Abstract
We present a 22-year-old pregnant woman at 15 weeks of gestation, with abdominal pain and vomiting. We demonstrate that diagnosis and treatment of vomiting and abdominal pain in pregnancy can be difficult. Therefore, involvement of other medical specialists is important when common treatments fail. Cholesterolosis can cause symptoms similar to those caused by cholelithiasis. Controversial to gallstones, identification of cholesterolosis by ultrasound is hard. Cholecystectomy is the only effective treatment option for cholesterolosis and can be performed safely during pregnancy. Cholecystectomy in pregnancy should be considered if, despite atypical symptoms, gallbladder disease is suspected and other diagnoses are ruled out. This may reduce recurrent symptoms, hospital admissions, exposure to harmful drugs and obstetric complications.
Keywords: pancreas and biliary tract, pregnancy, gastrointestinal surgery
Background
Abdominal pain and vomiting in pregnancy are known to have many causes. With an incidence up to 80%,1 hyperemesis gravidarum is the most common cause of vomiting in early pregnancy. Nevertheless, other diagnoses are applicable if vomiting persists over a long period of time or if other symptoms coexist. With this case report, we want to show that diagnosis and treatment of vomiting and abdominal pain in pregnancy can be difficult. To prevent doctor’s delay, involvement of other medical specialists is important when common treatments fail. In this case, involvement of several disciplines was required to make a diagnosis and to define safe treatment options.
With this case report, we also want to show that conservative management is probably not always the best option during pregnancy. Many interventions are contraindicated in pregnancy because of the fetus. When you consider surgery, you should always be aware of the risks the procedure may have for mother and fetus. However, no severe maternal or fetal complications of (laparoscopic) cholecystectomy during pregnancy are reported in literature.2–4
Case presentation
At 15 weeks of gestation, a 22-year-old gravida 2 para 0, previously diagnosed with hyperemesis gravidarum, was admitted to the hospital due to increased vomiting and sudden onset of discontinuous abdominal pain. The abdominal pain was located in the upper middle quadrant, accompanied by the urge to move. She had not had a bowel movement for a couple of days, and urine was slightly darker in colour. She had just returned from a holiday in the Caribbean. On presentation, we saw an obese woman (body mass index [BMI] 32 kg/m²), not acutely ill looking, no jaundice. She was vitally stable without fever. On examination, the pain was located in the epigastric region; there were no peritoneal signs. Awaiting follow-up research, patient got rehydrated and supplemented with potassium because of hypopotassaemia. Symptoms reduced in a couple of days. Nevertheless, the vomiting returned and the abdominal pain turned into chronic, continuous pain during her pregnancy.
Investigations
Blood tests (table 1) revealed elevated liver enzymes. C reactive protein and leucocytes were slightly increased. Infectious causes of vomiting and abdominal pain were ruled out. Repeated abdominal ultrasound showed thickened gallbladder wall (interpreted as gallbladder sludge), no stones, no signs of cholecystitis and no dilated bile ducts. Because the abdominal pain and vomiting were persistent, a Magnetic Resonance Cholangiopancreatography was performed with similar results. In addition, an endoscopic ultrasound showed no signs of cholecystitis or dilated bile ducts. Recurrent examination of the fetus was without anomalies.
Table 1.
Blood count on day of presentation
| Haemoglobin | 126 g/L |
| Leucocytes | 12.7×109/L |
| Alkaline phosphatase | 143 IU/L |
| Aspartate aminotransferase (ALAT) | 221 IU/L |
| Alanine aminotransferase (ASAT) | 104 IU/L |
| Bilirubin (total) | 14 μmol/L |
| Gamma-glutamyltransferase | 68 IU/L |
| C reactive protein | 28 mg/L |
Differential diagnosis
Because patient had just returned from the Caribbean, infectious diseases were considered. In consultation with internal medicine, hepatitis, cytomegalovirus, Epstein-Barr virus, HIV, Lues and Zika virus were ruled out. Stool culture was negative for Helicobacter pylori, Salmonella, Shigella, Yersinia, Campylobacter, Plesiomonas shigelloides and parasites. Because of the increased liver enzymes, Wilson’s disease was ruled out. The gastroenterologist and surgeon were consulted because symptomatic cholelithiasis was considered several times. Presentation of symptoms was atypical, and imaging was without signs of complicated cholelithiasis (including cholecystitis, pancreatitis, choledocholithiasis or cholangitis), therefore a cholecystectomy was not performed. Other causes of severe abdominal pain and vomiting had to be excluded. The psychiatrist ruled out any psychiatric origin of the symptoms. Anesthesiology suggested muscle tear of the rectus abdominus caused by prior vomiting or anterior cutaneous nerve entrapment syndrome or thoracic-abdominal intercostal neuralgia as a cause for the abdominal pain. When symptoms continued and liver enzymes increased again over time, pre-eclampsia, hemolysis elevated liver enzymes and low platelets syndrome and acute fatty liver were ruled out.
Treatment
No pain relief was obtained using paracetamol, buscopan and temazepam. Because non-steroidal anti-inflammatory drugs are contraindicated in pregnancy, they were not given. Morphine reduced the abdominal pain but was given as little as possible to prevent maternal addiction and neonatal abstinence syndrome.5 Because infection was not suspected, patient did not receive antibiotics. A duodenal probe decreased vomiting, but vomiting and abdominal pain persisted. Consulting a team specialised in pain treatment, an intercostal nerve block was given. This did not solve the severe abdominal pain. At last, epidural anaesthesia reduced her symptoms.
During her pregnancy, cholecystectomy was considered several times when symptoms persisted. Nevertheless, surgeons abstained from cholecystectomy in pregnancy because presentation of symptoms was atypical for gallbladder disease and complicated cholelithiasis was ruled out. Because imaging was accurate, the added value of diagnostic laparoscopy was not considered to outweigh any complications of surgery.4
Patient had to be admitted to hospital several times due to recurrent abdominal pain and vomiting. Because of the persistent symptoms, labour was induced at 37 weeks of gestation. Patient developed pre-eclampsia during delivery. After delivery, the abdominal pain and vomiting persisted. A relation between pregnancy and symptoms was now excluded. Despite no evident gallstones present at repeated imaging in both pregnancy and after delivery, but with other diagnoses ruled out, symptomatic cholelithiasis was the only likely cause of the symptoms. Patient underwent laparoscopic cholecystectomy 1 month after delivery.
Outcome and follow-up
After laparoscopic cholecystectomy, patient was free of symptoms. Histology showed a gallbladder with cholesterolosis and without gallstones (figure 1).
Figure 1.
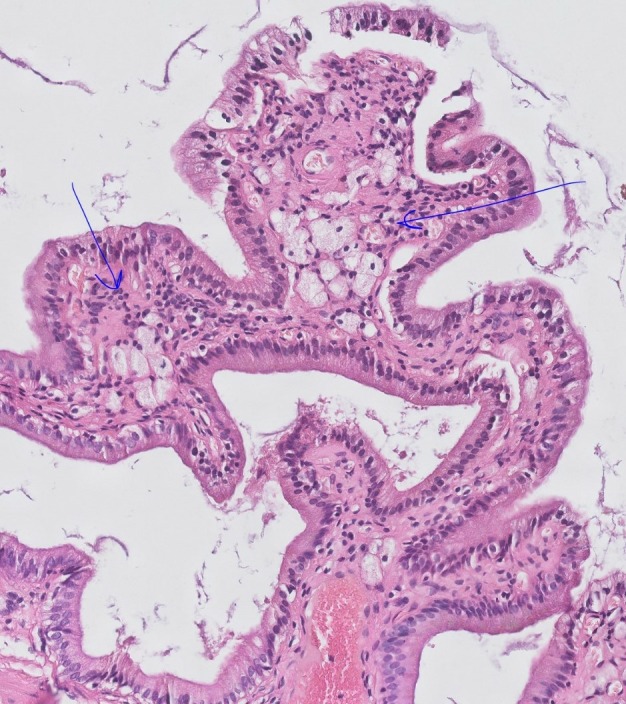
Pathology of the patient’s gallbladder. Typical macrophages with foamy appearance (foam cells) are marked with blue arrows, indicating cholesterolosis.
Discussion
Cholesterol polyps (cholesterolosis) are the most common, benign non-neoplastic, non-inflammatory lesions of the gallbladder.6 The prevalence of cholesterolosis varies from 9% to 26% and cholesterolosis is more likely to be present in young adults.7 8 An association between cholesterolosis and high BMI is found.9 Symptoms similar to those caused by gallstones may occur if the cholesterol polyps separate from the underlying mucosa.10 Ultrasonic identification of the cholesterolosis can be hard, because diffuse cholesterolosis has no ultrasonographic specifications.11 However, it has been found that wall thickness may be associated with the presence of cholesterolosis.12 Because cholecystectomy is the only effective treatment option for cholesterolosis, cholecystectomy has to be considered in symptomatic patients.13
Multiple studies researched risks and benefits of surgery during pregnancy. Although no severe maternal or fetal complications of (laparoscopic) cholecystectomy during pregnancy are reported, general risks of surgery obviously exist. Cholecystectomy in pregnancy can be performed in all trimesters. Several studies compared conservative management versus cholecystectomy in respect to symptomatic (uncomplicated) gallbladder disease. They demonstrated reduction of recurrent symptoms and hospital admissions if cholecystectomy was performed during pregnancy.2–4 14–20Dhupar et al 2 compared cholecystectomy versus non-operative management in respect to obstetric complications, including pre-eclampsia, preterm premature rupture of membranes and early induction. They found lower rates of obstetric complications if surgery was performed during pregnancy (18% vs 36%).2 In more than two-third of the cases, abdominal pain was resolved after elective surgery.21Compared with conservative management, cholecystectomy during pregnancy may reduce medical costs, patient suffering and may prevent recurrent maternal and fetal exposure to harmful drugs.
In our case, symptom presentation was atypical. Many diseases had to be ruled out with the help of multidisciplinary consultations. Several times during pregnancy, we considered cholecystectomy; however, because gallstones were never detected at imaging and the typical colic pain turned into chronic pain, cholecystectomy was not performed. If surgery had been performed early in pregnancy, recurrent hospital admissions, patient suffering and exposure to harmful drugs could have been avoided. In addition, our patient probably would not have needed induction at 37 weeks of gestation and might not have developed pre-eclampsia due to conservative management.2 Thickened gallbladder wall, interpreted as gallbladder sludge, was present at every imaging. Nevertheless, histology did not show gallstones or gallbladder sludge. In retrospect, thickened gallbladder wall on imaging due to cholesterolosis may be incorrectly interpreted as gallbladder sludge.
If symptoms similar to cholelithiasis are present in young obese women, abdominal ultrasound shows lack of gallstones and thickened wall is present, cholesterolosis should be considered. Cholecystectomy in pregnancy is an effective and safe treatment option and should be considered, since it may reduce recurrent symptoms, hospital admissions, exposure to harmful drugs and obstetric complications.
Patient’s perspective.
My pregnancy was very painful. The pain did not stop. I felt depressed. The vomiting was also inconvenient. I especially hated the duodenal probe. It was frustrating that the doctors were not sure where the pain was coming from. Nevertheless, I do understand that they postponed the operation until after the delivery because the diagnosis was not clear. I am glad the pain resolved after surgery.
Learning points.
Multidisciplinary involvement is important when common treatments fail in pregnant women with vomiting and abdominal pain.
Cholesterolosis can mimic symptoms caused by cholelithiasis.
When ultrasound shows a thickened gallbladder wall, cholesterolosis should be considered.
The only treatment option for symptomatic cholesterolosis is cholecystectomy.
Cholecystectomy during pregnancy is safe and may reduce recurrent symptoms, hospital admissions, exposure to harmful drugs and obstetric complications.
Footnotes
Contributors: Each author has indicated that she has met the journal’s requirements for authorship. EVJvLS, MGvP and EWMJ were all involved in patient’s care. Together with EWMJ, EVJvLS concepted a first version of the manuscript. MGvP made revisions to the manuscript. Because the gastro-enterologists were intensively involved in this case, JMJ made revisions to the manuscript as well. All authors accepted the final and submitted version of this manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Not required.
References
- 1. Boelig RC, Barton SJ, Saccone G, et al. Interventions for treating hyperemesis gravidarum: a Cochrane systematic review and meta-analysis. J Matern Fetal Neonatal Med 2018;31:2492–505. 10.1080/14767058.2017.1342805 [DOI] [PubMed] [Google Scholar]
- 2. Dhupar R, Smaldone GM, Hamad GG. Is there a benefit to delaying cholecystectomy for symptomatic gallbladder disease during pregnancy? Surg Endosc 2010;24:108–12. 10.1007/s00464-009-0544-x [DOI] [PubMed] [Google Scholar]
- 3. Athwal R, Bhogal RH, Hodson J, et al. Surgery for gallstone disease during pregnancy does not increase fetal or maternal mortality: a meta-analysis. Hepatobiliary Surg Nutr 2016;5:53–7. 10.3978/j.issn.2304-3881.2015.11.02 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pearl JP, Price RR, Tonkin AE, et al. Dimitrios Stefanidis. Guidelines for the use of laparoscopy during pregnancy. https://www.sages.org/publications/guidelines/guidelines-for-diagnosis-treatment-and-use-of-laparoscopy-for-surgical-problems-during-pregnancy [DOI] [PubMed]
- 5. Desai RJ, Huybrechts KF, Hernandez-Diaz S, et al. Exposure to prescription opioid analgesics in utero and risk of neonatal abstinence syndrome: population based cohort study. BMJ 2015;350:h2102 10.1136/bmj.h2102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Yang HL, Sun YG, Wang Z. Polypoid lesions of the gallbladder: diagnosis and indications for surgery. Br J Surg 1992;79:227–9. 10.1002/bjs.1800790312 [DOI] [PubMed] [Google Scholar]
- 7. Salmenkivi K. Cholesterosis of the gall-bladder. a clinical study based on 269 cholecystectomies. Acta Chir Scand Suppl 1964;105:1. [PubMed] [Google Scholar]
- 8. Maqsood H, Patel K, Ferdosi H, et al. intra- and postcholecystectomy: a retrospective cohort study of 6868 patients. International Journal of Surgery 2017;39:119–26. [DOI] [PubMed] [Google Scholar]
- 9. Liew PL, Wang W, Lee YC, et al. Gallbladder disease among obese patients in Taiwan. Obes Surg 2007;17:383–90. 10.1007/s11695-007-9068-4 [DOI] [PubMed] [Google Scholar]
- 10. Feldman M, FELDMAN M. Cholesterosis of the gallbladder; an autopsy study of 165 cases. Gastroenterology 1954;27:641. [PubMed] [Google Scholar]
- 11. Kubota K, Bandai Y, Noie T, et al. How should polypoid lesions of the gallbladder be treated in the era of laparoscopic cholecystectomy? Surgery 1995;117:481–7. 10.1016/S0039-6060(05)80245-4 [DOI] [PubMed] [Google Scholar]
- 12. Dairi S, Demeusy A, Sill AM, et al. Implications of gallbladder cholesterolosis and cholesterol polyps? J Surg Res 2016;200:467–72. 10.1016/j.jss.2015.08.037 [DOI] [PubMed] [Google Scholar]
- 13. Gurusamy KS, Abu-Amara M, Farouk M, et al. Cholecystectomy for gallbladder polyp. Chochrane Database Syst Rev 2009:CD007052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jorge AM, Keswani RN, Veerappan A, et al. Non-operative management of symptomatic cholelithiasis in pregnancy is associated with frequent hospitalizations. J Gastrointest Surg 2015;19:598–603. 10.1007/s11605-015-2757-8 [DOI] [PubMed] [Google Scholar]
- 15. de Bakker JK, Dijksman LM, Donkervoort SC. Safety and outcome of general surgical open and laparoscopic procedures during pregnancy. Surg Endosc 2011;25:1574–8. 10.1007/s00464-010-1441-z [DOI] [PubMed] [Google Scholar]
- 16. Date RS, Kaushal M, Ramesh A. A review of the management of gallstone disease and its complications in pregnancy. Am J Surg 2008;196:599–608. 10.1016/j.amjsurg.2008.01.015 [DOI] [PubMed] [Google Scholar]
- 17. Pearl J, Price R, Richardson W, et al. treatment, and use of laparoscopy for surgical problems during pregnancy. Surg Endosc 2011;25:3479–92. [DOI] [PubMed] [Google Scholar]
- 18. Othman MO, Stone E, Hashimi M, et al. Conservative management of cholelithiasis and its complications in pregnancy is associated with recurrent symptoms and more emergency department visits. Gastrointest Endosc 2012;76:564–9. 10.1016/j.gie.2012.04.475 [DOI] [PubMed] [Google Scholar]
- 19. Sedaghat N, Cao AM, Eslick GD, et al. Laparoscopic versus open cholecystectomy in pregnancy: a systematic review and meta-analysis. Surg Endosc 2017;31:673–9. 10.1007/s00464-016-5019-2 [DOI] [PubMed] [Google Scholar]
- 20. Hedström J, Nilsson J, Andersson R, et al. Changing management of gallstone-related disease in pregnancy - a retrospective cohort analysis. Scand J Gastroenterol 2017;52:1–6. 10.1080/00365521.2017.1333627 [DOI] [PubMed] [Google Scholar]
- 21. van Dijk AH, Lamberts M, van Laarhoven CJHM, et al. Laparoscopy in cholecysto-choledocholithiasis. Best Pract Res Clin Gastroenterol 2014;28:195–209. 10.1016/j.bpg.2013.11.015 [DOI] [PubMed] [Google Scholar]


