscopy diagnosis of preoperative chronic pelvic pain of undetermined origin.
The pre-laparoscopy diagnosis of complex ovarian cyst was related with the post-laparoscopy diagnosis of hemorrhagic corpus luteum (37.5%), ovarian tumor (ovarian teratoma on anatomopathology) (50%), and retention cyst (12.5%). In 40% of the cases with a preoperative diagnosis of ovarian tumor, and in 77.8% of cases with a diagnosis of adnexal mass of unknown etiology, laparoscopy detected uterine myoma, endometriosis, adhesions and tubo-ovarian abcesses, but with no statistical differences (Table 3).
Table 3 . Distribution of agreement between pre- and postoperative diagnoses.
| PRE-diagnosis | POST-diagnosis | Total | P value | |
|---|---|---|---|---|
| Agreement | Disagreement | |||
| Infertility | 40.4% | 59.6% | 47 | >0.05 |
| Pelvic pain | 6.3% | 93.7% | 32 | <0.01 |
| Complex ovarian cyst | 12.5% | 87.5% | 8 | < 0.05 |
| Ovarian tumor | 60.0% | 40.0% | 65 | >0.05 |
| u/e Adnexal mass | 22.2% | 77.8% | 9 | >0.05 |
| Acute abdomen | 0.0% | 100.0% | 2 | <0.05 |
| Tubo-ovarian abcess | 0.0% | 100.0% | 2 | <0.05 |
| Adhesions | 23.3% | 76.7% | 7 | >0.05 |
Diagnosis agreement test (pre-post) considering the proportions of events
P<0.05 statistical significance
u/e (unknown etiology)
In general, laparoscopy contributed to diagnosis elucidation in 59.6% of infertility cases (P>0.05), 93.7% of chronic pelvic pain of undetermined origin (P<0.01), 87.5% of complex ovarian cyst cases (P<0.05), 40% of ovarian tumor cases (P>0.05), and 77.8% of adnexal mass of unknown etiology cases (p>0.05) (Table 3). Furthermore, in this study, laparoscopy changed the preoperative diagnosis of acute abdomen to tubo-ovarian abcess (P<0.05), and ruled out the preoperative diagnostic hypothesis of tubo-ovarian abcess by revealing an ectopic pregnancy and apendicitis (P<0.05). Laparoscopy also determined a 76.7% increase in the diagnosis of pelvic-abdominal adhesions (P>0.05). The rate of complications in our study was low, with emphasis on bladder (0.6%), ureter (0.3%) and intestinal injuries (0.3%).
Discussion
Compared to conventional open surgery, laparoscopy has numerous advantages, such as (1) less postoperative pain, (2) shorter hospital stay, (3) lower rates of postoperative complications, (4) early return to daily activities, and (5) better esthetic effect. These benefits combined decrease the direct and indirect costs related to the surgical procedure 3 , 5 , 7 , 11 . In cases where the etiology of the condition is not fully clear, laparoscopy has been shown to be a safe and reliable adjunct to gynecological diagnosis that may spare patients an exploratory laparotomy and its greater risks of complications 14 - 19 .
To some authors, laparoscopy should be an integral part of the evaluation of women with pelvic pain of undetermined origin due to its safety and reliability 20 . Others additionally state that laparoscopy allows for a much more accurate gynecological diagnosis as it may confirm or rule out clinical impressions, establish a diagnosis, follow and explore the course of the disease as well as change or complement treatment 21 , 22 . Several comparative studies have shown that the use of laparoscopy increased the rate of success in the diagnosis of different gynecological conditions 9 , 22 , 23 . Despite the evidence reported in the literature, in many countries, medical residency programs aiming at providing basic introductory training in diagnostic laparoscopy do not integrate as part of the curriculum. In countries were those programs were implemented there is no standardized training adopted leading to a very heterogeneous formation of future professionals 24 - 26 .
Regulatory bodies have already emphasized the need of expanding validated training programs to prepare professionals for the increasing use of laparoscopy before progression to real procedures 25 . Nevertheless, difficulties in implementing a training program for residents in gynecology are encountered in many countries. The main obstacles reported are lack of planning and structure within institutions, cost constraints, shortage of skilled professionals available for teaching and guide residents and limited residents’ working hours 24 , 25 , 27 - 30 .
It is estimated that 73% of programs lead off laparoscopic skills in North America but only 29% of residencies provide a structured surgical curriculum and only 55% of residency programs have facilities for training in laparoscopy in the United States 26 , 31 , 32 . Moreover, a recent study on accredited North American Obstetrics and Gynecology residency programs revealed that more than 40% were dissatisfied with their current laparoscopy training 33 . As a matter of fact, despite residency programs are trying to incorporate simulation into the resident training curriculum to supplement the hands-on experience gained in the operating room, this simulation laboratories continue to be under utilized by surgical trainees 29 . In most countries, including Latin America, there is not even teaching models for laparoscopic skills or validated tools for its evaluation during residency 32 .
In this study, after excluding the cases of adnexal and/or ovarian diseases (adnexal masses of unknown etiology, ovarian tumors and complex ovarian cysts) which require histopathological confirmation and cannot be accurately identified surgically, diagnostic elucidation after laparoscopy occurred in 93.7% of the cases of pelvic pain of unknown etiology (P<0.01), and 59.6% of the cases of infertility with no apparent cause (p>0.05). Furthermore, laparoscopy was conclusive in the diagnosis of acute abdomen, even though there was a low number of cases with this condition in our series (P<0.05).
The introduction of laparoscopy into clinical practice has opened up new avenues for the diagnosis and management of chronic pelvic pain. It is estimated that more than half of patients with a normal preoperative pelvic examination will present abnormal findings during the laparoscopic procedure 11 , 34 . The literature shows that in women with chronic pelvic pain undergoing laparoscopy, the diagnosis may remain inconclusive in approximately 35% of cases, and endometriosis and adhesions can be diagnosed in 33% and 24%, respectively 10 , 11 , 34 , 35 . These findings represent about 90% of all laparoscopies in women with pelvic pain suggesting that the predominant role of laparoscopy in the evaluation of these patients is to diagnose or rule out endometriosis and adhesions.
Except in cases of endometrioma, ovarian retention syndrome and ovarian residual syndrome, ovarian cysts are not a common cause of chronic pelvic pain. The laparoscopic assessment of patients with chronic pelvic pain reveals ovarian cysts in only 4% of all cases excluding endometriomas 11 . Endometriosis, in turn, is a common laparoscopic diagnosis in patients with chronic pelvic pain, found in 15% to 80% of women undergoing surgery for chronic pelvic pain 12 , 36 .
Similarly, endometriosis is estimated to affect up to 50% of infertile women, and its severity appears to correlate with reduced fertility 37 . Infertility is the classical indication for propedeutic/therapeutic laparoscopy, which is indispensable to elucidate cases with no apparent cause 38 - 40 . According to non-controlled retrospective studies, diagnostic laparoscopy performed after several failed ovulation induction treatment cycles reveal significant pelvic pathology amenable to surgical treatment 40 . Laparoscopy indicates intra-abdominal abnormalities in 36%-68% of cases, even after normal hysterosalpingography 38 , 39 . Depending on the severity of laparoscopic findings, the initial treatment decision may be replaced by direct laparoscopic intervention, a laparotomic approach to fertility restoration or in vitro fertilization. This implies that, in addition to being a clinically important diagnostic tool, laparoscopy is essential for infertility treatment decision making 39 .
In this study, laparoscopy also proved to aid the diagnosis of tubo-ovarian abcess (P<0.05). Despite the small number of cases, these findings corroborate the role of laparoscopy as a specific clinical criterion for the diagnosis of complicated pelvic inflammatory disease 15 , 41 . Although no statistical difference was reached, laparoscopy increased in 76.7% the diagnosis of pelvic-abdominal adhesions, demonstrating that preoperative propedeutics is still ineffective to establish the diagnosis of this condition. Adhesions are commmon etiologic factors for infertility, dyspareunia, intestinal obstruction and chronic pelvic pain albeit their role in the physiopathology of pain remains unclear 42 . Laparoscopy in 1,061 patients revealed that pelvic adhesions (found in 32.5% of cases) is the most common cause of chronic pain 34 , 43 .
The use of laparoscopy can reveal treatable conditions, not detected using other methods, with a very low rate of complications. In our study, the rate of potentially severe complications ranged from 0.3% to 0.6%. A survey of 6.451 laparoscopic procedures showed an overall complication rate of 0.65% (42/6451). However, this rate rose to 0.80% (39/4865) when surgical laparoscopy was compared to merely diagnostic laparoscopy that was associated with a complication rate of 0.19% (3/1586) (P<0.001) 44 .
The benefits of this minimally invasive technique indicate that an in-depth discussion on reshaping medical residency programs is necessary as to adjust them to the new technology available as well as to today’s reality. Given its propedeutic nature and association with very low complications risks, diagnostic laparoscopy should be routinely addressed in the training of future gynecologists. All efforts should be made so that health policies contemplate the dissemination and increasing use of laparoscopy, which has been demonstrated to offer numerous advantages throughout the medical assistance system, especially in the field of gynecology.
Take home messages
Since it is not included in the training of resident doctors in most services worldwide, laparoscopy’s potential for development in still considerable;
The propedeutic role of laparoscopy for elucidating the diagnosis of several conditions of undetermined origin, notably complaints related to infertility and chronic pelvic pain, should not be disregarded;
Programs of medical residency in gynecology including training in the use of propedeutic/diagnostic laparoscopy should be encouraged by medical care improvement policies. This can bring direct and indirect benefits, besides reducing costs throughout the healthcare system;
Training in therapeutic laparoscopy should be provided in specialized centers because the learning curve, despite being reproducible, takes quite long and depends on the number of procedures performed by the surgeon.
Acknowledgements
Special thanks to Professors Eliana Aguiar Petri Nahás e Jorge Nahás Neto for their academic-scientific support, to Mariza Branco da Silva for manuscript English revision, and Rosemary Cristina da Silva for reviewing bibliography.
Financial source: none
Research performed at Clinics Hospital of Botucatu, Gynecological Endoscopy and Family Planning Sector, Department of Gynecology and Obstetrics, Botucatu Medical School, Universidade Estadual Paulista (UNESP), Botucatu-SP, Brazil.
References
- 1.Bachmann LM, ter Riet G, Clark TJ, Gupta JK, Khan KS. Probability analysis for diagnosis of endometrial hyperplasia and cancer in postmenopausal bleeding an approach for a rational diagnostic workup. Acta Obstet Gynecol Scand. 2003;82(6):564–569. doi: 10.1034/j.1600-0412.2003.00176.x. [DOI] [PubMed] [Google Scholar]
- 2.Reid MC, Lachs MS, Feinstein AR. Use of methodological standards in diagnostic test research Getting better but still not good. JAMA. 1995;274(8):645–651. [PubMed] [Google Scholar]
- 3.Tsaltas J, Magnus A, Mamers PM, Lawrence AS, Lolatgis N, Healy DL. Laparoscopic and abdominal hysterectomy a cost comparison. Med J Aust. 1997;166(4):205–207. doi: 10.5694/j.1326-5377.1997.tb140078.x. [DOI] [PubMed] [Google Scholar]
- 4.Flasar MH, Goldberg E. Acute abdominal pain. Med Clin North Am. 2006;90(3):481–503. doi: 10.1016/j.mcna.2005.11.005. [DOI] [PubMed] [Google Scholar]
- 5.Ou CS, Rowbotham R. Laparoscopic diagnosis and treatment of nontraumatic acute abdominal pain in women. J Laparoendosc Adv Surg Tech A. 2000;10(1):41–45. doi: 10.1089/lap.2000.10.41. [DOI] [PubMed] [Google Scholar]
- 6.Sozuer EM, Bedirli A, Ulusal M, Kayhan E, Yilmaz Z. Laparoscopy for diagnosis and treatment of acute abdominal pain. J Laparoendosc Adv Surg Tech A. 2000;10(4):203–207. doi: 10.1089/109264200421586. [DOI] [PubMed] [Google Scholar]
- 7.Kondo W, Rangel M, Tirapelle R, Garcia MJ, von Bahten LC, Laux GL, Smaniotto B. Emprego da laparoscopia em mulheres com dor abdominal aguda. Rev Bras Videocir. 2006;4(1):3–8. [Google Scholar]
- 8.Tan BP, Ong CL. Ultrasonographical diagnosis of acute gynaecological pain. Singapore Med J. 2008;49(6):511–515. [PubMed] [Google Scholar]
- 9.Hsu AL, Sinaii N, Segars J, Nieman LK, Stratton P. Relating pelvic pain location to surgical findings of endometriosis. Pt 1Obstet Gynecol. 2011;118(2):223–230. doi: 10.1097/AOG.0b013e318223fed0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Howard FM. The role of laparoscopy in the evaluation of chronic pelvic pain pitfalls with a negative laparoscopy. J Am Assoc Gynecol Laparosc. 1996;4(1):85–94. doi: 10.1016/s1074-3804(96)80116-2. [DOI] [PubMed] [Google Scholar]
- 11.Howard FM. The role of laparoscopy as a diagnostic tool in chronic pelvic pain. Baillieres Best Pract Res Clin Obstet Gynaecol. 2000;14(3):467–494. doi: 10.1053/beog.1999.0086. [DOI] [PubMed] [Google Scholar]
- 12.Lamvu G, Tu F, As-Sanie S, Zolnoun D, Steege JF. The role of laparoscopy in the diagnosis and treatment of conditions associated with chronic pelvic pain. Obstet Gynecol Clin North Am. 2004;31(3):619–630. doi: 10.1016/j.ogc.2004.05.003. [DOI] [PubMed] [Google Scholar]
- 13.Norman GR, Streiner DL. Biostatistics: the bare essentials. 3ed. Shelton, Conn: People's Medical Pub. House; 2008. [Google Scholar]
- 14.Mereu L, Ruffo G, Landi S, Barbieri F, Zaccoletti R, Fiaccavento A, Stepniewska A, Pontrelli G, Minelli L. Laparoscopic treatment of deep endometriosis with segmental colorectal resection short-term morbidity. J Minim Invasive Gynecol. 2007;14(4):463–469. doi: 10.1016/j.jmig.2007.02.008. [DOI] [PubMed] [Google Scholar]
- 15.Schorge JO, Williams JW. Williams gynecology. New York: McGraw-Hill Medical; 2008. [Google Scholar]
- 16.Shrestha J, Saha R. Comparison of laparoscopy and laparotomy in the surgical management of ectopic pregnancy. J Coll Physicians Surg Pak. 2012;22(12):760–764. [PubMed] [Google Scholar]
- 17.Coolen AL, van Oudheusden AM, van Eijndhoven HW, van der Heijden TP, Stokmans RA, Mol BW, Bongers MY. A Comparison of complications between open abdominal sacrocolpopexy and laparoscopic sacrocolpopexy for the treatment of vault prolapse. Obstet Gynecol Int. 2013;2013:528636–528636. doi: 10.1155/2013/528636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Liu M, Li L, He Y, Peng D, Wang X, Chen W, Fu X, Ma Y. Comparison of laparoscopy and laparotomy in the surgical management of early-stage ovarian cancer. Int J Gynecol Cancer. 2014;24(2):352–357. doi: 10.1097/IGC.0000000000000033. [DOI] [PubMed] [Google Scholar]
- 19.Terai Y, Tanaka T, Sasaki H, Kawaguchi H, Fujiwara S, Yoo S, Tanaka Y, Tsunetoh S, Kanemura M, Ohmichi M. Total laparoscopic modified radical hysterectomy with lymphadenectomy for endometrial cancer compared with laparotomy. J Obstet Gynaecol Res. 2014;40(2):570–575. doi: 10.1111/jog.12194. [DOI] [PubMed] [Google Scholar]
- 20.Newham AP, van der Spuy ZM, Nugent F. Laparoscopic findings in women with chronic pelvic pain. S Afr Med J. 1996;86(9 Suppl):1200–1203. [PubMed] [Google Scholar]
- 21.Sharma D, Dahiya K, Duhan N, Bansal R. Diagnostic laparoscopy in chronic pelvic pain. Arch Gynecol Obstet. 2011;283(2):295–297. doi: 10.1007/s00404-010-1354-z. [DOI] [PubMed] [Google Scholar]
- 22.Baloch S, Khaskheli MN, Malik AM. Diagnostic laparoscopic findings in chronic pelvic pain. J Coll Physicians Surg Pak. 2013;23(3):190–193. [PubMed] [Google Scholar]
- 23.Janssen EB, Rijkers AC, Hoppenbrouwers K, Meuleman C, D'Hooghe TM. Prevalence of endometriosis diagnosed by laparoscopy in adolescents with dysmenorrhea or chronic pelvic pain a systematic review. Hum Reprod Update. 2013;19(5):570–582. doi: 10.1093/humupd/dmt016. [DOI] [PubMed] [Google Scholar]
- 24.Patel NR, Makai GE, Sloan NL, Della Badia CR. Traditional versus simulation resident surgical laparoscopic salpingectomy training a randomized controlled trial. J Minim Invasive Gynecol. 2016;23(3):372–377. doi: 10.1016/j.jmig.2015.11.005. [DOI] [PubMed] [Google Scholar]
- 25.Shore EM, Grantcharov TP, Husslein H, Shirreff L, Dedy NJ, McDermott CD, Lefebvre GG. Validating a standardized laparoscopy curriculum for gynecology residents a randomized controlled trial. Am J Obstet Gynecol. 2016;215(2):204–204. doi: 10.1016/j.ajog.2016.04.037. [DOI] [PubMed] [Google Scholar]
- 26.Moawad GN, Tyan P, Kumar D, Krapf J, Marfori C, Abi Khalil ED, Robinson J. Determining the effect of external stressors on laparoscopic skills and performance between obstetrics and gynecology residents. J Surg Educ. 2017;74(5):862–866. doi: 10.1016/j.jsurg.2017.03.001. [DOI] [PubMed] [Google Scholar]
- 27.Nagendran M, Gurusamy KS, Aggarwal R, Loizidou M, Davidson BR. Virtual reality training for surgical trainees in laparoscopic surgery. Cochrane Database Syst Rev. 2013;(8):CD006575–CD006575. doi: 10.1002/14651858.CD006575.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Dehabadi M, Fernando B, Berlingieri P. The use of simulation in the acquisition of laparoscopic suturing skills. Int J Surg. 2014;12(4):258–268. doi: 10.1016/j.ijsu.2014.01.022. [DOI] [PubMed] [Google Scholar]
- 29.Shetty S, Zevin B, Grantcharov TP, Roberts KE, Duffy AJ. Perceptions, training experiences, and preferences of surgical residents toward laparoscopic simulation training a resident survey. J Surg Educ. 2014;71(5):727–733. doi: 10.1016/j.jsurg.2014.01.006. [DOI] [PubMed] [Google Scholar]
- 30.Enani G, Watanabe Y, McKendy KM, Bilgic E, Feldman LS, Fried GM, Vassiliou MC. What are the training gaps for acquiring laparoscopic suturing skills. J Surg Educ. 2017;74(4):656–662. doi: 10.1016/j.jsurg.2016.12.004. [DOI] [PubMed] [Google Scholar]
- 31.Kirby TO, Numnum TM, Kilgore LC, Straughn JM. A prospective evaluation of a simulator-based laparoscopic training program for gynecology residents. J Am Coll Surg. 2008;206(2):343–348. doi: 10.1016/j.jamcollsurg.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 32.Fernandes CF, Ruano JM, Kati LM, Noguti AS, Girao MJ, Sartori MG. Assessment of laparoscopic skills of Gynecology and Obstetrics residents after a training program. Einstein (Sao Paulo) 2016;14(4):468–472. doi: 10.1590/s1679-45082016ao3752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shore EM, Lefebvre GG, Grantcharov TP. Gynecology resident laparoscopy training present and future. Am J Obstet Gynecol. 2015;212(3):298–301. doi: 10.1016/j.ajog.2014.07.039. [DOI] [PubMed] [Google Scholar]
- 34.Chhetri S. Laparoscopy as a diagnostic tool in the evaluation of chronic pelvic pain in women. World J Laparosc Surg. 2009;2(2):30–32. doi: 10.3126/jnhrc.v7i1.2279. [DOI] [Google Scholar]
- 35.Cox L, Ayers S, Nala K, Penny J. Chronic pelvic pain and quality of life after laparoscopy. Eur J Obstet Gynecol Reprod Biol. 2007;132(2):214–219. doi: 10.1016/j.ejogrb.2006.04.020. [DOI] [PubMed] [Google Scholar]
- 36.Howard FM. The role of laparoscopy in chronic pelvic pain promise and pitfalls. Obstet Gynecol Surv. 1993;48(6):357–387. doi: 10.1097/00006254-199306000-00001. [DOI] [PubMed] [Google Scholar]
- 37.Cranney R, Condous G, Reid S. An update on the diagnosis, surgical management, and fertility outcomes for women with endometrioma. Acta Obstet Gynecol Scand. 2017;96(6):633–643. doi: 10.1111/aogs.13114. [DOI] [PubMed] [Google Scholar]
- 38.Fatum M, Laufer N, Simon A. Investigation of the infertile couple should diagnostic laparoscopy be performed after normal hysterosalpingography in treating infertility suspected to be of unknown origin? Hum Reprod. 2002;17(1):1–3. doi: 10.1093/humrep/17.1.1. [DOI] [PubMed] [Google Scholar]
- 39.Tanahatoe S, Hompes PG, Lambalk CB. Accuracy of diagnostic laparoscopy in the infertility work-up before intrauterine insemination. Fertil Steril. 2003;79(2):361–366. doi: 10.1016/s0015-0282(02)04686-1. [DOI] [PubMed] [Google Scholar]
- 40.Bosteels J, Van Herendael B, Weyers S, D'Hooghe T. The position of diagnostic laparoscopy in current fertility practice. Hum Reprod Update. 2007;13(5):477–485. doi: 10.1093/humupd/dmm014. [DOI] [PubMed] [Google Scholar]
- 41.Kreisel K, Torrone E, Bernstein K, Hong J, Gorwitz R. Prevalence of Pelvic inflammatory disease in sexually experienced women of reproductive age - United States, 2013-2014. MMWR Morb Mortal Wkly Rep. 2017;66(3):80–83. doi: 10.15585/mmwr.mm6603a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Karnath BM, Breitkopf DM. Acute and chronic pelvic pain in women. Hospital Physician. 2007:41–48. [Google Scholar]
- 43.Drozgyik I, Vizer M, Szabo I. Significance of laparoscopy in the management of chronic pelvic pain. Eur J Obstet Gynecol Reprod Biol. 2007;133(2):223–226. doi: 10.1016/j.ejogrb.2006.05.035. [DOI] [PubMed] [Google Scholar]
- 44.Wang PH, Lee WL, Yuan CC, Chao HT, Liu WM, Yu KJ, Tsai WY, Wang KC. Major complications of operative and diagnostic laparoscopy for gynecologic disease. J Am Assoc Gynecol Laparosc. 2001;8(1):68–73. doi: 10.1016/s1074-3804(05)60551-8. [DOI] [PubMed] [Google Scholar]


