ABSTRACT
Many argue that the solution to the NHS's quality and financial problems lies in the continuing reconfiguration and centralisation of hospital services. However, an ageing population requires good local access to care. This paper reviews the evidence that is available to help guide the reconfiguration of hospital services. The quality overall is poor and, in particular, there is little evidence that reconfiguring hospital services results in financial savings. For acute medical care, there is strong evidence both for enhanced direct and early consultant involvement, and for the importance of comprehensive supporting services. Clinical networks and new technologies may offer opportunities to sustain local access but more evidence is needed to guide network development and to ensure safe but sustainable medical staffing models.
KEYWORDS : Reconfiguration, clinical services, National Clinical Advisory Team, finance, workforce, safety, quality, access
Introduction
The mantra of ‘bigger is better’ has been the received wisdom guiding the reconfiguration of hospital services since the inception of the NHS, and the logic of this view has been compelling. Medical advances have led to clinical staff and equipment in hospitals becoming more specialised. As skilled specialist staff are scarce and budgets are limited, hospital services have become centralised to ensure that patients are cared for by those with the necessary skills and access to both specialist equipment and support services such as critical care. These trends have been reinforced by the limits to junior doctors’ working hours imposed by the European Working Time Directive (EWTD), and by the low numbers of consultant doctors employed in the UK compared with other developed countries.1 Finally, a key factor in determining the configuration of hospital services is clinical co-dependency. This can result in a domino effect whereby the loss of one speciality can destabilise the entire acute service provision in a hospital. Since 1962, the number of acute hospitals in England has reduced by 85%, and the number of sites at which elements of highly specialist care is delivered has reduced even further. The average acute hospital in England now serves a population of 300,000, compared with 54,000 for an average ‘general hospital’ elsewhere in the European Union.1
But is ‘bigger better’ and will continuing to centralise our hospital services, moving them further from the communities they serve, best meet the needs of an ageing population? Nearly two-thirds (65%) of people admitted to hospital are over 65 years old2 and, as described by the Royal College of Physicians3 and its Future Hospital Commission,4 these people have increasingly complex clinical, care and support needs, frequently requiring support from community-based health and social care services.
Simon Stevens (chief executive NHS England) recently argued for more creative thought about future service configuration,5 but what evidence exists from previous reconfigurations to help guide decisions about the future shape of hospital-based acute medical care?
This paper describes some of the evidence gathered as part of a major piece of research funded by the National Institute for Health Research (NIHR)6 and published subsequently by the King's Fund,7 taking as its starting point all of the reviews conducted by the National Clinical Advisory Team (NCAT) between 2007 and 2012. NCAT provided an independent clinical assessment of local reconfiguration proposals. To our knowledge, this is the first review of such a large number of reconfigurations, certainly in the UK.
The majority of the proposals reviewed by NCAT and much of the advice it provided relied on professional guidance as the prime source of evidence rather than peer-reviewed research. The King's Fund research looked for that peer-reviewed research alongside other sources of evidence. Relevant literature, reports, guidance and clinical guidelines were identified using an iterative or emergent approach employing a range of strategies, including hand searching, citation searching, and online keyword searching of healthcare databases, electronic resources and websites. We also sought advice on what we had gathered from key clinical and academic experts and asked them to highlight missing evidence.
What is driving the reconfiguration of services?
The drivers of clinical service change were also investigated. Previously,8 it has been argued that that workforce, quality, cost and access are the four key interlinked factors that need to be taken into account when reconfiguring services, and that the primary challenge is to achieve a configuration that optimises all of these elements. It emerged, however, that cost and workforce far outweighed quality and access in driving service change; finance featuring in 62 (57%) of proposals, and workforce in 53 (49%).
Workforce drivers were predominantly medical. The drive to extend senior medical cover out of hours and at weekends, and limits to the working hours of junior doctors imposed by EWTD, have made traditional medical cover arrangements hard to sustain. The improvement of outcomes and safety was a subsidiary driver, although local proposals often equated improvements in staffing to improvements in quality. Access was barely mentioned as a driver, but its loss was frequently cited (in 34 proposals) as a consequence of change.
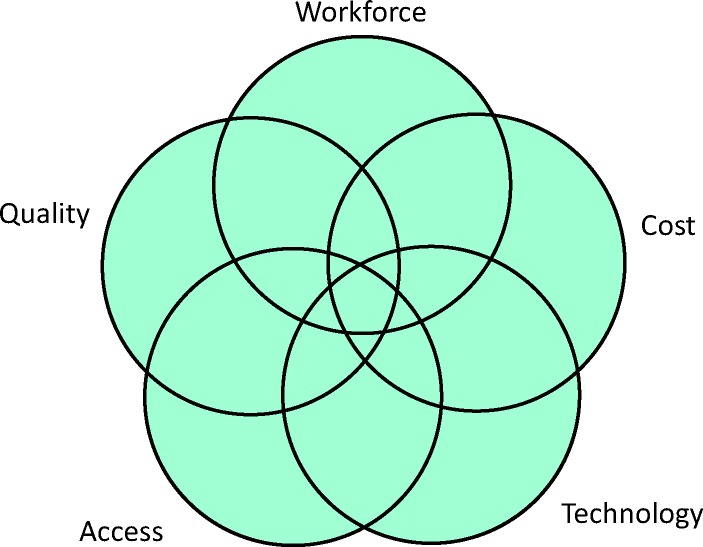
The driver ignored by the analysis described above is technology. While this was rarely mentioned in the NCAT reviews, it has emerged as a potentially significant driver. Digital technologies enable remote monitoring and consultation, and this in turn can help mitigate the pressures to centralise that result from the constraints on medical workforce. This suggests that five, not four, factors are key considerations when analysing clinical service change (see Fig 1).
Fig 1.
The five drivers of clinical service reconfiguration.
The evolving use of technology in healthcare means that both the evidence and the balance of trade off between the different factors is also evolving, and the assessment of benefit should be judged critically with this in mind. It is also important to note that different stakeholders may apportion different emphasis to each factor.8
What evidence is available to guide service change?
The evidence review confirmed longstanding concerns regarding the quality of evidence to guide the reconfiguration of clinical services.9,10 Particular gaps were identified around the impact of service change on finance. For hospital services, this evidence was almost entirely lacking as large-scale reconfiguration of hospital services is rarely tracked and evaluated. For community services, the evidence suggests that community-based alternatives may improve quality but are unlikely to deliver significant net savings. This is particularly worrying given the frequent assumptions that service reconfiguration will deliver large savings, which appear in many of the proposals reviewed by NCAT6 and by national bodies.11
The picture that emerges from the evidence concerning quality improvement is complex. The specialist services reviewed (stroke, trauma and vascular surgery) are areas where the benefits to quality from a more centralised model of care are generally well evidenced. However, as in other services, there was little evidence about the impact of centralisation on cost.
There is strong evidence to support the importance of senior medical and other senior clinical input to care, particularly for high-risk patients (as described more fully below). However, there is less information to guide how many professionals are needed, of what type, and for what time periods.12 In this context, the recent finding by Bray13 that the intensity of nurse staffing at weekends had a bigger impact on stroke outcomes than additional consultant ward rounds is particularly striking. Different specialties and levels of clinical need each require a different balance of senior medical and nursing staff, and have varying requirements for the level of input at night and during the daytime.
There is also increasing recognition of the importance of staff consistently following best-practice guidelines.14 For example, one of the best ways to improve outcomes from high-risk surgery is through the systematic application of known improvement techniques, such as the use of surgical checklists.15 An NCAT report that was particularly relevant in this regard is quoted in Box 1.
Box 1. Strategic reconfiguration of acute sites and quality of care.6

What evidence is available to guide the future configuration of acute medical services?
The research evidence summarised below is broken down according to the five key drivers of reconfiguration: quality, workforce, cost, access and technology. There is also a summary of the evidence on key clinical interdependencies.
Quality
A significant quality issue for acute medical services is the higher observed mortality rate for patients admitted at a weekend (when there is reduced on-site consultant presence) compared with the mortality rate for those admitted during the week.16,17,18 While this observation may in part be linked to a slightly different case mix of patients at weekends,18 it has led to calls for greater seven-day consultant presence, as well as improved access to diagnostics – a recommendation that is supported by the Future Hospital Commission and other authorities. For example, a continuous consultant presence on the acute medical unit is associated with reduced adjusted case fatality rates in hospital,19 and 24/7 consultant-delivered cardiology services are associated with marked reductions in all-cause mortality following admission with acute coronary syndromes.20 National Confidential Enquiry into Patient Outcome and Death (NCEPOD)21,22,23 consistently identifies a lack of consultant input as a contributor to poor-quality care.22
There is also evidence that hospitals with higher numbers of acute medical admissions (40 or more per day) are associated with a reduced adjusted case fatality rate.19 One study showed that consultants who treated greater volumes of medical patients achieved 25% higher survival rates and reduced lengths of stay when compared with ‘low volume’ colleagues.24 There is also an association between hospital volume and outcome for acute myocardial infarction, heart failure and pneumonia, but these benefits are exhausted at relatively low activity thresholds.25 Demonstrating a link between volume and outcomes in medical care is difficult because small units can demonstrate good outcomes while large units can perform poorly.26 This has led some to argue that more attention should be directed to understanding the process of care elements that result in improved outcomes in higher volume or more specialised hospitals, as well as to identifying ways to transfer these improvements from centres of excellence to other hospitals.27
Workforce
The need for more seven-day consultant presence adds to pressures on the consultant workforce3 and, as consultant physicians spend a considerable proportion of their time in outpatient activity, there is a tension between the demands of that service and the support needed for the delivery of high-quality inpatient care.28 There are also pressures on junior doctors as a result of changes to training and limits to working hours. There is evidence that nurses can safely substitute for junior doctors29 and that consultant-delivered multidisciplinary inpatient medical care, where a consultant is supported by a team of nurses and therapists, is as safe as care provided by a consultant-led team of doctors in training (see Box 2). Indeed, multidisciplinary teams may achieve shorter lengths of hospital stay.30 A major challenge is that there is little published data to define the minimum number of physician staff and an appropriate skill mix that will ensure optimum safe practice in acute medicine.12
Box 2. Key clinical and service interdependencies.
The past and anticipated expansion in the consultant workforce should help alleviate these pressures. The general internal and acute medicine consultant workforces grew by 200% between 2005 and 2010,31 but in absolute numbers still represent a relatively small proportion of the total physician workforce. Therefore, the management of emergency medical admissions still relies heavily on the contribution of consultants from other medical specialties. The latest Health Education England workforce plan shows variations in the predicted growth of different medical specialties by 2020, but the majority forecast significant expansion. For example, respiratory medicine is expected to grow by 93%, geriatric medicine by 65% and cardiology by 53% from 2012 to 2020.32 It is uncertain, however, that the forecast expansion will be affordable at a time when NHS budgets are heavily constrained. It is also uncertain whether there will be enthusiasm among graduates to take up these posts as many of the training posts involved in the acute medical take are currently unfilled.33
There is also growing evidence of the benefits of multi-disciplinary team working,30,34 and the opportunity for nurse practitioners and physician’ assistants to substitute for doctors.35 These strategies offer opportunities to reduce the pressure on medical staff while improving the quality of patient care.
Finance
We could find no evidence concerning the financial impact of reconfiguring emergency medical services.
Access
A few studies suggest that increasing distance to hospital is associated with an increased risk of mortality once illness severity has been taken into account. Nicholl et al 36 found that there was a 1% increase in mortality for each 10 km increase in distance, with the effect amplified in people with respiratory distress. The distances between hospitals in England are relatively small. Analysis by Monitor found only five trusts more than 60 km from the next nearest neighbour and only 45 more than 30 km away.37
These distances are relatively small when compared with hospital access in the more rural parts of the USA, Canada and Australia.
Technology
Emergency medical services require onsite critical care support and the capacity to deliver essential intensive care can be a key determinant of whether clinical services are sustainable. A US study of 118,990 patients found that the tele-ICUs had lower mortality rates and lengths of stay, due to case review within an hour of admission by intensivists and shorter response times during crises.38 A literature review of 55 studies found that tele-ICUs improved clinical outcomes.39
Telemedicine also provides opportunities to access specialist advice remotely. There is growing evidence for the benefits of this in the management of stroke40 and in helping to avoid admission for people with acute medical problems in the community.41 However the benefits have not been demonstrated in all areas of medicine and more evidence is needed.42
Summary of evidence7
Consultants should be actively involved in all stages of the care pathway. Acute medical units should have a continuous admitting consultant presence, enabling early consultant review and assessment (within 12 hours). Acute medical services should have rapid access to critical care, a surgical opinion (on site for unselected emergencies, can be off-site if selected), 24/7 access to diagnostics including MRI and CT, and seven-day support from therapies and pharmacy as well as liaison psychiatry. There is some evidence that units and/or consultants that undertake higher volumes of care deliver better outcomes, but the link between volume and outcome is not well understood and may not be the primary driver of improved outcomes.
Conclusions
Pressures in acute medicine encapsulate the challenge for the local hospital. How safe, high-quality services (that are well integrated with local primary and community services) can be realised given workforce and financial constraints remains unclear. There is some evidence to guide us but more is needed.
The balance between access, workforce, quality, finance and technology will vary in relation to patients’ differing levels of clinical risk and complexity. Clinical networks and new technologies offer opportunities to sustain local access, particularly for lower-risk patients, but systems and processes to accurately triage and rapidly transport patients will be required if a more tiered approach to care is adopted. Significant growth is also anticipated in the consultant medical workforce. We need to take account of this or risk designing tomorrow's services within the constraints of today.
Finally, we should never forget that reconfiguration is an important but insufficient approach to improve quality. It should be used alongside measures to strengthen how care is delivered and to instil a culture of improvement.
Acknowledgements
Candace Imison is director of healthcare systems at the Nuffield Trust. She was lead author of ‘The reconfiguration of clinical services: What is the evidence?’ in her previous role as deputy director of policy at The King's Fund. This publication draws on research funded by the National Institute for Health Research Health Services and Delivery Research Programme (project number 12/5001/59).
References
- 1.World Health Organisation , 2011. European database on human and technical resources for health (HealthRes-DB). Available online at http://data.euro.who.int/HlthResDB/ [Accessed 25 January 2014]. [Google Scholar]
- 2.Imison C, Poteliakhoff E, Thompson J. Older people and emergency bed use: exploring variation. London: The King's Fund, 2012. Available online at www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/older-people-and-emergency-bed-use-aug-2012.pdf [Accessed 23 March 2015]. [Google Scholar]
- 3.Royal College of Physicians Hospitals on the edge? The time for action. London: RCP, 2012. Available online at www.rcplondon.ac.uk/projects/hospitals-edge-time-action [Accessed 23 March 2015]. [Google Scholar]
- 4.Royal College of Physicians Future hospital: caring for medical patients. A report from the Future Hospital Commission to the Royal College of Physicians London: RCP, 2013. Available online at www.rcplondon.ac.uk/sites/default/files/consultant_physicians_revised_5th_ed_full_text_final.pdf [Accessed 23 March 2015]. [Google Scholar]
- 5.Stevens S. Thinking like a patient, acting like a tax payer – from NHS challenges to new solutions? Liverpool: NHS England, 2014. Available online at www.england.nhs.uk/2014/06/04/simon-stevens-speech-confed/ [Accessed 23 March 2015]. [Google Scholar]
- 6.Imison C, Sonola L, Honeyman M, Ross S, Edwards N. Insights from the clinical assurance of service reconfiguration in the NHS: the drivers of reconfiguration and the evidence that underpins it. A mixed methods study London: The King's Fund, 2015. Available online at www.nets.nihr.ac.uk/__data/assets/pdf_file/0011/126596/FLS-12-5001-59.pdf [Accessed 23 March 2015]. [PubMed] [Google Scholar]
- 7.Imison C, Sonola L, Honeyman M, Ross S. The reconfiguration of clinical services: what is the evidence. London: The King's Fund, 2014. [Google Scholar]
- 8.Imison C. Reconfiguring hospital services. London: The King's Fund; 2011. Available online at www.kingsfund.org.uk/publications/articles/briefing-reconfiguring-hospital-services [Accessed 23 March 2015]. [Google Scholar]
- 9.Edwards N, Harrison A. Planning hospitals with limited evidence: a research and policy problem. BMJ 1999;319:1361–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Posnett J. Are bigger hospitals better? In: McKee M, Healey J. (eds), Hospitals in a changing Europe. Buckingham: Open University Press, 2002. Available online at www.mheducation.co.uk/openup/chapters/0335209289.pdf [Accessed 23 March 2015]. [Google Scholar]
- 11.Monitor Closing the NHS funding gap: how to get better value health care for patients. London: Monitor; 2013. Available online at www.monitor.gov.uk/sites/default/files/publications/ClosingTheGap091013.pdf [Accessed 23 March 2015]. [Google Scholar]
- 12.Sabin J, Subbe CP, Vaughan L, Dowdle R. Safety in numbers: lack of evidence to indicate the number of physicians needed to provide safe acute medical care. Clin Med 2014;14:462–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bray BD, Ayis S, Campbell J, et al. Associations between stroke -mortality and weekend working by stroke specialist physicians and registered nurses: prospective multicentre cohort study. PLoS Med 2014;11:e1001705. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Prentiss KA, Vinci R. Children in emergency departments: who should provide their care? Arch Dis Child 2009;94:573–6. [DOI] [PubMed] [Google Scholar]
- 15.Finks JF, Osborne NH, Birkmeyer JD. Trends in hospital volume and operative mortality for high-risk surgery. N Engl J Med 2011;364:2128–37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Aylin P, Yunus A, Bottle A, Majeed A, Bell D. Weekend mortality for emergency admissions. A large, multicentre study. Qual Saf Health Care 2010;19:213–7. [DOI] [PubMed] [Google Scholar]
- 17.Freemantle N, Richardson M, Wood J, et al. Weekend hospitalization and additional risk of death: an analysis of inpatient data. J R Soc Med 2012;105:74–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med 2001;345:663–8. [DOI] [PubMed] [Google Scholar]
- 19.Bell D, Lambourne A, Percival F, Laverty AA, Ward DK. Consultant input in acute medical admissions and patient outcomes in hospitals in England: a multivariate analysis. PLoS ONE 2013;8:e61476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ng Kam Chuen MJ, Schofield R, Sankaranarayanan R, et al. Development of a cardiologist delivered service leads to improved outcomes following admission with acute coronary syndromes in a large district general hospital. Acute Card Care 2012;14:1–4. [DOI] [PubMed] [Google Scholar]
- 21.National Confidential Enquiry into Patient Outcome and Death An Acute Problem? A report of the national confidential enquiry into the patient outcome and death. London: NCEPOD, 2005. Available online at www.ncepod.org.uk/2005report/summary.pdf [Accessed 7 December 2013]. [DOI] [PubMed] [Google Scholar]
- 22.National Confidential Enquiry into Patient Outcome and Death Emergency Admissions: a journey in the right direction? London: NCEPOD, 2007. Available online at www.ncepod.org.uk/2007ea.htm [Accessed 23 March 2015]. [Google Scholar]
- 23.National Confidential Enquiry into Patient Outcome and Death Caring to the End? A review of the patients who died in hospital within four days of admission. London: NCEPOD, 2009. Available online at www.ncepod.org.uk/2009dah.htm [Accessed 12 July 2013]. [Google Scholar]
- 24.Conway R, O’Riordan D, Silke B. Consultant volume, as an outcome determinant, in emergency medical admissions. QJM Mon J Assoc Physicians 2013;106:831–7. [DOI] [PubMed] [Google Scholar]
- 25.Ross S, Curry N, Goodwin N. Case management: what is it and how can it be best implemented. London: The King's Fund, 2011. Available online at www.kingsfund.org.uk/sites/files/kf/Case-Management-paper-The-Kings-Fund-Paper-November-2011.pdf [Accessed 23 March 2015]. [Google Scholar]
- 26.Glanville J, Duffy S, Mahon J. et al. The impact of hospital treatment volumes on patient outcomes. York: The University of York, 2010. [Google Scholar]
- 27.Harrison A. Assessing the relationship between volume and outcome in hospital services: implications for service centralization. Health Serv Manage 2012;25:1–6. [DOI] [PubMed] [Google Scholar]
- 28.Royal College of Physicians Hospital workforce. Fit for the future? London: RCP, 2013. Available online at www.rcplondon.ac.uk/sites/default/files/hospital-workforce-fit-for-the-future.pdf [Accessed 23 March 2015]. [Google Scholar]
- 29.Gershengorn HB, Wunsch H, Wahab R, et al. Impact of non-physician staffing on outcomes in a medical ICU. Chest 2011;139:1347–53. [DOI] [PubMed] [Google Scholar]
- 30.Fielding R, Kause J, Arnell-Cullen V, Sandeman D. The impact of consultant-delivered multidisciplinary inpatient medical care on patient outcomes. Clin Med 2013;13:344–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Centre for Workforce Intelligence General internal medicine and acute internal medicine. London: Centre for Workforce Intelligence, 2011. Available online at www.cfwi.org.uk/publications/general-and-acute-internal-medicine-cfwi-medical-fact-sheet-and-summary-sheet-august-2011 [Accessed 31 December 2014]. [Google Scholar]
- 32.Health Education England Investing in people for health and healthcare: workforce plan for England proposed education and training commissions for 2014/15. Health Education England, 2013. Available online at http://hee.nhs.uk/wp-content/uploads/sites/321/2013/12/Workforce-plan-interactive1.pdf [Accessed 30 March 2015]. [Google Scholar]
- 33.Fuller G. Shape of training: a view from the specialties. Clin Med 2014;14:357–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.West MA, Guthrie JP, Dawson JF, Borrill CS, Carter M. Reducing patient mortality in hospitals: the role of human resource -management. J Organ Behav 2006;27:983–1002. [Google Scholar]
- 35.Zwijnenberg NC, Bours GJJW. Nurse practitioners and physician assistants in Dutch hospitals: their role, extent of substitution and facilitators and barriers experienced in the reallocation of tasks. J Adv Nurs 2012;68:1235–46. [DOI] [PubMed] [Google Scholar]
- 36.Nicholl J, West J, Goodacre S, Turner J. The relationship between distance to hospital and patient mortality in emergencies: an -observational study. Emerg Med J 2007;24:665–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Monitor Facing the future: smaller acute providers. London: Monitor, 2014. Available online at www.gov.uk/government/uploads/system/uploads/attachment_data/file/320075/smalleracuteproviders-report.pdf [Accessed 23 March 2015]. [Google Scholar]
- 38.Lilly CM, Zubrow MT, Kempner KM, et al. Critical care telemedicine: evolution and state of the art. Crit Care Med 2015;43:e64. [DOI] [PubMed] [Google Scholar]
- 39.Deslich S, Coustasse A. Expanding technology in the ICU: the case for the utilization of telemedicine. Telemed J E Health 2014;20:485–92. [DOI] [PubMed] [Google Scholar]
- 40.Müller-Barna P, Hubert GJ, Boy S, et al. TeleStroke units serving as a model of care in rural areas: 10-year experience of the TeleMedical Project for integrative stroke care. Stroke J Cereb Circ 2014;45:2739–44. [DOI] [PubMed] [Google Scholar]
- 41.Shah MN, McDermott R, Gillespie SM, Philbrick EB, Nelson D. Potential of telemedicine to provide acute medical care for adults in senior living communities. Acad Emerg Med 2013;20:162–8. [DOI] [PubMed] [Google Scholar]
- 42.Currell R, Urquhart C, Wainwright P, Lewis R. Telemedicine versus face to face patient care: effects on professional practice and health care outcomes. Cochrane Database Syst Rev 2000;(2):CD002098. [DOI] [PubMed] [Google Scholar]
- 43.Royal College of Physicians The interface between acute general medicine and critical care: report of a working party of the Royal College of Physicians. London: RCP, 2002. Available online at www.rcplondon.ac.uk/sites/default/files/documents/interface-acute-general-medicine-critical-care.pdf [Accessed 23 March 2015]. [Google Scholar]
- 44.Hearnshaw SA, Logan RFA, Lowe D, et al. Use of endoscopy for management of acute upper gastrointestinal bleeding in the UK: results of a nationwide audit. Gut 2010;59:1022–9. [DOI] [PubMed] [Google Scholar]
- 45.Royal College of Surgeons Emergency surgery: standards for unscheduled care: guidance for providers, commissioners and service planners. London: RCS, 2011. Available online at www.rcseng.ac.uk/publications/docs/emergency-surgery-standards-for-unscheduled-care/@@download/pdffile/rcs_emergency_surgery_2011_web.pdf [Accessed 23 March 2015]. [Google Scholar]
- 46.Oliver D, Foot C, Humphries R. Making our health and care services fit for an ageing population. London: The King's Fund, 2014. Available online at www.kingsfund.org.uk/publications/making-our-health-and-care-systems-fit-ageing-population [Accessed 23 March 2015]. [Google Scholar]
- 47.NHS NHS Services, Seven Days a Week Forum. Evidence base and clinical standards for the care and onward transfer of acute inpatients. NHS England, 2013. Available online at www.england.nhs.uk/wp-content/uploads/2013/12/evidence-base.pdf [Accessed 23 March 2015]. [Google Scholar]
- 48.Royal College of Psychiatrists Who cares wins: improving the outcome for older people admitted to general hospital. London: Royal College of Psychiatrists, 2005. Available online at www.rcpsych.ac.uk/pdf/whocareswins.pdf [Accessed 23 March 2015]. [Google Scholar]