Abstract
Objective:
Geographic differences may provide insight into what factors influence the likelihood that a child is diagnosed with ASD in the US, yet there have been few nationally representative surveys that have explored this topic. The current study expands the limited literature by analyzing regional differences in ASD prevalence, service utilization, and the presence of unmet needs within a nationally representative sample of children.
Methods:
Data were drawn from the 2014–2016 National Health Interview Survey (NHIS), a nationally representative household survey of the noninstitutionalized US population. Children 3–17 were included in the analytic sample. Prevalence estimates accounted for the complex survey design of the NHIS, and differences between geographic regions were compared using logistic/linear regressions with and without adjustment for child/family characteristics.
Results:
The prevalence of ASD was highest in the Northeast (3.0%), followed by the Midwest (2.4%), South (2.4%), and West (2.3%). A significant difference was found between the Northeast and West (p<.05). However, after accounting for child and family characteristics, this difference was no longer significant. Children with ASD in the Northeast were the most likely to have seen a specialist in the past year. Approximately 1 in 8 children with ASD experienced at least one unmet need, but there were no differences found by geographic region.
Conclusions:
Although differences in prevalence were not significant after adjustment, service utilization differences remained. It appears children with ASD in the Northeast utilize the greatest number of specialty services when compared to children with ASD from other parts of the country.
Keywords: autism spectrum disorder, national survey, children, prevalence, treatment
Autism spectrum disorder (ASD) refers to a group of neurodevelopmental disorders characterized by impairments in social communication and the presence of repetitive behaviors or restricted interests.1 Over the past two decades, numerous studies have shown an overall trend of increasing ASD prevalence over time.2–5 Previous studies have also consistently shown large geographic variation in the prevalence of ASD in the United States at a single time point.2–3,6 Multiple factors are thought to contribute to regional variation in ASD prevalence, including sociodemographic characteristics and availability of autism-related services.7–12
The most recent data from Centers for Disease Control and Prevention’s Autism and Developmental Disabilities Monitoring (ADDM) Network yielded an overall prevalence of 1.7%, with surveillance sites in different states reporting ASD prevalence ranging from 1.3% to 2.9%.2 ASD prevalence estimates based on administrative sources have also shown variability by geography.13–14 These geographic differences in ASD prevalence are not fully understood, although the distribution of surveillance site estimates from ADDM may be the product of some sites relying on data from medical records alone, while others utilized both medical records as well as educational records. Nonetheless, studies based exclusively on a review of existing records are usually not well-suited to simultaneously explore the array of factors that might contribute to regional differences—especially for individual- or family-level characteristics.
In the United States, sociodemographic characteristics have been observed to be associated with ASD prevalence. For instance, data from ADDM show that ASD prevalence is positively associated with increasing neighborhood-level socioeconomic status.15 One hypothesis for this association is that children of higher socio-economic status families are more likely to have access to services which may lead to ASD identification.16–17 It has also been posited that geographic differences in the availability of services might in themselves drive geographic differences in ASD prevalence,18 as previous research has suggested that a greater availability of autism services in urban areas might contribute to higher ASD prevalence in urban versus rural areas.19–20
An investigation of regional service utilization patterns among children with ASD may also provide insight in factors that may contribute to a higher ASD prevalence. In fact, two administrative studies of health service utilization (one utilizing data from the Healthcare Cost and Utilization Project (HCUP), the other from privately insured beneficiaries) have shown higher utilization of services in the Northeast than other regions of the country among children with ASD.21–22
As the observed prevalence of ASD continues to change over time, there is a need to investigate regional differences in ASD prevalence using recent and population-based information. Large national surveys such as the National Health Interview Survey (NHIS), from the National Center for Health Statistics (NCHS), are ideally suited for this type of investigation. The NHIS is designed to be nationally representative of the noninstitutionalized US population and collects timely, in-depth information on health conditions, health service utilization, and family sociodemographic characteristics. The primary goal of this study is to use recent NHIS data for children aged 3–17 years to examine: 1) whether regional differences in ASD prevalence exist in the United States, and 2) whether health service utilization and unmet needs differ among children with ASD living in different regions of the United States. Given notable health and service disparities seen between children living in rural and urban settings,23,24 a secondary analysis explores whether differential effects are seen by MSA status within different regions of the United States.
Methods
Data Source
The current study used data from the 2014–2016 NHIS. The NHIS is generally an in-person interview conducted in the respondent’s home, though some follow-up data collection may be conducted by telephone. The survey consists of three components, a family interview (collecting information about all members of the family), a sample adult interview (collecting detailed information about one randomly-selected adult per family), and a sample child interview (collecting detailed information about one randomly-selected child per family). The sample child interview is completed by a knowledgeable adult respondent, which is typically the child’s parent (approximately 91% of cases). Data for the current analysis utilized data from both the child and family interview. Response rates for the 2014–2016 Sample Child component of the NHIS ranged from 61.9%−66.6%. For more information about NHIS, visit https://www.cdc.gov/nchs/nhis.htm.
Sample
A total of 30,530 children between the ages of 3 and 17 years were included in the analytic sample, of which 711 children were ever diagnosed as having autism spectrum disorder. Missing data on ASD occurred in approximately 0.9% of cases.
Measures
Autism spectrum disorder:
An autism spectrum disorder case was defined based on an affirmative answer to the question “Has a doctor or other health professional ever told you that [child’s name] had autism, Asperger’s disorder, pervasive developmental disorder, or autism spectrum disorder?”
Geographic region:
States were grouped into four regions used by the U.S. Census Bureau, including the Northeast (Maine, Vermont, New Hampshire, Rhode Island, New York, New Jersey, Pennsylvania, Massachusetts, Connecticut), Midwest (Ohio, Illinois, Indiana, Michigan, Wisconsin, Minnesota, Iowa, Missouri, North Dakota, South Dakota, Kansas, Nebraska), South (Delaware, Maryland, District of Columbia, West Virginia, Virginia, Kentucky, Tennessee, North Carolina, South Carolina, Georgia, Florida, Alabama, Mississippi, Louisiana, Oklahoma, Arkansas, Texas), and West (Washington, Oregon, California, Nevada, New Mexico, Arizona, Idaho, Utah, Colorado, Montana, Wyoming, Alaska, Hawaii).
Sociodemographic characteristics:
Sociodemographic characteristics examined included the child’s sex, age (broken into age groups of 3–7, 8–12, 13–17 years of age), race and ethnicity (non-Hispanic white, non-Hispanic black, non-Hispanic other, Hispanic), insurance status (any private, public only (includes Medicaid, Children’s Health Insurance Program (CHIP), and other state sponsored coverage), uninsured), family income recorded as a percentage of the federal poverty level (<100%, 100–199%, 200–399%, ≥400%), educational attainment of the highest educated family member (less than high school education, high school education or General Education Diploma (GED), greater than high school education), family structure (two parents, single parent, other), metropolitan statistical area (MSA) status (large (a county or group of counties that includes an urbanized area with a population of at least 50 thousand, and has a combined population total of 1 million or more)), small (a county or group of counties that includes an urbanized area with a population of at least 50 thousand, but has a combined population total of less than 1 million), not in a MSA), and survey year.
Service utilization characteristics:
Respondents were asked a series of questions about the types of providers their child had seen in the past 12 months. The providers included a generalist (pediatrician, family medicine doctor, internal medicine doctor), a specialist, a mental health professional (psychiatrist, psychologist, psychiatric nurse, clinical social worker), or a therapist (physical therapist, speech therapist, respiratory therapist, audiologist, occupational therapist). A composite measure of specialty care was defined as children who had seen either a specialist, mental health professional, or therapist in the past 12 months. Respondents were also asked whether, and how many times, their child had received services at a series of locations, including a doctor’s office or clinic, an emergency department, or their own home. It was not possible to ascertain what specific services were received at each location.
Unmet needs:
Respondents were asked whether their child needed a series of services but were unable to get them because it couldn’t be afforded, including: a) medical care, b) seeing a specialist, c) follow-up care, d) prescription medicines, and e) mental health care or counseling.
Statistical analysis
Demographic differences between regions among children with ASD were compared using Rao-Scott χ2 tests that accounted for the survey design (presented as F-values) --- significant overall F-tests were followed up with bivariate comparisons between regions and the demographic characteristic. Multivariate logistic regressions examined differences in ASD prevalence between geographic regions adjusted for child (age, sex, race and ethnicity, insurance status) and family (federal poverty level, family structure, highest adult education level, MSA status) characteristics and survey year. Additional multivariate logistic regressions examined service utilization differences and unmet needs among children with ASD by geographic regions both unadjusted and adjusted for child and family characteristics. As part of a secondary analysis, a series of interaction terms between region and MSA status were included in adjusted models to determine if geographic density had a differential effect in different parts of the country.
All analyses were conducted using Stata 14.025 and made use of the survey sampling weights and the appropriate procedures to account for the complex survey design of the NHIS, as well as the imputed income data provided by NCHS. Weights accounted for nonresponse to the questionnaire and included a raking adjustment.
Results
Prevalence
Between 2014 to 2016, the prevalence of ASD among children 3 to 17 years of age in the United States was 2.5% (95% CI: 2.2–2.7). The prevalence of ASD was 3.0% (95% CI: 2.4–3.8) in the Northeast, 2.4% (95% CI: 2.0–3.0) in the Midwest, 2.4% (95% CI: 1.9–2.9) in the South, and 2.3% (95% CI: 1.9–2.7) in the West. A significant difference was found between the Northeast and West (OR = 0.74, 95% CI: 0.55–0.99; p<0.05). However, after accounting for child and family characteristics, this difference was no longer significant (AOR = 0.88, 95% CI: 0.64–1.20; p=0.42). A series of regression sensitivity analyses were used to examine the impact of each covariate in this adjusted model, revealing that the inclusion of children’s race and ethnicity (non-Hispanic white vs. all other races) had the greatest impact in shifting the association from significant to non-significant.
Demographics of Children with Autism Spectrum Disorder
Basic demographics by geographic region among children diagnosed with autism spectrum disorder appear in Table 1. Children with ASD in the Northeast and Midwest were more likely to be non-Hispanic white than children with ASD from other regions; children with ASD from the West were more likely to be Hispanic than children with ASD from other regions. Children with ASD in the Midwest were most likely to be living in a single parent household than children with ASD in other regions, but were less likely to be living in a household where the highest educated member had less than a high school education when compared to children with ASD from the South and West. Children with ASD were distributed similarly by MSA status across the four geographic regions, with approximately 7 out of 8 children with ASD living in an MSA.
Table 1.
Demographic characteristics of children with autism spectrum disorder, by geographic region
| Total (n=711) % (SE) |
Northeast (n=145) % (SE) |
Midwest (n=148) % (SE) |
South (n=234) % (SE) |
West (n=184) % (SE) |
F-value | |
|---|---|---|---|---|---|---|
| Child characteristics | ||||||
| Age | 0.63 | |||||
| 3–7 years | 30.1 (2.4) | 32.7 (5.3) | 24.3 (4.0) | 30.6 (4.6) | 32.7 (4.9) | |
| 8–12 years | 38.6 (2.5) | 40.6 (6.0) | 37.7 (5.5) | 36.9 (4.0) | 40.5 (5.1) | |
| 13–17 years | 31.3 (2.5) | 26.7 (5.5) | 38.0 (5.5) | 32.5 (4.5) | 26.8 (4.6) | |
| Sex | 0.02 | |||||
| Female | 75.3 (2.3) | 24.3 (5.2) | 24.3 (4.3) | 24.6 (3.8) | 25.9 (4.9) | |
| Male | 24.7 (2.3) | 75.7 (5.2) | 75.7 (4.3) | 75.4 (3.8) | 74.1 (4.9) | |
| Race and ethnicity | 6.18*** | |||||
| Non-Hispanic white | 60.7 (2.4) | 69.8 (5.0) | 75.5 (4.1) | 54.3ab (3.8) | 48.2ab (5.4) | |
| Non-Hispanic black | 16.8 (2.1) | 13.6 (4.1) | 13.5 (3.4) | 25.6b (4.3) | 8.2c (2.8) | |
| Non-Hispanic other and multiple race | 4.6 (1.0) | 0.6 (0.4) | 4.0a (1.8) | 3.0 (1.6) | 11.3abc (2.9) | |
| Hispanic | 18.0 (1.9) | 16.0 (3.6) | 7.0a (2.1) | 17.1b (3.2) | 32.3abc (5.2) | |
| Insurance type | 3.15** | |||||
| Any private | 50.8 (2.6) | 62.4 (5.4) | 54.6 (4.8) | 42.8a (4.8) | 49.2 (5.8) | |
| Public only1 | 46.4 (2.6) | 36.1 (5.3) | 44.8 (4.8) | 51.4a (4.5) | 49.3 (5.9) | |
| Uninsured | 2.8 (0.8) | 1.5 (0.9) | 0.6 (0.4) | 5.7b (2.1) | 1.6c (0.7) | |
| Family characteristics | ||||||
| Federal poverty level | 1.38 | |||||
| <100% | 21.4 (2.1) | 15.3 (3.4) | 24.8 (4.5) | 23.2 (4.0) | 20.7 (4.3) | |
| 100–199% | 28.8 (2.2) | 26.1 (5.6) | 26.0 (4.4) | 31.2 (3.4) | 30.0 (5.1) | |
| 200–399% | 25.9 (2.1) | 23.2 (4.3) | 30.7 (3.9) | 21.8 (3.7) | 30.4 (5.3) | |
| ≥400% | 23.8 (2.1) | 35.4 (5.5) | 18.6 (3.8) | 23.8 (3.2) | 18.8 (4.1) | |
| Family type | 2.55* | |||||
| Two parents | 63.7 (2.4) | 67.5 (4.8) | 56.5 (4.4) | 62.7 (4.5) | 69.2 (5.3) | |
| Single parent | 31.0 (2.3) | 27.4 (4.5) | 42.6a (4.3) | 28.6b (4.1) | 26.5b (4.6) | |
| Other | 5.3 (1.2) | 5.1 (2.9) | 0.8a (0.5) | 8.7b (2.5) | 4.3b (1.8) | |
| Highest educated member | 2.41* | |||||
| Less than high school | 8.9 (1.6) | 4.8 (1.9) | 3.3 (1.3) | 14.1ab (3.6) | 9.8b (3.2) | |
| High school diploma or GED | 19.0 (1.9) | 19.9 (3.9) | 24.7 (4.7) | 18.1 (3.5) | 13.9 (3.5) | |
| More than high school | 72.1 (2.1) | 75.3 (4.4) | 71.9 (4.7) | 67.8 (3.7) | 76.3 (4.2) | |
| MSA Status2 | 2.07 | |||||
| In MSA | 87.8 (1.7) | 92.8 (2.7) | 81.3 (5.0) | 87.2 (2.9) | 91.2 (2.5) | |
| Not in an MSA | 12.2 (1.7) | 7.3 (2.7) | 18.7 (5.0) | 12.8 (2.9) | 8.8 (2.5) |
NOTES: GED is General Education Diploma; SE is standard error; MSA is metropolitan statistical area
Significantly different from children in Northeast (p<0.05) using bivariate logistic regression.
Significantly different from children in Midwest (p<0.05) using bivariate logistic regression.
Significantly different from children in South (p<0.05) using bivariate logistic regression.
p<0.05
p<0.01
p<0.001
Public insurance includes Medicaid, Children’s Health Insurance Program (CHIP), and other state sponsored coverage.
A MSA consists of a county or group of counties that includes an urbanized area with a population of at least 50 thousand.
Service Utilization among Children with Autism Spectrum Disorder
More than 9 out of 10 children with ASD had received care at either a doctor’s office or clinic, emergency department, or their own home in the past 12 months, and approximately 4 in 5 children with ASD had multiple visits at one of these locations (Table 2). Additionally, the vast majority of children with ASD had seen at least one of the four provider types within the past year (95.2%; SE: 1.2).
Table 2.
Service utilization of children with autism spectrum disorder, by geographic region
| Total (n=711) % (SE) |
Northeast (n=145) % (SE) |
Midwest (n=148) % (SE) |
South (n=234) % (SE) |
West (n=184) % (SE) |
F-value | |
|---|---|---|---|---|---|---|
| Locations received care in past 12 months | ||||||
| Any office visits | 93.1 (1.6) | 97.2 (1.7) | 91.4 (4.3) | 90.7 (3.1) | 95.3 (2.0) | 1.17 |
| Multiple office visits | 80.9 (2.0) | 86.7 (3.6) | 78.5 (4.5) | 77.3 (3.7) | 84.0 (3.4) | 1.36 |
| Any emergency room visit | 22.1 (2.2) | 29.7 (5.3) | 22.0 (4.3) | 21.3 (3.8) | 16.8 (4.1) | 1.29 |
| Multiple emergency room visits | 8.5 (1.3) | 10.4 (3.0) | 11.5 (3.2) | 7.3 (2.0) | 5.9 (2.3) | 0.95 |
| Any home visit | 6.8 (1.4) | 11.6 (4.2) | 9.7 (3.4) | 2.0ab (0.8) | 7.5c (3.0) | 3.09* |
| Multiple home visits | 6.1 (1.4) | 9.9 (4.1) | 8.3 (3.4) | 1.8 (0.8) | 7.5 (3.0) | 2.38 |
| Any of these locations | 94.0 (1.6) | 97.8 (1.5) | 91.9 (4.3) | 92.2 (3.1) | 95.4 (2.0) | 0.95 |
| Multiple visits at any of these locations | 81.5 (2.0) | 88.0 (3.5) | 78.5 (4.5) | 78.2 (3.7) | 84.2 (3.4) | 1.45 |
| Providers seen in past 12 months | ||||||
| Generalist | 88.3 (1.7) | 94.3 (2.3) | 83.9 (3.9) | 88.1 (3.2) | 87.6 (2.8) | 1.56 |
| Specialist | 35.0 (2.5) | 42.2 (5.6) | 37.6 (4.8) | 33.5 (4.4) | 28.5 (4.8) | 1.25 |
| Mental health professional | 50.4 (2.5) | 56.1 (5.7) | 54.7 (4.4) | 45.7 (4.5) | 48.6 (5.1) | 1.07 |
| Therapist | 50.4 (2.6) | 60.6 (5.3) | 51.6 (5.2) | 40.6ab (4.9) | 41.0ab (4.7) | 3.43* |
| Any of these providers | 95.2 (1.2) | 99.3 (0.6) | 93.3 (2.3) | 93.3 (2.8) | 96.6 (1.3) | 2.33 |
NOTES: SE is standard error
Significantly different from children in Northeast after adjustment for child and family characteristics (p<0.05)
Significantly different from children in Midwest after adjustment for child and family characteristics (p<0.05)
Significantly different from children in South after adjustment for child and family characteristics (p<0.05)
p<0.05
In unadjusted models, children with ASD in the South were least likely to have received care at home over the past year, while children with ASD in the Northeast were more likely to have seen a therapist compared to children with ASD in the South and West. These differences remained significant in adjusted models accounting for child and family characteristics. There were no differences across regions in the proportion of children with ASD who received care multiple times in a given location.
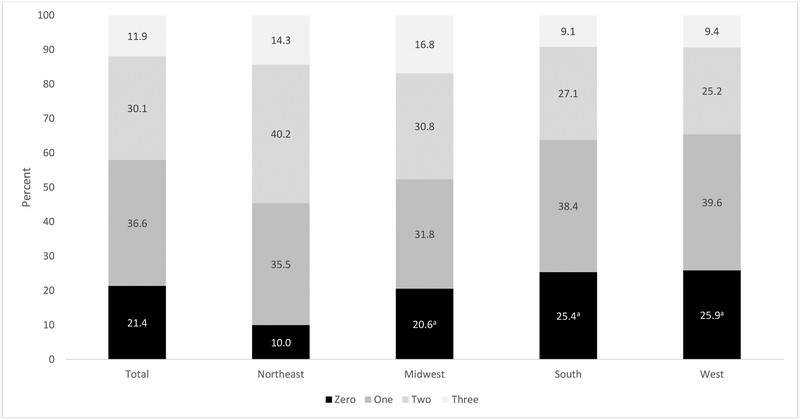
Specialty Care
Approximately 4 in 5 children with ASD saw either a specialist, mental health professional, or therapist in the past 12 months (78.6%; SE: 2.0) (See Figure 1). In unadjusted models, children with ASD in the Northeast were the most likely to have seen at least one type of specialist. This difference remained significant after accounting for child and family characteristics. While about half of the children with ASD in the Northeast (54.5%; SE: 5.5) and Midwest (47.6%; SE: 5.5) had seen multiple types of specialists, only approximately one in three children with ASD from the South (36.2%; SE: 4.2) and West (34.6%; SE: 5.1) had seen multiple types of specialists.
Figure 1. Number of type of specialists seen in the past year among children with autism spectrum disorder, by geographic region.
a Significantly different from children in Northeast after adjustment for child and family characteristics (p<0.05)
Unmet needs
Overall, approximately 1 in 8 children with ASD (12.1%; SE: 2.0) experienced at least one unmet need in either medical care, seeing a specialist, follow-up care, prescription medication, or mental health care or counseling due to cost --- 9.3% (SE: 3.6) of children with ASD in the Northeast, 8.5% (SE: 2.7) of children with ASD in the Midwest, 15.2% (SE: 4.0) of children with ASD in the South, and 13.4% (SE: 4.0) of children with ASD in the West (see Table 3). Overall there was not a significant difference found by region either adjusted or unadjusted, although children in the South with ASD were significantly more likely to have an unmet medical care need than children with ASD in the West after adjustment for child and family characteristics.
Table 3.
Unmet medical needs due to cost in past year among children with autism spectrum disorder, by geographic region
| Total % (SE) |
Northeast % (SE) |
Midwest % (SE) |
South % (SE) |
West % (SE) |
F-value | |
|---|---|---|---|---|---|---|
| Medical care | 1.8 (0.7) | 0.8 (0.6) | 1.1 (1.1) | 3.8 (1.8) | 0.2c (0.2) | 3.07* |
| Seeing a specialist | 6.3 (1.4) | 2.9 (2.3) | 6.7 (2.5) | 8.9 (2.8) | 4.9 (2.6) | 0.92 |
| Follow-up care | 4.2 (1.2) | 2.9 (2.3) | 3.9 (1.8) | 7.2 (2.8) | 0.7 (0.6) | 2.19 |
| Prescription medicine | 4.4 (1.0) | 4.2 (2.8) | 4.5 (2.0) | 4.5 (1.6) | 4.1 (2.1) | 0.01 |
| Mental health care or counseling | 4.2 (1.0) | 2.3 (1.4) | 3.9 (2.0) | 3.9 (1.5) | 6.6 (2.6) | 0.80 |
| Any unmet need | 12.1 (2.0) | 9.3 (3.6) | 8.5 (2.7) | 15.2 (4.0) | 13.4 (4.0) | 0.85 |
NOTES: SE is standard error
Significantly different from children in South after adjustment for child and family characteristics (p<0.05)
p<0.05
Discussion
Prevalence
Based on data from the 2014–2016 NHIS, approximately 1 in 40 children aged 3–17 years (2.5%) had ever been diagnosed with ASD. Children in the Northeast had the highest prevalence compared to other geographic regions in the country. This is consistent with findings from the recent ADDM Network, where the New Jersey surveillance site reported the highest ASD prevalence2 and from the Nurses’ Health Study II, where children in the “New England” area were more likely to be diagnosed with ASD.18 Though the Nurses’ Health Study II found that race and ethnicity could not fully explain geographic differences, it is important to note that neither of these studies recruited a representative sample of children, particularly as it relates to race and ethnicity.
The present study, however, did find that regional differences could be explained by the inclusion of child and family characteristics. A sensitivity analysis revealed that the child’s race and ethnicity had the greatest impact in attenuating the magnitude of the association and also resulted in a shift from significant to non-significant. More specifically, since non-Hispanic white children were more likely to be diagnosed with ASD and children in the Northeast were more likely to be non-Hispanic white relative to other regions,26 controlling for regional differences in the prevalence of non-Hispanic white children was sufficient to reduce the regional differences from statistically significant to non-significant.
It is also worth noting that MSA status was not significantly associated with prevalence, nor was there a significant difference found by MSA distribution across regions among children with ASD, which are intriguing findings given previous research has found such a relationship.19–20 In addition, the secondary analysis, designed to explore whether geographic density may have a differential effect in four geographic regions, did not produce any significant interactions between MSA status and region, after adjustment for child and family characteristics. A previous US study reported that urban areas were more likely to be geographically closer to autism-related service providers and diagnosticians, and that geographic proximity to these providers was associated with an earlier age of ASD diagnosis.10 These studies differ from the present study in several important ways: they covered time periods at least 10 years older than NHIS data used in this study, used different measures of “urbanicity”, covered portions of a single US state or Denmark, and the data were obtained—at least in part—from existing registries or from health care providers.
Service Utilization and Specialty Care
The vast majority of children with ASD had seen a health care provider in the past year (95.2%), with approximately half of all children receiving care from a mental health professional (50.4%) or a therapist (50.4%). Yet, children with ASD in the Northeast were the most likely to have received any specialty care (specialist, mental health professional, or therapist) in the past year. In the South and West, approximately 1 in 4 children with ASD hadn’t received any specialty care, and less than half had seen multiple specialists, significantly lower proportions than children with ASD in the Northeast and Midwest. Children with ASD in the South and West were also less likely to have seen a therapist than children with ASD in the Northeast and Midwest.
Children with ASD in the South were the least likely to have received care at home compared to children with ASD throughout the country. Overall however, children with ASD were not more likely to have received care multiple times at any one location over the past 12 months, nor were any of the interaction terms significant as part of the secondary analysis. Previous research utilizing Medicaid claim data found that although the proportion of children with ASD receiving services in urban versus rural settings did not differ significantly, the number of services used were higher in urban areas.27
Service availability could affect the likelihood of a child receiving an ASD diagnosis. For example, Hoffman and colleagues18 found differing odds of ASD diagnosis depending on where the child was located, with children living in New England having the greatest odds of being diagnosed with ASD, while children living in central and southern US had lower odds of having received a diagnosis. The authors hypothesized that available diagnostic resources and services (such as those provided by the school under a child’s Individualized Education Program) may explain these differences, assuming increased use of specialists reflects higher availability of specialists. This hypothesis that service availability influences ASD diagnosis and ASD prevalence (see also Hill and colleagues28) is consistent with the present study’s unadjusted prevalence estimates and service utilization patterns. The exact mechanisms that may lead to these regional differences are not entirely clear. For example, Mazumdar and colleagues12 analyzed smaller “clusters” of ASD in California neighborhoods and concluded that neither “institutional diagnostic dynamics” nor families moving to areas with greater services explained differences seen in ASD prevalence.
Unmet Needs
Although children with ASD in the Northeast showed the highest ASD prevalence, greatest service utilization, and most specialty care encounters, children with ASD were not less likely to have unmet needs regardless of geographic region for several measures. In contrast, a previous analysis of data on children with special health care needs (CSHCN) (defined broadly) from the 2009–2010 NS-CSHCN did identify regional differences in unmet need; in general it reported lower unmet need in the Northeast or Midwest, compared to the West and the South.29 Similarly, data from the 2005–2006 NS-CSHCN showed regional differences in unmet need for health services among children with ASD, with more unmet need in the West than the Northeast.8,30
It is unknown if differences between the current study and these previous findings are a reflection of changes in service availability for children with ASD over the past decade or perhaps differences between children with ASD with or without special health care needs. Given that children with ASD require additional services and experience greater levels of impairment than children with other special health care needs,31 findings for CSHCN may not be generalizable to children with ASD.
However, it is worth noting that the secondary analysis did not find differential effects of MSA status and region, nor MSA status alone, allowing for the possibility that some of the barriers previously identified to accessing care in rural settings for children with ASD32,33 may have resolved. Additional research into the impact of efforts to train practitioners to work in rural environments, such as those recommended by the American Medical Association,34 may provide insight into changes seen.
Limitations
The NHIS has notable strengths in its large sample size and high response rate. However, caution regarding estimates is warranted because of several survey-related limitations. The reliance on parent reports could result in misreporting of child’s ASD diagnosis; such reports may also be subject to recall biases. Additionally, parents’ reports were not validated through clinical evaluation or educational records, and parents were only asked to reflect on lifetime diagnosis of ASD rather than current diagnoses; therefore children who have lost their original diagnosis would be included in the sample of children with ASD and the reported prevalence. Previous research has found that most ASD diagnoses persist, but there are reasons children who received a diagnosis in the past may no longer meet the criteria for a diagnosis, including, but not limited to, maturation, misdiagnosis, and effective treatment.35 Some children may also be less likely to meet diagnostic criteria for ASD after the introduction of revised diagnostic criteria with the DSM-5 in 2013.36 Additionally, although data was pooled over three years of NHIS interviews, there is still the potential for the small sample size of children with ASD to impact the interpretability of some findings. Namely, there may not be sufficient power to rule out a true difference between regions when the prevalence of an outcome for children with ASD was low. Finally, as the NHIS is a survey of the noninstitutionalized population, children living in places other than the household (e.g., long-term care facilities) are not included in the estimates.
Conclusion
Although differences seen in the prevalence of ASD could be explained by child and family characteristics, such was not the case for differences seen in the receipt of specialized services by region. Additional research is warranted to further explore how child and family characteristics may lead to a disproportionate receipt of services or the ability to receive an ASD diagnosis.
What’s New?
The current study expands the literature exploring geographic regions among children with ASD using a nationally representative sample. While children with ASD in the Northeast were found to have a greater utilization of specialized services, they were not less likely to have unmet needs when compared to children with ASD from other geographic regions.
Footnotes
Conflicts of Interest and Source of Funding: The authors have no financial relationships relevant to this article to disclose. The authors have no conflicts of interest to disclose.
Publisher's Disclaimer: Disclaimer: The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
References
- 1.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Arlington, VA: American Psychiatric Publishing; 2013. [Google Scholar]
- 2.Baio J, Wiggins L, Christensen DL, et al. Prevalence of autism spectrum disorder among children aged 8 years—Autism and developmental disabilities monitoring network, 11 sites, United States, 2014. MMWR Morb Mortal Wkly Rep. 2018;67:1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Christensen DL, Baio J, Braun KVN, et al. Prevalence and characteristics of autism spectrum disorder among children aged 8 years—Autism and Developmental Disabilities Monitoring Network, 11 sites, United States, 2012. MMWR Morb Mortal Wkly Rep. 2016;65(3):1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Lyall K, Croen L, Daniels J, et al. The changing epidemiology of autism spectrum disorders. Annu Rev Public Health. 2017;38:81–102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zablotsky B, Black LI, Maenner MJ, et al. Estimated prevalence of autism and other developmental disabilities following questionnaire changes in the 2014 National Health Interview Survey. National Health Statistics Reports. 2015;87:1–20. [PubMed] [Google Scholar]
- 6.Mandell DS, Palmer R. Differences among states in the identification of autistic spectrum disorders. Arch Pediatr Adolesc Med. 2005;159(3):266–269. [DOI] [PubMed] [Google Scholar]
- 7.Benevides TW, Carretta HJ, Lane SJ. Unmet need for therapy among children with autism spectrum disorder: results from the 2005–2006 and 2009–2010 national survey of children with special health care needs. Matern Child Health J. 2016;20(4):878–888. [DOI] [PubMed] [Google Scholar]
- 8.Chiri G, Warfield ME. Unmet need and problems accessing core health care services for children with autism spectrum disorder. Matern Child Health J. 2012;16(5):1081–1091. [DOI] [PubMed] [Google Scholar]
- 9.Hoffman K, Kalkbrenner AE, Vieira VM, et al. The spatial distribution of known predictors of autism spectrum disorders impacts geographic variability in prevalence in central North Carolina. Environ Health. 2012;11(1):80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kalkbrenner AE, Daniels JL, Emch M, et al. Geographic access to health services and diagnosis with an autism spectrum disorder. Ann Epidemiol. 2011;21(4):304–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Liptak GS, Benzoni LB, Mruzek DW, et al. Disparities in diagnosis and access to health services for children with autism: data from the National Survey of Children’s Health. J Dev Behav Pediatr. 2008;29(3):152–160. [DOI] [PubMed] [Google Scholar]
- 12.Mazumdar S, Winter A, Liu KY, et al. Spatial clusters of autism births and diagnoses point to contextual drivers of increased prevalence. Soc Sci Med. 2013;95:87–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Polyak A, Kubina RM, Girirajan S. Comorbidity of intellectual disability confounds ascertainment of autism: implications for genetic diagnosis. Am J Med Genet B Neuropsychiatr Genet. 2015;168(7):600–608. [DOI] [PubMed] [Google Scholar]
- 14.Rzhetsky A, Bagley SC, Wang K, et al. Environmental and state-level regulatory factors affect the incidence of autism and intellectual disability. PLoS Comput Biol. 2014:10(3):e1003518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Durkin MS, Maenner MJ, Baio J, et al. Autism spectrum disorder among US children (2002–2010): socioeconomic, racial, and ethnic disparities. Am J Public Health. 2017;107(11):1818–1826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Schopler E Limits of methodological differences in family studies In Autism (pp. 297–301). Boston, MA: Springer, 1978. [Google Scholar]
- 17.Thomas P, Zahorodny W, Peng B, et al. The association of autism diagnosis with socioeconomic status. Autism. 2012;16(2):201–213. [DOI] [PubMed] [Google Scholar]
- 18.Hoffman K, Weisskopf MG, Roberts AL, et al. Geographic patterns of autism spectrum disorder among children of Nurses’ Health Study II women. Am J Epidemiol. 2017;186(7):834–842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lauritsen MB, Astrup A, Pedersen CB, et al. Urbanicity and autism spectrum disorders. J Autism Dev Disord. 2014;44(2):394–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Murphy MA, Ruble LA. A comparative study of rurality and urbanicity on access to and satisfaction with services for children with autism spectrum disorders. Rural Special Education Quarterly. 2012:31(3):3–11. [Google Scholar]
- 21.Lokhandwala T, Khanna R, West-Strum D. Hospitalization burden among individuals with autism. J Autism Dev Disord.2012;42(1):95–104. [DOI] [PubMed] [Google Scholar]
- 22.Nathenson RA, Zablotsky B. The transition to the adult health care system among youths with autism spectrum disorder. Psychiatr Serv. 2017;68:735–738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Johnson JA 3rd, Johnson AM. Urban-rural differences in childhood and adolescent obesity in the United States: a systematic review and meta-analysis. Childhood Obes. 2015;11(3):233–241. [DOI] [PubMed] [Google Scholar]
- 24.Bitsko RH, Holbrook JR, Robinson LR et al. Health care, family, and community factors associated with mental, behavioral, and developmental disorders in early childhood—United States, 2011–2012. MMWR Morb Mortal Wkly Rep. 2016;65(9):221–226. [DOI] [PubMed] [Google Scholar]
- 25.StataCorp. 2015. Stata Statistical Software: Release 14. College Station, TX: StataCorp LP. [Google Scholar]
- 26.United States Census Bureau. 2010 Census Demographic Profile Summary file: 2010 Census of Population and Housing. https://www2.census.gov/programs-surveys/decennial/2010/technical-documentation/complete-tech-docs/summary-file/dpsf.pdf. 2011. Accessed 7 December 2016.
- 27.Paul MH. Rural-urban disparities in the diagnosis and treatment of children with autism spectrum disorders (ASD). Doctoral dissertation; 2017;The Ohio State University [Google Scholar]
- 28.Hill AP, Zuckerman K, Fombonne E. Epidemiology of autism spectrum disorders In Translational Approaches to Autism Spectrum Disorder (pp. 13–38). Switzerland: Springer International Publishing, 2015. [Google Scholar]
- 29.Fulda KG, Johnson KL, Hahn K, et al. Do unmet needs differ geographically for children with special health care needs?. Matern Child Health J. 2013;17(3):505–511. [DOI] [PubMed] [Google Scholar]
- 30.Kogan MD, Strickland BB, Blumberg SJ, et al. A national profile of the health care experiences and family impact of autism spectrum disorder among children in the United States, 2005–2006. Pediatrics. 2008;122(6):e1149–e1158. [DOI] [PubMed] [Google Scholar]
- 31.Krauss MW, Gulley S, Sciegaj M, et al. Access to specialty medical care for children with mental retardation, autism, and other special health care needs. Ment Retard. 2003;41(5):329–339. [DOI] [PubMed] [Google Scholar]
- 32.Thomas KC. Ellis AR, McLaurin C, et al. Access to care for autism-related services. J Autism Dev Disord. 2007;37:1902–1912. [DOI] [PubMed] [Google Scholar]
- 33.Hutton AM, Caron SL. Experiences of families with children with autism in rural New England. Focus on Autism and Other Developmental Disabilities. 2005;20(3):180–189. [Google Scholar]
- 34.American Medical Association. Press Release: Future physicians should seek training to enhance access to rural care. https://www.ama-assn.org/press-center/press-releases/future-physicians-should-seek-training-enhance-access-rural-care. 2018. Accessed 31 December 2018.
- 35.Blumberg SJ, Zablotsky B, Avila RM, et al. Diagnosis lost: Differences between children who had and who currently have an autism spectrum disorder diagnosis. Autism. 2016;20(7):783–795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Maenner MJ, Rice CE, Arneson CL, et al. Potential impact of DSM-5 criteria on autism spectrum disorder prevalence estimates. JAMA Psychiatry. 2014;71(3):292–300. [DOI] [PMC free article] [PubMed] [Google Scholar]