Abstract
AIM:
The aims of this investigation were: 1) to study the Functional outcome of performing distraction osteogenesis in cases of infected non-union of tibia treated with Ilizarov and Limb Reconstruction System, and 2) to study the Radiological outcome of performing distraction osteogenesis in cases of infected non-union of tibia treated with Ilizarov and Limb Reconstruction System.
METHODS:
The study was done with 27 patients of infected gap nonunions of the tibia at Sir JJ Hospitals, Mumbai from 2013-2016. After implant removal, if required radical resection of necrotic tissue and fractures were stabilised with Ilizarov or mono-lateral fixator depending on non-union site. Corticotomy was either done proximally or distally. Patients were followed up at monthly intervals for a minimum of 6 months.
RESULTS:
The ASAMI-Bone healing score was Excellent or Good in 86% patients, and Functional score was Excellent or Good in 89% of patients. The commonest problems were of pin tract infection, wire loosening and angulation of the transported segment.
CONCLUSION:
Elderly age, persistent infection, sensory loss in the foot, the stiffness of the knee, and above all the patient’s reluctance to go any further given the protracted treatment besides, systemic disorders such as diabetes are all pointers for considering amputation as an alternative.
Keywords: Distraction Osteogenesis, Llizarov, LRS, Non-Union
Introduction
Fractures of the tibia are one of the commonest injuries especially with the rise in vehicular accidents. The large subcutaneous antero-medial surface predisposes to open fractures and often leads to a bone gap devoid of soft tissue cover. Soft tissue damage and periosteal stripping are common in high velocity and open injuries, and this can compromise the vascularity of the tissues around the fracture. Infection of the wound, deformity, limb shortening and non-union are all known complications of fracture of the tibia. They often lead to a bone gap which may further increase on debridement of the infected or necrotic bone.
In the musculoskeletal system, the biomechanical environment plays a key role in repairing, maintaining, and remodelling of bone to meet its functional demands. Fracture non-union is a chronic condition associated with pain, functional and psychosocial disability. Stability, vascularisation and good rehabilitation are required for successful union of tibia fractures. Thus the management of tibia non-union revolves around attempts at satisfactorily restoring the above-mentioned factors to bring about an adequate union for physical and psychological rehabilitation of the patient. Different methods of treatment have been recommended for the management of infected gap non-union. One of these methods is the “Conventional” or classic method. This method focuses on eliminating the existing infection and drainage from the bone thereby facilitating the healing process. This is achieved by sequential debridement of all the infected and nonviable tissues. This line of management mandates the use of prolonged antibiotic therapy, bypass bone grafting and long-term orthotic support. The process of healing in these cases takes place by secondary intention. The protracted time is taken in this procedure usually results in stiffness of adjacent joints. The second method is the “active” method in which attempts are made at obtaining early bony union and the period of convalescence is reduced to a minimum owing to which the motion in adjacent joints is preserved. In this method, the restoration of bony continuity gains priority over the treatment of underlying infection.
The requirements common to all successful techniques in the management of non-union are biomechanical stability, and biological vitality of bone obtained after all devitalized bone and soft tissue is removed, and infection is controlled aggressively. The distraction osteogenesis principle with bone transport is the mainstay of treatment in cases of infected non-union of the tibia with a bone gap.
The choice of the external fixator is now generally determined by the experience and preference of the surgeon, the complexity of the problem, and the number of sites that need treatment. As a general rule, monolateral fixators may not be as well suited as ring fixators for the mechanical correction of deformities with angulations or rotation or for those that need more than two sites of treatment. Each type of external fixator exhibits individual mechanical characteristics that may affect osteogenesis and healing. The stiffness and stability of a fixator system are dependent on many variables, including the diameter of the wires, the number of wires used, the tension on each wire, the diameter of the rings, the number of rings used, and the spacing between the rings. As the use of half-pins results in half the number of sites of soft-tissue transfixation, they can decrease the number of pain-related and soft-tissue complications and can potentially improve the comfort of the patient and the tolerance to treatment [1], [2], [3].
The conventional methods of treatment of infected gap non-union of tibia often require prolonged time to complete and are associated with many complications like the stiffness of joints, persistent deformity and limb length discrepancy. The distraction osteogenesis method of Ilizarov has the potential to correct the infection, deformity, limb length discrepancy, bone and soft tissue loss simultaneously. So we plan to evaluate the functional and radiologic outcome of distraction osteogenesis in patients with infected gap non-union of the tibia.
The aims of this investigation were: 1) to study the Functional outcome of performing distraction osteogenesis in cases of infected non-union of tibia treated with Ilizarov and Limb Reconstruction System, and 2) to study the Radiological outcome of performing distraction osteogenesis in cases of infected non-union of tibia treated with Ilizarov and Limb Reconstruction System.
Material and Methods
This prospective study was conducted at the Department of Orthopaedic Surgery, Grant Medical College and Sir J.J. Group of Hospitals, Mumbai from 2014-2016. A total number of twenty-seven patients of either sex of non-union tibia with an infected bone gap at fracture site were included in the study and treated by bone transport and distraction osteogenesis carried out by Ilizarov’s ring fixator or mono-lateral fixator.
Inclusion criteria: Patients with infected gap non-union of the tibia with a minimum gap of 1 cm after debridement.
Exclusion criteria: Patients with pathological fractures and fracture associated with bone disorders, the presence of any debilitating systemic disease, hormonal disorders, mental disorders and those lost to follow up were excluded from the study.
Written Informed consent of all the patients was taken. A detailed history was taken regarding the mode of injury and treatment taken before admission. A detailed examination was done to assess the level of non-union, bone gap present, shortening of extremity, neurovascular deficit, deformity, the extent of infection, the condition of soft tissue in the leg especially the anteromedial aspect of tibia and function or stiffness of the knee and ankle joints. The non-union was classified according to the AO Classification of infected non-union [4], [5]. Standard anteroposterior and lateral skiagrams of patients were taken. After all pre-op investigations and obtaining pre-anaesthetic fitness, patients with obvious infection (AO Stages-Infected, draining and Active, non-draining) were debrided and stabilised with external fixator under spinal anaesthesia. Any implant, if present was removed during debridement. All non-viable bone was radically excised from the fracture site until punctate bleeding spots from the cortex were seen (Paprika Sign). During debridement, pus from the wound or sinus was sent for culture and sensitivity. The tibia defect was measured and noted after debridement, and the gap non-union was classified based on Paley’s classification [4], [5].
In some cases, the local antibiotic depot was employed after debridement for 3-6 weeks, in order to achieve control of infection at the non-union site. STIMULAN® was also used along with antibiotics as a strategy for infection management. The advantage of STIMULAN® is that it is biocompatible, sets at body temperature, non-pyrogenic and fully resorbable owing to which it does not act as a nidus for bacteria and also does not require removal. The commonly used antibiotics were vancomycin (for gram-positive organisms especially Methicillin-resistant Staphylococcus aureus), gentamycin and tobramycin (gram-negative organisms). After the deep culture sensitivity report was available, the patients were shifted to sensitive intravenous antibiotics if required.
When loss of soft tissue cover was to an extent wherein the wound was less likely to heal by secondary intention, plastic surgery intervention was called for, and a pedicled myocutaneous gastrocnemius flap or other local flap was done. After the restoration of the soft tissue cover, any antibiotic spacers (if present) were removed. The patients who were not previously stabilised with a bone transport mechanism were operated upon, and either Ilizarov or LRS was applied in such cases. The Ilizarov ring fixator was applied in 12 patients while the monolateral fixator was used in 15 patients.
Application of Ilizarov frame/LRS
Preoperative planning
The operative plan was formulated considering the fracture/non-union configuration and the preference of the patient. A few patients preferred the monolateral fixator due to its light frame. The ring fixator was preferred when there was deformity or angulation, or the proximal or distal tibia segments were short. Acute docking was done preferably when post debridement bone gap was less than 4 cm. The patients were counselled about the long duration of the treatment and the consequences of non-compliance with the treatment protocol. Informed consent was taken for surgery, and the complications were explained in the language they understood. A day before the surgery, appropriately sized rings were chosen, and the apparatus was pre-constructed. It was kept in mind that the internal diameter of the rings was at least 4 cm larger than the maximum diameter of the limb segment to be treated. It was made sure that all of the rings are of the same size. After this, the frame was sterilised for use during the surgical procedure. In the case of the monolateral fixator, the length of rail, type of clamp and configuration of the pin in each clamp were decided.
Surgical procedure
The patient was placed in supine position with the affected lower extremity supported by a bump under the greater trochanter to prevent external rotation of the limb.
With mono-lateral fixator three clamps were applied, one to the advancing or docked segment and one each to the proximal and distal tibia. The first tapered threaded pin was inserted over the anteromedial aspect of the tibia at the level of head of fibula parallel to the tibia joint line just piercing the second cortex. Care was taken not to withdraw the tapered threaded pin as it led to a loosening of the pin. The second pin was inserted over the anteromedial surface 2 cms above and parallel to the ankle joint. Once these two pins were secured, the rail was put in place along with the template. Rest of the pins were inserted using the template as the guide.
In most cases, the pins were placed in 1, 3, 5 configuration. Following this, the dummy clamps were removed and were replaced with central/end clamps. All the clamps were tightened to provide rigid stabilisation at the fracture site.
In case of ring fixator, 4 or 5 rings and four rods were applied along with 10-12 wires. One ring to the advancing or docked segment and 2 rings on either side. If one of the segments at the extreme was short enough only one ring was applied. The optimum diameter of the wire is 1.5 mm for children and thin bones, and 1.8 mm for adults and large bones [6], [7]. The first wire was inserted from lateral to medial just anterior to the head of fibula and parallel to the tibia joint line. Once the wire was inserted through the second cortex, it was not drilled but was gently tapped through the soft tissue to avoid wrapping of the neurovascular structures. The second wire was placed parallel to the first, 2 cms proximal to the ankle joint. These wires were then fixed to the ring frame. First, the proximal block of rings was centred on the leg. The distal block was positioned such that the anterior distance from the leg to the rings was the same distance as that of the proximal blocks, i.e. at least 2 cms on either side. These wires were then tensioned to 130 kgs using the dynamometer. When tensioning the olive wire, the side with the olive was tightened, and the tensioning was performed from the opposite side. Stability of the frame was created by inserting additional wires proceeding from proximal to distal avoiding the neurovascular structures. Multi-planar positioning of wires on each side of the rings or introduction of more wires, further apart with the posts further increased the stability of the assembly. If the length between the two rings of the component was more, it was preferred to minimise unsupported length by introducing drop wires.
After assembly of the rings or LRS, a small incision was made at the junction of middle and distal fibula for performing a fibular osteotomy if fibula was intact. Through a small incision preferably in the region of the metaphyseal-diaphyseal junction, a tibial osteotomy was performed with the help of an osteotome. The periosteum was elevated and preserved. The osteotomy began on the edge of the tibial crest and extended on to the medial and lateral sides of the tibia. The posterior-most fringe of bone was often broken by gentle external rotation of the distal rings/clamps.
The periosteum was repaired. After wound closure, the pin sites and the osteotomy sites were given external compression in the form of large dressing pads. It was ensured that all the connection bolts in the frame were tight and that the wires were cut and bent smoothly so as not to snag on clothing. Finally, the range of motion of the joints proximal and distal to the fixator was checked along with distal pulsations.
Post-operative care
Broad spectrum antibiotics were given three days of post operation. On the first post-op day, evaluation of pin and wire sites was done. Physical therapy was started. Graduated gait-training was attempted with the help of crutches or walker. A passive dorsiflexion device was given for the foot and ankle. In cases of acute docking or the patients having limb-length discrepancy were tackled with a shoe raise. The patient’s bed was kept flat, and a pillow was placed under the most distal ring for a circular fixator or under the ankle for a unilateral fixator to force the knee into extension. Suture removal was done around 10-15 days post-operative, and pin-track dressings were done with normal saline if not infected. If redness or swelling was present, then betadine dressings were used. An adequate dose of NSAID was used consciously for pain management.
After the latency period which in our case was 7 days post-operatively, the frame was marked with adhesive tape, and the patient was taught distraction. The tape was placed in a position which will stop the patient from moving the nuts or the distraction elements in the wrong direction. The patient was taught to distract at the rate of 0.25 mm/6 hrs. Radiographs were taken every week during the initial period of distraction, and at monthly intervals after that The rate and frequency of distraction were altered relative to clinical circumstances and radiologic progression of the fibrous inter-zone. In the case of non-progression of the bony healing patient was taken up for bone grafting during treatment. The distraction was stopped when the desired bone transport or gain in length was achieved. The fixator continued to be in place to allow consolidation of callus.
Follow-up check-list
Patients were followed up at monthly intervals for a minimum of 6 months [8].
Clinical
- Distance moved on threaded rods compared to the previous visit.
- The range of motion of adjacent joints and physiotherapy.
- Neurological examination.
- Pin sites for signs of inflammation.
- Stability of frame and components.
- Ambulation.
- Assessment of complications like muscle contracture, joint subluxation.
Radiographic
- Distraction gap increasing as required
- Progress and correction of the deformity.
- Quality of regenerate
- Consolidation
Union was defined clinically by the absence of pain and motion at the fracture site. The radiological union was considered when at least three of four tibia cortices showed bridging callus with a sharp outline of the cortical bone. Finally, before actually removing the frame, the proximal and distal ends of bone were disconnected, and the patient was asked to bear weight. If the patient was able to do this, the fixator was removed. The patient was treated in patellar tendon bearing cast or crutches or brace for a minimum of 6 weeks. The patient was routinely followed up every 6 weeks for 6 months and thereafter every 3 months.
The final assessment for bone results and functional result was done using:
a) Healing time
b) External fixation index
c) Association for the Study and Application of the Method of Ilizarov (ASAMI) Scoring System
Results
Our study comprised of twenty-seven patients of infected gap non-union of tibia treated between September 2013 and November 2015. The treatment was done by an Ilizarov ring fixator in 12 (44%) patients and a monolateral fixator in 15 (55%) patients. Males (89%) outnumbered the fairer sex and were usually in the younger (25-35) age group (Figure 1, 2, and 3).
Figure 1.

Definitive management of infected non-union
Figure 2.

Sex distribution of patients with infected non-union
Figure 3.

Age distribution of patients with infected non-union
At the time of admission 18 patients were discharged via an open infected wound or sinus and were categorised as Infected Active draining (IAD).
Five patients who were not actively draining at admission, but showed evidence of infection such as fever or abscess due to the injury to the leg were included in the Infected Active Not Discharging (IAND) group.
There were 4 patients who conclusively showed evidence of infection of the bone or soft tissue in the form of a positive bacterial culture on exploration at the fracture site, a positive radioisotope scan, or imaging evidence including PET, but had not drained for the past three months and were not having fever or abscess. These patients were labelled as having Quiescent Infection (QI) (Figure 4).
Figure 4.
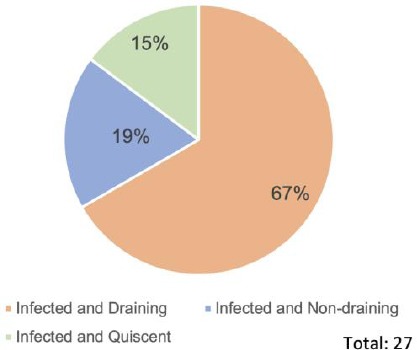
Type of Infected non-unions (AO Classification)
According to Paley’s classification of non-union, 16 of the patient’s post-debridement were in the B1 group having a bone gap > 1 cm with no bone shortening while rest 11 patients were in the B3 group with both bone defect and shortening. Though 20 of the patients did not present with an initial bone gap, the bone gap post radical debridement ranged between 1.3 cm to 9.3 cm with a mean of 4.38 cm (Figure 5).
Figure 5.

Paley’s Classification of Gap non-union after Debridement
Most of the patients had multiple procedures before presentation as infected non-union. The main previous treatment that outlived the others was an external fixator in 17; an intramedullary nail in 5; plating in 4 and POP cast in 1. The average time between the fracture and presentation to us was 9.4 months with a range of 6.5 months to 16.5 months (Figure 6).
Figure 6.

Predominant previous treatment modality
Acute Docking was done in 10 of our patients. The maximum post debridement bone gap in patients who underwent acute docking was 3.8 cm. Eight patients received a cancellous bone graft at the fracture site. We used Antibiotic-impregnated gradual release cement spacer in 6 of our patients and STIMULAN® pellets in 2 patients (Figure 7).
Figure 7.

Patients who underwent Adjunctive Treatment
The healing time ranged between 4.1 to 10.1 months, and the average time was 6.5 months. The average bone healing index was calculated as 1.44 months/cm and fell in the range of 1.04 months/cm to 1.81 months/cm. The external fixator was applied on an average of 12.86 months within a range of 7.2 months to 19.2 months excluding the patients with plating and two amputations. The external fixator index average was 2.9 months/cm with a range from 1.7 months/cm to 3.69 months/cm.
In one of the patients after adequate bone lengthening, the transported segment tilt made it desirable to correct it by plating and bone grafting. The LRS was removed at the time of plating after the duration of 4.8 months.
Infection persisted despite radical debridement in four of the twenty-seven patients and played an important role in the decision for amputation. Two patients underwent a below-knee amputation, and both had persistent infection with non-union. Of these two patients who finally landed as failures, one of the patients had approximately 15-degree fixed flexion deformity of the knee with stiffness while the other had a partial sensory loss with decubitus ulcer on foot. The sensory loss along with persistent infection and non-union paved the way for amputation in this patient.
The Bony union was assessed by the ASAMI SCORING SYSTEM. It was found to be Excellent in 67% (18) patients; Good in 19% (5) patients; Fair and Poor in 7% (2) each. The poor score represented the two amputations. The functional ASAMI Score was Excellent in 63% (17) patients, Good in 26% (7) patients, Fair in 4% (1) and Failure in 7% (2) (Figure 8 and 9).
Figure 8.

ASAMI-Bone
Figure 9.

ASAMI-Functional
Pin tract infection was commonly encountered. Grade 0-1 DAHL was present in almost all the patients at some point of time, and in nine of our patients, DAHL 2-3 grade infection was present which responded to conservative treatment.
Equinus deformity occurred in 6 patients. Two had concomitant heel varus deformity. These were corrected by SUV application in few patients.
Discussion
With distraction osteogenesis at command, bone gap ceased to be the crucial deterrent it was at salvaging limbs a couple of decades back. Furthermore, the liberty with which the treating surgeon can radically debride bone without the fear of shortening to achieve good vascularised bone for the union has lessened the persistence of infection. Nevertheless, these strides in treatment have been more than matched by the challenges of shattered bones with a bone gap and extensive soft tissue injury commonly seen in the ever-rising high-speed vehicular accidents, and of late in the not too uncommon blast and firearm injuries.
The predominance of the younger age group (average age 36.3 years; range 19-69 yrs.) shows the same trend as in other studies. In a study done by Tang LIU et al., 2011 [9] (average 37.3 years, range 18-64 years); Kiran et al., 2012 [10] (average 34.54 years, range 21-54 years); Vignes et al., 2014 [11] (average 36 years, range 24-51 years). The higher incidence in the younger population corresponds closely with the increased rate of road traffic accidents at this age.
Conventionally many methods have been employed to overcome the problem of infected gap non-union in tibia, but all of them have several shortcomings and limitations. Multiple debridements, sensitivity guided antibiotics, irrigation of the wound with novel topical antibiotic delivery systems have all been used to eradicate infection with limited success. Autologous bone graft is good for small defects, but if the defect is large, the graft may have to be harvested from more than one site, adding to the morbidity of the patient. Also, there is a limit to the quantity of autologous bone graft that can be procured, which may not be enough for large defects [12].
In a study by Zile S Kundu et al., [2], it was seen that in adults the hypertrophy of the fibula usually took a long time compared to children. Therefore, they needed prolonged protective weight-bearing with the help of a brace. Some shortening of limb persisted in almost all cases. In spite of shortening, tibialization of the fibula provided an acceptable function to many patients and served as a good enough alternative to amputation, where there were adequate vascularity and intact sensation in the sole.
The bone transport and distraction osteogenesis pioneered by Ilizarov solves many of these problems in a much better way. It can produce bone of similar size and shape as lost; fearless radical debridement gives the best chance to eradicate infection; circumferential control minimizes deviation and deformity; weight bearing can be allowed early; early joint mobility minimises stiffness; soft tissue lengthening is simultaneously achieved obviating need for soft tissue reconstruction often and above all the procedure has stood the test of time and given good results consistently [3], [13], [14], [15], [16].
The monolateral LRS fixator is a clever offshoot of the Ilizarov osteogenic tree that brings in some positive features at the expenses of others. Because of its application to one side of the bone it is relatively easier to apply, has a lighter frame and thereby easy to carry around during ambulation, often cheaper versions are available, and it provides for greater access due to its openness for dressings and procedures which can be accomplished without removal of the frame. The price to pay is mainly the loss of circumferential manipulation, which increases deviations and deformities.
In our selection of the procedure, the choice of the frame was at times arbitrary but many a time guided by the patient’s desire for a lighter frame or the requirements for dressings where an LRS was preferred. A small proximal tibia segment, need for deformity correction made a circular frame desirable. The average union time was 6.5 months and the average healing index 1.44 months/cm. Similarly, the average fixator application time was 12.86 months and the external fixator index 2.9 months/cm. Two of the twenty-seven patients did not achieve union. These results are not much different from other studies. In a study performed by Tranquilli et al., [17] in Italy on 20 patients with nonunion of the tibia, the mean time of union was 4.5 months. In a series of 25 cases studied by Kiran et al., [10], the mean time taken for union per cm of the bone gap was 1.7 months/cm.
We achieved an ASAMI Bone healing score of Excellent (67%) to Good (19%) in 86% of cases. The functional score was less in the excellent group (63%) but the Good group (26%) more than made up for it. The results compare favourably with other studies. Paley et al., [13] reported 60.87% excellent and 26.09% good result. His functional results were 64% and 28% respectively. Magadum et al., [14] had bony results of 76% (Excellent) and 20% (Good); and functional result of 60% (Excellent) and 32% (Good).
Two patients landed in non-union and had to undergo below knee amputation. Infection persisted in both. One of them had partial sensory loss in the sole and pressure ulceration along with ankle equinus deformity. The other had a stiff osteoarthritis knee and developed diabetes after the LRS system was in place. Although amputation is never a pleasant option either for the patient or surgeon but at times is the best option and saves lots of morbidities and should not be prolonged unnecessarily. They were aged 56 and 69 respectively. The ripe age, persistence of infection, neuropathy, and significant joint deformities all put their weight in favour of amputation.
Pin track infection [6] usually mild (Grade 0-1 DAHLS) often occurred at some time or the other in almost all patients and was managed conservatively. Grade 2-3 occurred in 33% of cases. Vignes et al., [11] reported Grade 0 Dahl in all patients and Grade 1 in 17 out of 20 patients. In a study by S.B Naique [18] significant pin-tract infections requiring a surgical procedure were seen in four of 45 fractures (7%) which had been stabilised with half pins and external fixators.
Equinus deformity occurred in five of the twenty-five healed patients, and two of them had varus deformity. Knee stiffness was present in one of the healed patients besides one amputee. Limb shortening of clinical significance producing limp was present in four cases and was corrected by the required rise in the shoe. Kiran et al., [10] reported equinus deformity and knee stiffness each in 4 of their series of 25 cases.
In conclusion, tibia fractures with or without bone gap are becoming increasingly common due to high-speed road traffic accidents and often present a challenge in reconstruction. The low vascularity of the leg in general and the accompanying soft tissue loss often with exposed and de-vascularised bone provides a fertile bed for infection. Even if the bone gap is not present initially significant bone gap results as radical debridement forms an essential pillar of successful treatment to eradicate the infection.
Distraction osteogenesis and bone transport can be considered to be the gold standard for infected gap non-union of the tibia as it simultaneously solves the problem of the bone gap, infection (radical debridement without fear of bone gap), deformity correction, early weight bearing and concomitant soft tissue expansion.
The classical ring fixator of Ilizarov is the principal device used for distraction osteogenesis and bone transport, but the monolateral fixator can be used in select cases where the lighter frame is preferred and is relatively easy to apply. LRS is not preferred when deformities need correction or are anticipated and if the fixation is too close to a joint. Intramedullary nailing or plating is best avoided till infection clears. General factors such as correction of anaemia, cessation of smoking, adequate nutrition or control of blood sugar in people with diabetes can never be overlooked. Besides counselling of the patient in preparation of the protracted treatment after an already long earlier attempt at the union is of crucial importance.
The present study comprised of twenty-seven patients of infected gap nonunion of the tibia {24 males: 3 females}. Fifteen {56 %} of these patients were treated with an LRS-mono-lateral fixator and the rest with Ilizarov ring fixator.
The overall ASAMI-Bone healing score was Excellent or Good in 86% patients {Excellent-67%; Good-19%}. ASAMI Functional score was Excellent or Good in 89% of patients {Excellent -63%; Good -26%}. The commonest problems were of pin tract infection and wire loosening, and angulation of the transported segment. Joint stiffness especially of the ankle in equinus was also encountered.
Elderly age, persistent infection, sensory loss in the foot, the stiffness of the knee, and above all the patient’s reluctance to go any further given the protracted treatment besides, systemic disorders such as diabetes are all pointers for considering amputation as an alternative.
Footnotes
Funding: This research did not receive any financial support
Competing Interests: The authors have declared that no competing interests exist
Reference
- 1.Aronson J, Rock L, Arkansas Limb lengthening, Skeletal reconstruction and bone transport with the Ilizarov methods. J Bone Joint Surg Am. 1997;79:1243–58. doi: 10.2106/00004623-199708000-00019. https://doi.org/10.2106/00004623-199708000-00019 PMid:9278087. [DOI] [PubMed] [Google Scholar]
- 2.Zile S Kundu, Gupta V. Gap non-union of tibia treated by Huntington's procedure. Indian J Orthop. 2012;46(6):653–658. doi: 10.4103/0019-5413.104197. https://doi.org/10.4103/0019-5413.104197 PMid:23325967 PMCid:PMC3543882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dendrinos G.K, S Kontos. Use of the Ilizarov Technique for Treatment of nonunion of the tibia associated with infection. J Bone Joint Surg. 1995;77-A:835–46. doi: 10.2106/00004623-199506000-00004. https://doi.org/10.2106/00004623-199506000-00004. [DOI] [PubMed] [Google Scholar]
- 4.Paley D, Catagni MA, Arganani F, et al. Ilizarov treatment of tibia nonunions with bone loss. Clin Orthop Relat Res. 1989;241:146–65. PMid:2924458. [PubMed] [Google Scholar]
- 5.Rosen H. Pseudoarthroses :Infected, Manual of Internal fixation by AO-ASIF Group. (3rd Edition) 1991;(Chap 19.5.2):722–23. [Google Scholar]
- 6.Dahl MT, Gulli B, Berg T. Complications of limb lengthening a learning curve. Clin Orthop. 1994;301:10–18. https://doi.org/10.1097/00003086-199404000-00003. [PubMed] [Google Scholar]
- 7.Kulkarni GS. Biomechanics of Ilizarov Ring Fixator, Textbook of Orthopaedics and Trauma. (2nd Edition) 2008;(177):1506–1518. [Google Scholar]
- 8.Parihar M. Post-operative care in the Ilizarov method. Textbook of Orthopaedics and Trauma. (2nd Edition) 2008;(196):1753–1758. [Google Scholar]
- 9.Tang LIU, et al. One stage management of post traumatic tibial infected non union using bone transport after debridement. Turk J Med Sci. 2012;42(6):1111–1120. [Google Scholar]
- 10.Kiran M, Jee R. Bone Transport in Tibial Gap Non-Union—A Series of 25 Cases. Open Journal of Orthopedics. 2012;2(04):144. https://doi.org/10.4236/ojo.2012.24027. [Google Scholar]
- 11.Vignes GS, Arumugam S, Ramabadran P. Functional outcome of infected non-union tibia fracture treated by Ilizarov fixation. Int J Sci Study. 2014;2(7):87–92. [Google Scholar]
- 12.Chaddha M, Gulati D, Singh AP, Singh AP, Maini L. Management of massive posttraumatic bone defects in the lower limb with the Ilizarov technique. Acta Orthopædica Belgica. 2010;76(6):811–820. PMid:21302581. [PubMed] [Google Scholar]
- 13.Paley FB, Chirstianson D. An analysis of Illizarov and external fixators. Clin Orthop Relat Res. 1989;241:195. [Google Scholar]
- 14.Magadum MP, Yadav CB, Phaneesha MS, Ramesh LJ. Acute compression and lengthening by the Ilizarov technique for infected nonunion of the tibia with large bone defects. Journal of Orthopaedic Surgery. 2006;14(3):273–9. doi: 10.1177/230949900601400308. https://doi.org/10.1177/230949900601400308 PMid:17200528. [DOI] [PubMed] [Google Scholar]
- 15.Farmanullah Khan MS, Awais SM. Evaluation of management of tibial non union defect with Ilizarov fixator. J Ayub Med Coll Abbottabad. 2007;19:34–6. [PubMed] [Google Scholar]
- 16.Madhusudhan TR, Ramesh B, Manjunath KS, Shah HM, Sundaresh DC, Krishnappa N. Outcomes of Ilizarov ring fixation in recalcitrant infected tibial non-unions–a prospective study. Journal of trauma management & outcomes. 2008;2(1):6. doi: 10.1186/1752-2897-2-6. https://doi.org/10.1186/1752-2897-2-6 PMid:18651977 PMCid:PMC2515289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tranquilli PL, Merolli A, Perrone V, Caruso L, Giannotta L. The effectiveness of the circular external fixator in the treatment of post-traumatic of the tibia nonunion. La Chirurgia degli organi di movimento. 2000;85(3):235–42. [PubMed] [Google Scholar]
- 18.Naique SB, Pearse M, Nanchahal J. Management of severe open tibial fractures:the need for combined orthopaedic and plastic surgical treatment in specialist centres. The Journal of bone and joint surgery. British volume. 2006;88(3):351–7. doi: 10.1302/0301-620X.88B3.17120. https://doi.org/10.1302/0301-620X.88B3.17120 PMid:16498010. [DOI] [PubMed] [Google Scholar]


