Abstract
Controversy exists regarding whether doctors who perform abortions should be required to hold hospital admitting privileges, but no research exists as to the extent to which they actually hold and use such privileges. Extensive Internet and government data sources were used to identify and verify abortionists in Florida. All medical and osteopathic abortion doctors who were licensed to practice at any time during the period 2011 to 2016 were included in the study (n = 85). Every abortionist hospital admission of a female patient aged 15 to 44 occurring during the 6-year study period was identified (n = 21 502). Abortionist physicians are 74.1% male, 62% have been in practice for 30 years or longer, 27.1% are graduates of foreign medical schools, and 55.3% are board certified. Nearly half (48.2%) of the abortionists had at least 1 malpractice claim, public complaint, disciplinary action, or criminal charge. Half (50.6%) of the abortionists reported hospital privileges, but only 32 (37.6%) admitted at least 1 patient to a hospital. Seven physicians accounted for 68.2% of all the admissions, and 79.6% of all admissions were related to a live birth. Black was the modal race (47.6%) and Medicaid the most frequent (64.9%) pay source. Nearly one-fifth (19.4%) of admissions came through the emergency department. Physicians who hold hospital privileges are significantly (P < .05) more likely to be board certified and to be approved for Medicaid payment than their colleagues without privileges. Of those doctors who hold and use hospital privileges, the lowest admission volume physicians are significantly less likely to be involved in live births, more likely to admit commercially insured and white inpatients, and much more likely to use the emergency room as the route to hospital admissions for their Medicaid-eligible and black patients. Further study of abortionist physicians is indicated regarding their heterogeneous personal and professional characteristics; their career pathways and practice concentrations; their relative integration with or isolation from peers and the professional network; the importance of black and poor induced abortion patients in their total caseload; and, especially for abortionists without hospital privileges, the means by which their patients requiring emergency care and hospitalization are accommodated.
Keywords: hospital privileges, abortionist physicians, emergency room admissions, racial disparities, emergency visits
Introduction
Hospital Privileges, Abortion, and the Need for Research
Within the past few years, a number of state laws were enacted which required that physicians who provide abortions have admitting privileges at a hospital within 30 miles of the location of abortion. The justification offered by proponents of this legislation was that it would reduce the risk factor for patients who had potentially deadly complications during or after an abortion by expediting their emergency treatment and admission, if necessary, at a hospital. Opponents of these state laws argued, by contrast, that admitting privileges were medically unjustified largely based upon the opinion that abortion was a relatively safe procedure and that adverse events requiring a hospital admission or emergency department (ED) visit were rare.1,2 From a research perspective, it is clear that findings concerning the incidence and outcomes of abortion complications remain inconclusive, largely because of the demonstrably inadequate systems of abortion certification and reporting in the United States.3 Research from Finland and Denmark, countries with comprehensive systems for reporting abortions and other pregnancy outcomes, concluded that there is a 4 times greater risk of mortality following abortion than childbirth.4,5 These findings contrast with the often-referenced conclusion that childbirth-related mortality is 14 times that of abortion.6
Similarly, no research exists on the comparative outcomes of women who experience complications of an induced abortion performed by providers with and without hospital admitting privileges. More fundamentally, there has been no research at all on the extent to which abortionists actually hold and use hospital privileges. In particular, the question of whether and how often abortion doctors utilize the ED as a pathway to hospital admission is relevant to the legal issue of requiring privileges for abortionists.
The objectives of this analysis, therefore, were to describe the characteristics of physicians who perform induced abortions and to describe the extent to which they hold and use hospital admitting privileges, with an emphasis on the involvement of the ED in the admission. Specific foci of the analyses were on the differences in physicians with and without privileges and the differences in patient and practice characteristics associated with the volume of hospital admissions accounted for by each doctor. In a domain with literally no preceding research, this analysis was intended to explore and formulate important research questions and to inform the design and data needs of future hypothesis testing studies.
There is a broad professional consensus that the process of credentialing and hospital privileging for physicians enhances their competency and the quality of care rendered to patients. Hospital admitting privileges are obviously essential for surgeons who require the necessary technology, personnel, and support services found in the inpatient setting to practice their specialty. Many insurance companies require that a physician hold admitting privileges as a condition of participation in their provider networks.7 The benefits of obtaining hospital privileges do not, however, accrue only to those physicians who practice exclusively within the inpatient setting. The American College of Surgeons and the American Medical Association produced 10 core principles for patient safety for office-based surgery and practice. The principles were approved by more than 3 dozen interested parties including the major accrediting organizations for ambulatory and office-based surgery (Joint Commission on the Accreditation of Healthcare Organization, Accreditation Association for Ambulatory Health Care, Inc, American Association for Accreditation of Ambulatory Surgical Facilities, Inc); surgical and medical specialty societies, including the American College of Obstetricians and Gynecologists and the American Society for Reproductive Medicine; and various state medical associations (Massachusetts, New York, Kansas, Indiana, and Missouri). Two of the 10 core principles relate directly to the process of securing and maintaining hospital admitting privileges. Core principle No. 4 states that “physicians performing office based surgery must have admitting privileges at a nearby hospital…or a transfer agreement with another physician who has admitting privileges at a nearby hospital.” Core principle No. 8 states that “a physician may show competency by maintaining core privileges at an accredited licensed hospital or ambulatory surgery center.”8 Finally, it is clear that hospital privileges are valued and sought in some form not only by physician–surgeons but also by nonsurgical primary care physician–practitioners such as family practice doctors, and even by nonphysician practitioners such as psychologists, optometrists, nurse-midwives, and others.9-11 Hospital privileges also provide an opportunity for physicians to gain access to important diagnostic and treatment technology as well as a diverse network of provider specialists, which should enable each privileged physician to play a more complete and integrated role in optimizing the care delivered to each patient.
Methods
Abortion Physician Identification, Verification, and Inclusion Process
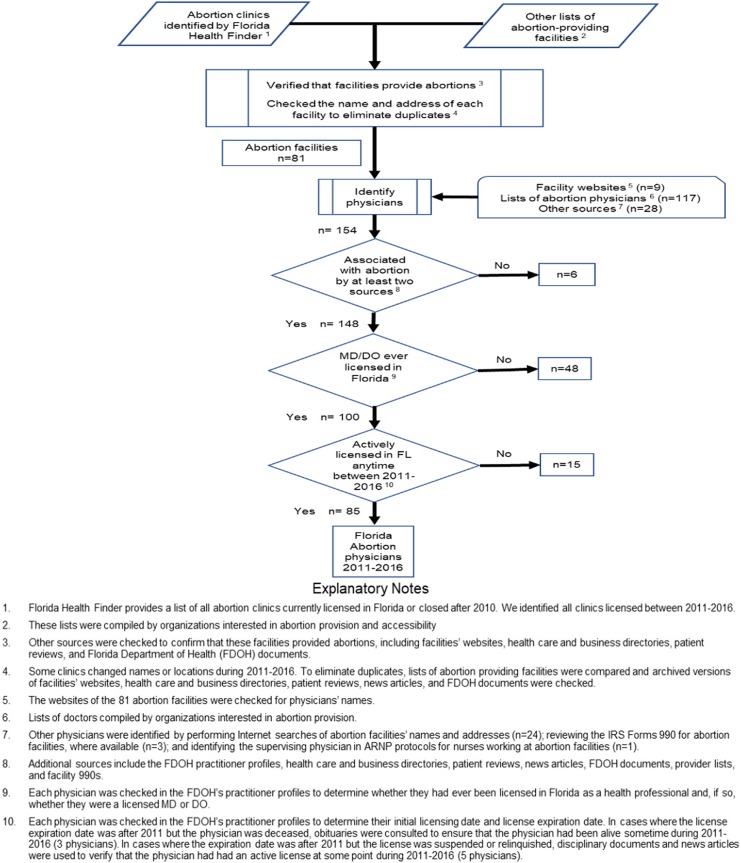
Abortionist physicians licensed in Florida between 2011 and 2016 were selected for the study using a 3-step process (Figure 1). First, a complete list of Florida abortion facilities was compiled using lists published by the Florida Department of Health (FDoH) and organizations interested in abortion provision. Second, the websites of these facilities were checked for physician names and Internet searches were performed to find physicians associated with the facilities. Third, each physician was associated with abortion by at least 2 different sources and then each physician’s FDoH practitioner profile was checked to ensure that he or she was a medical doctor or osteopathic physician who was licensed in Florida between 2011 and 2016. Physicians who self-identified as board certified by the American Board of Obstetricians and Gynecologists (ABOG) were validated by the ABOG Diplomate Verification Search System.
Figure 1.
Identifying and validating abortionist physicians in Florida.
The Florida Practitioner Profile
The primary source of physician characteristics for this analysis is the Florida Practitioner Profile (FPP), maintained by the Division of Medical Quality Assurance. Required by law since 1997, all medical doctors; osteopathic, chiropractic, and podiatric physicians; and licensed advanced registered nurse practitioners must report their profiles. Data elements residing in the FPP include practice address; participation in Medicaid; hospitals and other provider facilities at which the doctor holds privileges; other state licensures; year licensed in any jurisdiction; education and training, including postgraduate and professional (including dates); specialty certification; and proceedings and actions such as medical sanctions and termination, criminal offenses, and disciplinary actions undertaken against them by various organizations.
Florida Agency for Health Care Administration State Inpatient Database
The state inpatient database (SID) contains more than 100 clinical and nonclinical variables, such as principal and secondary diagnoses and procedures, admission and discharge status, patient demographic characteristics (eg, gender and race), expected payment sources, length of stay, and total charges. The FPP and SID are linkable via the physicians’ licensure numbers.
We identified every patient discharge from Florida hospitals for women aged 15 to 44, for the years 2011 to 2016, attributable to any of our identified physicians. For each admission, we identified the Medicare Severity Diagnosis-Related Group (MSDRG), whether the admission had occurred through the ED, and the race and pay source of the patient. Abortion doctors were also segmented into high-, medium-, and low-volume groups based upon their total number of admissions.
We used Pearson (2×2) χ2 statistic to test the significance of differences in the characteristics of physicians with and without hospital privileges. Similarly, we used the χ2 test of independence for assessing significant differences between the 3 admission volume determined physician groups (2×3) for the racial, pay source, ED involvement, and clinical composition of their inpatients. Significance was at the P < .05 level for all tests.
Findings
Physician Characteristics
Table 1 summarizes selected demographic and practice characteristics of the Florida abortionists identified in the sample. The 85 physicians are divided into those with (43, 50.6%) and without (42, 49.4%) hospital admitting privileges. Most abortionist physicians are men (63, 74.1%). Nearly 62% (n = 52) of the physicians have been in practice for more than 30 years. Twenty-three (27.1%) of the abortionists are foreign medical school graduates. The foreign medical schools represented were located in the following nations and territories: Belgium, Canada, Cayman Islands, Chile, Dominica, Germany, Grenada, Italy, Iran, India, Nicaragua, Philippines, Puerto Rico, Romania, Russia, Spain, and Thailand. Physicians with hospital privileges are significantly (P < .05) more likely to be board certified (χ2 = 5.195, P = .22652) and to be approved for Medicaid payment (χ2 = 11.693, P = .00627). Nearly half of the physicians (n = 41, 48.2%) had at least 1 malpractice claim, disciplinary action, public complaint, or criminal charge lodged against them.
Table 1.
Characteristics of Abortionist Physicians, n (%).
| Characteristic | Total, n (%) | With Privileges | Without Privileges | P Value |
|---|---|---|---|---|
| Total, n (%) | 85 (100) | 43 (50.6) | 42 (49.4) | |
| Sex | ||||
| Female | 22 (25.9) | 9 (20.9) | 13 (31.0) | .2907 |
| Male | 63 (74.1) | 34 (79.1) | 29 (69.0) | |
| Board certification | ||||
| Yes | 47 (55.3) | 29 (67.4) | 18 (42.9) | .0226a |
| No | 38 (44.7) | 14 (32.6) | 24 (57.1) | |
| Years in practiceb,c | ||||
| <10 | 2 (2.35) | 0 | 2 (4.76) | .0552 |
| 10-19 | 17 (20.0) | 12 (27.9) | 5 (11.9) | |
| 20-29 | 14 (16.5) | 9 (20.9) | 5 (11.9) | |
| 30-39 | 31 (36.5) | 15 (34.9) | 16 (38.1) | |
| 40-49 | 15 (17.6) | 6 (14.0) | 9 (21.4) | |
| ≥50 | 6 (7.06) | 1 (2.33) | 5 (11.9) | |
| Medical school | ||||
| International | 23 (27.1) | 12 (27.9) | 11 (26.2) | .8608 |
| Domestic | 62 (72.9) | 31 (72.1) | 31 (73.8) | |
| Accepts Medicaid | ||||
| Yes | 36 (42.4) | 26 (60.5) | 10 (23.8) | .0007a |
| No | 49 (57.6) | 17 (39.5) | 32 (76.2) | |
| Sanctionsd | ||||
| None | 44 (51.8) | 20 (46.5) | 24 (57.1) | .3310 |
| ≥1 | 41 (48.2) | 23 (53.5) | 18 (42.9) | |
aSignificant at P < .05.
bIf year practice began not specified by physician, default was year issued followed by year graduated from residency.
cSignificance tested difference between ≤29 years practice versus ≥30 years.
dSanctions include malpractice, disciplinary action, public complaint, or criminal charge(s).
Admission Volume
Between 2011 and 2016, 32 (37.6%) of the Florida abortionist physicians had at least a single inpatient hospital admission of a woman aged 15 to 44 for any reason. In total, they were involved in 21 502 admissions. The distribution of the admissions by physician volume is highly skewed, and physicians were allocated into 3 groups based on admission volume. Group 1 (high volume) was composed of 7 physicians who each accounted for 1019 to 4366 admissions over the 6-year period, representing 14 665 admissions or 68.2% of the total, averaging 349 admissions per doctor per year. Group 2 (medium volume) was composed of 8 physicians who each accounted for 430 to 881 admissions, representing 5799 admissions or 27.0% of the total, averaging 121 admissions per doctor per year. Group 3 (low volume) was composed of 17 physicians who each accounted for 1 to 288 admissions, representing 1038 admissions or 4.8% of the total, averaging 10 admissions per doctor per year.
Admissions by DRG
Admissions involving vaginal or cesarean deliveries, both with and without complicating diagnoses, account for 17 127 (79.6%) of total admissions. 1082 (5.0%) of the admissions involve surgical repair of the uterus and adnexa (fallopian tubes, ovaries) for various nonmalignant conditions both with and without complicating diagnosis. A total of 1081 (5.0%) of the admissions involve medical management of other antepartum diagnoses both with and without medical complications. Another 887 (4.1%) admissions involve abortions with and without dilation and curettage, postabortion diagnosis with and without an operating room procedure, and threatened abortion. Only 21 MSDRG categories account for nearly 97% of all admissions, with the remaining 3% of admissions distributed among nearly 300 MSDRG groups (Table 2).
Table 2.
Total Inpatient Admissions (2011-2016) by Abortionist Physicians, by MSDRG.
| MSDRG | Admissions | Description (%) | Cumulative (%) |
|---|---|---|---|
| 775 | 8762 | Vaginal delivery without complicating diagnoses (40.75) | 40.75 |
| 766 | 4697 | Cesarean delivery without CC/MCC (21.84) | 62.59 |
| 765 | 2432 | Cesarean delivery with CC/MCC (11.31) | 73.90 |
| 774 | 1005 | Vaginal delivery with complicating diagnoses (4.67) | 78.58 |
| 743 | 864 | Uterine and adnexa procedure for nonmalignancy without CC/MCC (4.02) | 82.60 |
| 781 | 816 | Other antepartum diagnoses with medical complications (3.79) | 86.39 |
| 782 | 265 | Other antepartum diagnoses without medical complications (1.23) | 87.62 |
| 777 | 261 | Ectopic pregnancy (1.21) | 88.84 |
| 778 | 255 | Threatened abortion (1.19) | 90.02 |
| 767 | 223 | Vaginal delivery with sterilization and/or D&C (1.04) | 91.06 |
| 770 | 221 | Abortion with D&C, aspiration curettage or hysterotomy (1.03) | 92.09 |
| 742 | 218 | Uterine and adnexa procedure for nonmalignancy with CC/MCC (1.01) | 93.10 |
| 779 | 218 | Abortion without D&C (1.01) | 94.12 |
| 776 | 161 | Postpartum and postabortion diagnoses without OR procedure (0.75) | 94.87 |
| 812 | 83 | Red blood cell disorders without MCC (0.39) | 95.25 |
| 761 | 77 | Menstrual and other female reproductive system disorders without CC/MCC (0.36) | 95.61 |
| 759 | 67 | Infections, female reproductive system without CC/MCC (0.31) | 95.92 |
| 392 | 46 | Esophagitis, gastroenteritis, and miscellaneous digest disorders without MCC (0.21) | 96.14 |
| 745 | 38 | D&C, conization, laparoscopy, and tubal interruption without CC/MCC (0.18) | 96.31 |
| 780 | 32 | False labor (0.15) | 96.46 |
| 769 | 32 | Postpartum and postabortion diagnoses with OR procedure (0.15) | 96.61 |
| All other | 729 | All other (3.39) | 100.00 |
| Grand total | 21 502 |
Abbreviations: CC, complication or comorbidity; D&C, dilation and curettage; MCC, major complication or comorbidity; MSDRG, Medicare Severity Diagnosis-Related Group; OR, operating room.
Volume group differences in the composition of admissions by DRG are apparent (Table 3). Increasing volume is associated with a higher percentage of admissions associated with live births by vaginal or cesarean deliveries. Births comprise 83.5% of the high-volume doctor admissions, but only 48.2% for the low-volume group (χ2 = 837.0343, P = <.00001). By contrast, uterine procedures for nonmalignant conditions are more than one-fourth (27.0%) of low-volume doctor admissions, but only 3.4% for the high-volume group (χ2 = 1127.7516, P < .00001). Differences in the number of abortion-related admissions between the groups are not significant. High-volume group admissions are concentrated in a small number of DRGs compared to a dispersed pattern of a larger number of low incidence DRGs among the medium- and low-volume doctors.
Table 3.
Total Inpatient Admissions by Physician Volume Groups, by DRGs.
| DRGs | Combined Description | Admissions (%) | P Value | ||
|---|---|---|---|---|---|
| High | Medium | Low | |||
| 765, 766, 767, 768, 774, 775 | Vaginal and cesarean section deliveries with and without complicating comorbidities or conditions | 12 257 (83.6) | 4369 (75.3) | 501 (48.3) | <.00001a |
| 742, 743 | Uterine and adnexa procedures for nonmalignancy, with and without complicating comorbidities or conditions | 499 (3.4) | 303 (5.2) | 280 (27.0) | <.00001a |
| 781, 782 | Other antepartum diagnoses with and without medical complications | 821 (5.6) | 190 (3.3) | 70 (6.7) | <.00001a |
| 769, 770, 776, 777, 778, 779 | Abortions with and without dilation and curettage; postpartum and postabortion diagnoses with and without an OR procedure; threatened abortion; ectopic pregnancy | 778 (5.3) | 303 (5.2) | 67 (6.4) | .25424 |
| All other DRGs | 310 (2.1) | 634 (11.0) | 120 (11.6) | ||
| Total | 14 665 | 5799 | 1038 | ||
Abbreviations: DRG, Diagnosis-Related Group; OR, operating room.
aSignificant P < .05.
Admissions Involving a Live Birth
Only 24 (28.2%) of the 85 physicians who perform abortions had 1 or more hospital admissions involving a live birth in the 6-year study period. Of the total 17 127 birth-related admissions, 2006 (11.7%) came through the ED. The top 5 doctors by birth volume accounted for 10 334 (60.3%) births. A single physician admitted nearly half (49.2%) of the births that came via ED, and only 5 doctors accounted for 1673 (83.4%) of total ED birth admissions. Ten doctors averaged 10 or more births per month, considered as a normal obstetrical case load. Five physicians averaged between 2 and 10 births per month, and 9 doctors averaged fewer than 2 births per month (Table 4).
Table 4.
Birth-Related Inpatient Admissions (2011-2016) by Abortionist Physician, ED/Non-ED, Per Month.
| Physician # | Non-ED | ED (%) | Total | Per Month |
|---|---|---|---|---|
| 1 | 3394 | 162 (4.5) | 3556 | 49.4 |
| 2 | 2168 | 67 (3.0) | 2235 | 31.0 |
| 3 | 1419 | 78 (5.3) | 1477 | 20.5 |
| 4 | 1349 | 128 (8.6) | 1477 | 20.5 |
| 5 | 946 | 1 (0.001) | 947 | 13.1 |
| 6 | 788 | 168 (17.6) | 956 | 13.2 |
| 7 | 783 | 2 (0.002) | 785 | 10.9 |
| 8 | 743 | 1 (0.001) | 744 | 10.3 |
| 9 | 647 | 46 (6.6) | 693 | 9.6 |
| 10 | 601 | 988 (62.2) | 1589 | 22.0 |
| 11 | 591 | 227 (27.7) | 818 | 11.4 |
| 12 | 460 | 0 | 460 | 6.4 |
| 13 | 446 | 3 (0.006) | 449 | 6.2 |
| 14 | 420 | 0 | 420 | 5.8 |
| 15 | 113 | 73 (39.2) | 186 | 2.6 |
| 16 | 72 | 0 | 72 | 1.0 |
| 17 | 51 | 30 (37.0) | 81 | 1.10 |
| 18 | 53 | 32 (37.6) | 85 | 1.20 |
| 19 | 40 | 0 | 40 | 0.50 |
| 20 | 14 | 0 | 14 | 0.19 |
| 21 | 10 | 0 | 10 | 0.14 |
| 22 | 5 | 0 | 5 | 0.07 |
| 23 | 4 | 0 | 4 | 0.05 |
| 24 | 4 | 0 | 4 | 0.05 |
| Total | 15 121 | 2006 (11.7) | 17 127 | 9.91 |
Abbreviation: ED, emergency department.
Total Admissions by Race, Pay Source, and ED Use
Of the 21 502 total admissions, 4171 (19.4%) were admitted through the ED and 17 331 (80.6%) through the normal admitting process. The distribution of admissions by pay source was Medicaid 13 955 (64.9%), commercial 5478 (25.5%), other 1804 (8.4%), and Medicare 267 (1.2%). By race, the discharges were black 10 237 (47.6%), white 8182 (38.1%), and other 3083 (14.3%). Admissions which were both black and Medicaid numbered 7591 (35.3%), of which 1632 (21.5%) were admitted through the ED (Table 5).
Table 5.
Total Inpatient Admissions (2011-2016) by Abortionist Physicians, by Race, Pay Source, and ED/Non-ED.
| Pay Source | Black | White | Other | Total (%) |
|---|---|---|---|---|
| Emergency room | ||||
| Commercial | 375 | 403 | 75 | 853 (20.4) |
| Medicaid | 1632 | 702 | 314 | 2648 (63.5) |
| Medicare | 51 | 41 | 3 | 95 (2.3) |
| Other | 270 | 237 | 68 | 575 (13.8) |
| Total (%) | 2328 (55.8) | 1383 (33.2) | 460 (11.0) | 4171 (19.4) |
| Nonemergency room | ||||
| Commercial | 1443 | 2512 | 668 | 4623 (26.7) |
| Medicaid | 5959 | 3577 | 1771 | 11 307 (65.2) |
| Medicare | 104 | 58 | 10 | 172 (<1.0) |
| Other | 403 | 652 | 174 | 1229 (7.1) |
| Total (%) | 7909 (45.6) | 6799 (39.2) | 2623 (15.2) | 17 331 (80.6) |
Abbreviation: ED, emergency department.
Volume Group–Specific Admissions
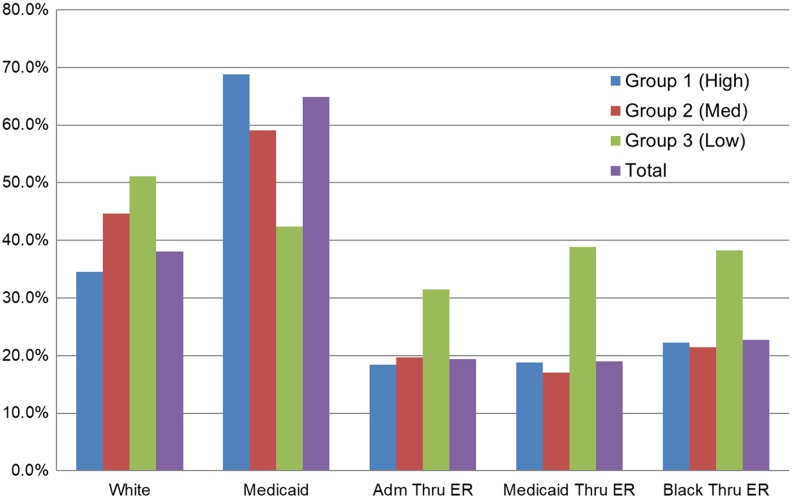
Within-group admissions through the ED were as follows: group 1: 2703 (18.4%); group 2: 1141 (19.7%); and group 3: 327 (31.5%; χ2 = 106.3229, P = <.00001; Figure 2).
Figure 2.
By volume group, white, Medicaid, and ED admissions. ED indicates emergency department.
Within-group admissions by pay source were as follows: Medicaid—group 1: 10 089 (68.8%); group 2: 3426 (59.1%); and group 3: 440 (42.4%; χ2 = 414.899, P = <.00001). Commercial—group 1: 3463 (23.6%); group 2: 1602 (27.6%); and group 3: 411 (39.6%; χ2 = 149.9167, P = <.00001). Other—group 1: 983 (6.7%); group 2: 660 (11.4%); and group 3: 161 (15.5%; χ2 = 190.2832, P = <.00001). Medicare—group 1: 130 (.90%); group 2: 111 (1.9%); and group 3: 26 (2.5%; χ2 = 49.9764, P = <.00001).
Within-group discharges by race were as follows: black—group 1: 7449 (50.8%); group 2: 2359 (40.6%); and group 3: 429 (41.3%); white—group 1: 5061 (34.5%); group 2: 2590 (44.8%); and group 3: 531 (51.2%); other—group 1: 2155 (14.7%); group 2: 850 (14.6%); and group 3: 78 (7.5%; χ2 = 295.5377, P = <.00001).
Medicaid and the ED
Of the total of 13 955 Medicaid discharges, 2648 (18.9%) were admitted through the ED. At the group level, the number and percentage of Medicaid admissions through the ED were as follows: group 1: 1892 (18.7%); group 2: 585 (17.1%); and group 3: 171 (38.9%; χ2 = 121.5676, P = <.00001).
Black Race and the ED
Of the total of 10 237 black admissions, 2328 (22.7%) were admitted through the ED. At the group level, the number and percentage of black admissions through the ED were as follows: group 1: 1658 (22.2%); group 2: 506 (21.4%); and group 3: 164 (38.2%; χ2 = 61.7952, P = <.00001).
Overall, admissions from doctors who do abortions are most likely to be Medicaid-eligible and black. Admissions of black Medicaid patients were more than one-third of the total. Admissions from the low-volume group of doctors were less likely to be black or Medicaid-eligible than the higher volume groups, but much more likely to flow through the ED.
Discussion
The profile of Florida abortionist characteristics and the findings related to their holding of hospital admitting privileges and subsequent utilization of the hospital raise questions of consequential public policy importance. This group of abortionists is relatively senior, is predominantly composed of doctors who have been in practice for more than 30 years, and is disproportionally male. Some anecdotal literature suggests that there may be barriers to abortion practice for early career doctors and that doctors who choose to do abortions often try to keep knowledge of this activity from their professional colleagues. The relatively advanced age distribution and large percentage of abortionists with some malpractice claim, disciplinary action, public complaint, or criminal charge suggest that these doctors may be a subset of practicing physicians for whom abortion practice may be a final professional expedient. A little more than half of the group is board certified, more than one-fourth are foreign trained, and less than half admit patients to the hospital. At the same time, we find a number of board-certified obstetricians with apparently high-volume delivery practices among the group. The obvious conclusion is that abortionists are heterogeneous in terms of both personal and practice characteristics.
Only 43 of the 85 abortionists held privileges and, of those with privileges, only 32 had at least a single admission during the entire 6-year study period. A few of the doctors used the hospital extensively, those being board-certified obstetricians. The overwhelming number of admissions among this small group was for deliveries. The extent to which abortion doctors are also involved in delivering babies is of considerable research interest. The typical abortionist uses the hospital infrequently. Since only a very small fraction of induced abortions occur in an inpatient setting, it seems plausible to conclude that most abortionists concentrate on outpatient abortions and practice very little medical care that is related to other illnesses and injuries, which frequently result in the need for an inpatient hospitalization.
Since volume is associated with positive outcomes across a broad array of health services, the volumes and types of induced abortions performed by each physician and their pattern of adverse outcomes (eg, complications resulting in an ED visit) are of vital interest. An analysis of physician abortion volume and inpatient admission volume, controlling for important physician characteristics (eg, board certification), would provide insight into a profile of quality determinants for abortion-related care.
Despite the relatively sparse use of the hospital, nearly one-fifth (19.9%) of the admissions come from a visit to the ED, and this percentage is nearly 40% for black and Medicaid admissions from the lowest volume doctors. Inpatient admissions through the ED are expedited if the patient is under the care of a physician who is a frequent admitter to whom the inpatient admission can be assigned. This finding also supports the conclusion that doctors who do abortions are, in fact, involved in the care of patients whose illness or condition often requires an ED visit which frequently results in an admission. Further, abortionists who use the hospital the least are proportionally more likely to use the ED as a path to admission. For hospitalizations resulting from complications of an induced abortion performed in an ambulatory setting, whether and where the abortionist holds admitting privileges is likely an important explanatory factor in the conduct and ultimate outcome of the process of care. With the ED admission as such a prominent occurrence for the Florida abortionist with hospital privileges, what is the experience of those patients who require an ED admission but whose doctor lacks privileges?
Finally, the disproportionate racial (black) and pay source (Medicaid) characteristics of abortionist inpatients confirm what is known about the large and long-standing racial disparity in abortion in the United States. In the period between 1990 and 2014, in states that reported race-specific abortion data to the Centers for Disease Control and Prevention, the black abortion rate was 3.4 times the white rate.12 The fact that inpatient admissions from abortionist physicians are also disproportionally black and poor should stimulate further research on this understudied population.
Studies of doctors who perform abortions are absent from the peer-reviewed literature. How and why a physician becomes an abortionist are largely unexplored questions. Similarly, the extent to which these physicians are integrated with or isolated from the typical processes and communication networks of medical care, including the patient hospitalization event, is largely unknown and unexplained. A fundamental question made explicit but unanswered by this exploratory analysis is how many doctors restrict their practice exclusively to abortion. A major barrier to advancing this domain of science continues to be the lack of a universal and comprehensive reporting requirement for all induced abortions and the health-care professionals who perform them. Valid hypothesis testing analyses of these important research questions will require statistically representative samples of physicians and patients derived from such a comprehensive surveillance system.
Author Biographies
James Studnicki is currently vice president and director of data analytics at the Charlotte Lozier Institute in Arlington, Virginia. Over a span of four decades, he held academic appointments at the Johns Hopkins University School of Hygiene and Public Health, the University of South Florida College of Public Health, and the University of North Carolina, Charlotte, where for ten years he served as the Irwin Belk Endowed Chair in Health Services Research. Studnicki holds Doctor of Science (ScD) and Master of Public Health (MPH) degrees from Johns Hopkins and a Master of Business Administration (MBA) from the George Washington University.
Tessa Longbons is a research associate with the Charlotte Lozier Institute. Her research focuses on abortion statistics at the state and national levels and the changing landscape of abortion policy, provision, and access in the United States. She received her BA from Thomas Edison State University.
John W. Fisher is currently an associate Scholar at the Charlotte Lozier Institute. Following a 22 year career as a nuclear submarine officer, he served as the Director of Life Support and engineering at the Florid Aquarium, Chief Financial Officer of Technology Transfer Services, and 10 years as an Assistant Professor at the University of North Carolina at Charlotte College of Health and Human Services. Dr. Fisher holds a PhD in Information Systems and Decision Sciences from the University of South Florida, a JD from Massachusetts School of Law, and Master's degrees from the Massachusetts Institute of Technology (Ocean Engineering), University of Notre Dame (Administration), Indiana University (Business Administration), and the United States Naval War College (National Security Policy). He is currently a member of the bar in New Hampshire and Massachusetts.
Donna J. Harrison, MD dip ABOG received her MD from the University of Michigan and completed ObGyn residency at a University of Michigan Affiliate hospital (St. Joseph Mercy Hospital). She is currently Executive Director of the American Association of Pro-Life Obstetricians and Gynecologists.
Ingrid Skop received her MD from Washington University School of Medicine, and completed ob/gyn residency at University of Texas Health Science Center, San Antonio. She has practiced obstetrics and gynecology for 23 years, and is the chairman-elect of the American Association of Pro-Life Obstetricians and Gynecologists.
Sharon J. Mackinnon, PhD, RN, FNP has over 25 years of health care experience. MacKinnon completed her doctoral work in Health Services Research at the University of North Carolina at Charlotte. Her current research focuses on the development of secure attachments and experiential relational skills training in local faith communities as they relate to the primary prevention of abortion.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: James Studnicki  https://orcid.org/0000-0003-2958-7493
https://orcid.org/0000-0003-2958-7493
References
- 1. Carr G. Appeals court upholds Louisiana law requiring doctors at abortion facilities to have admitting privileges with nearby hospitals. The Daily Caller. 2018. https://dailycaller.com/2018/09/27/louisiana-abortion-nearby-hospital/. Accessed January 21, 2019.
- 2. American Public Health Association. APHA Policy Statement 20151: opposition to requirements for admitting privileges and transfer agreements for abortion providers. 2015. https://www.apha.org/policies-and-advocacy/public-health-policy-statements/policy-database/2015/12/14/11/04/opposition-to-requirements-for-hospital-admitting-privileges-for-abortion-providers. Accessed January 21, 2019.
- 3. Schaible B. Improving the accuracy of maternal mortality and pregnancy related death. Issues Law Med. 2014;29(2):231–242. [PubMed] [Google Scholar]
- 4. Reardon DC, Coleman PK. Short and long term mortality rates associated with first pregnancy outcome: population register based study for Denmark, 1980–2004. Med Sci Monit. 2012;18(9):PH71–PH76. doi:10.12659/MSM.883338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Gissler M, Kaupilla R, Merilainen J, Toukomaa H, Hemminki E. Pregnancy-associated deaths in Finland, 1987–1994—definition problems and benefits of record linkage. Acta Obstet Gynecol Scand. 1997;76(7):651–657. [DOI] [PubMed] [Google Scholar]
- 6. Raymond EG, Grimes DA. The comparative safety of legal induced abortion and childbirth in the United States. Obstet Gynecol. 2012;119(2 pt 1):215–219. doi:10.1097/AOG.0b013e31823fe923. [DOI] [PubMed] [Google Scholar]
- 7. Provider requirements. Blue Shield of California. 2019. https://www.blueshieldca.com/provider/guidelines-resources/prospective-providers/join/providers-requirements.sp. Accessed January 21, 2019.
- 8. American College of Surgeons. Statement on the patient safety principles for office-based surgery utilizing moderate sedation/analgesia, deep sedation/analgesia or general anesthesia. B Am Coll Surg. 2004;89(4). https://www.facs.org/about-acs/statements/46-office-based-surgery. Accessed January 21, 2019. [PubMed] [Google Scholar]
- 9. Hospital privileging for family physicians. American Academy of Family Physicians. n.d https://www.aafp.org/practice-management/administration/privileging.html. Accessed January 21, 2019.
- 10. Bailey DS. Psychologists’ hospital privileges benefit patients. Monitor Psychology. 2006;37:44 https://www.apa.org/monitor/may06/privileges.aspx. Accessed January 23, 2019. [Google Scholar]
- 11. Primary Care Optometry News. Hospital privileges improve patient care, raise public awareness of optometry. Healio. 2001. https://www.healio.com/optometry/primary-care-optometry/news/print/primary-care-optometry-news/%7B4603b126-3b7d-4e61-87e7-22354f17ac67%7D/hospital-privileges-improve-patient-care-raise-public-awareness-of-optometry. Accessed January 23, 2019.
- 12. Dehlendorf C, Harris LH, Weitz TA. Disparities in abortion rates: a public health approach. Am J Public Health. 2013;103(10):1772–1779. doi:10.2105/ajph.2013.301339. [DOI] [PMC free article] [PubMed] [Google Scholar]