Abstract
Familial combined hyperlipidemia, which presents as hypercholesterolemia or hypertriglyceridemia, is the commonest form of genetic hyperlipidemia and is associated with premature coronary artery disease. This is a rare case report of a 27 day-old neonate born out of a third-degree consanguineous marriage, with grade III lipemia retinalis secondary to familial-combined hyperlipidemia.
Keywords: Familial combined hyperlipidemia, Lipemia Retinalis, neonate
Lipemia retinalis is a rare manifestation of both primary as well as secondary hyperlipidemia.[1] It was first described by Heyl in 1880 and occurs more commonly in patients with familial hyperchylomicronemia.[2,3] However, it may also be one of the manifestations of familial combined hyperlipidemia, which has a prevalence of 1--2% in the general population.[4] The characteristic fundoscopic changes include retinal blood vessel discoloration, which ranges from salmon pink to creamish white, depending on the level of plasma triglycerides.[1] Fundus changes become evident when the triglyceride levels exceed 2,500 mg/dl.[3]
Case Report
A 27-day-old newborn male was admitted in pediatric ward with chief complains of bleeding from the umbilicus and left ear since 1 day. The bleeding was profuse and light pink in color. Child was born at term, to parents with third-degree consanguineous marriage and was exclusively breastfed since birth. There was family history of hyperlipidemia in the mother and immediate maternal siblings.
Preabdominal examination revealed grade III hepatomegaly and grade II splenomegaly.
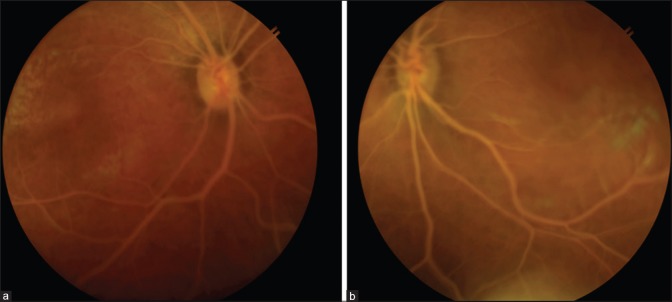
Ophthalmological evaluation was performed and revealed normal anterior segments of both eyes. Fundus examination revealed pale optic discs with peripapillary atrophy, salmon pink retinal background, and tortuous dilated milky white retinal blood vessels bilaterally, suggestive of lipemia retinalis [Fig. 1].
Figure 1.
Fundus Photographs, (a) Right eye, (b) Left eye. In the photographs, a pale optic disc with peripapillary atrophy is visualized along with milky white retinal blood vessels and salmon pink retinal background (Source: By author)
During sampling, his blood was found to be highly viscous and milky. Total serum cholesterol was 4,560 mg/dl (normal range 50--92 mg/dl), serum triglycerides were 10,350 mg/dl (normal range 30--105 mg/dl), serum LDL was 498 mg/dl (normal range 3--39 mg/dl), and serum HDL was 16 mg/dl (normal range 23--58 mg/dl). Serum Apo B was 171 mg/dl (normal range 55--140 mg/dl).[5] Liver, kidney, and thyroid function tests were normal. Hb was 7.6 g/dl.
As genetic testing was not available, the neonate was clinically diagnosed to have lipemia retinalis secondary to familial-combined hyperlipidemia. Other causes of secondary hyperlipidemias, such as obesity, diabetes, liver disease, kidney disease, and hypothyroidism were ruled out in the newborn as well as family members.
The neonate was then weaned on skimmed milk and started on lipid lowering agents. Antibiotics, IV fluids, and blood transfusions were also given. However, the newborn succumbed to sepsis and passed away.
Google Scholar and PubMed databases were reviewed to ascertain the number of cases of lipemia retinalis which have been reported in newborns and infants less than 16 weeks, till the year 2018. To the best of our knowledge only 20 cases have been reported so far [Table 1].
Table 1.
Literature review of cases of Lipemia Retinalis reported in newborns and infants less than 16 weeks, till 2018
| Name of Study | Authors | Journal | Age/Sex of infant | Cause of Lipemia Retinalis |
|---|---|---|---|---|
| Lipemia Retinalis in a 29-day-old infant with type 1 hyperlipoproteinaemia. | Hayasaka et al., 1985[6] | British Journal of Ophthalmology | 29 days/Female | Hyperlipoproteinemia |
| Lipemia Retinalis of prematurity | Ikesugi et al., 1996[7] | Archives of Ophthalmology | 28 days (Premature baby born at 31 weeks)/Male | Hyperlipemia secondary to lipoprotein lipase deficiency |
| Lipemia Retinalis in a premature infant with type I hyperlipoproteinaemia | Rotchford et al., 1997[8] | Eye | 11 weeks (Premature baby born at 26 weeks)/Female | Familial chylomicronemia |
| Lipoprotein lipase deficiency | Shankar et al., 1997[9] | Journal of Postgraduate Medicine | 12 weeks/Male | Hyperlipemia secondary to lipoprotein lipase deficiency |
| Familial combined hyperlipidemia in a North Indian kindred | Sriram et al., 2005[4] | Indian Journal of Pediatrics | 16 weeks/Male | Familial combined hyperlipidemia |
| Lipemia retinalis in a 35-day-old infant with hyperlipoproteinemia: case report | Cypel et al., 2008[10] | Abo-Arquivos Brasileiros Oftalmologia | 35 days/Female | Hyperlipoproteinemia |
| Pink-creamy whole blood in a 3-month-old infant with a homozygous deletion in the lipoprotein lipase gene | Avis et al., 2010[11] | Clinical Genetics | 12 weeks/Female | Hyperlipemia secondary to lipoprotein lipase deficiency |
| Grade III Lipemia Retinalis in a newborn | Čermàkovà et al., 2010[12] | Acta Ophthalmologica | 28 days/Female | Hyperlipemia secondary to lipoprotein lipase deficiency |
| Lipoprotein lipase deficiency in an infant | Nampoothiri et al., 2011[13] | Indian Pediatrics | 38 days/Male | Familial chylomicronemia |
| Lipemia Retinalis: case report and review of the literature | Zahavi et al., 2013[3] | Journal of American Association for Pediatric Ophthalmology and Strabismus | 12 weeks/Male | Hyperlipemia secondary to lipoprotein lipase deficiency |
| An Infant with Milky Blood: An Unusual but Treatable Case of Familial Hyperlipidemia | Chaurasiya et al., 2013[14] | Indian Journal of Clinical Biochemistry | 8 weeks/Male | Familial hyperlipidemia |
| A 3-day-old neonate with severe hypertriglyceridemia from novel mutations of the GPIHBP1 gene | Buonuomo et al., 2015 [15] | Journal of clinical Lipidology | 3 days/Female | Familial chylomicronemia with GPIHBP1 gene mutation |
| Lipemia Retinalis | Chaudhury et al., 2015[1] | Delhi Journal of Ophthalmology | 12 weeks/Female | Hypertriglyceridemia |
| Familial Chylomicronemia Syndrome (FCS) in a 10- Day- Old Neonate: A Case Report | Manzoor et al., 2015[16] | International Journal of Pediatrics | 10 days/Female | Familial chylomicronemia syndrome (FCS) |
| Severe Hypertriglyceridemia due to a novel p.Q240H mutation in the Lipoprotein Lipase gene | Soto et al., 2015[17] | Lipids in Health and Disease | 11 weeks (Premature baby born at 26 weeks)/Male | Hypertriglyceridemia secondary to p.Q240H mutation in the lipoprotein lipase gene |
| Exceptionally elevated triglyceride in severe Lipemia Retinalis | Yin et al., 2016[18] | International Medical Case Reports Journal | 6 weeks/Female | Hypertriglyceridemia |
| Extreme hypertriglyceridemia, pseudohyponatremia, and pseudoacidosisin a neonate with lipoprotein lipase deficiency due to segmental uniparentaldisomy | Ashraf et al., 2017[19] | Journal of clinical Lipidology | 36 days/Female | Hyperlipemia secondary to lipoprotein lipase deficiency |
| Familial chylomicronemia: A rare case report | Sowjanya et al., 2017[20] | Indian Journal of Case report | 5 days/Female | Familial chylomicronemia |
| Lipemia Retinalis in a 1 month old infant | Jain et al., 2017[21] | Oman Journal of Ophthalmology | 28 days/Female | Hyperlipemia secondary to lipoprotein lipase deficiency |
| Lipemia Retinalis in an infant treated for retinopathy of prematurity | Jain et al., 2017[22] | Journal of American Association for Pediatric Ophthalmology and Strabismus | 14 days (Premature baby born at 30 weeks)/Female | Hypertriglyceridemia |
Discussion
Hyperlipidemias may be classified as primary or secondary. Primary hyperlipidemias are mainly genetic and include conditions listed in Table 2.[23] Secondary hyperlipidemias are attributed to lifestyle and other factors such as diabetes, liver or kidney disease, hypothyroidsm, alcohol abuse.
Table 2.
Conditions causing Primary Hyperlipidemia
| Genetic Hyperlipidemias | |
|---|---|
| Disorder | Mechanism |
| Familial hypercholesterolemia | LDL receptor defect |
| Familial defective Apo B-100 | Apo B (LDL receptor-binding region) defect |
| PCSK9 gain of function mutations | Increased degradation of LDL receptors |
| Polygenic hypercholesterolemia | Unknown; Multiple mechanisms |
| LPL deficiency | Endothelial LPL defect |
| Apo C-II deficiency | Apo C-II; Functional LPL deficiency |
| Familial hypertriglyceridemia | Unknown; Multiple mechanisms |
| Familial combined hyperlipidemia | Unknown; Multiple mechanisms |
| Familial dysbetalipoproteinemia | Apo E; Reduced chylomicron and VLDL clearance |
| Primary hypoalphalipoproteinemia | Unknown; Multiple mechanisms |
| Familial Apo AI deficiency/mutations | Apo AI |
| Familial LCAT deficiency | LCAT gene |
| Fisheye disease (partial LCAT deficiency) | LCAT gene |
| Tangier disease | ABCA1 gene |
| Familial HDL deficiency | ABCA1 gene |
| Hepatic lipase deficiency | Hepatic lipase |
| Cerebrotendinous xanthomatosis | Hepatic mitochondrial 27-hydroxylase defect |
| Sitosterolemia | ABCG5 and ABCG8 genes |
| Cholesteryl ester storage disease and Wolman disease | Lysosomal acid lipase deficiency |
Source: Goldberg[23]
Lipemia retinalis is the ocular manifestation of marked hyperlipidemia, more commonly hypertriglyceridemia, and fundus changes begin to manifest when the serum triglyceride level exceeds 2,500 mg/dl.[3] It starts off by affecting the periphery and later the posterior pole of the retina.[24] The grading system of lipemia retinalis has been given by Vinger et al.[25] [Table 3]. The arteries as well as veins assume the creamish milky white color and can be distinguished only by their size. However, reversal of signs may be expected with the reduction of serum triglyceride levels.[26] According to the above grading system, the neonate in this case report was found to have grade III changes.
Table 3.
Grading of Lipemia Retinalis
| Grade | Intensity | Clinical Appearance |
|---|---|---|
| I | Early | White and creamy aspect of peripheral retinal vessels |
| II | Moderate | Creamy-colored vessels extending towards optic disc |
| III | Marked | Salmon-colored retina, all vessels having milky aspect |
Source: Vinger and Sachs[25]
Familial combined hyperlipidemia, which shows prevalence of 1--2% in the general population, is the commonest form of genetic hyperlipidemia and carries a high risk of premature coronary artery disease. This condition should be ruled out in any child presenting with high levels of serum total cholesterol and serum triglycerides, with a positive family history of hyperlipidemia, as there is no single diagnostic marker for this condition.[4,27]
As per our literature review, very few cases of lipemia retinalis have been reported in newborns and infants. Out of the 20 cases which we reviewed, seven cases were reported in male infants, out of which only three were in newborn males. Out of these three cases, one was reported in a 38-day-old male and was found to be secondary to familial chylomicronemia and the other two were reported in premature babies, the former being in a 28-day-old neonate born at 31 weeks gestation, which was due to familial hyperlipidemia secondary to lipoprotien lipase deficieny, whereas the latter was in a 11-week-old infant born at 26 weeks gestation which was secondary to hypertriglyceridemia because of p.Q240H mutation in the lipoprotein lipase gene. Among female newborns, the youngest case has been reported in a 3-day-old neonate, which was secondary to familial chylomicronemia with GPIHBP1 gene mutation.
To the best of our knowledge, no other case of familial combined hyperlipidemia showing grade III lipemia retinalis, with such markedly elevated serum total cholesterol and serum triglycerides levels, has been reported in a neonate as young as 27 days, which makes this case report unique.
Furthermore, it was also noticed in the literature review that few cases of lipemia retinalis have been accidentally detected while screening premature newborns for retinopathy of prematurity. This warrants appropriate referral of suspicious cases and their detailed ophthalmological evaluation in order to detect the presence of lipemia retinalis.
Medical management in patients with familial-combined hyperlipidemia consists of restriction of dietary fats, such as the use of skimmed milk in this case and use of lipid lowering drugs such as statins, which have proven safety and efficacy for short-term use in newborns and infants.[28]
Conclusion
Persistent and uncontrolled hypercholesterolemia and hypertriglyceridemia, especially in newborns and infants, can lead to other morbidities such as premature atherosclerosis and coronary artery disease, pancreatitis, hepatic failure, which may be fatal.[27] Hence, early detection and demonstration of lipemia retinalis in such cases is important.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Chaudhury D, Meenakshi R, Ramakrishnan R, Mitra A, Raju S. Lipaemia retinalis. Delhi J Ophthalmol. 2015;26:107–10. [Google Scholar]
- 2.Heyl A. Intra-ocular lipæmia. Trans Am Ophthalmol Soc. 1880;3:54–66. [PMC free article] [PubMed] [Google Scholar]
- 3.Zahavi A, Snir M, Kella YR. Lipemia retinalis: Case report and review of the literature. J AAPOS. 2013;17:110–1. doi: 10.1016/j.jaapos.2012.10.010. [DOI] [PubMed] [Google Scholar]
- 4.Sriram CS, Gulati S, Chopra V, Vashist S, Menon PSN. Familial combined hyperlipidemia in a North Indian kindred. Indian J Pediatr. 2005;72:987–9. doi: 10.1007/BF02731678. [DOI] [PubMed] [Google Scholar]
- 5.Chandar V, Gidvani C, Gupta A, Wilson C, Sharma Y. Lipid profile in normal healthy children. Med J Armed Forces India. 1994;50:101–4. doi: 10.1016/S0377-1237(17)31008-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hayasaka S, Fukuyo T, Kitaoka M, Suzuki H, Omura K, Kondo Y, et al. Lipaemia retinalis in a 29-day-old infant with type 1 hyperlipoproteinaemia. Br J Ophthalmol. 1985;69:280–2. doi: 10.1136/bjo.69.4.280. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ikesugi K, Doi M, Nishi A, Uji Y. Lipemia retinalis of prematurity. Arch Ophthalmol. 1996;114:1283–4. doi: 10.1001/archopht.1996.01100140483027. [DOI] [PubMed] [Google Scholar]
- 8.Rotchford AP, Newman DK, Moore AT, Flanagan DW, Miles R. Lipaemia retinalis in a premature infant with type I hyperlipoproteinaemia. Eye. 1997;11:940–1. doi: 10.1038/eye.1997.235. [DOI] [PubMed] [Google Scholar]
- 9.Shankar K, Bava H, Shetty J, Joshi M. Lipoprotein lipase deficiency. J Postgrad Med. 1997;43:81–2. [PubMed] [Google Scholar]
- 10.Cypel M, Manzano R, Reis F. Lipemia retinalis in a 35-day-old infant with hyperlipoproteinemia: Case report. Arq Bras Oftalmol. 2008;71:254–6. doi: 10.1590/s0004-27492008000200022. [DOI] [PubMed] [Google Scholar]
- 11.Avis HJ, Scheffer HJ, Kastelein JJP, Dallinga-Thie GM, Wijburg FA. Pink-creamy whole blood in a 3-month-old infant with a homozygous deletion in the lipoprotein lipase gene. Clin Genet. 2010;77:430–3. doi: 10.1111/j.1399-0004.2009.01369.x. [DOI] [PubMed] [Google Scholar]
- 12.Čermàkovà I, Pettenazzo A, Perrone S, Burlina A, Zannin ME. Grade III lipaemia retinalis in a newborn. Acta Ophthalmol. 2010;88:e141–2. doi: 10.1111/j.1755-3768.2009.01581.x. [DOI] [PubMed] [Google Scholar]
- 13.Nampoothiri S, Radhakrishnan N, Schwentek A, Hoffmann MM. Lipoprotein lipase deficiency in an infant. Indian Pediatr. 2011;48:805–6. [PubMed] [Google Scholar]
- 14.Chaurasiya OS, Kumar L, Sethi RS. An infant with milky blood: An unusual but treatable case of familial hyperlipidemia. Indian J Clin Biochem. 2013;28:206–9. doi: 10.1007/s12291-012-0285-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Buonuomo PS, Bartuli A, Rabacchi C, Bertolini S, Calandra S. A 3-day-old neonate with severe hypertriglyceridemia from novel mutations of the GPIHBP1 gene. J Clin Lipidol. 2015;9:265–70. doi: 10.1016/j.jacl.2014.10.003. [DOI] [PubMed] [Google Scholar]
- 16.Wani K, Rashid M, Alaqaband MM, Manzoor S, Mushtaq S. Familial chylomicronemia syndrome (FCS) in a 10- day- old neonate: A case report. Int J Pediatr. 2015;3:449–53. [Google Scholar]
- 17.Soto AG, McIntyre A, Agrawal S, Bialo SR, Hegele RA, Boney CM. Severe hypertriglyceridemia due to a novel p.Q240H mutation in the lipoprotein lipase gene. Lipids Health Dis. 2015;14:102–5. doi: 10.1186/s12944-015-0107-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Yin HY, Warman R, Suh EH, Cheng AMS. Exceptionally elevated triglyceride in severe lipemia retinalis. Int Med Case Rep J. 2016;9:333–6. doi: 10.2147/IMCRJ.S118594. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ashraf AP, Hurst ACE, Garg A. Extreme hypertriglyceridemia, pseudohyponatremia, and pseudoacidosis in a neonate with lipoprotein lipase deficiency due to segmental uniparental disomy. J Clin Lipidol. 2017;11:757–62. doi: 10.1016/j.jacl.2017.03.015. [DOI] [PubMed] [Google Scholar]
- 20.Sowjanya S, Lakshmi V, Thiagarajan K. Familial chylomicronemia: A rare case report. Indian J Case Rep. 2017;3:211–5. [Google Scholar]
- 21.Jain NC, Vanteri J, Shah PK, Narendran V. Lipemia retinalis in 1-month-old infant. Oman J Ophthalmol. 2017;10:50–1. doi: 10.4103/0974-620X.200698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Jain A, Mochi TB, Braganza SD, Agrawal S, Shetty BK, Pachiyappan B. Lipemia retinalis in an infant treated for retinopathy of prematurity. J AAPOS. 2017;21:254–7. doi: 10.1016/j.jaapos.2017.05.021. [DOI] [PubMed] [Google Scholar]
- 23.Goldberg A. Dyslipidemia (Hyperlipidemia) Merck Manual Prof Ver. 2018 [Google Scholar]
- 24.Martinez K, Cibis G, Tauber J. Lipemia retinalis. Arch Ophthalmol Ophthalmol. 1992;110:1171. doi: 10.1001/archopht.1992.01080200151044. [DOI] [PubMed] [Google Scholar]
- 25.Vinger PF, Sachs BA. Ocular manifestations of hyperlipoproteinemia. Am J Ophthalmol. 1970;70:563–7. doi: 10.1016/0002-9394(70)90890-1. 569-73. [DOI] [PubMed] [Google Scholar]
- 26.Ram J, Pandav SS, Sandeep J, Ram J, Gupta A, Sharma A. Reversal of lipaemia retinalis with dietary control. Eye. 1993;7:763–5. doi: 10.1038/eye.1993.178. [DOI] [PubMed] [Google Scholar]
- 27.Cortner JA, Coates PM, Liacouras CA, Jarvik GP. Familial combined hyperlipidemia in children: Clinical expression, metabolic defects, and management. J Pediatr. 1993;123:177–84. doi: 10.1016/s0022-3476(05)81686-5. [DOI] [PubMed] [Google Scholar]
- 28.Thompson G. Lipid lowering in the young. Heart. 1996;76:1–2. doi: 10.1136/hrt.76.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]