Abstract
Antecubital pain can be caused by a myriad of pathologies. Abnormalities of the brachialis, in particular, tendinopathy at its insertion, are extremely rare, with no case report in the literature. We report the first case of tendinopathy of the brachialis tendon at its insertion in a 42-year-old male who presented with a year-long history of antecubital pain. The anatomy of the brachialis and the technique for ultrasound-guided steroid injection of the brachialis will also be described.
Keywords: Brachialis, Tendinopathy, Injection, Ultrasound
Introduction
Antecubital pain can be caused by a myriad of pathologies. Abnormalities of the brachialis, in particular, tendinopathy at its insertion, are extremely rare, with no case report in the literature.
We report the first case of tendinopathy of the brachialis tendon at its insertion. The anatomy of the brachialis and the technique for ultrasound-guided steroid injection of the brachialis are also described.
Case report
A 42-year-old normally fit and well male presented with a 1-year history of atypical antecubital pain. There was no significant past medical history. Although he was an active sportsman, regularly lifting weights in the gym, there was no preceding history of trauma, and the onset of antecubital pain was insidious.
Bicipital tendinopathy was initially suspected clinically, and the patient was managed conservatively with physiotherapy and analgesia, without any benefit. Following clinical review by a sports physician, an MRI of the elbow was performed to investigate the cause of the atypical antecubital pain.
Imaging
An MRI of the elbow was performed to evaluate the cause of the patient’s pain. Images were acquired in three planes relative to the transepicondylar axis. Standard sequences included axial and coronal proton density (PD) and PD fat saturated and sagittal T1 sequences. The imaging field of view was between 15 and 20 cm, extending from the distal humerus to the bicipital tuberosity of the radius. A dedicated elbow coil was used. The MRI demonstrated isolated moderate paratendinitis of the deep head of the brachialis tendon at its insertion onto the coronoid process and ulnar tuberosity (Fig. 1). The superficial head was normal in appearance. No full or partial-thickness tear or haematoma was seen in relation to brachialis muscle belly. No bone marrow signal abnormality was demonstrated; in particular, the coronoid process and ulnar tuberosity were normal, with no evidence of stress fracture/response. The biceps tendon was normal, and there was no bicipitoradial bursitis. The remainder of the elbow was normal.
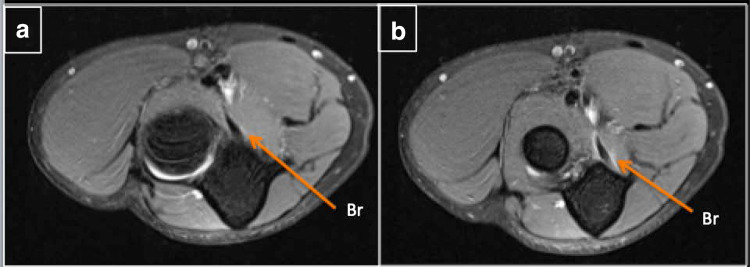
Fig. 1.
Axial PDFS (a and b) demonstrates paratendinitis in relation to the brachialis (Br) tendon at its insertion
Treatment
Ultrasound-guided injection of the tendinopathic brachialis tendon was performed via a medial approach (Fig. 2) with a solution containing 1 mL of 2.5 mg/mL levobupivacaine local anaesthetic (Chirocaine®) and 40 mg of methylprednisolone acetate steroid (Depomedrone®) The patient was advised to avoid heavy lifting/strenuous upper arm gym routines for 1 week, and dedicated physiotherapy was recommended. His symptoms significantly decreased post-injection from a VAS scale of 3–1 over a 2-week period, which was aided by physiotherapy. The patient reported a significant (90%) decrease in symptoms at the 6-week follow up.
Fig. 2.
Transverse image of ultrasound (a and b) demonstrates needle (arrows) with tip adjacent to the tendon of the deep head of the brachialis (brachialis T). Diagrammatic representation of the brachialis (Br) is shown in image (c). Br (brachioradialis), ECRL (extensor carpi radialis longus), ECRB (extensor carpi radialis brevis), PT (pronator teres), FCR (flexor carpi radialis), FDS (flexor digitorum superficialis), FCU (flexor carpi ulnaris), and FDP (flexor digitorum profundus)
Discussion
The antecubital fossa is a triangular space anterior to the elbow joint that forms the transition between the upper arm and forearm. The causes of antecubital pain typically arise from the contents or boundaries of this space, and include pathologies involving the biceps tendon (tendinopathy, bicipitoradial bursitis, and tears), lateral and medial epicondylitis, joint effusion with synovitis, arthropathy, ligamentous injuries, and neuropathies relating to the medial nerve and posterior interosseous nerve. The brachialis muscle forms the floor of the antecubital fossa, and abnormalities involving the brachialis are extremely rare. A total of eight cases of traumatic brachialis injuries involving the muscle and myotendinous junction have been reported in the literature to date [1–8]. There are no previous case reports describing brachialis tendinopathy. This may lead to misdiagnosis of the injury and a delay in treatment.
The brachialis muscle is a major elbow flexor in conjunction with the biceps brachii muscle, and is particularly important in the initiation and continuation of elbow flexion [9]. It comprises two heads—a larger superficial head and smaller deep head. The superficial head arises from the anterolateral aspect of the middle third of the humerus and the lateral intermuscular septum. The deep head arises from the distal third of the humerus and medial intermuscular septum [9]. The distal brachialis insertion onto the proximal ulna is complex and varied [10]. The insertion of the deep head onto the coronoid process and ulnar tuberosity as a tendinous structure is small in comparison to that of the superficial head, which inserts more distally onto the ulnar tuberosity as a broad, fan-shaped musculoaponeurosis [10]. The tendon of the deep head is medial to the superficial head. These two components can be clearly delineated on ultrasound (US) (Fig. 3) and MRI. The musculocutaneous nerve and a branch from the radial nerve innervate the brachialis [11].
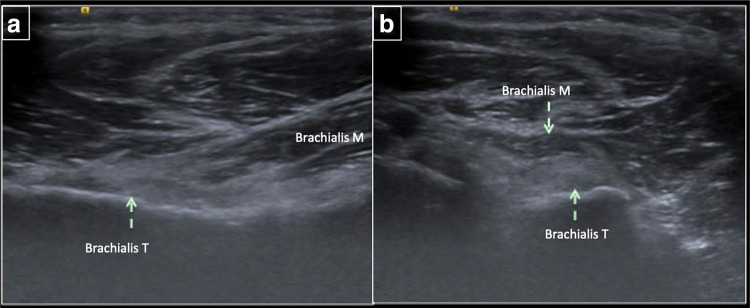
Fig. 3.
Longitudinal (a) and transverse (b) ultrasound images demonstrating the anatomy of the brachialis muscle (Brachialis M) and tendon of the deep head of the brachialis (Brachialis T) in a normal patient
Tendinopathy is a common pathology, but its exact prevalence is difficult to ascertain. Hopkins and co-workers reported the prevalence of tendinopathies of several joints, but none involves the brachialis [12]. Tendinopathy may affect normal daily activities, and can contribute to work absence and loss of productivity [12]. An accurate and timely diagnosis is vital to allow appropriate management to be instigated. Although US is commonly used to identify tendinopathy at other locations in the body, assessment of the brachialis tendon can be challenging using this modality owing to the location of the brachialis tendon deep under the pronator teres. The pronator teres muscle can be hypertrophied in young, fit patients, which can limit visualisation and assessment of the brachialis tendon. Therefore, MRI is a more reliable imaging technique in diagnosing brachialis tendinopathy.
Biceps tendinopathy and bicipitoradial bursitis are the most common causes of antecubital pain. However, as part of the evaluation of the anterior part of the elbow, the brachialis should be assessed. Paratendinitis of the brachialis, as seen in our case, is an uncommon cause of antecubital pain.
In this case, ultrasound-guided injection of the tendinous portion (deep head) resulted in a significant decrease in symptoms. This was performed under ultrasound guidance by first identifying the biceps tendon at the elbow in the axial plane. The muscle underneath this is the brachialis, which is seen as bulky muscular structure and hyperechoic tendon in its deeper portion. The lateral part of this tendon is the superficial head, and the medial portion is the deep head of the brachialis. Following aseptic technique, a needle was inserted through the pronator teres muscle belly and into the brachialis, stopping just proximal to the tendon of the brachialis, where steroid and local anaesthetic were injected. US-guided steroid injection of the deep head (tendinous portion) was effective in treating our patient and should be considered in patients with brachialis tendinopathy.
Conclusion
Brachialis tendinopathy and/or paratendinitis should be considered in the differential diagnosis for the antecubital fossa, and should be evaluated with axial fat-suppressed MRI. Recognition of this pathology can allow ultrasound-guided injection to be performed for therapeutic purposes.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures in studies involving human participants were in accordance with ethical standard of the institutional and /or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Schönberger TJ, Ernst MF. A brachialis muscle rupture diagnosed by ultrasound; case report. Int J Emerg Med. 2011;4(1):46. doi: 10.1186/1865-1380-4-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Winblad JB, Escobedo E, Hunter JC. Brachialis muscle rupture and hematoma. Radiol Case Rep. 2015;3(4):251. doi: 10.2484/rcr.v3i4.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sharma P, Mehta N, Narayan A. Isolated traumatic brachialis muscle tear: a case report and review of literature. Bull Emerg Trauma. 2017;5(4):307–310. doi: 10.18869/acadpub.beat.5.4.476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Van den Berghe GR, Queenan JF. Isolated rupture of the brachialis: a case report. J Bone Joint Surg Am. 2001;83-A:1074–1075. doi: 10.2106/00004623-200107000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Nishida Y, Tsukushi S. Brachialis muscle tear mimicking an intramuscular tumor: a report of two cases. J Hand Surg Am. 2007;32:1237–1241. doi: 10.1016/j.jhsa.2007.06.002. [DOI] [PubMed] [Google Scholar]
- 6.Wasserstein D, White L. Traumatic brachialis muscle injury by elbow hyperextension in a professional hockey player. Clin J Sport Med. 2010;20:211–212. doi: 10.1097/JSM.0b013e3181df1ed4. [DOI] [PubMed] [Google Scholar]
- 7.Murugappan KS, Mohammed K. Acute traumatic brachialis rupture in a young rugby player: a case report. J Shoulder Elbow Surg. 2012;21:e12–e14. doi: 10.1016/j.jse.2011.10.009. [DOI] [PubMed] [Google Scholar]
- 8.Krych AJ, Kohen RB, Rodeo SA, Barnes RP, Warren RF, Hotchkiss RN. Acute brachialis muscle rupture caused by closed elbow dislocation in a professional American football player. J Shoulder Elbow Surg. 2012;21(7):e1–e5. doi: 10.1016/j.jse.2011.11.007. [DOI] [PubMed] [Google Scholar]
- 9.Leonello DT, Galley IJ, Bain GI, Carter CD. Brachialis muscle anatomy: a study in cadavers. J Bone Joint Surg Am. 2007;89:1293–1297. doi: 10.2106/00004623-200706000-00018. [DOI] [PubMed] [Google Scholar]
- 10.Sanal HT, Chen L, Negrao P, Haghighi P, Trudell DJ, Resnick DL. Distal attachment of the brachialis muscle: anatomic and MRI Study in Cadavers. Am J Roentgenol. 2009;192(2):468–472. doi: 10.2214/AJR.08.1150. [DOI] [PubMed] [Google Scholar]
- 11.Tagliafico A, Michaud J, Perez MM, Martinoli C. Ultrasound of distal brachialis tendon attachment: normal and abnormal findings. Br J Radiol. 2013;86(1025):20130004. doi: 10.1259/bjr.20130004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Hopkins C, Fu SC, Chua E, Hu X, Rolf C, Mattila VM, Qin L, Yung PS, Chan KM. Critical review on the socio-economic impact of tendinopathy. Asia Pac J Sports Med Arthrosc Rehabil Technol. 2016;22(4):9–20. doi: 10.1016/j.asmart.2016.01.002. [DOI] [PMC free article] [PubMed] [Google Scholar]