Introduction
Key Teaching Points.
-
•
There are limitations of wide complex tachycardia differentiation algorithms when there is a history of a large myocardial infarction, even in presence of a clinical history highly suggestive of ventricular tachycardia.
-
•
Cardiac devices, even externally placed devices such as atrial clips, may cause local endocardial scar that can contribute to slow conduction and be a set-up for reentrant arrhythmias.
-
•
Detailed mapping of atrial tachycardia/atypical atrial flutter is imperative in identifying the mechanism and for successful ablation.
The use of algorithms to distinguish ventricular tachycardia (VT) from supraventricular tachycardia (SVT) with aberrancy when wide complex tachycardia (WCT) is encountered are well validated, with a sensitivity and specificity as high as 90%.1, 2, 3, 4 Some electrocardiogram (ECG) findings such as initial R wave in lead aVR have a specificity and positive predictive value reported nearing 100%. We present a case of a patient with WCT in whom clinical and ECG algorithms were highly suggestive of VT, but electrophysiological findings proved a macroreentrant left atrial (LA) flutter related to an AtriClip left atrial appendage (LAA) exclusion system (AtriCure, Mason, OH).
Case report
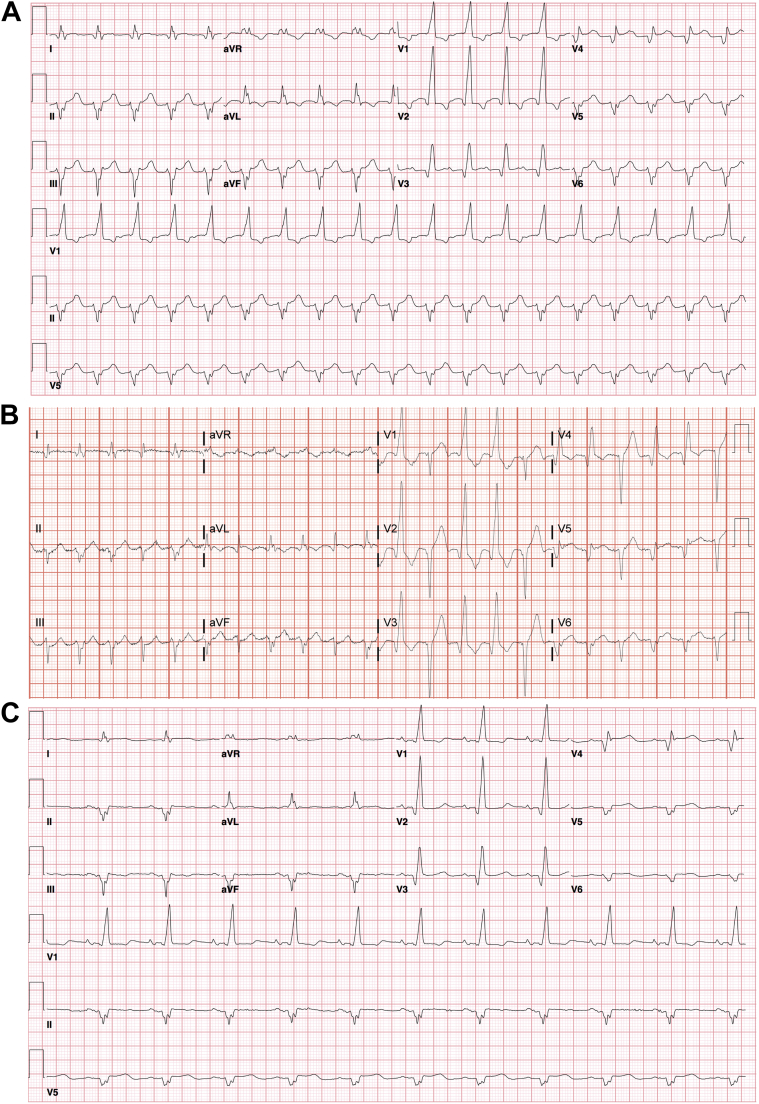
A 58-year-old male patient with a history of paroxysmal atrial fibrillation, aortic valve replacement for severe aortic stenosis, ischemic cardiomyopathy with an unrevascularized left anterior descending infarct, and left ventricular ejection fraction of 20%–25% was transferred to our institution with incessant, hemodynamically tolerated WCT. WCT was consistent with VT based on an atypical right bundle morphology with QRS duration of 160 ms, possible capture beats, and prominent R wave in lead aVR (Figure 1).1, 3 QRS morphology during sinus rhythm was not known at the time of his presentation.
Figure 1.
A: The 12-lead electrocardiogram (ECG) during wide complex tachycardia (WCT) showing atypical right bundle branch block and R wave in lead aVR. B: The 12-lead ECG during WCT with occasional narrow QRS complexes, possibly consistent with capture beats C: The 12-lead ECG during sinus rhythm after termination of WCT.
Intravenous adenosine given at the transferring facility reportedly had no effect on the tachycardia; however, rhythm strips were not available for review. The ECG morphology, while meeting all VT criteria, had a somewhat sharp initial component. This was potentially explained by a VT originating near the conduction system, and given his history of an anterior myocardial infarction a septal VT was suspected. The patient was taken to the electrophysiology laboratory for an electrophysiology study and presumptive VT ablation.
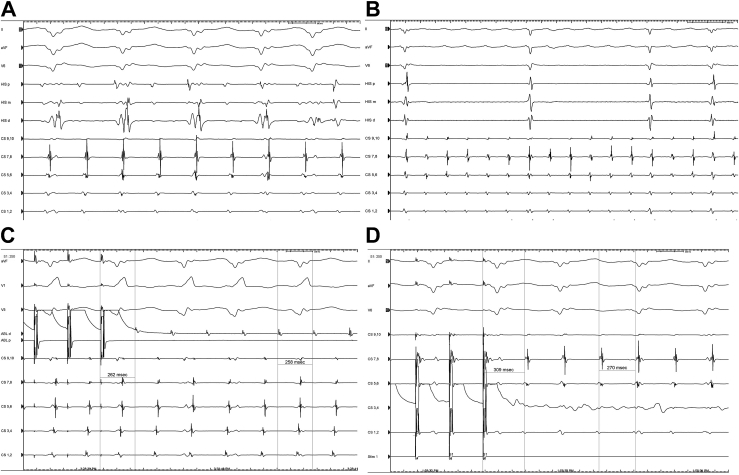
A coronary sinus decapolar catheter was placed to assess atrial rhythm and to exclude dual tachycardia and SVT with aberrancy. Coronary sinus recordings were consistent with atrial flutter (AFL) with a tachycardia cycle length of 220 ms, which was half the ventricular cycle length. Intravenous adenosine (24 mg) resulted in atrioventricular nodal block with continuation of AFL and resumption of 2:1 conduction with identical wide QRS morphology shortly after. During atrioventricular nodal block, intermittent narrow complex beats with precordial Q waves were also noted. The atrial rhythm was proven to be LA roof flutter by entrainment and activation mapping (Figure 2).
Figure 2.
A: Surface leads and intracardiac tracing during wide complex tachycardia showing atrial flutter (AFL) with cycle length of 220 ms and ventricular cycle length of 440 ms. B: Following 24 mg of intravenous adenosine, AFL persists despite atrioventricular node (AVN) block. Note surface electrocardiogram during AVN block shows 2 beats of narrow complex QRS (second and third QRS complex) with precordial Q waves similar to narrow complexes in Figure 1B. C: Entrainment of AFL from the left atrial roof shows concealed fusion with a postpacing interval (PPI)–tachycardia cycle length (TCL) of 4 ms. D: Entrainment of AFL from CS3,4 (distal CS) shows PPI–TCL of 39 ms. ABL = ablation; CS = coronary sinus; HIS = His catheter proximal (p), mid (m), and distal (d).
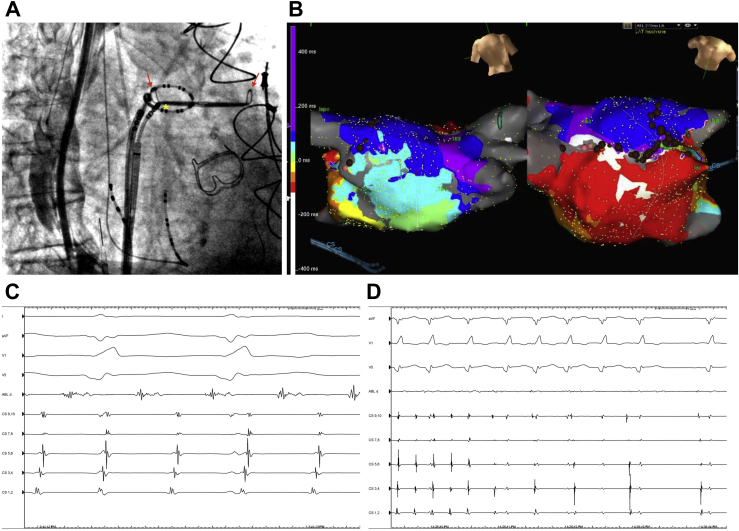
Endocardial voltage mapping (NavX, St Jude Medical, St Paul, MN) showed LA scar, most prominent near the right superior pulmonary vein. Additional localized scar was noted at the roof adjacent to the LAA. This scar fluoroscopically correlated with the position of an AtriClip LAA exclusion system (Figure 3) that was identified on initial fluoroscopic imaging. An LA roof line connecting left superior pulmonary vein (LSPV) to right superior pulmonary vein was performed with slowing and termination of AFL at the anterosuperior LAA/LSPV ridge adjacent to the AtriClip. The termination site consisted of a long fragmented signal (Figure 3). A line of block across the LA roof was confirmed with differential pacing.
Figure 3.
A: Right anterior oblique fluoroscopic view demonstrating the position of the AtriClip left atrial appendage (LAA) exclusion system (AtriCure, Mason, OH) with red arrows. Circular mapping catheter is in the left superior pulmonary vein (LSPV). Ablation catheter tip is at the location where atrial flutter (AFL) terminated during ablation (asterisk). B: Activation map of AFL showing propagation up the posterior left atrial wall and down the anterior wall. Brown dots show sites of ablation and green dot is the site of AFL termination. C: ABL d shows fractionated continuous signal on ABL distal positioned at the anterosuperior LAA/LSPV ridge (adjacent to AtriClip) at the site of AFL termination. D: Termination of atrial flutter with resumption of sinus rhythm. ABL = ablation; CS = coronary sinus.
The patient was discharged shortly after and had remained free of arrhythmias on 6-month follow-up.
Discussion
ECG algorithms for diagnosis of WCT failed to correctly identify the tachycardia. VT was highly likely based on ECG criteria in addition to the clinical history of ischemic cardiomyopathy. In the clinical background of cardiomyopathy, WCT unresponsive to adenosine is overwhelmingly suggestive of VT and should be treated as such, as was done upon initial presentation. ECG algorithm criteria may have limited utility in the presence of preexcited SVT, preexistent septal Q waves and bundle branch block, and idiopathic VT. However, presence of an initial R wave in aVR had a 98% specificity for VT based on the algorithm by Vereckei and colleagues.3
A low-amplitude fractionated R wave was seen in lead aVR during both tachycardia and sinus rhythm (the latter was identified only after termination of tachycardia). In addition, there was ECG evidence of a prior inferolateral and anterior myocardial infarction and right bundle branch block. Anterior plus inferior wall infarction increased the incidence of initial R wave in lead aVR during sinus rhythm in a large study.5 We postulated that the infarct pattern and the related preferential conduction around the large scar was responsible for the aVR pattern owing to loss of initial anteriorly and inferiorly directed forces with predominantly rightward activation.
The macroreentrant LA roof flutter in this case appears to be at least in part attributable to the LA scar adjacent to the surgically placed LAA exclusion device. De novo left AFL is uncommon in the absence of LA scar, which is usually owing to ablation of atrial fibrillation or previous mitral valve or left atrial surgery.6, 7, 8 Endocardial LA scar related to an Atriclip LAA exclusion device has not been previously described. Given the presence of scar at other sites in the left atrium, we could not rule out de novo scar in the region of the LAA exclusion device in this case.
Footnotes
Dr Shivkumar was supported by the National Institutes of Health (grant number R01HL084261 & OT2OD023848).
References
- 1.Brugada P., Brugada J., Mont L., Smeets J., Andries E.W. A new approach to the differential diagnosis of a regular tachycardia with a wide QRS complex. Circulation. 1991;83:1649–1659. doi: 10.1161/01.cir.83.5.1649. [DOI] [PubMed] [Google Scholar]
- 2.Vereckei A., Duray G., Szénási G., Altemose G.T., Miller J.M. Application of a new algorithm in the differential diagnosis of wide QRS complex tachycardia. Eur Heart J. 2007;28:589–600. doi: 10.1093/eurheartj/ehl473. [DOI] [PubMed] [Google Scholar]
- 3.Vereckei A., Duray G., Szénási G., Altemose G.T., Miller J.M. New algorithm using only lead aVR for differential diagnosis of wide QRS complex tachycardia. Heart Rhythm. 2008;5:89–98. doi: 10.1016/j.hrthm.2007.09.020. [DOI] [PubMed] [Google Scholar]
- 4.Vereckei A. Current algorithms for the diagnosis of wide QRS complex tachycardias. Curr Cardiol Rev. 2014;10:262–276. doi: 10.2174/1573403X10666140514103309. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Okamoto N., Simonson E., Ahuja S., Manning G. Significance of the initial R wave in lead aVR of the electrocardiogram in the diagnosis of myocardial infarction. Circulation. 1967;35:126–131. doi: 10.1161/01.cir.35.1.126. [DOI] [PubMed] [Google Scholar]
- 6.Garan H. Atypical atrial flutter. Heart Rhythm. 2008;5:618–621. doi: 10.1016/j.hrthm.2007.10.031. [DOI] [PubMed] [Google Scholar]
- 7.Anselme F. Macroreentrant atrial tachycardia: pathophysiological concepts. Heart Rhythm. 2008;5:S18–S21. doi: 10.1016/j.hrthm.2008.01.034. [DOI] [PubMed] [Google Scholar]
- 8.Morady F., Oral H., Chugh A. Diagnosis and ablation of atypical atrial tachycardia and flutter complicating atrial fibrillation ablation. Heart Rhythm. 2009;6:S29–S32. doi: 10.1016/j.hrthm.2009.02.011. [DOI] [PubMed] [Google Scholar]