Abstract
With an increasing use of intraoperative fluoroscopy in operating rooms worldwide, the topic of radiation exposure has become a major concern among hospital staff, doctors and patients alike. Since fluoroscopy has become an integral part in orthopedic intraoperative management, we sought to identify whether surgeon grade or experience plays a role in the amount of radiation used and consequently exposed. We performed a systematic review examining the association between surgeon experience and radiation exposure using primary outcome measures (radiation dose and total screening time/fluoroscopy time). To be included in the review, the study population had to compare varying surgeon experience levels and their effect on the primary outcomes. A total of eighteen studies were included in the review. The studies were a mix of prospective and retrospective studies with low to moderate quality as evaluated by the MINORs criteria. Studies were variable in defining surgeon experience levels and in the type of operations being performed. Majority of the studies showed that inexperienced surgeons/trainees had a higher total fluoroscopy time and a higher mean radiation exposure as compared to experienced surgeons. We conclude that higher surgeon experience significantly reduces usage of fluoroscopy and the consequent radiation exposure in orthopedic procedures. Introduction of strict radiation guidelines involving limited usage of fluoroscopy and supervision of trainees may be beneficial in controlling radiation exposure in the future.
Key words: Radiation Exposure, Surgeon experience, Radiation, Fluoroscopy
Abstract
Ever since the introduction of mobile fluoroscopy or the C-arm in 1950s, their use and popularity has increased phenomenally in surgery. Though initially only introduced for trauma operating rooms, the C-arm has now become a core component for various surgical subspecialties especially in Orthopedics. One of the most valuable tools in an orthopedic surgeon’s arsenal is the mobile C-arm. The principle of allowing real-time image capturing to ensure adequate anatomical reduction and appropriate fixation of complex fractures has been a major cause of success in orthopedic surgery. Even though the C-arm allows real time image capturing and intensification to allow accurate placement of implants and fixation devices with minimal incisions, it does come at a very grave cost of large amounts of ionizing radiation exposure to the operating room personnel.1-3 Though the risks of radiation exposure to major areas of the body(thyroid, gonads and hands of surgeons) have been recognized4 and linked to the development of blood cancers such as leukemias and thyroid cancers,5,6 there have been few studies showing whether surgeon experience is correlated with the amount of radiation exposure. From a practical perspective, it makes sense to consider that the higher the number of cases done by an orthopedic surgeon, more experience would be gained and lesser would be the dependence on the mobile C-arm to ensure adequate reduction with more reliance on clinical expertise. However, studies have shown conflicting results with respect to such a question.7-9 With a myriad of studies from all over the world presenting varying results and with a lack of a review to consolidate findings of the past half century, we sought to conduct a detailed systematic review to gather all pertinent information and attempt to arrive at a definitive conclusion on whether surgeon experience has an impact on radiation exposure in orthopedic surgeries. Results from this study will allow not only allow orthopedic personnel and new trainees to better ensure a strict rigid approach to limiting the use of excessive fluoroscopy to prevent harmful exposure, but also allow supervising hospital personnel to implement new rules and behavior modification in their staff to ensure better and safer outcomes for both patient and doctors.
Eligibility criteria
To be included in the review, the study population had to compare primary outcomes between varying degrees of orthopedic surgical experience. The primary outcomes that were included in the systematic review included total fluoroscopy time/screening time and radiation dose exposure. Studies were not limited to the type of orthopedic procedure being performed. Studies that involved investigating the impact of surgeon experience on radiation exposure in other surgical specialties were excluded from the review. Relevant papers were reviewed using the Preferred Reporting Items for Systematic reviews and Meta Analyses (PRISMA) statement as a guideline.10
Information sources and study selection
We searched the Pubmed, OVID MED-LINE (1966 to 2017) and Google Scholar databases in September 2017 using a variety of combinations of the following search criteria words: “Surgeon experience”, “Radiation Dose”, “Radiation Exposure”, “Radiation”, “Experience”, “Trainees”. No restrictions were placed on publication date and study design. Only articles using English as their primary language were retrieved from the database. A total of 2279 publications were retrieved using the search criteria. Two authors screened all titles and abstracts retrieved from this search. Full-length texts of articles that seemed clinically relevant to the study were then retrieved. Additionally, the bibliographies of these full-length articles were reviewed and full-length articles retrieved for those references deemed potentially relevant or of uncertain relevance. For manuscripts where further clarification was required, a third author was used for reaching mutual agreement of including the paper or not. Full-length articles were reviewed and data was independently extracted. Studies that contained data on other surgical specialties were excluded from the study. Flowchart of data extraction is shown in Figure 1. The studies were a mix of prospective and retrospective studies with an absence of a properly detailed constructed randomized clinical trial (Table 1).
Figure 1.
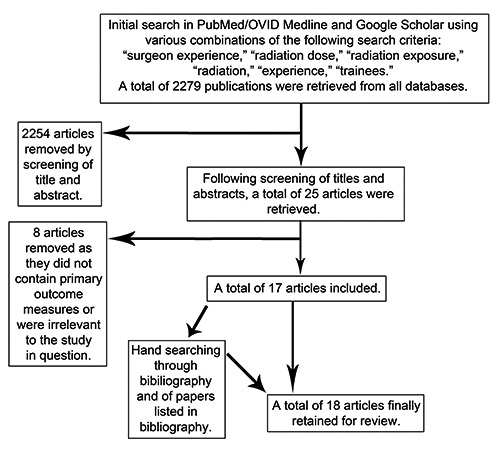
Flowchart showing extraction of data.
Table 1.
Characteristics of studies included in review.
| Author (Year) | Study design | Sample size (N) | Country of origin | Primary outcomes studied |
|---|---|---|---|---|
| Goldstone (1993) | Prospective case series | 44 | United Kingdom | Radiation dose (microSv) |
| Giannoudis (1998) | Retrospective cohort study | 60 | United Kingdom | Screening time and radiation dose (cGy/cm2) |
| Madan (2002) | Retrospective cohort study | 184 | United Kingdom | Radiation time (screening time) and radiation dose (cGy cm2) |
| Blattert (2004) | Prospective cohort study | 23 | Germany | Radiation dose (mSv)/txposure of dominant hand of primary surgeon and total fluoroscopy/screening time |
| Hafez (2005) | Prospective cohort study | 47 | United Kingdom | Screening time and radiation dose (mSv) (to hands) |
| Bahari (2006) | Prospective cohort study | 30 | United Kingdom | Duration of exposure/screening time and number of exposures |
| Botchu(2008) | Retrospective cohort study | 120 | United Kingdom | Screening time and radiation dose/exposure (Gy/cm2) |
| Bar-on (2010) | Prospective cohort study | 43 | Israel | Screening/fluoroscopy time and radiation dose/exposure (millirems) |
| Tuohy (2011) | Prospective case series | 198 | USA | Screening/fluoroscopy time and radiation dose (rem-cm2) |
| Khan (2012) | Prospective Case series | 50 | United Kingdom | Screening time and radiation exposure (mSv) |
| Patel (2013) | Retrospective cohort study | 782 | United Kingdom | Screening/fluorsocopy time and radiation exposure (Gy/cm2) |
| Kraus (2013) | Retrospective Cohort study | 100 | Germany | Total fluoroscopy time/duration of radiation emission |
| Kheiran (2013) | Retrospective cohort study | 95 | United Kingdom | Radiation dose (Gy/cm2) |
| Eisman (2014) | Prospective cohort study | 78 | USA | Total fluoroscopy time (TFT) Number of films with part of surgeon’s body in view (exposure % of beam radiation) |
| Cannon (2014) | Retrospective cohort study | 121 | USA | Radiation exposure (mSv/patient) |
| Rashid (2017) | Retrospective cohort study | 849 | United Kingdom | Screening/fluoroscopy time, no. of images taken and radiation exposure/DAP (mGy/cm2) |
| Quah (2017) | Retrospective cohort study | 1203 | United Kingdom | Radiation exposure/dose (mSv) |
| Smith (2017) | Prospective cohort study | 100 | USA | Screening/fluoroscopy time and radiation dose/exposure (mGy) |
Data extraction
Data was independently extracted by two reviewers and tabulated. Variables that were documented included author, year of publication, study design, country of publication, type of orthopedic surgery/intervention, type of radiologic procedures performed (fluoroscopy, X-rays, CT scans etc.), sample size, how surgical experience was defined and primary outcomes and their P-values wherever given if applicable.
Quality appraisal of studies
The studies that were included in our review underwent an appraisal of the quality of methodology using the revised MINORS criteria for non-randomized studies.11 The revised MINORs criteria contain a series of questions with grading done from 0-2. ‘0’ is reported as item/question not reported, ‘1’ is reported as reported but inadequate and ‘2’ is reported as reported and adequate. For non-comparative studies, the maximum score is calculated out of 16 by adding up individual scores of components and for comparative studies the maximum score is out of 24. In accordance with the declaration of Helsinki, details of the study have been made available to the public at ResearchRegistry.com (reviewregistry373).
Study selection
After screening of initial abstracts and removal of duplicates, a total of 798 titles were defined. After reviewing abstracts of the aforementioned titles, a total of 25 studies were finally selected. Additionally, bibliographies of all 25 studies were reviewed for identification of additional articles that may be relevant to the current review. Following detailed review of text and references, 8 articles were removed from as they did not contain pertinent information about the primary outcome measures.9,12-18 One article was retrieved from bibliographic review and was included in the study.19 A total of 18 studies were finally included in the systematic review.7,8,19-34 Details and characteristics of studies are shown in Table 1.
Study design
The studies included in the review were a mix of prospective and retrospective studies. Nine studies were prospective in nature,8,19-22,25,27,28,33 while the remaining nine were retrospective.7,23,24,26,29-32,34
Sample size
Sample Size (N) was recorded as the number of patients in the study. All studies reported total sample sizes. The total sample size comprised by all 17 studies was 3966. The range of sample sizes quoted by different studies was 22-1203 patients.
Origin of studies
Majority of the studies were from the United Kingdom with eleven studies from that region.7,19,20,23,26-28,30-32,34 Four studies were from the United States.8,24,25,33 The remainder of the studies were from Germany22,29 and Israel21 (Table 1).
Type of orthopedic procedures in which fluoroscopy was used
A wide variety of orthopedic procedures were reported in the studies included in the review. This is necessary to take note of as different orthopedic procedures have different average fluoroscopy times, therefore this caused a large variation in the primary outcomes especially with respect to Screening/Total fluoroscopy time. The variation is one of the reasons why a metaanalysis was not possible for this study. Past published systematic reviews investigating radiation exposure in orthopedics have also encountered the same problem.35,36 The complete list of procedures, individual grading of surgeon experience and outcomes for each study is shown in Supplementary Table S1.
Grading of surgeon experience
Due to differences in the origin of the studies, there was marked variation in how surgeon experience was defined. This is also another reason why a meta-analysis was not possible as uniform groups could not be set to allowing pooling of effects to take place.
Eismann et al. grouped the study population into two groups – residents vs. attending physicians.25 Blattert et al. predefined two groups for analyzing their primary outcome measures in IM nailing for long bones – Senior group and Junior Group.22 The Senior group was led by an attending orthopedic trauma surgeon who had performed more than 30 IM nails in the last two years along with assisting surgeons. The junior group consisted of an orthopedic trauma fellow in-training along with assisting surgeons.
Instead of defining surgeon level of the operating surgeon only, Kraus et al. decided to create a point-based system to score the whole surgical team based on their experience.29 The score was calculated by adding the experience level of the surgeon + the experience level of the first assist. Individual points were given as follows: Resident with 1-3 years of experience (1 point), resident with 4-6 years of experience (2 point), Specialist (3 points), Consultant (4 points) and Head of department (5 points).
Tuohy et al. based their study on 3 orthopedic hand surgeons and one hand surgery fellow in training.8 Patel et al. conducted their study in the UK, and thus their grading was based on the traditional UK specialization tiers of consultants, senior registrars and junior registrars.30 Quah,31 Madan,7 Bahari20 and Giannoudis,26 followed as similar tier system.
Similar to Patel, Rashid et al. also divided experience levels based on tiers of consultants, Staff Grade/Associate Specialists and Specialist training registrars.32 Botchu et al. instead of using grade/tier, used the number of years practicing to define experience level.23 Level I was defined as less than 3 years, II was 3-10 years of experience and III was greater than 10 years of experience. Hafez et al. clearly define the level of the operating trainee (first year specialist registrar) and also mentioned a difference in the number of cases being performed by a trainee (6 IM nails in 5 months) vs that of a consultant (14 cases in 2 months).28 Kheiran used a similar classification by dividing operating surgeon into three groups: 1) Consultants, 2) Junior Orthopedic trainee >3years of experience and 3) Orthopedic trainee with <3 years of experience.34
Khan based their study on five registrars performing dynamic hip screw fixation for hip fractures.19 The five registrars were primary operating surgeons in the procedures, each at a different year of training from year one to year three.
Smith33 and Cannon et al.,24 used progressive cases being performed over a set period of time as a method of measuring experience. Smith et al. conducted their study on 100 arthroscopies and based their reasoning of dividing the sample size into 4 groups of 25 scopes each. The first 25 scopes performed by a surgeon would be the inexperienced group as the surgeon would not be proficient enough to perform a new surgery. Eventually as the number of operations being performed by the surgeon increased, his/her experience also increased. Therefore, they named the rest of the groups in accordance with the last group of 25 hip arthroscopies as high experience. Cannon et al. devised a similar method, by comparing surgeries performed early during a period to those performed later during a period. Both studies based their division of surgeon experience on the reasoning of the presence of a learning curve in operations.
Outcomes studied
Our main outcomes of measure were Total Fluoroscopy/Screening time and Radiation Dose Exposure. Different units were used for measuring Radiation Dose in various studies from Gy/cm2 to mSev units. Radiation doses were usually picked up from the dosimeters located on the surgeons lead apron. In a few studies, radiation dose was measured from the dominant hand of the primary surgeon.19,20,22 Two studies additionally reported the number of films/exposures taken.25,32 One study used the number of films with part of surgeon’s body as a measure of radiation exposure.25 This was expressed in terms of percentage of the total number of films.
Quality appraisal of studies
The studies were a mix of retrospective and prospective case series and cohort studies. The revised MINORs criteria were used to grade individual studies based on their methodology. Scores of individual studies are shown in Supplementary Table S2.
Study results
A complete description of outcomes for all studies can be found in Supplementary Table S1.
Total Fluoroscopy time/Screening time
With the exception of four studies,24,27,31,34 all remaining studies reported Total Fluoroscopy time(TFT)/Screening time. Majority of the studies found a longer TFT when surgeries were being performed by a junior inexperienced resident/trainee. However, Bahari et al., Khan et al. and Hafez et al. defined no P-values so a significant conclusion could not be derived in their studies. Bahri et al. show a lower TFT when comparing consultants with senior house officers (SHOs) performing percutaneous wiring in hand and wrist procedures -15.2s (consultants) vs 29.8s (SHOs).20 Similarly, Khan et al. showed a lower TFT of 33s when dynamic hip screws were being performed by a Year III registrar versus a TFT of 62s of a Year I registrar.19 Hafez et al. showed that operating trainees who performed 6 IM nails per month had a longer mean screening time (154.5s±34.37) vs. that of a consultant (65.43±43.36).28 Both Tuohy et al.8 and Eismann25 found no significant between the experience level of the surgeon the amount of radiation exposed with P=0.56 and P=0.28 respectively.
Rashid et al.32 reported a shorted TFT when comparing Consultants (26s) vs Specialist Registrars (36s) (P=0.011) but not when comparing Consultants (26s) with Associate Specialists (32s) (P=0.059).
Radiation dose exposure
With the exception of three studies,20,25,29 all remaining 15 studies reported radiation dose exposure in various units. Majority of the studies found a significant association between a higher surgeon experience level and a lower intraoperative radiation dose/exposure.
Tuohy et al.8 when comparing radiation exposure in hand and wrist surgeries being performed by attending surgeons (3 attending surgeons with following fluoroscopy dose/case – 18,1864 rad/cm2; 10,890rad-cm2 and 13,386 rad-cm2) vs hand surgery fellow (fluoroscopy dose/case of 20,089 rad-cm2) found no statistically significant association (P=0.83). Botchu et al.23 found that there was no significant association when comparing surgeons who had more than 10 years of experience in managing ankle fractures versus those who had less than three years of experience (0.12 Gycm2 vs. 0.19 Gycm2; P=0.10). However, they did show a significant increase in radiation exposure when the same groups performed hip fractures (0.59 Gycm2 vs. 1.62 Gycm2; P=0.005). Madan et al.7 also showed no significant association between surgeon experience and radiation dose when comparing consultant (0.026 mSv) vs. middle grade surgeons (0.049mSv) using fluoroscopy to identify proximal insertion site when managing long bone fractures of the lower limb (P=0.3177).7 Similar non-significance was also found for distal locking site.
Bahari,20 Goldstone27 and Khan et al.19 showed that increased experience decreased radiation exposure however they failed to give any P-values to conclude a statistically significant answer to their question.
Discussion
The necessity to use the mobile C-arm/Fluoroscopy in orthopedic surgeries will always be present. Moreover, with an increase in trauma-related accidents worldwide it can easily be hypothesized that the usage will definitely increase over time. With studies showing that ionizing radiation is a well-established risk factor in the development of adult and childhood cancers,37 both doctors and patients are now concerned about the excessive usage of X-rays during operations. However, since one cannot completely limit the presence of the C-arm in an orthopedic operating room – strategies to minimize its usage to prevent harmful effects of ionizing radiation to operating personnel need to be implemented and monitored. The results from our systematic review show that the more experienced the operating surgeon would be the less he/she would be inclined to using the C-arm regularly and thus have lower screening times with a concurrent lower radiation dose. A possible explanation for this phenomenon could be that at a junior level, majority of trainees are under-confident about their reduction and fixation and thus under peer-pressure and to avoid disappointment from supervising surgeons they resort to excessive screening or procurement of multiple images to ensure adequate reduction and fixation of fracture. Another reason as detailed by Patel et al.,30 was that they found that trainees performed either less common or more complex procedures which accounted for the large difference in exposure/screening times. One way of tackling such a problem would be via strict supervision by more senior surgeons while at the same time allowing a decent hands-on approach to the junior to allow building of technical skill as well as controlling excessive fluoroscopy. The study by Kheiran et al. supports this hypothesis by showing that junior trainees when supervised by a senior person used less radiation then those not supervised.34 A third possible reason is that juniors may lack technical skill; skill that is only developed by performing the procedure repeatedly. A common example is misinterpretation of exact screw sizes which trainees discover after repeated exposures of fluoroscopy. We propose that a very good way of tackling this is to promote the use of cadaveric, anatomic and surgical skills workshops so that trainees and residents can effectively re-hone their surgical skills from time to time. Another important yet plausible reason is that usually more difficult and complex fractures are of the open type, and these are managed by more senior surgeons rather than junior ones. It is well established that Gustilo/Anderson type II and III open fractures can be reduced openly therefore would require less of fluoroscope usage intraoperatively as compared to closed fractures. Since closed fractures are majorly given to junior surgeons to handle, this sort of lends a technical bias or advantage in terms of fluoroscopy time and radiation dose to senior surgeons. However, to reach a more affirmative answer on this question there needs to be a completely randomized trial involving both open and closed fractures to better answer this question.
Introducing radiation usage guidelines in hospitals may be of a benefit to younger surgeons. However, one cannot stop there as research has shown that despite technical radiological training according to guidelines, younger surgeons still tend to ignore specific rules and excessively use the C-arm.21 Younger surgeons also don’t tend to use all measure to prevent radiation exposure such as shielding.38 The best way to tackle is to promote a highly strict approach to following guidelines. It would be an advantage if there is a technical radiographer in the room who can make a reminder of the number of clicks/exposures for the surgeon so that he/she can carefully gauge. Hospitals may consider using a certain limit of number of exposures for residents and surgeons alike. However, careful multicenter prospective studies are needed to define such a limit if present.
Additionally, advancements in technology have allowed the use of cached or saved images which doctors can recall back while fixation to prevent pointless screening of the same site over and over again. Though such technology is present, it tends to be underused by orthopedic surgeons. Juniors should be guided by skilled colleagues through at least 20-30 cases to gain experience with the mobile C-arm before allowing complete independence with its usage.
Often, though radiation dosimeters are present on lead aprons worn by surgeons they are usually attached the either at the waist or on the neck which only measures scatter beams rather than direct beam exposures. Since the extremities of surgeons are more prone to being exposed to direct beam radiations,9,39 we suggest placement of wrist or ring dosimeters to better ascertain for the dose exposure and then correlate it with acceptable threshold guidelines.
Introduction of strict approaches to wearing lead lined aprons, thyroid covers, lead lined eyeglasses and lead lined gloves have been suggested by previous researches to prevent exposure to excessive radiation.40
Studies have shown that certain fracture types require more radiation exposure such as type C fractures of the distal radius.29 Further research involving investigation of fracture types requiring more fluoroscopy can be flagged and guidelines can be developed to have these cases managed by senior surgeons rather than junior ones or at least allow strict supervision by senior surgeons and radiographers to allow adequate and appropriate screening times.
One limitation of this review is that radiation dose measured by studies was not uniform. Some studies measured it on the hand, some at the waist and some from the neck. Since it is well established that waist and neck dosimeters only pick up scatter beam radiations, these would produce dosages that are actually quite low as compared to if the radiation was picked up by the wrist or the ring. Secondly, a lot of institutions do not routinely support the use of ring and wrist dosimeters and introduction of such in researches may have lent a Hawthorne effect where those being studied change their behaviors unconsciously. Clinically it is difficult to double blind this aspect, and the only way uniformity can be established in future researches is buy introducing ring and wrist dosimeters throughout hospitals way before a study can be conducted. Thirdly, none of studies were properly randomized. Though it is a common scenario that immediate urgent cases get handled by whoever is on call (regardless of a senior or a junior) some studies investigating elective non-emergent cases such as those by Eismann involving management of supracondylar fractures25 and Kraus and Touhy for wrist injuries would be flawed in this aspect as senior surgeons tend to take the complex cases leaving easier ones for the junior group thus skewing the primary outcome measures. Fourthly, the total sample size of studies was very small. We propose a large multicenter prospective and randomized trial be conducted for a more definitive conclusion. Finally, the study collated evidence from studies investigating various types of orthopedic procedures with various grades of experience. This is a major limitation of study which has been faced by studies in the past too,36 and is one of the reasons why a meta-analysis was not possible. However, given that the purpose of the study was to collate and review evidence in a systematic manner, the results of the study are still important from a clinical point of view.
Conclusions
Based on this systematic review, we conclude that there is a general trend towards higher surgeon experience significantly associated with reduced usage of the image intensifier and the consequent radiation exposure in orthopedic procedures. However, since it is equally important to train newer orthopedic surgeons, we recommend the introduction of radiation guidelines in Orthopedic training curriculums. In addition, adequate supervision by senior surgeons can also bring about better results while not compromising the training of the junior trainee. Regular use of alarms when total screening time or number of images taken go over the limit can also serve as a useful tool for juniors to manage radiation exposures during surgery.
Funding Statement
Funding: none.
References
- 1.Riley SA. Radiation exposure from fluoroscopy during orthopedic surgical procedures. Clin orthop relat res 1989:257-60. [PubMed] [Google Scholar]
- 2.Singer G. Occupational radiation exposure to the surgeon. J Am Acad Orthop Surg 2005;13:69-76. [DOI] [PubMed] [Google Scholar]
- 3.Radhi AM, Masbah O, Shukur MH, et al. Radiation exposure to operating theatre personnel during fluoroscopic-assisted orthopaedic surgery. Med J Malaysia 2006;61:50-2. [PubMed] [Google Scholar]
- 4.Kaplan DJ, Patel JN, Liporace FA, Yoon RS. Intraoperative radiation safety in orthopaedics: a review of the ALARA (As low as reasonably achievable) principle. Patient Saf Surg 2016;10:27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Picano E, Piccaluga E, Padovani R, et al. Risks Related To Fluoroscopy Radiation Associated With Electrophysiology Procedures. J Atrial Fibrill 2014;7:1044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Devalia KL, Guha A, Devadoss VG. The need to protect the thyroid gland during image intensifier use in orthopaedic procedures. Acta Orthop Belg 2004;70:474-7. [PubMed] [Google Scholar]
- 7.Madan S, Blakeway C. Radiation exposure to surgeon and patient in intramedullary nailing of the lower limb. Injury 2002;33:723-7. [DOI] [PubMed] [Google Scholar]
- 8.Tuohy CJ, Weikert DR, Watson JT, Lee DH. Hand and body radiation exposure with the use of mini C-arm fluoroscopy. J Hand Surg 2011;36:632-8. [DOI] [PubMed] [Google Scholar]
- 9.Mahajan A, Samuel S, Saran AK, et al. Occupational radiation exposure from C arm fluoroscopy during common orthopaedic surgical procedures and its prevention. JCDR 2015;9:RC01-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Int J Surg 2009;8:336-41. [DOI] [PubMed] [Google Scholar]
- 11.Slim K, Nini E, Forestier D, et al. Methodological index for non-randomized studies (minors): development and validation of a new instrument. NZ J Surg 2003;73:712-6. [DOI] [PubMed] [Google Scholar]
- 12.Muller LP, Suffner J, Wenda K, et al. Radiation exposure to the hands and the thyroid of the surgeon during intramedullary nailing. Injury 1998;29:461-8. [DOI] [PubMed] [Google Scholar]
- 13.Tasbas BA, Yagmurlu MF, Bayrakci K, et al. Which one is at risk in intraoperative fluoroscopy? Assistant surgeon or orthopaedic surgeon? Arch Orthop Trauma Surg 2003;123:242-4. [DOI] [PubMed] [Google Scholar]
- 14.Nakahara M, Yasuhara T, Inoue T, et al. Accuracy of Percutaneous Pedicle Screw Insertion Technique with Conventional Dual Fluoroscopy Units and a Retrospective Comparative Study Based on Surgeon Experience. Global Spine J 2016;6:322-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hu X, Lieberman IH. What is the learning curve for robotic-assisted pedicle screw placement in spine surgery? Clin Orthop Relat Res 2014;472:1839-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mehta VM, Paxton EW, Fithian DC. Does the use of fluoroscopy and isometry during anterior cruciate ligament reconstruction affect surgical decision making? Clin J Sport Med 2009;19:46-8. [DOI] [PubMed] [Google Scholar]
- 17.Archibeck MJ, White RE, Learning curve for the two-incision total hip replacement. Clin Orthop Relat Res 2004:232-8. [DOI] [PubMed] [Google Scholar]
- 18.Coetzee JC, van der Merwe EJ. Exposure of surgeons-in-training to radiation during intramedullary fixation of femoral shaft fractures. South Afr Med J 1992;81:312-4. [PubMed] [Google Scholar]
- 19.Khan IA, Kamalasekaran S, Fazal MA. Risk of ionising radiation to trainee orthopaedic surgeons. Acta Orthop Belgica 2012;78:106-10. [PubMed] [Google Scholar]
- 20.Bahari S, Morris S, Broe D, et al. Radiation exposure of the hands and thyroid gland during percutaneous wiring of wrist and hand procedures. Acta Orthop Belgica 2006;72:194-8. [PubMed] [Google Scholar]
- 21.Bar-On E, Weigl DM, Becker T, et al. Intraoperative C-arm radiation affecting factors and reduction by an intervention program. J Pediatr Orthop 2010;30:320-3. [DOI] [PubMed] [Google Scholar]
- 22.Blattert TR, Fill UA, Kunz E, et al. Skill dependence of radiation exposure for the orthopaedic surgeon during interlocking nailing of long-bone shaft fractures: a clinical study. Arch Orthop Trauma Surg 2004;124:659-64. [DOI] [PubMed] [Google Scholar]
- 23.Botchu R, Ravikumar K. Radiation exposure from fluoroscopy during fixation of hip fracture and fracture of ankle: Effect of surgical experience. Indian J Orthop 2008;42:471-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cannon TA, Astur Neto N, Kelly DM, et al. Characterization of radiation exposure in early-onset scoliosis patients treated with the vertical expandable prosthetic titanium rib. J Pediatr Orthop 2014;34:179-84. [DOI] [PubMed] [Google Scholar]
- 25.Eismann EA, Wall EJ, Thomas EC, Little MA. Direct beam radiation exposure to surgeons during pinning of supracondylar humerus fractures: does C-arm position and the attending surgeon matter? J Pediatr Orthop 2014;34:166-71. [DOI] [PubMed] [Google Scholar]
- 26.Giannoudis PV, McGuigan J, Shaw DL. Ionising radiation during internal fixation of extracapsular neck of femur fractures. Injury 1998;29:469-72. [DOI] [PubMed] [Google Scholar]
- 27.Goldstone KE, Wright IH, Cohen B. Radiation exposure to the hands of orthopaedic surgeons during procedures under fluoroscopic X-ray control. Br J Radiol 1993;66:899-901. [DOI] [PubMed] [Google Scholar]
- 28.Hafez MA, Smith RM, Matthews SJ, et al. Radiation exposure to the hands of orthopaedic surgeons: are we underestimating the risk? Arch Orthop Trauma Surg 2005;125:330-5. [DOI] [PubMed] [Google Scholar]
- 29.Kraus M, Röderer G, Max M, et al. Influence of fracture type and surgeon experience on the emission of radiation in distal radius fractures. Arch Orthop Trauma Surg 2013;133:941-6. [DOI] [PubMed] [Google Scholar]
- 30.Patel NG, Mohamed AM, Cooper G, McFadyen I. Ionising radiation exposure in paediatric trauma. Ann Royal Coll Surg Eng 2014;96:190-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Quah C, Mehta R, Shivji FS, et al. The effect of surgical experience on the amount of radiation exposure from fluoroscopy during dynamic hip screw fixation. Ann Royal Coll Surg Eng 2017;99:198-202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Rashid MS, Aziz S, Haydar S, et al. Intra-operative fluoroscopic radiation exposure in orthopaedic trauma theatre. Eur J Orthop Surg 2018;28:9-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Smith KM, Duplantier NL, Crump KH, et al. Fluoroscopy Learning Curve in Hip Arthroscopy-A Single Surgeon’s Experience. Arthroscopy 2017;33:1804-9. [DOI] [PubMed] [Google Scholar]
- 34.Kheiran A, Makki D, Banerjee P, Ricketts D. Intraoperative radiation use by trainees during ankle fracture fixation. Orthopedics 2013;36:e1165-8. [DOI] [PubMed] [Google Scholar]
- 35.Yu E, Khan SN. Does less invasive spine surgery result in increased radiation exposure? A systematic review. Clin Orthop Relat Res 2014;472:1738-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kesavachandran CN, Haamann F, Nienhaus A. Radiation exposure of eyes, thyroid gland and hands in orthopaedic staff: a systematic review. Eur J Med Res 2012;17:28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ron E. Ionizing radiation and cancer risk: evidence from epidemiology. Radiat Res 1998;150:S30-41. [PubMed] [Google Scholar]
- 38.Nugent M, Carmody O, Dudeney S. Radiation safety knowledge and practices among Irish orthopaedic trainees. Irish J Med Sci 2015;184:369-73. [DOI] [PubMed] [Google Scholar]
- 39.Giordano BD, Ryder S, Baumhauer JF, DiGiovanni BF. Exposure to direct and scatter radiation with use of mini-c-arm fluoroscopy. J Bone Joint Surg Am 2007;89:948-52. [DOI] [PubMed] [Google Scholar]
- 40.Narain AS, Hijji FY, Yom KH, et al. Radiation exposure and reduction in the operating room: Perspectives and future directions in spine surgery. Wrld J Orthop 2017;8:524-30. [DOI] [PMC free article] [PubMed] [Google Scholar]


